Introduction
The spleen is an important immune organ that has
antitumor activity and an abundance of blood cells, a small amount
of which are afferent lymphatic cells. All of these features
contribute to a relatively low tumor incidence, accounting for only
0.03% of all types of tumors in humans (1). Splenic tumors can be divided into three
types: Benign, malignant and metastatic, all of which are rare. The
malignant tumors that occur in the spleen are typically
lymphosarcoma, reticulosarcoma, angiosarcoma and fibrosarcoma
(2). The most common primary lesion
sites with splenic metastases are, in order of decreasing
frequency, the lungs, stomach, pancreas, liver and colon (3). As has been noted, primary tumors in the
spleen are usually of lymphatic or vascular origin, whereas an
epithelial tissue origin is rare. To the best of our knowledge,
there has only been one previous case report of metastatic
adenocarcinoma of the spleen, with no primary lesion found by
general examination, exploratory laparotomy or postoperative
follow-up (4). However, single
squamous cell carcinoma of the spleen with no identified lesion in
a different organ has not been previously reported. The study aims
to share this exception and demonstrate its poor response to
chemotherapy and only a 14-month overall survival despite receiving
surgery.
Case report
Case presentation
A 28-year-old male without a history of trauma was
admitted to the Second Xiangya Hospital in February 2015, Central
South University (Changsha, China) on an emergency basis due to a
sudden pain in the left upper abdomen. There were no clear
abnormalities in the physical examination, aside from tenderness,
