Introduction
Cervical cancer is one of the major types of
malignant tumor that has a negative impact on women's health. In
economically underdeveloped countries, cervical cancer is the
leading cause of mortality among women (1). According to an epidemiologic study, the
incidence of cervical cancer and associated mortality rates in
China have increased yearly over the last 10 years (2). In addition, due to the implementation of
cervical cancer screening, the detection of early cervical cancer
has increased; however, the recurrence rate remains at ~30%.
Post-operative recurrences are correlated to clinical stage,
surgical method and post-operative pathologic reports (3). However, the correlation between surgical
method and prognosis is weaker. In 2015, the National Comprehensive
Cancer Network (NCCN) guidelines for the clinical diagnosis and
treatment of cervical cancer updated the criteria for cervical
cancer surgery. The new guidelines recommend using the Querleu and
Morrow (QM) surgical classification system (4). In China, modified radical hysterectomy
is a common surgical procedure for cervical cancer, which is
similar to the B type of the QM classification (5). In the present study, the location of
recurrence and the route of metastasis in 86 patients with early
stage cervical cancer were retrospectively analyzed following a
type B surgical procedure. The present study aimed to retroactively
analyze the recurrent sites and patterns of spread following
radical surgery for early cervical cancer. In doing so, the
associations between recurrence and metastasis, age, time, and
postoperative pathologic changes were investigated.
Materials and methods
Clinical data
The present study was a single site retrospective
study performed between October 2009 and March 2015 involving 86
patients who were diagnosed with cervical cancer metastases and
recurrence following surgery at Henan Cancer Hospital (Henan,
China). The patient ages ranged between 31 and 79 years, with a
median age of 45 years, and all patients had complete medical
records. Of the 86 patients, 78 had squamous cell carcinoma of the
uterine cervix and 8 had adenocarcinoma. The primary treatment was
modified radical hysterectomy with bilateral pelvic lymph node
dissection. With respect to the classification criteria for
surgery, according to the 2015 NCCN clinical practice guidelines
for cervical cancer, all of the patients were classified as having
cervical cancer radical surgery type B. The post-operative
pathologic diagnosis was confirmed and all surgical margins were
negative. There was no post-operative residual tumor tissue. None
of the patients received radiotherapy prior to the recurrence
(Table I).
 | Table I.Association between metastatic site
and time and post-operative pathologic changes. |
Table I.
Association between metastatic site
and time and post-operative pathologic changes.
|
|
|
| Pelvic recurrence
site (cases) |
|---|
|
|
|
|
|
|---|
| Post-operative
pathology | Cases (n) | Median recurrence
(months) | Primary cardinal and
sacral ligament | Vagina | Paravaginal | Pelvic lymph
nodes | Only external Pelvic
metastases (cases) |
|---|
| SCC <1/2
full-thickness invasion | 10 | 24 | 4 | 4 | 1 | 1 | 0 |
| SCC ≥1/2
full-thickness invasion | 58 | 22 | 35 | 6 | 12 | 4 | 1 |
| Adenocarcinoma | 8 | 21 | 6 | – | – | 2 | 0 |
| Lymph node metastasis
and other | 10 | 8 | 3 | – | 1 | 5 | 1 |
Positron emission tomography/computed
tomography (PET/CT) (General Electric Company, New Fairfield,
Connecticut, American)
When a recurrence or metastasis was suspected in
patients with early stage cervical cancer, they underwent a
whole-body PET/CT examination. All local recurrences were
pathologically confirmed. If a distant metastasis biopsy was
difficult to obtain, further confirmation was required. In the
present study, all of the patients received at least one PET/CT
examination.
Statistical analysis
SPSS 17.0 statistical software (SPSS, Inc., Chicago,
IL, USA) was used for analyses. χ2 and Fisher's exact
probability tests were used to compare the constitute ratios.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Association between recurrence and
metastasis, age, time of recurrence and post-operative pathologic
changes
Among the sites of post-operative recurrence and
metastases, 45 simple recurrences involved the primary sacral
ligament, 10 were vaginal recurrences, 14 were paravaginal
recurrences, seven involved the pelvic lymph nodes, and five were
pelvic metastases. Metastasis to the sacral ligament and pelvic
region occurred in three patients and simple pelvic metastases
occurred in two patients (Table I).
