Introduction
Metastasis is a major cause of mortality in breast
cancer. The metastatic cascade is composed of a series of
biological steps that enables tumor cells to detach from the
primary tumor, invade into the bloodstream and lymphatic system,
extravasate into the parenchyma and establish a new metastatic
lesion (1). This process may occur at
the early stages of breast cancer. Circulating tumor cells (CTCs)
may have a crucial role in the metastatic cascade and are a
prognostic factor in patients with primary and metastatic breast
cancer (2). CTC dissemination, as a
part of metastasis, is a highly inefficient process, and only a
minority of tumor cells that escape from local and systemic immune
surveillance are capable of forming metastases (3–5).
Therefore, immune changes in the primary tumor microenvironment may
be involved in the dissemination of CTCs in breast cancer. Current
evidence concerning the association between CTCs and the immune
system in breast cancer is limited (6,7).
Tumor-infiltrating lymphocytes (TILs) are
heterogeneous immune cells infiltrating in the tumor
microenvironment and are considered to be the main components of
the body's immune surveillance mechanism against cancer. In breast
cancer, TILs are a heterogeneous population that may promote
humoral and cellular antitumor responses (3,8). For
example, as the predominant T lymphocytes infiltrate the tumor
microenvironment, cluster of differentiation CD8+ T
lymphocytes may exert cytotoxic activity towards tumor cells by
triggering apoptosis (9). Therefore,
CD8+ T lymphocytes are hypothesized to be the frontline
defense against cancer. Several studies have observed an
association between a high number of CD8+ TILs and
favorable clinical outcomes (10,11). When
CD8+ T lymphocytes fail to eliminate tumor cells, these
tumors cells, which have reduced immunogenicity, may break through
the primary tumor microenvironment (12). Accordingly, poor infiltration of
CD8+ T lymphocytes may have a role in the initial
dissemination of CTCs. Apart from a decrease in immune
surveillance, several subsets of TILs are known to suppress
anti-tumor immunity (3), which may
participate in the dissemination of CTCs.
Considerable attention has been paid to regulatory T
cells (Tregs), which have been identified as forkhead box
(Foxp)3+ T cells (12,13). Tregs
have an important role in immune evasion in cancer cells (14,15).
Studies have confirmed that an increased number of intratumoral or
peritumoral Tregs has a negative impact on the prognosis of breast
cancer depending on the localization in the tumor microenvironment
(16–18). Due to their opposing actions in tumor
immunity and established use for breast cancer prognosis, a
combined assessment of CD8+ T lymphocytes and
infiltration of Tregs may be used to assess the impact of the
immune microenvironment on the dissemination of CTCs in breast
cancer (19–21).
The present study was conducted to assess the
association between the number of tumor infiltrating
CD8+ T lymphocytes/Tregs and the presence of CTCs in the
peripheral blood. The TILs analyzed in the present study include
the intratumoral and peritumoral cell types. A multi-marker
quantitative polymerase chain reaction (qPCR) platform was
established by using a combination of three widely used mRNA
markers: Cytokeratin 19 (CK19), human mammaglobin (hMAM) and small
breast epithelial mucin (SBEM) (21,22). In
addition, the infiltrating CD8+ lymphocytes and Tregs
were detected using antibodies against CD8 and Foxp3 by
immunohistochemistry (IHC). Then, the association between the
prevalence of CTCs and intratumoral/peritumoral Tregs or
CD8+ T lymphocytes was analyzed.
Materials and methods
Patients
Between May 2015 and January 2017, 167 patients with
invasive breast cancer, who were treated at the Department of
Thyroid and Breast Surgery of The Affiliated Hospital of Nantong
University (Nantong, China), were enrolled in the present study.
The median age of the patients was 50 years (range, 26–84 years).
The clinicopathological parameters evaluated for each patient
included age, menstrual status, tumor size, tumor-node-metastasis
(TNM) stage, histological grade, estrogen receptor (ER) and
progesterone receptor (PR) status and human epidermal growth factor
receptor 2 (HER2) status (Table I).
For each patient, a detailed past medical history was recorded to
exclude liver and kidney dysfunction, autoimmune disease, bone
marrow disease and chronic infection. All tissue and blood samples
were collected prior to chemotherapy, radiotherapy, endocrine
therapy or any other treatment that could affect the immune state.
A complete diagnostic evaluation, including history, physical
examination, ultrasound, chest computed tomography (CT), abdominal
CT, bone scan and tumor marker tests, was performed to exclude
distant metastasis.
 | Table I.Association between the CTC-positive
rate in the peripheral blood of patients with breast cancer and
clinicopathological parameters. |
Table I.
Association between the CTC-positive
rate in the peripheral blood of patients with breast cancer and
clinicopathological parameters.
