Introduction
Papillary thyroid cancer (PTC) is the most common
subtype of thyroid cancer, accounting for more than 90% of all
cases (1). The incidence of PTC has
been increasing rapidly in recent years, largely because of
advances in early detection using ultrasonography and fine-needle
aspiration biopsy (1,2). Cervical lymph node metastases are common
in patients with PTC, in whom the reported metastatic rate is
30–80%, with the central neck being the most common site (3,4).
Recurrence following treatment is common, occurring in up to 30% of
all patients and 75% of local recurrence occurs in the central
neck; it can occur up to 20 years after the initial diagnosis
(5,6),
Therapeutic central neck dissection (CND) is routinely performed in
patients with PTC and clinically positive lymph nodes (7,8). Although
the use of prophylactic CND in patients with clinically negative
lymph nodes remains controversial because of its potential
morbidity and unclear benefit (9,10), many
clinicians continue to recommend prophylactic CND owing of the high
rate of central lymph node metastasis; however, up to 80% of
positive lymph node are undetectable, microscopic metastatic lymph
node disease (11,12). Prophylactic CND can remove microscopic
disease in central lymph nodes, which is unlikely to be eradicated
by radioactive iodine therapy (13).
Evidence indicates that prophylactic CND may prevent recurrence and
improve overall survival (14).
Reoperation for recurrent PTC in the central lymph node has a high
rate of complications, including, hypoparathyroidism and recurrent
laryngeal nerve palsy (15).
Prophylactic CND can permit accurate nodal staging [one-third of
patients increased to stage III disease due to lymph node
metastasis detected by prophylactic CND (16)] and provide information about prognosis
and guidelines for treatments such as radioactive iodine therapy
and hormone suppression therapy (17). Routine prophylactic CND has been
recommended by the Japanese Society of Thyroid Surgeons and the
French Society of Otolaryngology Head and Neck Surgery (18).
Controversy remains regarding the extent of
prophylactic CND in unilateral PTC (unilateral vs. bilateral CND).
Although the majority of metastatic lymph nodes are located in the
ipsilateral central neck, the metastatic rate of bilateral central
neck was reported to be 18.9–30.6% (19). Owing to the potential higher risks of
complications for bilateral CND and the lower metastatic rate of
contralateral central neck, efforts have been made to predict
contralateral central neck metastasis using clinicopathological
characteristics (8). As a novel
lymphatic tracer, the use of carbon nanoparticles (CNs) have been
reported to efficiently guide CND (20). The present study reports the use of
CNs on predicting contralateral central neck metastasis and
evaluates its clinical value.
Materials and methods
Imaging agent for lymphatic
vessels
CNs (China Food and Drug Administration approval no.
H20041829; Chonqing Lummy Pharmaceutical Co., Ltd., Chongqing,
China) can be injected as a suspension (50 mg/ml) (21,22). This
product is a stable suspension of CNs 150 nm in diameter. The
diameter of the CNs is greater than the capillary endothelial cell
gap (20–50 nm) and smaller than the lymphatic capillary endothelial
cell gap (120–500 nm), so a small proportion of the CNs may be
captured by macrophages, then enter the lymphatic duct but not the
blood circulation. There have been no reports of CNs exerting toxic
side effects in humans (23,24).
Patients
A total of 70 consecutive patients were enrolled
into this study between January 2012 and June 2013; all patients
were diagnosed with PTC by preoperative aspiration pathology and
underwent the initial surgery in the Department of Head and Neck
Surgery, Peking University Cancer Hospital & Institute
(Beijing, China), all the tumors were located in one lobe. The
inclusion criterion was PTC (size of lesion, 1–4 cm). Exclusion
criteria included non-thyroid cancer, previous thyroid or
parathyroid surgery, preoperative hypoparathyroidism or
hypocalcemia, pregnancy or lactation, surgery confirming suspicion
of the presence of lateral neck lymph node metastasis, age <18
years, and an inability to comply with the follow-up protocol. In
total, 14 patients were males and 56 were female, with a male to
female ratio of 1:4. The ages of patients ranged between 19 and 75
years, with a median of 45.23 years. All surgery was performed by
the same medical team, and all the patients underwent total or
near-total thyroidectomy plus bilateral CND. Approval was obtained
from the Ethics Committee of Beijing University Cancer Hospital
prior to these procedures; all patients provided informed consent
for inclusion in the present study.
