|
1
|
Tickoo SK, de Peralta-Venturina MN, Harik
LR, Worcester HD, Salama ME, Young AN, Moch H and Amin MB: Spectrum
of epithelial neoplasms in end-stage renal disease: An experience
from 66 tumor-bearing kidneys with emphasis on histologic patterns
distinct from those in sporadic adult renal neoplasia. Am J Surg
Pathol. 30:141–153. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gobbo S, Eble JN, Grignon DJ, Martignoni
G, Maclennan GT, Shah RB, Zhang S, Brunelli M and Cheng L: Clear
cell papillary renal cell carcinoma: A distinct histopathologic and
molecular genetic entity. Am J Surg Pathol. 32:1239–1245. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Aydin H, Chen L, Cheng L, Vaziri S, He H,
Ganapathi R, Delahunt B, Maqi-Galluzzi C and Zhou M: Clear cell
tubulopapillary renal cell carcinoma: A study of 36 distinctive
low-grade epithelial tumors of the kidney. Am J Surg Pathol.
34:1608–1621. 2010.PubMed/NCBI
|
|
4
|
Adam J, Couturier J, Molinié V,
Vieillefond A and Sibony M: Clear-cell papillary renal cell
carcinoma: 24 cases of a distinct low-grade renal tumour and a
comparative genomic hybridization array study of seven cases.
Histopathology. 58:1064–1071. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Srigley JR, Delahunt B, Eble JN, Egevad L,
Epstein JI, Grignon D, Hes O, Moch H, Montironi R, Tickoo SK, et
al: The International Society of Urological Pathology (ISUP)
Vancouver Classification of renal neoplasia. Am J Surg Pathol.
37:1469–1489. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Moch H, Cubilla AL, Humphrey PA, Reuter VE
and Ulbright TM: The 2016 WHO Classification of Tumours of the
urinary system and male genital organs-part A: Renal, penile, and
testicular tumours. Eur Urol. 70:93–105. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhou H, Zheng S, Truong LD, Ro JY, Ayala
AG and Shen SS: Clear cell papillary renal cell carcinoma is the
fourth most common histologic type of renal cell carcinoma in 290
consecutive nephrectomies for renal cell carcinoma. Hum Pathol.
45:59–64. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Park JH, Lee C, Suh JH and Moon KC: Clear
cell papillary renal cell carcinoma: A report of 15 cases including
three cases of concurrent other-type renal cell carcinomas. Korean
J Pathol. 46:541–547. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Williamson SR, Eble JN, Cheng L and
Grignon DJ: Clear cell papillary renal cell carcinoma: Differential
diagnosis and extended immunohistochemical profile. Mod Pathol.
26:697–708. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Alexiev BA and Drachenberg CB: Clear cell
papillary renal cell carcinoma: Incidence, morphological features,
immunohistochemical profile, and biologic behavior: A single
institution. Pathol Res Pract. 210:234–241. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bhatnagar R and Alexiev BA: Renal-cell
carcinomas in end-stage kidneys: A clinicopathological study with
emphasis on clear-cell papillary renal-cell carcinoma and acquired
cystic kidney disease-associated carcinoma. Int J Surg Pathol.
20:19–28. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Aron M, Chang E, Herrera L, Hes O, Hirsch
MS, Comperat E, Camparo P, Rao P, Picken M, Michal M, et al: Clear
cell-papillary renal cell carcinoma of the kidney not associated
with end-stage renal disease: Clinicopathologic correlation with
expanded immunophenotypic and molecular characterization of a large
cohort with emphasis on relationship with renal angiomyoadenomatous
tumor. Am J Surg Pathol. 39:873–888. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Leroy X, Camparo P, Gnemmi V, Aubert S,
Flamand V, Roupret M, Fantoni JC and Compérat E: Clear cell
papillary renal cell carcinoma is an indolent and low-grade
neoplasm with overexpression of cyclin-D1. Histopathology.
64:1032–1036. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rao P, Monzon F, Jonasch E, Matin SF and
Tamboli P: Clear cell papillary renal cell carcinoma in patients
with von Hippel-Lindau syndrome-clinicopathological features and
comparative genomic analysis of 3 cases. Hum Pathol. 45:1966–1972.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gill S, Kauffman EC, Kandel S, George S,
Schwaab T and Xu B: Incidence of clear cell papillary renal cell
carcinoma in low-grade renal cell carcinoma cases: A 12-year
retrospective clinicopathologic study from a single cancer center.