| Clinicopathological
parameters | Total, n=167 | CTC-positive rate
(%), n=92 | CTC-negative rate
(%), n=75 | P-value |
|---|
| Age, years |
|
|
| 0.530 |
|
≤45 | 45 | 23 (51) | 22 (49) |
|
|
>45 | 122 | 69 (57) | 53 (43) |
|
| Menopausal
status |
|
|
| 0.084 |
|
Premenopausal | 68 | 32 (47) | 36 (53) |
|
|
Postmenopausal | 99 | 60 (61) | 39 (39) |
|
| Tumor
sizea |
|
|
| 0.012 |
| T1 | 65 | 27 (42) | 38 (58) |
|
| T2 | 98 | 62 (63) | 36 (37) |
|
| T3 | 4 | 3 (75) | 1 (25) |
|
| Lymph node
stagea |
|
|
| 0.120 |
|
pN0 | 102 | 52 (51) | 50 (49) |
|
|
pN1 | 34 | 20 (59) | 14 (41) |
|
|
pN2 | 15 | 7 (47) | 8 (53) |
|
|
pN3 | 16 | 13 (81) | 3 (19) |
|
| Disease
stagea |
|
|
| 0.095 |
| I | 43 | 18 (42) | 25 (58) |
|
| II | 92 | 53 (58) | 39 (42) |
|
|
III | 32 | 21 (66) | 11 (34) |
|
| Histological
grade |
|
|
| 0.494 |
| 1 | 12 | 6 (50) | 6 (50) |
|
| 2 | 98 | 51 (52) | 47 (48) |
|
| 3 | 57 | 35 (61) | 22 (39) |
|
| ER/PR
statusb |
|
|
| 0.600 |
|
Negative | 50 | 26 (52) | 24 (48) |
|
|
Positive | 117 | 66 (56) | 51 (44) |
|
| HER2
statusc |
|
|
| 0.143 |
|
Negative | 127 | 65 (51) | 62 (49) |
|
|
Positive | 40 | 27 (67) | 13 (33) |
|
To define the baseline expression and positive
threshold of the three markers (CK19, hMAM and SBEM), peripheral
blood samples were also collected from control subjects. A total of
30 healthy female volunteers (aged 23–85 years; median, 44 years)
and 60 patients with pathologically diagnosed benign breast disease
(aged 23–72 years; median, 38 years) were enrolled between May 2015
and January 2017. The present study was approved by the Ethics
Committee of Nantong University (Nantong, China) and The Affiliated
Hospital of Nantong University (Nantong, China). All donors and
patients provided written informed consent.
Blood processing
Following shedding of the first 2 ml of peripheral
blood to reduce contamination by epithelial cells from the skin, 10
ml peripheral blood was collected in an EDTA-treated vacuum tube
from each patient or control subject. Peripheral blood mononuclear
cells (PBMCs) were isolated from the blood by Ficoll density
gradient centrifugation (Ficoll-Paque Plus; TBDscience, Tianjin,
China) using standard procedures and frozen at −80°C until RNA
extraction.
Reverse transcription-qPCR
Total RNA was isolated from PBMCs of patients with
invasive breast cancer control subjects and 4 breast cancer tissue
specimens. These were were selected as breast cancer tissues have
been proven to express the genes CK19, hMAM and SBEM, it was chosen
to verify the stability of the multi-maker RT-PCR system, and
served as a positive control. Total RNA was isolated using TRIzol
(Thermo Fisher Scientific, Inc., Waltham, MA, USA) according to the
manufacturer's protocol. The purity and quantification of RNA were
assessed by measuring the optical density at 260 and 280 nm. The
RNA quality was also verified by electrophoresis in a 1.5%
non-denaturing agarose gel. The RNA integrity was assessed by qPCR
amplification of the housekeeping gene, β-actin. Reverse
transcription of the RNA was performed using the Prime-Script RT
Master Mix system (Takara Biotechnology Co., Ltd.). cDNA was
synthesized from 1.5 mg total RNA that was isolated from PBMCs in a
total volume of 30 µl according to the manufacturer's protocol.
The primers for CK19, SBEM, hMAM and β-actin were
designed using the software Primer version 5.0 (PREMIER, Palo Alto,
CA, USA). All primers were synthesized by Invitrogen (Table II) (Invitrogen; Thermo Fisher
Scientific, Inc.). All PCR reactions were performed using the ABI
StepOnePlus real-time PCR system (Applied Biosystems, Thermo Fisher
Scientific, Inc.) and fluorescent SYBR-Green I. qPCR was performed
using the SYBR Premix Ex Taq (Takara Biotechnology Co., Ltd.)
according to the protocol in a final volume of 20 µl containing 10
µl 2× SYBR Premix Ex Taq, 0.4 µl PCR forward primer (10 µM), 0.4 µl
PCR reverse primer (10 µM), 0.4 µl 50× ROX reference dye, 2 µl cDNA
template and 6.8 µl dH2O. The thermocycling conditions
consisted of 30 sec of predenaturation at 95°C and 40 cycles of PCR
(denaturation at 95°C for 5 sec, annealing at 60°C for 30 sec and
extension at 72°C for 30 sec).
 | Table II.Prime sequences. |
Table II.
Prime sequences.
| Gene | Sequence
(5′-3′) |
|---|
| CK19 |
|
|
Sense |
TCCGAACCAAGTTTGAGACG |
|
Antisense |
CCCTCAGCGTACTGATTTCCT |
| hMAM |
|
|
Sense |
AGAACTGCAGGGTATGGTGAGAA |
|
Antisense |
ACATGTATAGCAGGTTTCAACAATTGT |
| SBEM |
|
|
Sense |
GATCTTCAGGTCACCACCATG |
|
Antisense |
GGGACACACTCTACCATTCG |
| β-actin |
|
|
Sense |
GCTGTGCTATCCCTGTACGC |
|
Antisense |
TGCCTCAGGGCAGCGGAACC |
The relative expression of the marker genes was
normalized to β-actin expression and calculated using the formula:
2−ΔΔCq (23). The relative
gene expression value for the marker genes (CK19, hMAM and SBEM),
in the peripheral blood of a healthy volunteer was set to 1.
qPCR positivity was defined as gene expression
beyond the cut-off threshold, which was set for each gene marker at
three standard deviations from the mean expression in the control
subjects (24). Positivity of the
multi-marker method was defined as positivity for at least one of
the markers.