with no rebound pain, in the left upper abdomen. An abdominal
computed tomography (CT) scan suggested that there was a lesion on
the spleen, which may have been caused by a rupture of a splenic
hemangioma. Subsequently, exploratory laparotomy revealed that
there was a palpable hard mass on the surface of the spleen, which
invaded the retroperitoneum. The patient subsequently received an
excision of the splenic lump.
Postoperative pathological
analysis
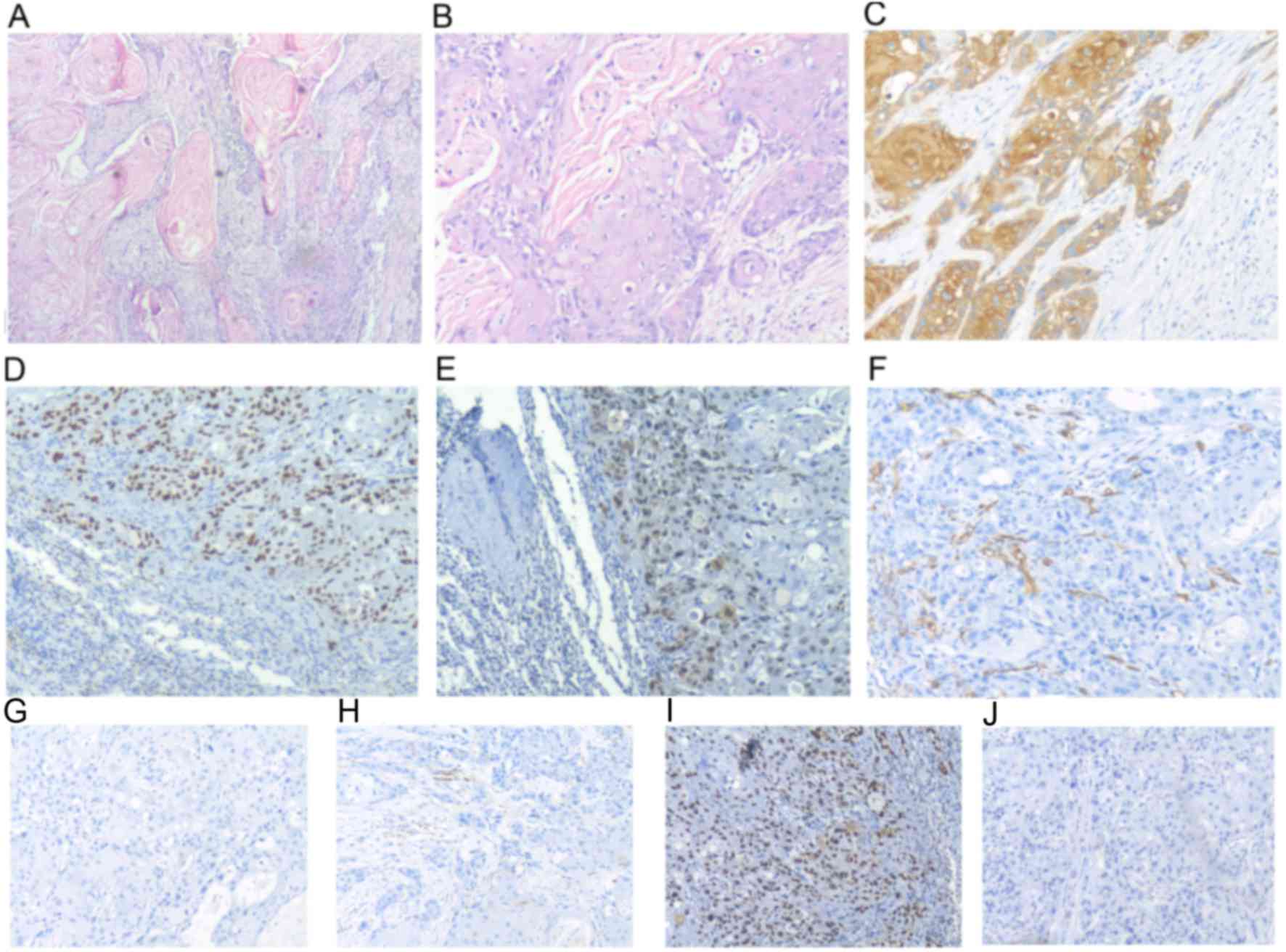
The postoperative pathological examination revealed
a 6×7×8-cm mass, with partial membrane invasion, which is an
indicator of well to moderately differentiated squamous cell
carcinoma (Fig. 1). The results of
immunohistochemistry were as follows: Thyroid transcription
factor-negative, cytokeratin 7-negative, p63-positive,
p40-positive, cluster of differentiation 34-negative, creatine
kinase-positive, leucocyte common antigen-negative and p53-positive
(Fig. 1).
The fluorescence microscope (Nikon Eclipse 55i;
Nikon Corporation, Tokyo, Japan) was used to observe the slides of
the tumor.
PET-CT
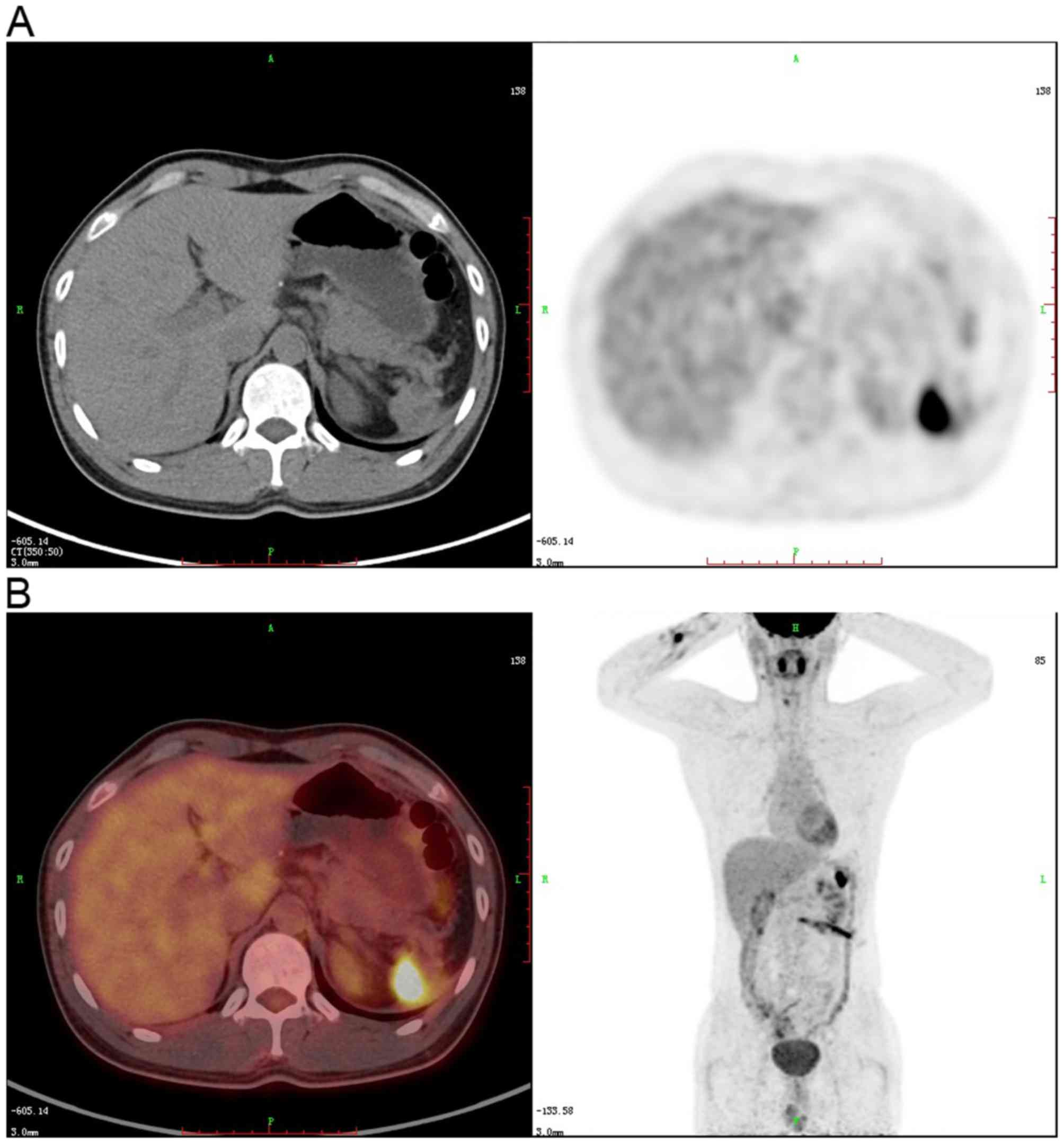
A postoperative systemic PET-CT scan indicated that
nodular soft tissue located in the spleen area, next to the
diaphragm, with an abnormal increase in glucose metabolism, was a
residual postoperative effect. Apart from this, there was no
abnormal increase in glucose metabolism according to the whole-body
PET-CT imaging (Fig. 2).
Treatment
Subsequent to 4 cycles of chemotherapy (120 mg
docetaxel (day 1) and 40 mg cisplatin (day 1–3) were administered
intravenously; 21 days comprised a single cycle), the patient
underwent another PET-CT examination, which showed that the