The rate of recurrence was 79% (68/86) with a pelvic metastatic
rate of 100% (10/10), within 2 years following surgery.
In patients with negative margins, negative lymph
nodes, a cervical stromal invasion depth of <1/2 and a cervical
stromal invasion depth of >1/2, the cancer recurrence rates at
the primary sacral ligament remnant and the vagina were 40% (4/10),
10% (1/10), 40% (4/10), 60.3% (35/58), 20.7% (12/58) and 10.3%
(6/58), respectively.
With the increase in the depth of invasion, the
recurrence rate of cancer of the uterine cervix was greater than
the vaginal recurrence rate (χ2=6.24, P=0.031). The
incidence of pelvic lymph node and distant metastases was 50%
(5/10), which was higher when compared with the pelvic lymph
node-negative patients [7% (5/76); P=0.001]. The median relapse
time was 8 months, which was significantly shortened.
In patients >60 years of age, the paravaginal
recurrence rate was significantly higher, compared with that in the
<60 years of age group (χ2=19.9, P<0.01). With
increasing age, the recurrence time was prolonged (Table II). In terms of metastases, three
patients were identified with pulmonary metastases, five with
abdominal aortic lymph node metastases, one with small intestine
metastasis and one patient with greater retinal metastasis.
 | Table II.Association between metastatic site
and age. |
Table II.
Association between metastatic site
and age.
|
|
|
| Pelvic recurrence
site (cases) |
|---|
|
|
|
|
|
|---|
| Age (years) | Cases (n) | Median recurrence
(months) | Primary sacral
ligament | Vaginal and
paravaginal | Pelvic lymph
nodes | External pelvic
metastases (cases) |
|---|
| 30–40 | 16 | 14.2 | 8 | 3 | 4 | 1 |
| 41–60 | 51 | 18.1 | 35 | 8 | 7 | 1 |
| 61–70 | 19 | 21.3 | 5 | 13 | 1 | 0 |
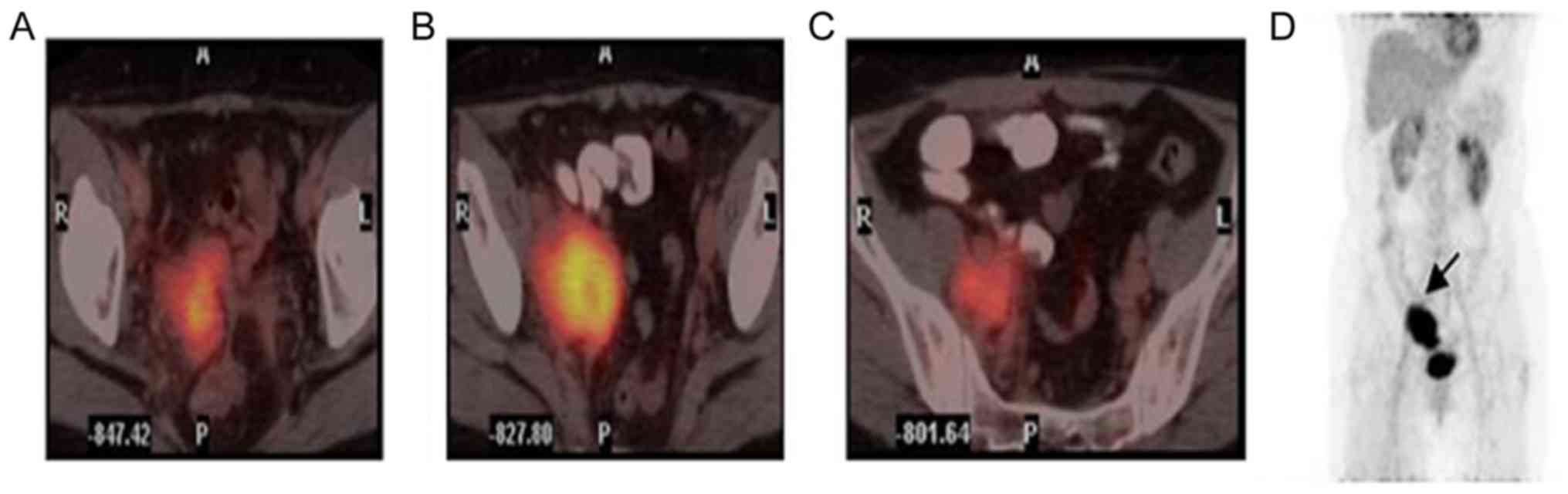
Transfer pathway
Cancer recurrence and metastasis along
the main ligament
Among the 85 patients in included the present study,
cancer spread along the cardinal ligament in 27 patients, including
19 first diagnosed with a proximal cardinal ligament stump and
eight with infiltration along the total length of the remaining
ligament all the way to the pelvic wall. Continuous images in
combination with a change in the standardized uptake value (SUV) =
showed that the cardinal ligament invasion pathways were as
follows: The earliest cancer recurrence involved the cardinal
ligament stump, followed by the internal iliac vascular axis (the
main vascular ligament) as the center, followed by a spread
outwards and upwards, close to the iliac arterial bifurcation and
terminating at the basin wall between the internal and external
iliac vessels (Fig. 1A-D).