IHC staining and quantification of CD8
and Foxp3
Formalin-fixed (concentration 10%, room temperature,
fixed for 24 h) paraffin sections (4 µm) of the tumor tissues were
subjected to IHC staining. Briefly, the sections were
deparaffinized and rehydrated in graded alcohol. Antigen retrieval
was performed at 121°C for 2 min in citrate buffer (pH 6.0). After
serial blocking with hydrogen peroxide and normal goat serum
(Luoshen Biotechnologies, Inc., Shanghai, China, http://eastdiagno.bioon.com.cn/index_93476.html) at
room temperature for 10 min, the sections were incubated with a
primary monoclonal antibody against CD8 (catalog no, MA5-13473;
clone C8/144B; dilution, 1:40; Thermo Fisher Scientific, Inc.) or
Foxp3 (catalog no, ab20034; clone 236A/E7; dilution, 1:100; Abcam,
Cambridge, UK) overnight at 4°C. Labeling was detected using the
PV-6000 Polymer Detection system (OriGene Technologies, Inc.,
Beijing, China). Sections were counterstained with hematoxylin at
room temperature for 3 min. Positive staining controls were
performed in parallel with tonsil sections provided by patients in
otolaryngology between October 2016 and January 2017, including 2
males and 3 females. A negative staining control was performed by
omitting the use of the primary antibody.
The CD8+ T lymphocytes and
Foxp3+ Tregs were quantified independently by two
trained investigators, who were blinded to the clinical data and
positivity of peripheral CTCs. A total of 5 intratumoral and 5
peritumoral areas were selected and imaged using an ×10 objective
lens of a light microscope (Nikon 50i and Nikon DS-U3; Nikon
Corporation, Tokyo, Japan). The images were obtained using an ×40
objective lens for cell counting. Due to the extensive
heterogeneity in peritumoral infiltrating CD8+ T
lymphocytes and Foxp3+ Tregs, a modified grading system
for semi-quantitative scoring was used. In this system, G0
corresponded to the absence of lymphocytes. G1 corresponded to the
mean number of CD8+ T lymphocytes ≤50 and
Foxp3+ Tregs ≤25. G2 corresponded to the mean number of
CD8+ T lymphocytes >50 and ≤100 and Foxp3+
Tregs >25 and ≤50. G3 corresponded to the mean number of
CD8+ T lymphocytes >100 and Foxp3+ Tregs
>50.
Statistical analysis
The associations between variables were evaluated by
Pearson's χ2 test or Fisher's exact test if required. A
univariate analysis was used to test if there are associations
between CTC-positive rate and the number of Tregs, CD8+
T lymphocytes and clinicopathological parameters. A multivariate
logistic regression model was also performed to analyze the
independent factors associated with the CTC-positive rate.
Statistical analysis was performed using SPSS 18.0 software (SPSS,
Inc., Chicago, IL, USA). In all analyses, a two-sided P<0.05 was
considered statistically significant.
Results
Multi-marker qPCR analysis of CTCs in
patients with breast cancer
The marker gene expression baseline was precisely
quantified in 90 control subjects by qPCR. The median relative gene
expression values for CK19, hMAM and SBEM in the control subjects
were 1.18, 1.92 and 1.29, respectively. The cut-off threshold for
marker gene positivity, that is, abnormal expression, was set at
three standard deviations from the mean 2−ΔΔCq value for
each gene. The cut-off thresholds for CK19, hMAM and SBEM were
4.92, 7.71 and 6.38, respectively. Of 167 patients, 62 (37%) were
positive for CK19, 37 (22%) were positive for hMAM, and 40 (24%)
were positive for SBEM (Table III).
In total, 92 (55%) patients were positive for at least one marker.
The sensitivities for the individual markers CK19, hMAM, and SBEM
were 37, 22 and 24%, respectively, and the specificities were 100,
99 and 99%, respectively. The multi-marker qPCR platform yielded a
sensitivity of 55% and a specificity of 98% (Table III).
 | Table III.CTC-positive rate in controls and
patients with breast cancer. |
Table III.
CTC-positive rate in controls and
patients with breast cancer.