Int J Surg Pathol. 24:207–212. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sahni VA, Hirsch MS and Silverman SG:
Renal angiomyoadenomatous tumour: Imaging features. Can Urol Assoc
J. 6:E140–E143. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shao T, Yousef P, Shipilova I, Saleeb R,
Lee JY and Krizova A: Clear cell papillary renal cell carcinoma as
part of histologically discordant multifocal renal cell carcinoma:
A case report and review of literature. Pathol Res Pract.
212:229–233. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shi SS, Shen Q, Xia QY, Tu P, Shi QL, Zhou
XJ and Rao Q: Clear cell papillary renal cell carcinoma: A
clinicopathological study emphasizing ultrastructural features and
cytogenetic heterogeneity. Int J Clin Exp Pathol. 6:2936–2942.
2013.PubMed/NCBI
|
|
19
|
Deml KF, Schildhaus HU, Compérat E, von
Teichman A, Storz M, Schraml P, Bonventre JV, Fend F, Fleige B,
Nerlich A, et al: Clear cell papillary renal cell carcinoma and
renal angiomyoadenomatous tumor: Two variants of a morphologic,
immunohistochemical, and genetic distinct entity of renal cell
carcinoma. Am J Surg Pathol. 39:889–901. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yan WX, Cao WR, Zhao J, Zhang W, Wang XL,
Yuan Q and Dang SQ: Clear cell papillary renal cell carcinoma: A
clinicopathologic analysis of 6 cases. Int J Clin Exp Pathol.
8:4595–4599. 2015.PubMed/NCBI
|
|
21
|
Lawrie CH, Larrea E, Larrinaga G,
Goicoechea I, Arestin M, Fernandez-Mercado M, Hes O, Cáceres F,
Manterola L and López JI: Targeted next-generation sequencing and
non-coding RNA expression analysis of clear cell papillary renal
cell carcinoma suggests distinct pathological mechanisms from other
renal tumour subtypes. J Pathol. 232:32–42. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Diolombi ML, Cheng L, Argani P and Epstein
JI: Do clear cell papillary renal cell carcinomas have malignant
potential? Am J Surg Pathol. 39:1621–1634. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Alexiev BA and Zou YS: Clear cell
papillary renal cell carcinoma: A chromosomal microarray analysis
of two cases using a novel Molecular Inversion Probe (MIP)
technology. Pathol Res Pract. 210:1049–1053. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fisher KE, Yin-Goen Q, Alexis D,
Sirintrapun JS, Harrison W, Benjamin Isett R, Rossi MR, Moreno CS,
Young AN and Osunkoya AO: Gene expression profiling of clear cell
papillary renal cell carcinoma: Comparison with clear cell renal
cell carcinoma and papillary renal cell carcinoma. Mod Pathol.
27:222–230. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Munari E, Marchionni L, Chitre A, Hayashi
M, Marrtignoni G, Brunelli M, Gobbo S, Arqani P, Allaf M, Hoque MO
and Netto GJ: Clear cell papillary renal cell carcinoma: micro-RNA
expression profiling and comparison with clear cell renal cell
carcinoma and papillary renal cell carcinoma. Hum Pathol.
45:1130–1138. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Alexiev BA, Thomas C and Zou YS: Clear
cell papillary renal cell carcinoma with angiomyomatous stroma: A