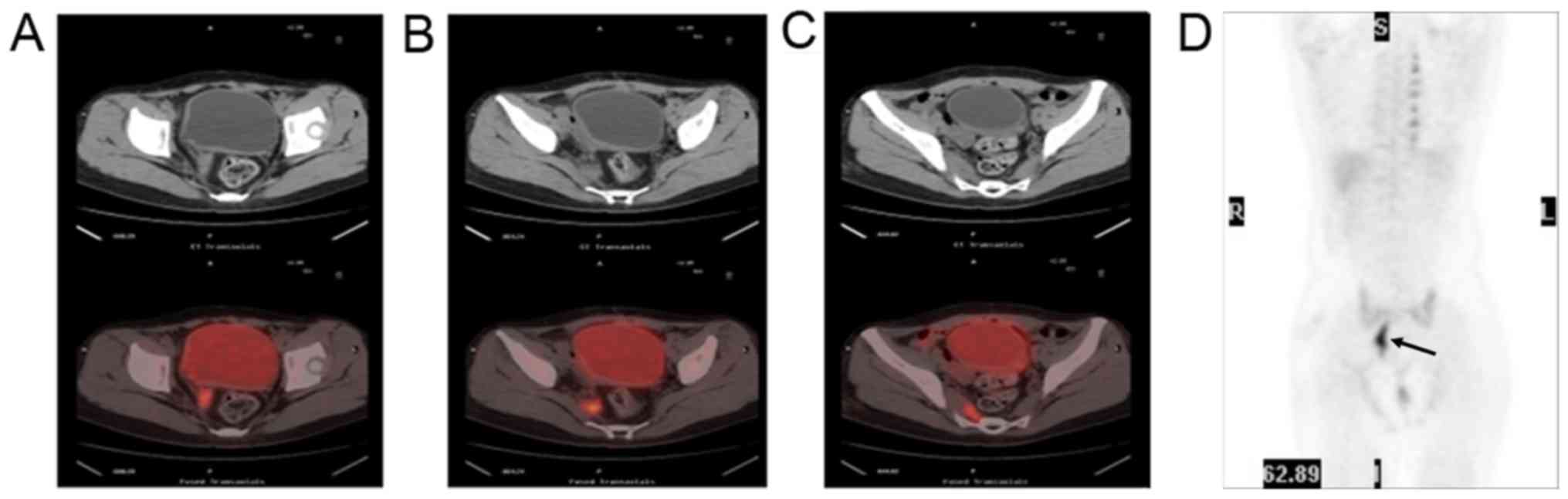
Invasion and metastatic recurrence of
cervical cancer along the uterosacral ligament
In the present study, the recurrence and metastasis
along the sacral ligament occurred in 21 patients, 18 of whom were
first diagnosed with involvement of the proximal sacral ligament
stump. Infiltration of the entire length of the residual sacral
ligament occurred in three patients, reaching the third and fourth
vertebral bodies. Continuous images in combination with changes in
the SUV showed that the invasion pathway along the uterosacral
ligament was recurrent tumor infiltration from the sacral ligament
stump. The cancer spread to the mesorectum and backward to the
second, third and fourth sacral vertebrae. If the invasion
continued to expand, the cancer invaded the mesorectum, the
piriformis muscle and the soft tissues of the pelvic wall, as shown
in Fig. 2A-D.