|
|
| CTC-positive rate
of individual marker genes (%) |
|---|
|
|
|
|
|---|
| Groups | CTC-positive rate
of three marker genes (%) | CK19 | hMAM | SBEM |
|---|
| Control (n=90) | 2/90 (2.2) | 0/90 (0.0) | 1/90 (1.1) | 1/90 (1.1) |
| Breast cancer
(n=167) | 92/167 (55) | 62/167 (37) | 37/167 (22) | 40/167 (24) |
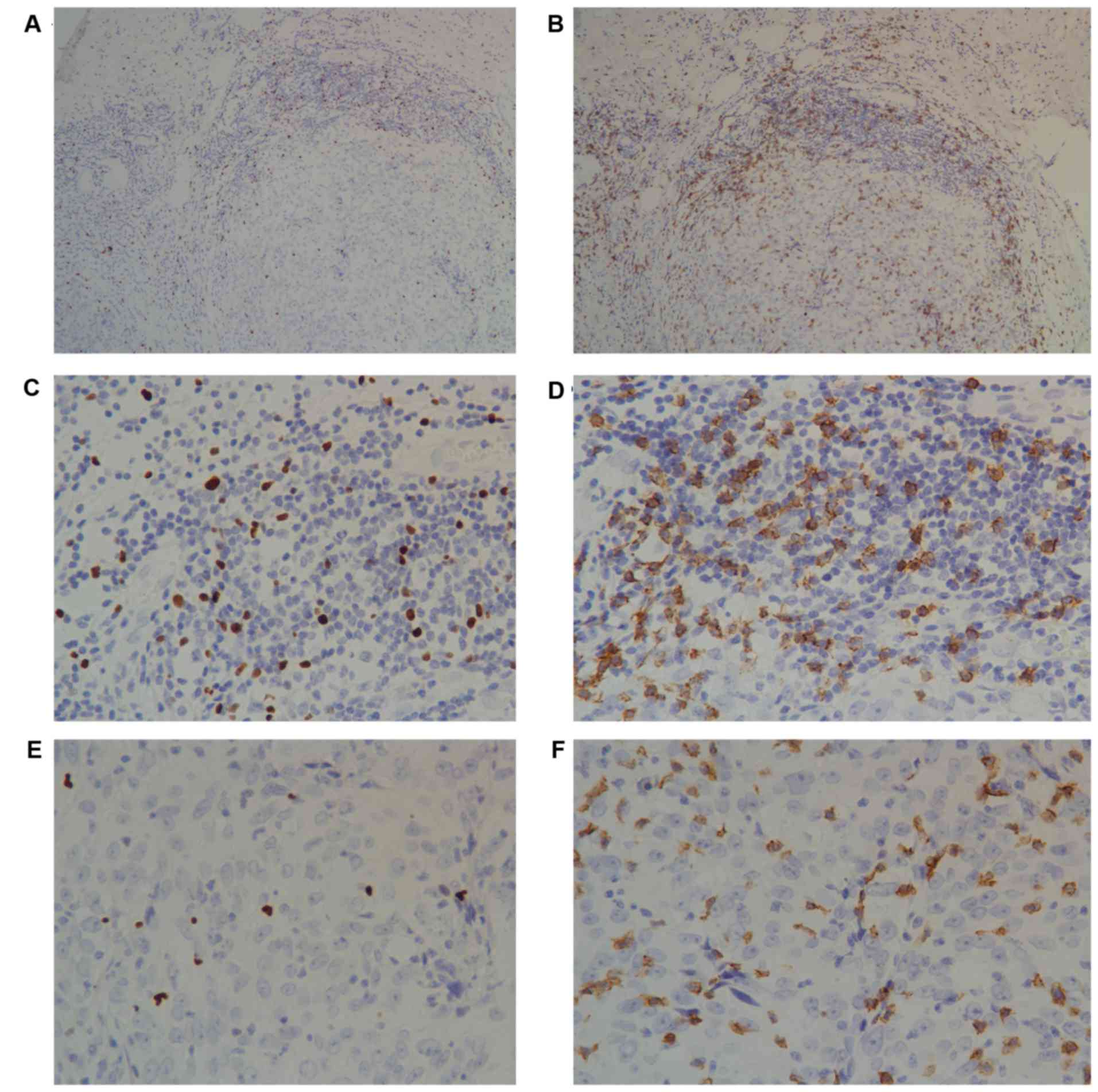
Detection of CD8+ T
lymphocytes and Foxp3+ Tregs in the tumor
microenvironment of breast cancer
Infiltrating intratumoral CD8+ T
lymphocytes and Foxp3+ Tregs presented with a diffuse
pattern, and the peritumoral infiltration was more abundant and
tended to form lymphoid aggregates (Fig.
1). There were significantly more CD8+ T lymphocytes
(median, 79.03 vs. 25.00; range, 0–254.11 vs. 0–138.67) and
Foxp3+ Tregs (median, 34.12 vs. 10.33; range 0–188.03
vs. 0–85.67) in the peritumoral than the intratumoral areas (data
not shown).
Association between CTC-positive rate
and the clinicopathological parameters of patients with breast
cancer
The peripheral CTC-positive rate was statistically
significant between the different tumor sizes (P<0.05) and was
associated with a larger tumor size (T1, 42%; T2, 63%; T3, 75%)
(Table I). The peripheral
CTC-positive rate was also weakly associated with a higher disease
stage and histological grade, although this association did not
reach significance (P>0.05). Associations between CTC-positive
rate and the remaining clinicopathological parameters were not
observed (P>0.05; Table I).