Surgical procedure
All patients underwent general anesthesia
intubation, and were placed supinely with necks hyperextended. A
transverse incision of ~5 cm was performed in a skin crease 2 cm
above the sternal notch. The skin, subcutaneous tissue, and
platysma were cut layer by layer. Flap separation was performed
under the platysma before making a longitudinal incision in the
linea alba cervicalis. The strap muscles retracted and the front
ipsilateral thyroid was revealed; the side and rear parts of the
lobe were kept intact to reduce damage to the lymphatic network
around the thyroid. In the CN group, 0.1 ml of carbon nanoparticles
per point was injected into tissues surrounding the tumor using a
skin test syringe. In total, 2 or 3 spots were injected for each
tumor, with the total amount injected being no more than 0.5 ml per
lobe. Prior to injection, the CN suspension was inserted deeply and
aspirated to ensure it would not be injected into the blood
vessels. The CNs suspension was slowly injected into the thyroid
tissues. Upon completion, gentle pressure was applied on the needle
puncture site to prevent solution leakage.
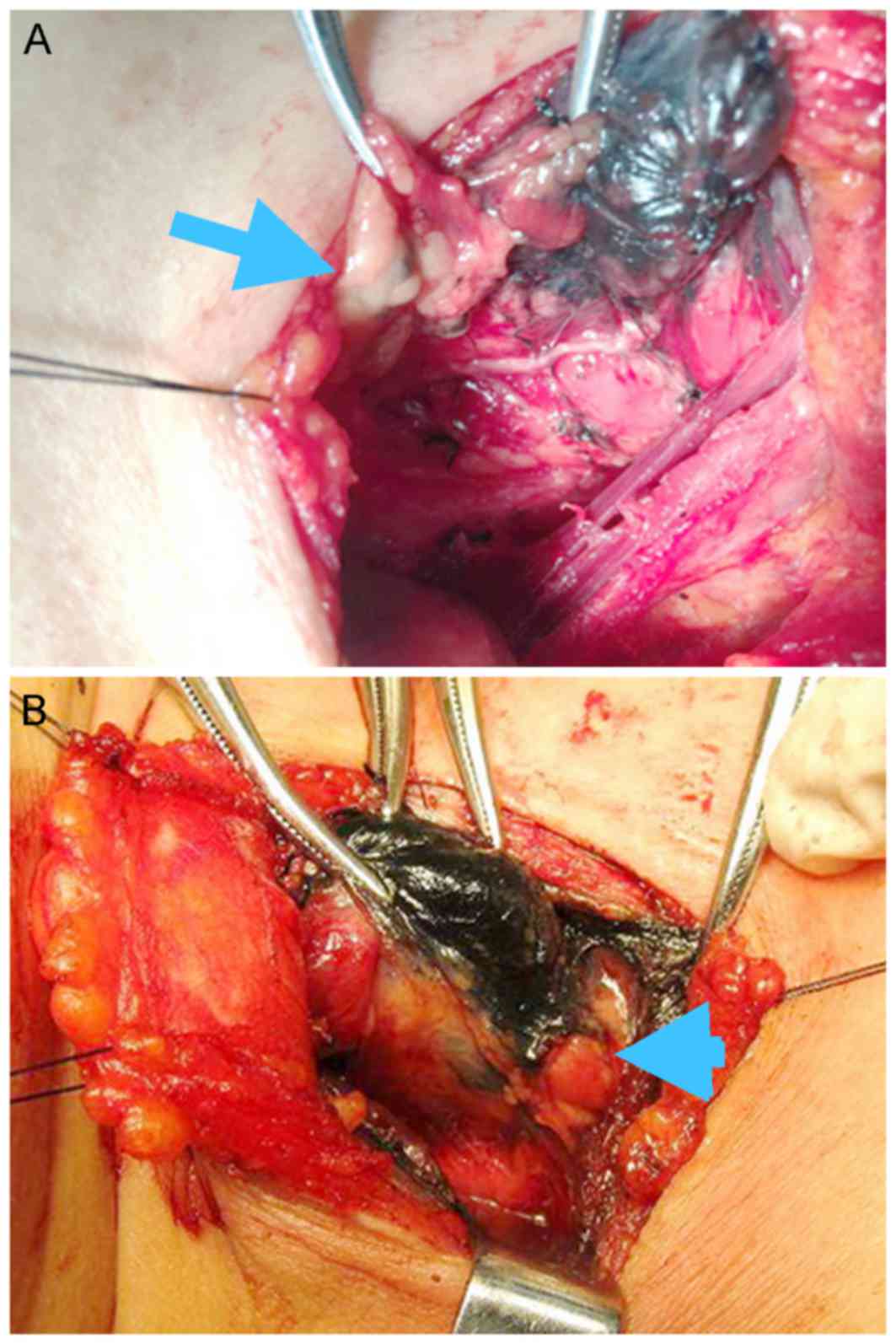
After 5 min, the lymphatic ducts and the lymph nodes
became black-stained (Fig. 1). Total
thyroidectomy or near-total thyroidectomy was then performed
according to the meticulous capsular dissection technique. Node
clearance of the central neck compartment was performed cranially
to the two superior thyroid arteries and the pyramidal lobe,
caudally to the innominate vein, laterally to the carotid sheaths,
and dorsally to the prevertebral fascia (25). When the thyroidectomy was completed,
the tumors were sent for routine frozen pathology examination to
confirm the preoperative aspiration pathological diagnosis.
Ipsilateral CND included the removal of prelaryngeal, pretracheal
and paratracheal nodes on the side of the tumor. The resected
specimens of lymph nodes were carefully checked and labeled as
being either black-stained or non-stained in the CN group. All
metastatic lymph node specimens were sent for pathological
examination. Specimens were checked for the presence of the
parathyroid, for unintentionally removed parathyroid glands, frozen
section biopsy of one-fourth to one-third of the removed
parathyroid glands was performed during surgery for pathological
confirmation. When confirmed to be the parathyroid gland, the