previous nodular soft tissue had increased in size (57×44 mm vs.
23×22 mm; SUVmax 13.7 vs. 6.4). Additionally, new nodules appeared
with increased glucose metabolism in the clearance between the
curvatura gastrica major and the diaphragm, and enlarged lymph
nodes were present in the left side of the abdominal aorta, which
were considered metastases, while no abnormalities were found in
the other organs. Subsequently, the patient received a single
circle of second-line chemotherapy (Gemcitabine, administered at
1,800 mg intravenously on day 1 and 8, or Capecitabine,
administered at 1,500 mg orally twice a day on day 1–14). However,
the patient was reluctant to proceed to the second cycle of
treatment, therefore the treatment ceased.
Follow-up
The patient was discharged in good general condition
in August 2015. Afterwards, the patient elected to use a Chinese
herbal treatment. Since February 2016, the patient begun to suffer
from bloating and abdominal pain due to the intestinal obstruction
resulting from peritoneal metastasis and subsequently, the patient
succumbed to cachexia in April 2016, 14 months after diagnosis.
Discussion
As previously referenced, the analysis of Zhan
(4) of 194 cases of spleen tumors
categorized 95 cases as primary malignant lymphoma, 45 as
metastatic tumors and the remaining as mesenchymal malignant
tumors, including angiosarcoma, malignant fibrous sarcoma and
liposarcoma. However, none were identified as squamous cell
carcinoma. In the data, a median survival of stage I–III malignant
lymphomas are 30, 18, and 2 months (4). However, in the case outlined by the
present study, no metastases was detected at diagnosis and the
overall survival overall survival was merely 14 months.