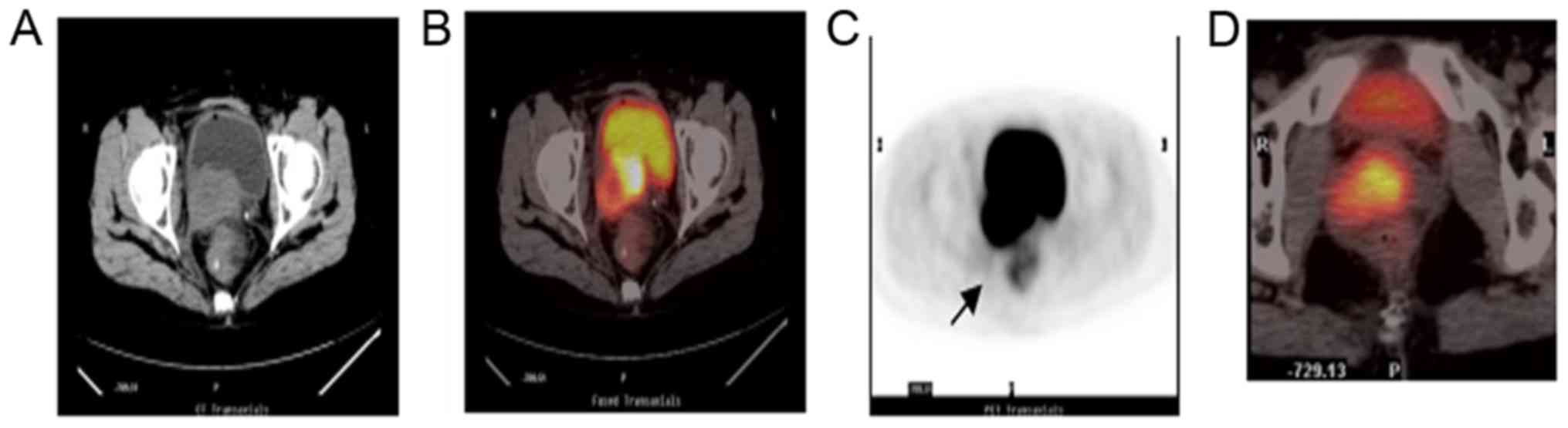
Tumor recurrences spread along the
vagina and surrounding tissue ligaments
In the present study, 11 patients had vaginal
recurrences and seven patients had an abnormal vaginal discharge.
Regular examination via Thinprep cytologic test vaginal cytology
revealed abnormalities in eight cases. Biopsies of the vaginal
mucosal surfaces showed that the tumors or vaginal abnormalities
were squamous cell carcinomas. Paravaginal recurrences were found
in 13 patients. Deep myometrial invasion was demonstrated in
post-operative pathology. If the patient had no abnormal vaginal
discharge, abnormal cytology or abnormal findings on gynecologic
examination of the vaginal mucosal, a submucosal paravaginal tissue
mass was noted and a biopsy was performed. Paravaginal tumors arose
in the fascial tissues, of which nine cases involved the cervical
vaginal ligament, which spread forwards and medially to invade the
posterior walls of the ureter and bladder, and then infiltrated
downwards to the urethra. The tumor spread laterally and
posteriorly along the same side of the rectovaginal fascia tumor,
as shown in Fig. 3A-D. In the present
study, five patients had vaginal and rectal fascia or vaginal
fascia involvement, however, no recurrences were noted in the
anterior pelvic wall space.
Discussion
Clinical studies (6,7) have shown
that the recurrence and metastasis rate of stage IB-IIA cervical
cancer is ~30%. The majority of the metastatic tumors were pelvic
metastases. With an increase in risk factors, including lymph node
metastasis, infiltration of the uterus and tumor diameter ≥2 cm,
the post-operative recurrence rate can increase to 40–50%.
Post-operative concurrent radiotherapy and chemotherapy can reduce
the recurrence rate to 46%, however, there are 15% of patients
remaining, who exhibit post-operative radiotherapy recurrence.