remaining tissue was transplanted into the sternocleidomastoid
muscle.
Surveillance and management of
postoperative complications
Serum calcium was assessed at 6:00 am on the first
postoperative day, postoperative hypocalcemia was defined as a
calcium level of <2.0 mmol/l (reference range, 2.10–2.60
mmol/l), with or without clinical symptoms of hypocalcemia or
subnormal serum calcium levels (2.0–2.1 mmol/l) with neuromuscular
symptoms. Calcium supplementation was not routinely administered to
patients. Calcium and vitamin D were routinely prescribed to
patients with symptomatic hypocalcemia, Intravenous substitution of
calcium was not routine unless serious symptomatic hypocalcemia was
present. Vocal cord palsy, as confirmed by laryngoscopy, was
considered permanent if it lasted for >6 months.
Statistical analysis
The Student t-test and χ2 test were used
for the measurement and count data, respectively. SPSS 17.0 (SPSS,
Inc., Chicago, IL, USA) was used to perform statistical analysis;
P<0.05 was considered to indicate a statistically significant
difference.
Results
General information of patients
The clinicopathological characteristics of the
patients are summarized in Table I.
All the tumors were located in one lobe. All patients underwent
total or near-total thyroidectomy plus bilateral CND. Papillary
thyroid cancer was confirmed by perioperative and postoperative
pathology for all patients. The mean age of all the patients was
45.49±18.97 years (range, 19–75 years). Of the patients enrolled,
52.86% (37/70) were <45 years of age, and 47.14% (33/70) were
≥45 years of age. A total of 56 women (80.00%) and 14 men (20.00%)
participated. The mean size of the primary tumor was 1.98±0.72 cm.
All patients had a primary tumor ≥1 cm, multifocal tumors were
observed in 16 patients (22.86%). Extrathyroid extension was
observed in 28 patients (40.00%).
 | Table I.The clinical pathological
characteristics of the patients. |
Table I.
The clinical pathological
characteristics of the patients.
| Clinicopathological
characteristics | Value |
|---|
| Age,
yearsa | 45.49±18.97 |
|
<45 | 37 (52.86) |
| ≥45 | 33 (47.14) |
| Sex, n |
|
| Male | 14 |
|
Female | 56 |
| Size of primary
tumor, cma | 1.98±0.72 |
| Extrathyroid
extention, n (%) | 28 (40.00) |
| Multifocal tumor, n
(%) | 16 (22.86) |
Central lymph node metastasis
The central lymph node metastasis status of the
patients is summarized in Table II.