The spleen consists of a membrane, the trabeculae,
white pulp, red pulp and the marginal zone, which are all
mesenchymal (5). While squamous cell
carcinoma is a malignant tumor that originates from the epidermis
or adnexa, its cancer cells have various degrees of
diversification, which is common in the areas covered by squamous
epithelia, including the skin, mouth, esophagus, cervix and vagina,
or in cases of immune suppression, such as in organ transplant
patients (6). In addition, certain
regions of the body, including the bronchi, bladder and renal
pelvis, that do not have a squamous epithelial covering, can also
develop squamous cell carcinoma by squamous metaplasia (7). Notably, there is no epithelial tissue in
the spleen. Therefore, the cause of squamous cell carcinoma of the
spleen is considered to be as follows. First, metastatic squamous
cell carcinoma should be taken into consideration. False-negative
PET-CT examinations can occur when the size of the primary tumor is
too small, or when the metabolism is not active (8). Even subsequent to disease progression
and tumor metastasis to the peritoneum and the abdominal cavity,
the primary tumor is occasionally still not observed upon review of
the PET-CT scan results. The other possible mechanism may be, to a
certain degree, similar to endometriosis (9). Due to the abundant blood flow through
the spleen, fragments of epithelial tissue from other areas of the
body enter the spleen with the blood and implant in it. Stimulated
by inflammation or hormones over time, squamous metaplasia can then
occur (7), followed by atypical
hyperplasia, and finally, squamous cell carcinoma develops.
Therefore, the origin and the mechanism of the tumor in the present
case study remains unknown, and due to the reluctance of the
patient, imaging data or a biopsy of the metastatic lesions were
not obtained.
In conclusion, the present study details a case of
squamous cell carcinoma of the spleen, where no primary lesion was
found, which to the best of our knowledge, has not been reported
previously. Furthermore, in this case, the survival rate was
notably short when compared with other malignant metastasis of the
spleen and therefore provides potentially useful information
pertaining to the response for standard treatment and the prognosis
of the splenic squamous cell carcinoma for a single case.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The authors declare that materials described in the
manuscript, including all relevant raw data, will be freely
available to any scientist wishing to use them for non-commercial
purposes, without breaching participant confidentiality from the
department of Oncology, Pathology and Radiology of The Second
Xiangya Hospital of Central South University.
Authors' contributions
XL was in charge of the patient, decided the
treatment and revised the manuscript critically for important
intellectual content. FM assisted with data collection and
analysis. ZJ came up with the idea, planned out the article and
wrote the manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
The Second Xiangya Hospital of Central South University (Changsha,
China).
Consent for publication
Written patient consent was obtained. The IRB name
is the Ethics Committee of The Second Xiangya Hospital of Central
South University, located in the Second Xiangya Hospital of Central
South University, Changsha, Hunan, China.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Coon WW: Surgical aspects of splenic
disease and lymphoma. Curr Probl Surg. 35:543–646. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Badiani R, Schaller G, Jain K, Swamy R and
Gupta S: Angiosarcoma of the spleen presenting as spontaneous
splenic rupture: A rare case report and review of the literature.
Int J Surg Case Rep. 4:765–767. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lam KY and Tang V: Metastasic tumors to
the spleen: A 25-year clinicopathologic study. Arch Pathol Lab Med.
124:526–530. 2000.PubMed/NCBI
|
|
4
|
Zhan S: Spleen cancer of 194 cases. Chin J
Gen Surg. 12:183–184. 1997.(In Chinese).
|
|
5
|
Lewis JT, Gaffney RL, Casey MB, Farrell
MA, Morice WG and Macon WR: Inflammatory pseudotumor of the spleen
associated with a clonal Epstein-Barr virus genome. Case report and
review of the literature. Am J Clin Pathol. 120:56–61. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Singh MK and Brewer JD: Current approaches
to skin cancer management in organ transplant recipients. Semin
Cutan Med Surg. 30:35–47. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Clouston D and Lawrentschuk N: Metaplastic
conditions of the bladder. BJU Int. 2 Suppl 112:27–31. 2013.
View Article : Google Scholar
|
|
8
|
Padma S, Sundaram PS and George S: Role of
positron emission tomography computed tomography in carcinoma lung
evaluation. J Cancer Res Ther. 7:128–134. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Meola J, Rosa e Silva JC, Dentillo DB, da
Silva WA Jr, Veiga-Castelli LC, Bernardes LA, Ferriani RA, de Paz
CC, Giuliatti S and Martelli L: Differentially expressed genes in
eutopic and ectopic endometrium of women with endometriosis. Fertil
Steril. 93:1750–1773. 2010. View Article : Google Scholar : PubMed/NCBI
|