Distant metastasis is the main contributor to mortality rates in
patients with cervical cancer recurrence (8). Stratified studies on the mode of surgery
have been limited, and the precise location of pelvic recurrences,
and the examination of invasion and spread are also deficient. Gene
mutations, metabolic abnormalities and morphological changes are
essential in the process of tumor development. PET/CT combined with
imaging medicine and tumor metabolism can be used for follow-up
monitoring of cervical cancer following treatment (9), which not only facilitates earlier
detection of recurrence and metastatic lesions (10), but also assists in confirming the
metastasis of local cancer. In the present study, PET/CT was used
to analyze the first site of recurrence of cervical cancer, and the
anatomical basis of invasion and spread.
Post-operative recurrence and metastasis in type B
radical resection in the 86 patients with early cervical cancer
showed that the simple parametrial recurrence rate was 67.4%
(58/86), the vaginal recurrence rate was 12.8% (11/86), the pelvic
lymph node recurrence rate was 8.1% (7/86), the pelvic lymph node
and extra-pelvic metastatic rate was 5.8% (5/86), the parametrial
recurrence and pelvic metastatic rate was 3.5% (3/86) and the
simple pelvic external transfer rate was 2.3% (cultured). The
results were similar to the results reported by Wang et al
(11). Among the 86 patients, 45 had
simple uterine cervix recurrences, including recurrences of the
primary sacral ligament and 13 vaginal recurrences, which is the
first site of recurrence. For patients with negative margins,
negative lymph nodes and an interstitial infiltration depth ≥1/2,
the recurrence rate was higher, compared with patients with
interstitial infiltration <1/2 depth. The parametrial and
vaginal recurrence rates were reduced (χ2=6.24,
P=0.031). Elit et al (12)
summarized and analyzed 17 retrospective clinical studies and found
that the detection rate for recurrences of cervical cancer
following surgery were as follows: Physical examination, 29–71%;
CT, 0–34%; vaginal cytology, 0–17%. As the principal method of
screening for cervical cancer, vaginal cytology is significant in
reducing the incidence of cervical cancer, but is less important in
detecting recurrent cervical cancer. The present study showed that
the recurrence of early invasive cervical cancer was primarily
extended from the mid-uterus to the vagina. The tumor continues to
grow and infiltrates the surrounding tissue, including the vagina.
Prior to positive-vaginal cytology, the tumor has formed and can be
detected by gynecologic examination and imaging. Therefore, the
monitoring of post-operative patients, imaging and physical
examinations are more useful, compared with vaginal cytology. In
addition, the present study showed the correlation between age and
site of recurrence; for elderly patients, particularly patients
>60 years of age, the recurrence rate was 68.4% (13/19) in the
vaginal and paravaginal tissues. Compared with the ≤60-year-old
group, in which the recurrence rate was 16.4% (11/67), the
recurrence rate was statistically increased in the ≥60-year-old
group (χ2=19.9, P<0.01).