Of the enrolled 70 patients, 51 patients (72.86%) were confirmed to
have lymph node metastasis in the central neck. A total of 50
(71.43%) patients had lymph node positive for metastasis in the
ipsilateral central neck, which included the prelaryngeal,
pretracheal and paratracheal nodes on the side of the tumor. By
contrast, 14 (20.00%) patients had contralateral central neck lymph
node metastases, with only 1 (1.43%) exhibiting contralateral
metastasis but not the ipsilateral central compartment metastasis
(skip metastasis). A total of 682 lymph nodes were found in this
group, with an average of 9.74±4.33 per patient (range, 4–22
pieces). The diameter of 279 (40.91%) lymph nodes was <5 mm.
Among the 682 detected lymph nodes, 579 (84.90%) were black-stained
by CNs. Of the 193 metastatic lymph nodes, 168 were located in
ipsilateral central compartment and the other 25 in the
contralateral central compartment. Of the 193 metastatic lymph
nodes, 147 (76.17%) were black-stained and the other 46 (23.83%)
were not. A total of 63 metastatic lymph nodes were found that were
<5 mm in the metastatic black-stained lymph nodes. A total of
128 lymph nodes were stained black in the ipsilateral central
compartment and 21 in the contralateral central compartment; 4
metastatic lymph nodes in the contralateral central compartment
were not stained black. The sensitivity and specificity of CNs for
contralateral metastasis were 84 and 25%, respectively. Statistical
analysis of the clinicopathological factors associated with
contralateral lymph nodes metastases (Table III) revealed that contralateral
central lymph nodes metastasis was significantly associated with
extrathyroid extension and the presence of ipsilateral central neck
lymph node metastasis. By contrast, sex, presence of multifocality
and age were not associated with contralateral lymph nodes
metastasis. Of the 14 patients with contralateral central neck
lymph node metastasis, 13 had nodes positive for metastasis in the
ipsilateral central neck and 9 patients had extrathyroid
extension.
 | Table II.Central neck metastasis of patients
under the guidance of carbon nanoparticles. |
Table II.
Central neck metastasis of patients
under the guidance of carbon nanoparticles.
| Variables (%) | Ipsilateral central
neck, n (%) | Contralateral
central neck, n |
|---|
| Patients with
metastases | 50 (71.43) | 12 (17.14) |
| Dissected lymph
nodes | 425 | 257 |
| Lymph nodes <5
mm | 161 (37.88) | 118 (45.91) |
| Black stained lymph
nodes | 384 (90.35) | 195 (75.88) |
| Metastatic lymph
nodes | 168 (39.53) | 25 (9.73) |
| Black-stained
metastatic lymph nodes | 126 (75.00) | 21
(84.00) |
 | Table III.Clinicopathological factors
associated with contralateral central neck metastasis. |
Table III.
Clinicopathological factors
associated with contralateral central neck metastasis.
| Variable | Patients with
central neck contralateral metastasis, n (%) | P-value |
|---|
| Age, years |
|
|
|
<45 | 7 (18.92) |
|
|
≥45 | 7 (21.21) | 0.811 |
| Sex |
|
|
|
Male | 3 (11.00) |
|
|
Female | 11 (45.00) | 0.881 |
| Extrathyroid
extension |
|
|
|
Yes | 9 (32.14) |
|
| No | 5 (11.90) | 0.038 |
| Multifocal
tumor |
|
|
|
Yes | 4 (25.00) |
|
| No | 10 (18.52) | 0.569 |
| Ipsilateral central
neck lymph node |
|
|
|
Yes | 13 (26.00) |
|
| No | 1 (5.26) | 0.047 |
Side effects and operative
complications
No evident systemic toxicity occurred in these
patients during and following surgery. Hoarseness occurred to two
patients due to tumor adhesion. Notably, the parathyroid glands
could be well protected during surgery as parathyroid glands could
not be stained black, unlike the black-stained lymph nodes
(Fig. 1), so could be easily
distinguished and kept in situ. In total, 12 patients
(17.14%) were confirmed to be hypocalcemia. Pathological results
revealed that 5 incidences of accidental parathyroid resection
occurred; the resected parathyroid glands were re-implanted into
sternocleidomastoid muscle, as described previously (26).