Association of CTC-positive rates with
Foxp3 T cells but not with CD8+T cells in the tumor
microenvironment
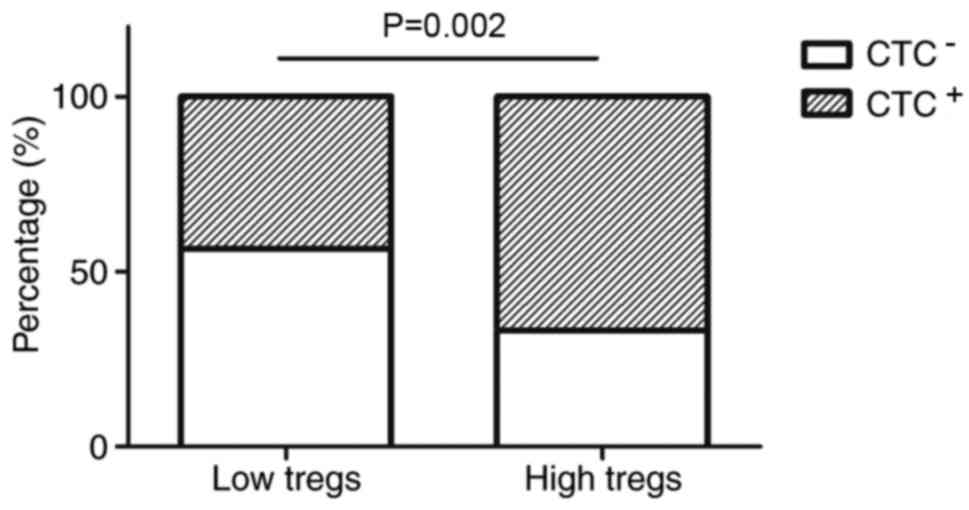
It was determined that increased numbers of
intratumoral Tregs are associated with the CTC-positive rate in
patients with breast cancer (Table
IV). Patients with an increased number of intratumoral Tregs
exhibited higher CTC-positive rates compared with those with a
decreased number of Tregs (67 vs. 43%, P=0.002; Fig. 2). The same trend was observed for
peritumoral infiltrating Tregs (G0, 48%; G1, 42%; G2, 57%; G3, 73%,
P=0.045) (Table IV). Detection of
peripheral CTCs was weakly and inversely associated with the number
of infiltrating peritumoral CD8+ lymphocytes, although
this association did not reach statistical significance (P=0.47;
Table IV).
 | Table IV.Association between the CTC-positive
rate in the peripheral blood of patients with breast cancer and
tumor-infiltrating CD8+ T lymphocytes and
Foxp3+ Tregs in the tumor microenvironment. |
Table IV.
Association between the CTC-positive
rate in the peripheral blood of patients with breast cancer and
tumor-infiltrating CD8+ T lymphocytes and
Foxp3+ Tregs in the tumor microenvironment.
| Infiltration of
lymphocytes | CTC-positive rate
(%) | CTC-negative rate
(%) | P-value |
|---|
| Intratumoral
Foxp3+ Tregsa |
|
| 0.002 |
|
Low | 36 (43) | 47 (57) |
|
|
High | 56 (67) | 28 (33) |
|
| Intratumoral
CD8+ T lymphocytesa |
|
| 0.846 |
|
Low | 44 (54) | 37 (46) |
|
|
High | 48 (56) | 38 (44) |
|
| Peripheral
Foxp3+ Tregsb |
|
| 0.045 |
| G0 | 24 (48) | 26 (52) |
|
| G1 | 14 (42) | 19 (58) |
|
| G2 | 27 (57) | 20 (43) |
|
| G3 | 27 (73) | 10 (27) |
|
| Peripheral
CD8+ T lymphocytesb |
|
| 0.470 |
| G0 | 17 (65) | 9 (35) |
|
| G1 | 22 (59) | 15 (41) |
|
| G2 | 23 (55) | 19 (45) |
|
| G3 | 30 (48) | 32 (52) |
|
Multivariate analysis indicated that the prevalence
of CTCs was independently associated with tumor size (OR=2.18, 95%
CI, 1.02–4.64; P=0.044) and infiltrating intratumoral Tregs
(OR=2.23, 95% CI, 1.02–4.87; P=0.044) (Table V).
 | Table V.Multivariate analysis of the
association between circulating tumor cells in the peripheral blood
of breast cancer patients and clinicopathological parameters as
well as Foxp3+ Tregsa. |
Table V.
Multivariate analysis of the
association between circulating tumor cells in the peripheral blood
of breast cancer patients and clinicopathological parameters as
well as Foxp3+ Tregsa.
| Variables | OR | 95% CI | P-value |
|---|
| Menopausal
status | 0.49 | 0.25–0.98 | 0.052 |
| Tumor size | 2.18 | 1.02–4.64 | 0.044 |
| TNM stage | 1.17 | 0.64–2.14 | 0.608 |
| Intratumoral
Tregs | 2.23 | 1.02–4.87 | 0.044 |
| Peritumoral
Tregs | 1.16 | 0.83–1.60 | 0.369 |
Discussion
The association between CTCs and the immune system
in breast cancer was reported (25,26). The
effect of TILs on the prevalence of CTCs in patients with breast
cancer is poorly understood. In the present study, it was
demonstrated that the number and distribution of tumor-infiltrating
Tregs were significantly associated with the presence of peripheral
CTCs in patients with breast cancer.
CTCs can be identified and characterized in the
peripheral blood of patients with breast cancer (27) and may represent the emergence of early
hematological metastasis in breast cancer. CTCs have the ability to
form clusters of microscopic tumors, and their detection,
persistence or elevation is associated with poor prognosis
(2). Therefore, it is essential to
elucidate the factors that affect the dissemination of CTCs, which
would provide a theoretical basis for improving breast cancer
treatment. Immune cells, cytokines and other factors in the
microenvironment are present throughout tumor development and have
an impact on tumor progression (28);
therefore, the effects of immune factors on disease progression may
be partially mediated by the suppression of hematological
micrometastasis in breast cancer.
Due to the heterogeneity of tumor cells and the
instability of gene expression, there is no identified and specific
standard for CTCs detection to date (29). Our center has established a
multi-marker (CK19, hMAM, SBEM) qPCR platform for detection of CTCs
in the peripheral blood of patients with breast cancer. The
sensitivity and specificity of this method have been confirmed in
several laboratories (30,31). CK19, hMAM and SBEM mRNA were detected
in 37, 22 and 24% of the patients with breast cancer, respectively.