histological, immunohistochemical, and fluorescence in situ
hybridization study. Virchows Arch. 464:709–716. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Dhakal HP, Mckenney JK, Khor LY, Reynolds
JP, Magi-Galluzzi C and Przybycin CG: Renal neoplasms with
overlapping features of clear cell renal cell carcinoma and clear
cell papillary renal cell carcinoma: A clinicopathologic study of
37 cases from a single institution. Am J Surg Pathol. 40:141–154.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
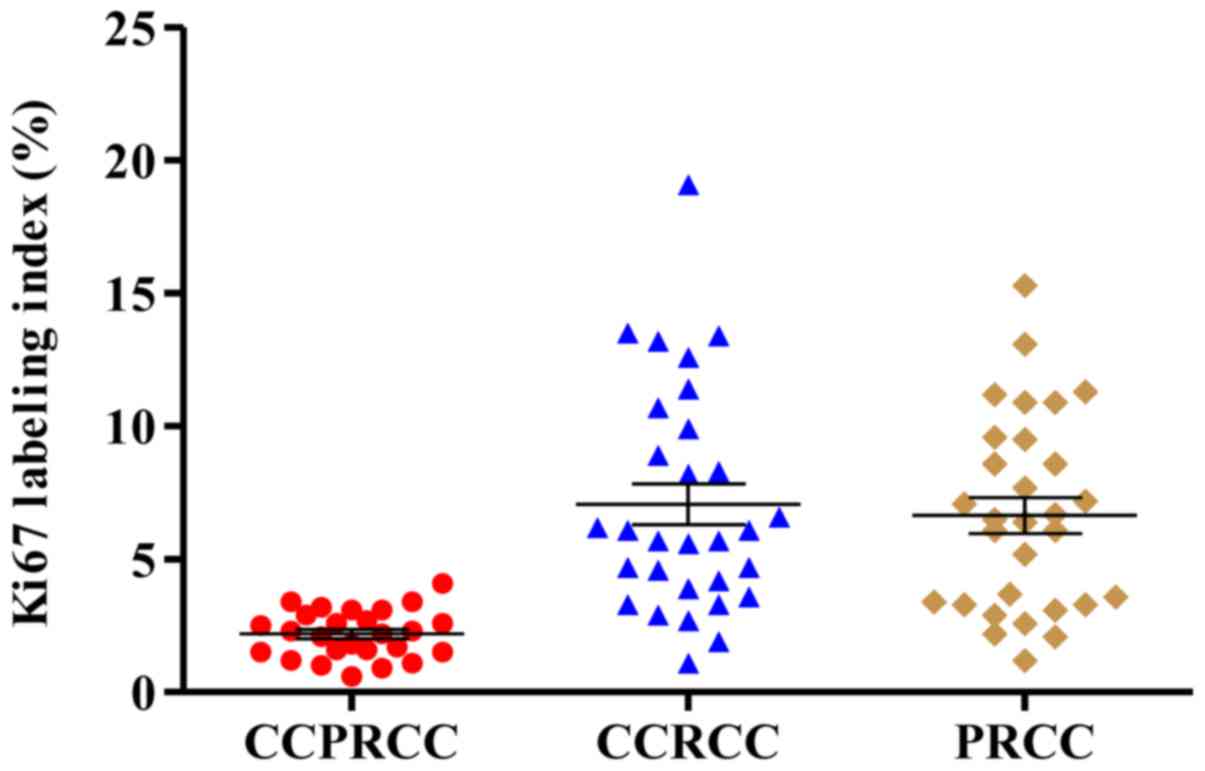
Delahunt B, Bethwaite PB, Thornton A and
Ribas JL: Proliferation of renal cell carcinoma assessed by
fixation-resistant polyclonal Ki-67 antibody labeling. Correlation
with clinical outcome. Cancer. 75:2714–2719. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chow WH, Gridley G, Fraumeni JF Jr and
Järvholm B: Obesity, hypertension, and the risk of kidney cancer in
men. New Engl J Med. 343:1305–1311. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sanfilippo KM, Mctigue KM, Fidler CJ,
Neaton JD, Chang Y, Fried LF, Liu S and Kuller LH: Hypertension and
obesity and the risk of kidney cancer in 2 large cohorts of US men
and women. Hypertension. 63:934–941. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Khandekar MJ, Cohen P and Spiegelman BM:
Molecular mechanisms of cancer development in obesity. Nat Rev
Cancer. 11:886–895. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Shoji K, Tanaka T and Nangaku M: Role of
hypoxia in progressive chronic kidney disease and implications for
therapy. Curr Opin Nephrol Hypertens. 23:161–168. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kabaria R, Klaassen Z and Terris MK: Renal
cell carcinoma: Links and risks. Int J Nephrol Renovasc Dis.
9:45–52. 2016.PubMed/NCBI
|
|
34
|
Weikert S, Boeing H, Pischon T, Weikert C,
Olsen A, Tjonneland A, Overvad K, Becker N, Linseisen J,
Trichopoulou A, et al: Blood pressure and risk of renal cell
carcinoma in the European prospective investigation into cancer and
nutrition. Am J Epidemiol. 167:438–446. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kuroda N, Ohe C, Kawakami F, Mikami S,
Furuya M, Matsuura K, Moriyama M, Nagashima Y, Zhou M, Petersson F,
et al: Clear cell papillary renal cell carcinoma: A review. Int J
Clin Exp Pathol. 7:7312–7318. 2014.PubMed/NCBI
|
|
36
|
Pramick M, Ziober A and Bing Z: Useful
immunohistochemical panel for differentiating clear cell papillary
renal cell carcinoma from its mimics. Ann Diagn Pathol. 17:437–440.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Gayed BA, Youssef RF, Bagrodia A, Darwish
OM, Kapur P, Sagalowsky A, Lotan Y and Margulis V: Ki67 is an
independent predictor of oncological outcomes in patients with
localized clear-cell renal cell carcinoma. BJU Int. 113:668–673.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Gerdes J: Ki-67 and other proliferation
markers useful for immunohistological diagnostic and prognostic
evaluations in human malignancies. Semin Cancer Biol. 1:199–206.