Discussion
Central neck lymph node metastasis is fairly common
in papillary thyroid cancer and is observed in 20–90% of patients
(1,2,12).
Therapeutic CND is routinely performed in patients with PTC with
lymph nodes clinically positive for metastasis (7,8). Although
controversy exists regarding prophylactic CND in patients with
clinically negative lymph nodes owing to its potential morbidity
and unclear benefit (9,10). At the time of writing, there was no
effective means of predicting central neck lymph node metastasis.
Ultrasound and computerized tomography are the most common methods
used to preoperatively evaluate metastatic lymph nodes in PTC
patients (27,28). Ultrasound is a sensitive and specific
test for detecting lateral cervical lymph node metastasis; however,
it was not sufficiently sensitive in assessing central neck lymph
nodes owing to the presence of multifocal thyroid nodules and
surrounding structures in the central neck (27). Ultrasound has a sensitivity of 66.3%
with a specificity of 88.4% (27).
Computerized tomography has been found to have a sensitivity of 67%
and a specificity of 79–91% (28).
Positron emission tomography is not routinely preoperatively used
in PTC patients as its sensitivity has been reported to be <40%
(29).
Microcarcinoma and tumors >1 cm require different
surgical treatment, as certain microcarcinomas may be treated
without surgery (30), whilst tumors
>1 cm must be treated by surgery. A tumor size >1 cm was
reported to be an independent predictor of central metastasis and
disease-free survival (25); as such,
only patients with tumors >1 cm were selected as subjects in the
present study. In the study group, 51 patients (72.86%) were
confirmed to have lymph node metastasis in the central neck, 50
(71.43%) in the ipsilateral central neck, and 14 (20.00%) patients
in the contralateral central neck. The results of the present
study, in accordance with those of a previous study, indicate that
ipsilateral central neck metastasis was the most frequently
involved region in the central neck compartment (25). Skip metastasis is generally uncommon
(31), and was only observed in one
patient (1.43%) in the present study, characterized by metastasis
to the contralateral but not the ipsilateral central compartment.
The results of the current study revealed that contralateral
central lymph node metastasis was significantly associated with the
presence of ipsilateral central neck lymph node metastasis, a
finding that was also strongly supported by other studies (9,25,32). Lim et al (33) demonstrated that ipsilateral central
lymph node metastasis was the only independent predictor for the
presence of contralateral central lymph node metastasis and
suggested that elective contralateral CND should be considered when
performing initial surgery for PTC with a tumor diameter of >1
cm and the presence of ipsilateral central lymph node metastasis.
The results of the present study also revealed that contralateral
central lymph nodes metastasis was significantly associated with
extrathyroid extension, which tallied with the findings of previous
studies (10,25), whereas extrathyroid extension was
difficult to diagnose pre- or intra-operatively. Other factors
associated with contralateral lymph nodes metastasis are male
gender, lateral neck lymph nodes metastasis and tumor multifocality
(34,35). Among these clinicopathological
factors, ipsilateral central lymph node metastasis was strongly
indicated to be the predictive factors. Raffaelli et al
(36) reported that routine
ipsilateral CND plus frozen section examination of the ipsilateral
nodes may represent a valid alternative to prophylactic bilateral
CND. As the rate of metastasis to the ipsilateral central neck is
high, many metastatic lymph nodes are too small to be detected by
frozen section examination, meaning that this strategy may aid
prediction of contralateral central lymph node metastasis.