When using the multi-marker platform (for which positivity was
defined as positivity for at least one of the markers), the
sensitivity was improved to 55%, which was greater compared with
the values reported in similar studies (31,32). In
addition, the specificity of the multi-marker platform was 98% due
to contamination of only minor samples. Therefore, the multi-marker
qPCR platform provides high sensitivity and specificity for the
detection of CTCs.
TILs exert an important role in tumor immunity.
Tregs were initially characterized as CD4+
CD25+ cells and are thought to be the main obstacles
that hinder the efficacy of antitumor immunity and immunotherapy
(30,33). Tregs effectively suppress the
proliferation and activation of CD8+ T lymphocytes in a
contact-dependent manner or via the release of cytokines (33). The impact of Tregs on the prognosis of
breast cancer depends on their distribution and the expression of
hormone receptors (34). The majority
of studies have reported that an elevated number of
intratumoral/peritumoral Tregs confers a poor clinical outcome
(16–19) and is associated with disease
progression in breast cancer (34).
However, West et al (35)
concluded that Tregs exhibit an antitumor activity as it may favor
the survival time of patients with ER-negative breast cancer.
Therefore, the present study investigated the association between
the number of intratumoral/peritumoral Tregs and the presence of
peripheral CTCs. Univariate analysis demonstrated that patients
with an increased number of intratumoral/peritumoral Tregs
exhibited a higher CTC-positive rate compared with those with a
lower number of Tregs. Therefore, increasing the number of
intratumoral/peritumoral Tregs may increase local immunosuppressive
capabilities and reduced anti-tumor immunity, consequently forming
an immunosuppressive microenvironment conducive to tumor growth,
invasion and metastasis.
A local antitumor immunity deficiency may indicate a
depressed systemic immune system (36,37). A
depressed immunity in the tumor microenvironment may inefficiently
stimulate tumor-antigen presentation or the immune response, which
would enable breast cancer cells to escape from local or systemic
immune surveillance and potentially form distant metastases
(34). Previous studies regarding the
prognostic value of Tregs in breast cancer were consistent with the
results of the present study (16–19). In
addition, the multivariate analysis in the present study
demonstrated that an increasing number of intratumoral Tregs but
not peritumoral Tregs was an independent risk factor for detection
of CTCs. The prognosis data from Liu et al (19) supported the present findings that an
increased number of intratumoral Tregs but not peritumoral Tregs
was associated with a poorer clinical outcome (16,19).
However, the present results were different from those reported by
Mahmoud et al (17). One
explanation for these contradictory results may be the tissue
volume used (19). The tissue array
used by Gobert et al (18)
contained only a small volume of tumor tissue. The use of such
small tissue fragments may not be optimal to obtain a sufficient
number of cells for a reliable count of Tregs in different areas.
In the present study full block tissue sections were used to enable
the selection of areas with abundant intratumoral/peritumoral
Tregs.
Rich infiltration by CD8+ T lymphocytes,
which are a representative subset of lymphocytes that are
associated with immune surveillance in the tumor microenvironment,
may indicate strong anti-tumor immunity (37). The results of the present study
revealed that an elevated grade for peritumoral CD8+ T
lymphocytes was inversely associated with the detection of
peripheral CTCs, although this association did not reach
statistical significance. The hypothesis that CD8+ T
lymphocytes suppress the dissemination of CTCs was not confirmed in
the present study. This may be due to the following factors. First,
either by a hematological or lymphangial route, breast cancer cells
may invade the circulatory system and cause distant metastases. In
the present study, the function of local immune suppression was
examined in hematological micrometastasis rather than via the
lymphangial route. In a study on human colorectal carcinoma, Chiba
et al (38) observed that the
effects of CD8+ T lymphocytes may be mediated by the
suppression of lymphangial micrometastasis rather than growth
suppression in the primary tumor. Secondly, the effect of
CD8+ T lymphocytes on tumor progression depends not only
on their number and distribution but also on their activity
(3,39). Cytotoxic CD8+ T cells,
which are merely active CD8+ T lymphocytes, may exert
anti-tumor immunity. Although a significant association between
tumor-infiltrating CD8+ T lymphocytes and the detection
of peripheral CTCs was not observed, the possibility of this
association cannot be ignored. Accumulating studies indicate that
CD8+ T lymphocytes have antitumor activity, as they may
favor the survival time of patients with breast cancer (9) Therefore, it is possible that
CD8+ T lymphocytes may contribute to patient survival
time via other mechanisms, and thus further research is
required.
In conclusion, the results of the present study
indicated that the role of Tregs in the progression of breast
cancer may be mediated by the suppression of dissemination of CTCs,
and the effect is mainly determined by intratumoral Tregs.
Nevertheless, the impact of the phenotypic and functional qualities
of Tregs or CD8+ T lymphocytes on hematological
micrometastasis in breast cancer was not assessed comprehensively.
Prospective studies are required to understand better the molecular
mechanisms by which TILs affect the prevalence of CTCs and their
potential role in breast cancer immunotherapy.
Acknowledgements
Not applicable.
Funding
The research was supported by The Nantong
demonstration project for the people's livelihood (grant no.