Landoni et al (13) pathologically analyzed the tissue
specimens of 230 patients with cervical cancer stage IB-IIA,
following radical surgery. The proportion of cancer infiltration to
the main ligaments (vesicouterine and uterosacral) and rectovaginal
septum were 34, 23, 15 and 15%, respectively. The paracervical
infiltration depth was first associated with cervical stromal
infiltration. The post-operative cervical cancer recurrence can
spread along the lateral residual sacral and vaginal ligaments to
the pelvic wall. According to the characteristics of PET/CT images
in several patients, the invasion pathway of the main ligament was
as follows: Continuous images in combination with changes in SUV
demonstrated that cardinal ligament invasion pathways were the
earliest cancer recurrence in the cardinal ligament stump. The
internal iliac vascular axis (the main vascular ligament) was
central with cancer spreading outwards and upwards, close to the
iliac arterial bifurcation, terminating at the basin wall between
the internal and external iliac vessels. Recurrent tumor
infiltration occurred from the sacral ligament stump, and extended
from the mesorectum backwards to the second, third and fourth
sacral vertebrae. If invasion continued, the cancer invaded the
mesorectum, the piriformis muscle and soft tissues of the pelvic
wall, as shown in Fig. 2. If the
patient had no abnormal vaginal discharge, abnormal cytology and
the gynecologic examination of the vaginal mucosal was normal, but
a submucosal paravaginal tissue mass was palpated, a biopsy was
performed. Paravaginal tumors arose in the fascial tissues in nine
cases, which involved the cervical vaginal ligament and progressed
to the medial aspect of the posterior wall of the ureter and
bladder, further infiltrating downward to the urethra. The tumor
spread along the same side of the rectovaginal fascia, as shown in
Fig. 3, in agreement with Xiaohong
et al and Zhou et al (14,15), who
found that the majority of the sacral ligaments attached to the
first, second and third sacral vertebrae, and the morphology of the
fourth vertebral body was altered. The recurrence rate of cervical
deep muscle invasive carcinoma was twice that of vaginal
recurrences. The PET/CT imaging showed that the tumor appeared in
the vaginal stump and vaginal bladder ligament. The primary sacral
ligament is a three-dimensional connective tissue extending from
the cervix to the upper vagina. The primary sacral ligament exists
as a complex form in the cervix and vagina, separates in the
process of extending outward, and terminates on the side wall of
the basin and the sacrum, whereas the main sacral ligament complex
extends down to the vagina. Following surgery, the remnants spread
out through the residual ligament, and the type and modality of
surgery affects the rate of recurrence of early cervical cancer
(16,17). Following a type B radical resection,
the basin wall of each ligament remains partially connected. The
tumor can spread along the main and paravaginal ligaments, and
invade the adjacent organs.
In the early stage, the local spread of cervical
cancer is not random. Höckel (18)
and Höckel et al (19)
reported that early cervical cancer invasion and metastasis are
limited to the cervix, uterus, and the surrounding mesentery
ligaments. These tissues are derived from the gyneduct in the
embryonic stage. For tissues from other embryonic sources, there
was less infiltration, even for adjacent structures, including
nervous tissue. For patients with cervical cancer in early stage
IB-IIA, total hysterectomy (removal of the pelvic wall of the main
sacral ligament) can preserve the nerves and avoid post-operative
prophylactic radiotherapy. In the present study, 67.4% of the
patients with recurrent cervical cancer had tumors confined to the
posterior peritoneum with spread along these ligaments. These
ligaments are also barriers to outward spread of the tumor. In the
early stage, recurrence along the ligament is rare and metastasis
of the pelvic peritoneal organs is singular. In the present study,
only one patient with squamous cell carcinoma of the vagina had
intestinal obstruction and one patient with adenocarcinoma had
metastasis to the abdominal cavity.
The biological behavior of tumor development
determines its treatment. The present study analyzed the recurrence
and spread of early stage cervical cancer following type B radical
surgery, and the results showed that the recurrence rateinthe
cardinal and uterosacral ligament was 52.3%, and that thiswas the
most common site of recurrence. According to the QM classification,
C type surgery is always recommended in cervical cancer stage
IB-IIA. Type C1 surgery is recommended to maintain the sacral
ligament close to the pelvic wall of the resection and preservation
of the bladder nerve. For patients with adjuvant radiotherapy
following type B surgery, all cervical residual ligaments require
treatment as part of the region involved, however, the dosage of
radiation requires further evaluation. As the patients in the
present study were from a number of treatment centers,
heterogeneity cannot be excluded. Therefore, to improve the
treatment of cervical cancer, a prospective clinical study is
required.
Acknowledgements
This study was supported by the Science and
Technology Department of Henan province (grant no.
132300410047).