Recently, a suspension of CNs has been used to aid
the identification lymph nodes in lymph node dissection (20). This product is a stable suspension of
CNs of 150 nm in diameter, which is greater than the capillary
endothelial cell gap (20–50 nm) and smaller than the lymphatic
capillary endothelial cell gap (120–500 nm). Following injection
into the thyroid glands around the tumor, CNs are rapidly captured
by macrophages. The particles then enter the lymphatic vessels and
accumulate in the lymph nodes, staining them black. CNs have been
successfully used in the detection of sentinel lymph nodes in
breast and gastric cancer (21). Hao
et al (37) used CNs as
tracers for sentinel lymph node biopsy on patients with papillary
thyroid microcarcinoma who underwent CND; the sensitivity,
specificity, accuracy rate, and false negative rate were 93.3, 100,
97 and 5.2%, respectively. The authors concluded that the CNs
method better aided the screening and selection of patients who are
most likely to benefit from cervical lymph node dissection
(37). CNs stain the majority of
lymph nodes, with the reported rate of CN staining was 69.89–95.26%
(20,37,38), with
the black-staining rate in the present study being 84.90%. More
lymph nodes <5 mm were detected with the assistance of CNs,
which cannot be easily recognized without any assistance. The
diameter of 279 (40.91%) lymph nodes in the present study was <5
mm. Zhu et al (20) reported
that significantly more small lymph nodes, particularly those <2
mm, were detected, compared with the control group for whom CNs
were not used. A total of 63 metastatic lymph nodes were found that
were <5 mm in the metastatic black-stained lymph nodes in this
study using CNs.
CNs have been demonstrated to detect more lymph
nodes, particularly small lymph nodes in the present study. To the
best of our knowledge, the present study evaluated the potential
role of predicting contralateral central lymph node metastasis in
PTC under the guidance of CNs for the first time. The results of
the present study revealed that 21/25 (84%) metastatic lymph nodes
were stained black in the contralateral central compartment. the
sensitivity and specificity of CNs for contralateral metastasis
were 84 and 25%, respectively. CNs may be useful to aid prediction
of the presence of contralateral central lymph node metastasis; the
majority of the metastatic lymph nodes were stained black, the
black-stained lymph nodes may be resected for fast-frozen pathology
to determine whether contralateral CND should be performed.
Additionally, all the black stained lymph nodes may be resected
(limited CND) instead of standard CND, so as to decrease the
potential complications (such as hypoparathyroidism and recurrent
laryngeal nerve palsy). Further studies could evaluate whether fast
frozen pathology or limited CND is feasibility in prophylactic
contralateral CND.
The present study found that, unlike the lymph
nodes, parathyroid glands could not be stained black following CNs
injection, as revealed in previous studies (20,37). CNs
cannot enter the blood circulation, meaning that parathyroid glands
and the surrounding blood supply appear different from the
black-stained lymph nodes. In total, 12 patients (17.14%) were
confirmed to be hypocalcemic in the present study, lower than the
number found in a previous study (30.77%) (39) (the patients in the two studies
received the same treatment). Further study is warranted to
evaluate the potential protective role of CNs to the parathyroid
glands.
The results of the present study indicate that the
use of CNs is safe, and that no evident systemic toxicity was
observed in patients during and following surgery. These results
suggest that CNs can effectively predict contralateral CND, which
could have promise in clinical use.
Acknowledgements
The authors would like to thank Professor Wei Zhao
from the Beijing Cancer Hospital for providing technical assistance
during the experiments.
Funding
The present study was supported by Beijing Cancer
Hospital Fund (grant no. 10-02).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
WY performed the experiments and wrote the
manuscript. JS and NZ analyzed and interpreted the patient data. GX
was a major contributor in the design of the study, and writing of
the manuscript.
Ethics approval and consent to
participate
Ethical approval was obtained from the Ethics
Committee of Beijing University Cancer Hospital prior to these
procedures, and all patients provided informed consent for
inclusion in the present study.
Consent for publication
All patients provided informed consent for inclusion
in the present study, and provided consent for publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen AY, Jemal A and Ward EM: Increasing
incidence of differentiated thyroid cancer in the United States,
1988–2005. Cancer. 115:3801–3807. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cooper DS, Doherty GM, Haugen BR, Kloos
RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Sherman SI and
Tuttle RM: American Thyroid Association Guidelines Taskforce:
Management guidelines for patients with thyroid nodules and
differentiated thyroid cancer. Thyroid. 16:109–142. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shaha AR, Shah JP and Loree TR: Patterns
of nodal and distant metastasis based on histologic varieties in
differentiated carcinoma of the thyroid. Am J Surg. 172:692–694.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hay ID, Thompson GB, Grant CS, Bergstralh
EJ, Dvorak CE, Gorman CA, Maurer MS, McIver B, Mullan BP, Oberg AL,
et al: Papillary thyroid carcinoma managed at the Mayo Clinic
during six decades (1940–1999): Temporal trends in initial therapy
and long-term outcome in 2444 consecutively treated patients. World
J Surg. 26:879–885. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wong KP and Lang BH: The role of
prophylactic central neck dissection in differentiated thyroid
carcinoma: Issues and controversies. J Oncol. 2011:1279292011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Keum HS, Ji YB, Kim JM, Jeong JH, Choi WH,
Ahn YH and Tae K: Optimal surgical extent of lateral and central
neck dissection for papillary thyroid carcinoma located in one lobe
with clinical lateral lymph node metastasis. World J Surg Oncol.