MS32015029).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Author's contributions
DX analyzed the data and was a major contributor in
writing the manuscript. TX made substantial contribution in
analysis and interpretation of the data. JW performed
immunohistochemistry and cell counting. MC collected the
information regarding the subjects enrolled in the present study
and detected CTCs. SW had major role in designing the study. CZ
designed the study and gave the final approval of the version to be
published. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Nantong University (Nantong, China) and The Affiliated
Hospital of Nantong University (Nantong, China). All donors and
patients gave informed consent.
Patient consent for publication
Informed consent was obtained from all patients
included in this study for publication of the associated data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hunter KW, Crawford NP and Alsarraj J:
Mechanisms of metastasis. Breast Cancer Res. 10 Suppl 1:S22008.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhang L, Riethdorf S, Wu G, Wang T, Yang
K, Peng G, Liu J and Pantel K: Meta-analysis of the prognostic
value of circulating tumor cells in breast cancer. Clin Cancer Res.
18:5701–5710. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Smith HA and Kang Y: The
metastasis-promoting roles of tumor-associated immune cells. J Mol
Med. 91:411–429. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wong CW, Lee A, Shientag L, Yu J, Dong Y,
Kao G, Al-Mehdi AB, Bernhard EJ and Muschel RJ: Apoptosis: An early
event in metastatic inefficiency. Cancer Res. 61:333–338.
2001.PubMed/NCBI
|
|
5
|
Baccelli I, Schneeweiss A, Riethdorf S,
Stenzinger A, Schillert A, Vogel V, Klein C, Saini M, Bäuerle T,
Wallwiener M, et al: Identification of a population of blood
circulating tumor cells from breast cancer patients that initiates
metastasis in a xenograft assay. Nat Biotechnol. 31:539–544. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Santos MF, Mannam VK, Craft BS, Puneky LV,
Sheehan NT, Lewis RE and Cruse JM: Comparative analysis of innate
immune system function in metastatic breast, colorectal, and
prostate cancer patients with circulating tumor cells. Exp Mol
Pathol. 96:367–374. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Noman MZ, Messai Y, Muret J, Hasmim M and
Chouaib S: Crosstalk between CTC, immune system and hypoxic tumor
microenvironment. Cancer Microenviron. 7:153–160. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim ST, Jeong H, Woo OH, Seo JH, Kim A,
Lee ES, Shin SW, Kim YH, Kim JS and Park KH: Tumor-infiltrating
lymphocytes, tumor characteristics, and recurrence in patients with
early breast cancer. Am J Clin Oncol. 36:224–231. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Al-Saleh K, Abd El-Aziz N, Ali A, Abozeed
W, Abd El-Warith A, Ibraheem A, Ansari J, Al-Rikabi A, Husain S and
Nabholtz JM: Predictive and prognostic significance of
CD8+ tumor-infiltrating lymphocytes in patients with
luminal B/HER 2 negative breast cancer treated with neoadjuvant
chemotherapy. Oncol Lett. 14:337–344. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mahmoud SM, Paish EC, Powe DG, Macmillan
RD, Grainge MJ, Lee AH, Ellis IO and Green AR: Tumor-infiltrating
CD8+ lymphocytes predict clinical outcome in breast cancer. J Clin
Oncol. 29:1949–1955. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pagès F, Kirilovsky A, Mlecnik B, Asslaber
M, Tosolini M, Bindea G, Lagorce C, Wind P, Marliot F, Bruneval P,
et al: In situ cytotoxic and memory T cells predict outcome in
patients with early-stage colorectal cancer. J Clin Oncol.
27:5944–5951. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dunn GP, Bruce AT, Ikeda H, Old LJ and
Schreiber RD: Cancer immunoediting: From immunosurveillance to
tumor escape. Nat Immunol. 3:991–998. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tang J, Yang Z, Wang Z, Li Z, Li H, Yin J,
Deng M, Zhu W and Zeng C: Foxp3 is correlated with VEGF-C
expression and lymphangiogenesis in cervical cancer. World J Surg
Oncol. 15:1732017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Linehan DC and Goedegebuure PS: CD25+CD4+
regulatory T-cells in cancer. Immunol Res. 32:155–168. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ménétrier-Caux C, Gobert M and Caux C:
Differences in tumor regulatory T-cell localization and activation
status impact patient outcome. Cancer Res. 69:7895–7898. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bates GJ, Fox SB, Han C, Leek RD, Garcia
JF, Harris AL and Banham AH: Quantification of regulatory T cells
enables the identification of high-risk breast cancer patients and
those at risk of late relapse. J Clin Oncol. 24:5373–5380. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mahmoud SM, Paish EC, Powe DG, Macmillan
RD, Lee AH, Ellis IO and Green AR: An evaluation of the clinical
significance of FOXP3+ infiltrating cells in human breast cancer.
Breast Cancer Res Treat. 127:99–108. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gobert M, Treilleux I, Bendriss-Vermare N,
Bachelot T, Goddard-Leon S, Arfi V, Biota C, Doffin AC, Durand I,
Olive D, et al: Regulatory T cells recruited through CCL22/CCR4 are
selectively activated in lymphoid infiltrates surrounding primary
breast tumors and lead to an adverse clinical outcome. Cancer Res.
69:2000–2009. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Liu F, Lang R, Zhao J, Zhang X, Pringle
GA, Fan Y, Yin D, Gu F, Yao Z and Fu L: CD8+ cytotoxic T
cell and FOXP3+ regulatory T cell infiltration in
relation to breast cancer survival and molecular subtypes. Breast
Cancer Res Treat. 130:645–655. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang ZK, Yang B, Liu H, Hu Y, Yang JL, Wu
LL, Zhou ZH and Jiao SC: Regulatory T cells increase in breast
cancer and in stage IV breast cancer. Cancer Immunol Immunother.