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hu SY, Zheng RS, Zhao FH, Zhang SW, Chen
WQ and Qiao YL: Trend analysis of cervical cancer incidence and
mortality trends from 1989 to 2008 in Chinese women. Zhongguo Yi
Xue Ke Xue Yuan Xue Bao. 36:119–125. 2014.(In Chinese). PubMed/NCBI
|
|
3
|
Ryu SY, Kim MH, Nam BH, Lee TS, Song ES,
Park CY, Kim JW, Kim YB, Ryu HS, Park SY, et al: Intermediate-risk
grouping of cervical cancer patients treated with radical
hysterectomy: A Korean Gynecologic Oncology Group study. Br J
Cancer. 110:278–285. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Querleu D and Morrow PC: Classification of
radical hysterectomy. Lancet Oncol. 9:297–303. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Khatun S, Huda AQ, Begum SK and Ferdous J:
Evaluation of pelvic lymphadenectomy during radical hysterectomy
for cervical cancer. Mymensingh Med J. 26:287–292. 2017.PubMed/NCBI
|
|
6
|
Rotman M, Sedlis A, Piedmonte MR, Bundy B,
Lentz SS, Muderspach LI and Zaino RJ: A phase III randomized trial
of postoperativepelvic irradiation in Stage IB cervical carcinoma
with poor prognostic features: Follow-up of a gynecologic oncology
group study. Int J Radiat Oncol Biol Phys. 65:169–176. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Monk BJ, Wang J, Im S, Stock RJ, Peters WA
III, Liu PY, Barrett RJ II, Berek JS, Souhami L, Grigsby PW, et al:
Rethinking the use of radiation and chemotherapy afterradical
hysterectomy: A clinical-pathologic analysis of a Gynecologic
OncologyGroup/Southwest Oncology Group/Radiation Therapy Oncology
Group trial. Gynecol Oncol. 96:721–728. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Vandecaveye V, Dresen R and De Keyzer F:
Novel imaging techniques in gynaecological cancer. Curr Opin Oncol.
29:335–342. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hanprasertpong J, Jiamset I, Geater A,
Rattanaburi A and Thannil S: Clinical aspect and prognostic factors
for survival in patients with recurrent cervical cancer after
radical hysterectomy. Oncol Res Treat. 39:704–711. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Brooks RA, Rader JS, Dehdashti F, Mutch
DG, Powell MA, Thaker PH, Siegel BA and Grigsby PW: Surveillance
FDG-PET detection of asymptomatic recurrences in patients with
cervical cancer. Gynecol Oncol. 112:104–109. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang J, Wang T, Yang YY, et al: Analysis
of recurrence and metastasis after radical treatment of cervical
cancer. Modern Oncol. 21 Suppl:S120–S122. 2013.
|
|
12
|
Elit L, Fyles AW, Devries MC, Oliver TK
and Fung-Kee-Fung M: Gynecology Cancer Disease Site Group:
Follow-up for women after treatment for cervical cancer: A
systematic review. Gynecol Oncol. 114:528–535. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Landoni F, Maneo A, Colombo A, Placa F,
Milani R, Perego P, Favini G, Ferri L and Mangioni C: Randomised
study of radical surgery versus radiotherapy for stage Ib-IIa
cervical cancer. Lancet. 350:535–540. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xiaohong Y, Wei C, Huicheng X, et al:
Observation of MRI in female pelvic floor. J Local Surg.
21:252–254. 2012.
|
|
15
|
Zhou XH, Ouyang SX and Xiao PZ: Applied
anatomy and clinical significance of uterosacral ligament. J Nanhua
Univ. 35:175–179. 2007.
|
|
16
|
Kong TW, Chang SJ, Piao X, Paek J, Lee Y,
Lee EJ, Chun M and Ryu HS: Patterns of recurrence and survival
after abdominal versus laparoscopic/robotic radical hysterectomy in
patients with early cervical cancer. J Obstet Gynaecol Res.
42:77–86. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ungár L, Pálfalvi L, Tarnai L, Nechushkina
V, Lintner B and Novák Z: FACOG Committee on Practice Bulletins:
Surgical treatment of stage IB cervical cancer. Int J Gynecol
Cancer. 22:1597–1603. 2012.PubMed/NCBI
|
|
18
|
Höckel M: Do we need a new classification
for radical hysterectomy? Insights in surgical anatomy and local
tumor spread from human embryology. Gynecol Oncol. 107 1 Suppl
1:S106–S112. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Höckel M, Horn LC, Manthey N, Braumann UD,
Wolf U, Teichmann G, Frauenschläger K, Dornhöfer N and Einenkel J:
Resection of the embryologically defined uterovaginal (Müllerian)
compartment and pelvic control in patients with cervical cancer: A
prospective analysis. Lancet Oncol. 10:683–692. 2009. View Article : Google Scholar : PubMed/NCBI
|