10:2212012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sadowski BM, Snyder SK and Lairmore TC:
Routine bilateral central lymph node clearance for papillary
thyroid cancer. Surgery. 146:696–705. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Carling T, Long WD III and Udelsman R:
Controversy surrounding the role for routine central lymph node
dissection for differentiated thyroid cancer. Curr Opin Oncol.
22:30–34. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shaha AR: Prophylactic central compartment
dissection in thyroid cancer: A new avenue of debate. Surgery.
146:1224–1227. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Clark OH: Thyroid cancer and lymph node
metastases. J Surg Oncol. 103:615–618. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kouvaraki MA, Shapiro SE, Fornage BD,
Edeiken-Monro BS, Sherman SI, Vassilopoulou-Sellin R, Lee JE and
Evans DB: Role of preoperative ultrasonography in the surgical
management of patients with thyroid cancer. Surgery. 134:946–955.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Besic N, Pilko G, Petric R, Hocevar M and
Zgajnar J: Papillary thyroid microcarcinoma: Prognostic factors and
treatment. J Surg Oncol. 97:221–225. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tisell LE, Nilsson B, Mölne J, Hansson G,
Fjälling M, Jansson S and Wingren U: Improved survival of patients
with papillary thyroid cancer after surgical microdissection. World
J Surg. 20:854–859. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lundgren CI, Hall P, Dickman PW and
Zedenius J: Clinically significant prognostic factors for
differentiated thyroid carcinoma: A population-based, nested
case-control study. Cancer. 106:524–531. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hughes DT, White ML, Miller BS, Gauger PG,
Burney RE and Doherty GM: Influence of prophylactic central lymph
node dissection on postoperative thyroglobulin levels and
radioiodine treatment in papillary thyroid cancer. Surgery.
148:1100–1107. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kim WW, Park HY and Jung JH: Surgical
extent of central lymph node dissection in clinically node-negative
papillary thyroid cancer. Head Neck. 35:1616–1620. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Takami H, Ito Y, Okamoto T and Yoshida A:
Therapeutic strategy for differentiated thyroid carcinoma in Japan
based on a newly established guideline managed by Japanese Society
of Thyroid Surgeons and Japanese Association of Endocrine Surgeons.
World J Surg. 35:111–121. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Roh JL, Kim JM and Park CI: Central lymph
node metastasis of unilateral papillary thyroid carcinoma: Patterns
and factors predictive of nodal metastasis, morbidity, and
recurrence. Ann Surg Oncol. 18:2245–2250. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhu Y, Chen X, Zhang H, Chen L, Zhou S, Wu
K, Wang Z, Kong L and Zhuang H: Carbon nanoparticle-guided central
lymph node dissection in clinically node-negative patients with
papillary thyroid carcinoma. Head Neck. 38:840–845. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Catarci M, Guadagni S, Zaraca F, Pistoia
MA, Mastracchio A, Trecca A, Ruco L and Carboni M: Prospective
randomized evaluation of preoperative endoscopic vital staining
using CH-40 for lymph node dissection in gastric cancer. Ann Surg
Oncol. 5:580–584. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cai HK, He HF, Tian W, Zhou MQ, Hu Y and
Deng YC: Colorectal cancer lymph node staining by activated carbon
nanoparticles suspension in vivo or methylene blue in vitro. World
J Gastroenterol. 18:6148–6154. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
de Freitas Conti LC, Phelan E, Liu L,
Gardecki J, Namati E, Warger WC, Tearney GJ and Randolph GW:
Optical coherence tomography imaging during thyroid and parathyroid
surgery: A novel system of tissue identification and
differentiation to obviate tissue resection and frozen section.