61:911–916. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Andergassen U, Kölbl AC, Mahner S and
Jeschke U: Real-time RT-PCR systems for CTC detection from blood
samples of breast cancer and gynaecological tumour patients
(Review). Oncol Rep. 35:1905–1915. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chong MH, Zhao Y, Wang J, Zha XM, Liu XA,
Ling LJ, Du Q and Wang S: The dynamic change of circulating tumour
cells in patients with operable breast cancer before and after
chemotherapy based on a multimarker QPCR platform. Br J Cancer.
106:1605–1610. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2−ΔΔCT method. Methods. 25:402–408. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mikhitarian K, Martin RH, Ruppel MB,
Gillanders WE, Hoda R, del Schutte H, Callahan K, Mitas M and Cole
DJ: Detection of mammaglobin mRNA in peripheral blood is associated
with high grade breast cancer: Interim results of a prospective
cohort study. BMC Cancer. 8:552008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mego M, Gao H, Cohen EN, Anfossi S,
Giordano A, Tin S, Fouad TM, De Giorgi U, Giuliano M, Woodward WA,
et al: Circulating tumor cells (CTCs) are associated with
abnormalities in peripheral blood dendritic cells in patients with
inflammatory breast cancer. Oncotarget. 8:35656–35668. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mego M, Gao H, Cohen EN, Anfossi S,
Giordano A, Sanda T, Fouad TM, De Giorgi U, Giuliano M, Woodward
WA, et al: Circulating tumor cells (CTC) are associated with
defects in adaptive immunity in patients with inflammatory breast
cancer. J Cancer. 7:1095–1104. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Benoy IH, Elst H, Philips M, Wuyts H, Van
Dam P, Scharpé S, Van Marck E, Vermeulen PB and Dirix LY: Real-time
RT-PCR detection of disseminated tumour cells in bone marrow has
superior prognostic significance in comparison with circulating
tumour cells in patients with breast cancer. Br J Cancer.
94:672–680. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zamarron BF and Chen W: Dual roles of
immune cells and their factors in cancer development and
progression. Int J Biol Sci. 7:651–658. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kallergi G, Politaki E, Alkahtani S,
Stournaras C and Georgoulias V: Evaluation of isolation methods for
circulating tumor cells (CTCs). Cell Physiol Biochem. 40:411–419.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Curiel TJ: Tregs and rethinking cancer
immunotherapy. J Clin Invest. 117:1167–1174. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Krishnamurthy S, Cristofanilli M, Singh B,
Reuben J, Gao H, Cohen EN, Andreopoulou E, Hall CS, Lodhi A,
Jackson S, et al: Detection of minimal residual disease in blood
and bone marrow in early stage breast cancer. Cancer.
116:3330–3337. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chen Y, Zou TN, Wu ZP, Zhou YC, Gu YL, Liu
X, Jin CG and Wang XC: Detection of cytokeratin 19, human
mammaglobin, and carcinoembryonic antigen-positive circulating
tumor cells by three-marker reverse transcription-PCR assay and its
relation to clinical outcome in early breast cancer. Int J Biol
Markers. 25:59–68. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zou W: Regulatory T cells, tumour immunity
and immunotherapy. Nat Rev Immunol. 6:295–307. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Liu S, Foulkes WD, Leung S, Gao D, Lau S,
Kos Z and Nielsen TO: Prognostic significance of FOXP3+
tumor-infiltrating lymphocytes in breast cancer depends on estrogen
receptor and human epidermal growth factor receptor-2 expression
status and concurrent cytotoxic T-cell infiltration. Breast Cancer
Res. 16:4322014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
West NR, Kost SE, Martin SD, Milne K,
Deleeuw RJ, Nelson BH and Watson PH: Tumour-infiltrating FOXP3+
lymphocytes are associated with cytotoxic immune responses and good
clinical outcome in oestrogen receptor-negative breast cancer. Br J
Cancer. 108:155–162. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Liyanage UK, Moore TT, Joo HG, Tanaka Y,
Herrmann V, Doherty G, Drebin JA, Strasberg SM, Eberlein TJ,
Goedegebuure PS, et al: Prevalence of regulatory T cells is
increased in peripheral blood and tumor microenvironment of
patients with pancreas or breast adenocarcinoma. J Immunol.
169:2756–2761. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Li CH, Kuo WH, Chang WC, Huang SC, Chang
KJ and Sheu BC: Activation of regulatory T cells instigates
functional down-regulation of cytotoxic T lymphocytes in human
breast cancer. Immunol Res. 51:71–79. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Chiba T, Ohtani H, Mizoi T, Naito Y, Sato
E, Nagura H, Ohuchi A, Ohuchi K, Shiiba K, Kurokawa Y and Satomi S:
Intraepithelial CD8+ T-cell-count becomes a prognostic factor after
a longer follow-up period in human colorectal carcinoma: Possible
association with suppression of micrometastasis. Br J Cancer.
91:1711–1717. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Campbell MJ, Scott J, Maecker HT, Park JW
and Esserman LJ: Immune dysfunction and micrometastases in women
with breast cancer. Breast Cancer Res Treat. 91:163–171. 2005.
View Article : Google Scholar : PubMed/NCBI
|