1990.PubMed/NCBI
|
|
39
|
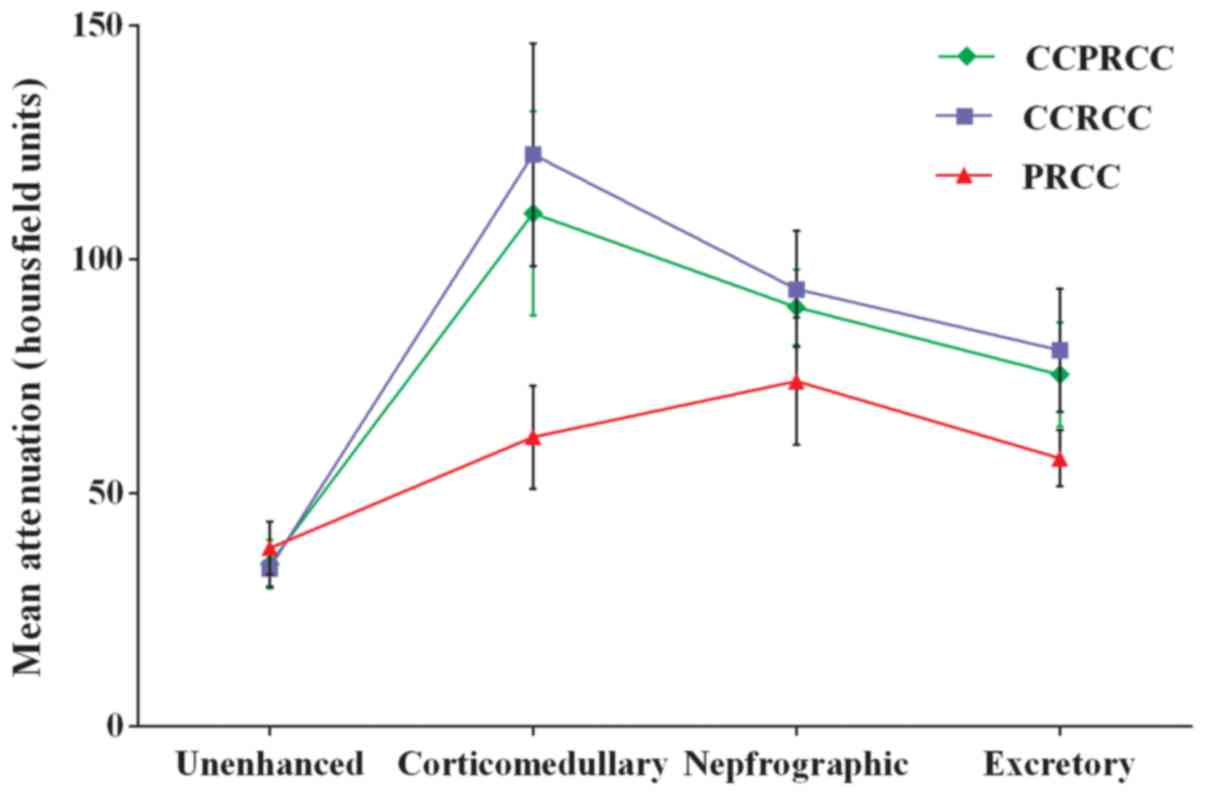
Young JR, Margolis D, Sauk S, Pantuck AJ,
Sayre J and Raman SS: Clear cell renal cell carcinoma:
Discrimination from other renal cell carcinoma subtypes and
oncocytoma at multiphasic multidetector CT. Radiology. 267:444–453.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zhang J, Lefkowitz RA, Ishill NM, Wang L,
Moskowitz CS, Russo P, Eisenberg H and Hricak H: Solid renal
cortical tumors: Differentiation with CT. Radiology. 244:494–504.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Tsuda K, Kinouchi T, Tanikawa G, Yasuhara
Y, Yanagawa M, Kakimoto K, Ono Y, Meguro N, Maeda O, Arisawa J and
Usami M: Imaging characteristics of papillary renal cell carcinoma
by computed tomography scan and magnetic resonance imaging. Int J
Urol. 12:795–800. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kim JM, Song PH, Kim HT and Park TC: The
prognostic factors for patients with pT1a renal cell carcinoma.
Korean J Urol. 51:233–238. 2010. View Article : Google Scholar : PubMed/NCBI
|