Head Neck. 36:1329–1334. 2014.PubMed/NCBI
|
|
24
|
Ladurner R, Hallfeldt KK, Al Arabi N,
Stepp H, Mueller S and Gallwas JK: Optical coherence tomography as
a method to identify parathyroid glands. Lasers Surg Med.
45:654–659. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Glover AR, Gundara JS, Norlén O, Lee JC
and Sidhu SB: The pros and cons of prophylactic central neck
dissection in papillary thyroid carcinoma. Gland Surg. 2:196–205.
2013.PubMed/NCBI
|
|
26
|
Kihara M, Miyauchi A, Kontani K, Yamauchi
A and Yokomise H: Recovery of parathyroid function after total
thyroidectomy: Long-term follow-up study. ANZ J Surg. 75:532–536.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lee YJ, Kim DW, Park HK, Kim DH, Jung SJ,
Oh M and Bae SK: Pre-operative ultrasound diagnosis of nodal
metastasis in papillary thyroid carcinoma patients according to
nodal compartment. Ultrasound Med Biol. 41:1294–1300. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mulla M and Schulte KM: Central cervical
lymph node metastases in papillary thyroid cancer: A systematic
review of imaging-guided and prophylactic removal of the central
compartment. Clinical Endocrinol (Oxf). 76:131–136. 2012.
View Article : Google Scholar
|
|
29
|
Kim BS, Ryu HS and Kang KH: The value of
preoperative PET-CT in papillary thyroid cancer. J Int Med Res.
41:445–456. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Feng J and Wang J: Diagnosis and treatment
of thyroid microcarcinoma. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke
Za Zhi. 28:1911–1917. 2014.(In Chinese). PubMed/NCBI
|
|
31
|
Machens A, Holzhausen HJ and Dralle H:
Skip metastases in thyroid cancer leaping the central lymph node
compartment. Arch Surg. 139:43–45. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ito Y, Jikuzono T, Higashiyama T, Asahi S,
Tomoda C, Takamura Y, Miya A, Kobayashi K, Matsuzuka F, Kuma K and
Miyauchi A: Clinical significance of lymph node metastasis of
thyroid papillary carcinoma located in one lobe. World J Surg.
30:1821–1828. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lim YC, Choi EC, Yoon YH, Kim EH and Koo
BS: Central lymph node metastases in unilateral papillary thyroid
microcarcinoma. Br J Surg. 96:253–257. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lee KE, Chung IY, Kang E, do Koo H, Kim
KH, Kim SW, Youn YK and Oh SK: Ipsilateral and contralateral
central lymph node metastasis in papillary thyroid cancer: Patterns
and predictive factors of nodal metastasis. Head Neck. 35:672–676.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mamelle E, Borget I, Leboulleux S,
Mirghani H, Suárez C, Pellitteri PK, Shaha AR, Hamoir M, Robbins
KT, Khafif A, et al: Impact of prophylactic central neck dissection
on oncologic outcomes of papillary thyroid carcinoma: A review. Eur
Arch Otorhinolaryngol. 272:1577–1586. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Raffaelli M, De Crea C, Sessa L, Fadda G,
Bellantone C and Lombardi CP: Ipsilateral central neck dissection
plus frozen section examination versus prophylactic bilateral
central neck dissection in cN0 papillary thyroid carcinoma. Ann
Surg Oncol. 22:2302–2308. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hao RT, Chen J, Zhao LH, Liu C, Wang OC,
Huang GL, Zhang XH and Zhao J: Sentinel lymph node biopsy using
carbon nanoparticles for Chinese patients with papillary thyroid
microcarcinoma. Eur J Surg Oncol. 38:718–724. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sun SP, Zhang Y, Cui ZQ, Chen Q, Zhang W,
Zhou CX, Xie PP and Liu BG: Clinical application of carbon
nanoparticle lymph node tracer in the VI region lymph node
dissection of differentiated thyroid cancer. Genet Mol Res.
13:3432–3437. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Yu W, Wang T and Zhang N: Parathyroid
protection in surgery of bilateral papillary thyroid cancer.
Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 50:406–410. 2015.(In
Chinese). PubMed/NCBI
|