Introduction
Osteosarcoma is the most common type of primary bone
sarcoma in teenagers and represents the second highest cause of
cancer-associated mortality in this age group worldwide (1). At present, the treatment of osteosarcoma
consists of preoperative chemotherapy, followed by wide surgical
resection and a postoperative chemotherapy regimen, modified
according to the proportion of necrotic cells (2). However, in spite of the advancements in
early detection and combined therapy strategies, the prognosis for
patients with osteosarcoma remains poor, and between 30 and 40% all
patients develop lung metastasis, which is the primary cause of
mortality from this disease (3). In
addition, the majority of chemotherapeutics exhibit the risk of
short- and long-term toxic effects. The emerging knowledge of the
pathogenesis and genetic abnormalities associated with osteosarcoma
has exposed the field to new potential molecular targets (4).
Baculoviral IAP repeat containing 7 (termed Livin)
is a novel member of the inhibitor of apoptosis proteins (IAPs)
family, which controls the basal level of apoptosis in mammalian
cells (5). The expression of Livin is
associated with aggressive disease and poor clinical outcome in
patients with osteosarcoma (6). Tumor
growth and metastasis are dependent on the degree of
neovascularization, which is regulated by pro-angiogenic and
anti-angiogenic factors. Vascular endothelial growth factor (VEGF)
is an important angiogenic factor and has been studied most
extensively in a number of types of cancer, including breast cancer
and renal cell carcinoma (7,8). Previous studies have demonstrated that
VEGF stimulation may increase Livin expression and induce the
pathogenesis of human esophageal carcinoma and cervical cancer
(9,10). Placenta growth factor (PlGF) is a
dimeric glycoprotein, and is structurally and functionally
associated with VEGF (11). PlGF is
not produced by the majority of types of normal human tissue and
serves a function in pathological angiogenesis (12). In addition, it has been revealed that
PlGF secretion in MG-63 osteosarcoma cells was induced by bone
morphogenetic protein-2, and led to the paracrine regulation of
angiogenesis and hemopoiesis in bone formation (13). To date, the expression of PlGF in
osteosarcoma and any association between PlGF and Livin remains
unknown. On the basis of previous studies (14,15), the
present study examined the expression levels of Livin and PlGF in
human osteosarcoma tissues and osteosarcoma cells, and analyzed
their associations and prognostic values in osteosarcoma.
Materials and methods
Cell culture
Human osteosarcoma cell lines (U2OS, SaOS-2 and
MG-63) purchased from the Cell Bank of Chinese Academy of Science
(Shanghai, China) were cultured in Dulbecco's modified Eagle's
medium (Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA),
supplemented with 10% fetal bovine serum (Gibco; Thermo Fisher
Scientific, Inc.). All cell lines were maintained in an atmosphere
of 5% CO2 with humidity at 37°C.
Patients and tissue samples
The present study was retrospective. Human
osteosarcoma specimens were obtained from 48 patients with
osteosarcoma between Enneking's stages IB and III. The present
study was approved by the institutional review board of Zhongshan
Hospital (Shanghai, China) and all aspects of the study comply with
the Declaration of Helsinki. As this is a retrospective study, the
Ethics Committee approved that informed consent was not required
because data would be analyzed anonymously. However, the patients
or their guardians signed informed consent for biopsy or tumor
excision surgery. No patients received pre-surgical chemotherapy or
radiotherapy. Specimens were fixed at 4°C in 10% formalin-buffered
solution for 24 h, embedded in paraffin and cut into 5-µm tissue
sections prior to immunohistochemistry. A total of 30 males and 18
females were included in the present study, with a mean age of 22.6
years (range, 6–72 years). According to Enneking's staging
(16), 17 patients were staged
between IB and IIA, and the remaining 31 patients were staged
between IIB and IIIB (16). The
tumors were located on the distal femur in 27 patients, proximal
tibia in 7 patients, proximal fibula in 2 patients, proximal
humerus in 7 patients and at other sites (vertebra, pelvis and
tarsus) in 5 patients (Table I). The
histological type of osteosarcoma was osteoblastic, chondroblastic
and fibroblastic in 29, 11 and 8 patients, respectively, which was
determined by the combination of imaging manifestation, clinical
manifestation and pathological features. There were 30 cases with a
tumor diameter ≤5 cm and a total of 18 cases exhibited a tumor
diameter >5 cm. A total of 10 normal bone tissue samples were
selected from 3 male and 7 female healthy donors, with a mean age
of 61.1 years (range, 55–64 years) who had undergone total knee
arthroplasty from Jan 2013 to Dec 2014 at the Zhongshan Hospital.
The samples were frozen in liquid nitrogen at −196°C immediately
following excision and then cut into 5-µm tissue sections.
Protocols were approved by the Institutional Review Boards of
Zhongshan Hospital and each patient in the healthy controls group
provided written informed consent for total knee arthroplasty
surgery. Clinical data were obtained from the medical records.
Follow-up time was calculated from the date of surgery to the death
of the patient or 5 years after surgery.
 | Table I.Association between the expression of
Livin and PlGF and the clinicopathological characteristics of
patients with osteosarcoma. |
Table I.
Association between the expression of
Livin and PlGF and the clinicopathological characteristics of
patients with osteosarcoma.
| Characteristic | n | Livin positive, n
(%) | P-value | PlGF positive, n
(%) | P-value |
|---|
| Cases | 48 | 28 (58.3) |
| 29 (60.4) |
|
| Sex |
|
| 0.762 |
| 0.594 |
| Male | 30 | 17 (56.7) |
| 19 (63.3) |
|
|
Female | 18 | 11 (61.1) |
| 10 (55.6) |
|
| Age, years |
|
| 0.922 |
| 0.863 |
|
≤20 | 26 | 15 (57.7) |
| 16 (61.5) |
|
|
>20 | 22 | 13 (59.1) |
| 13 (59.1) |
|
| Tumor site |
|
| 0.883 |
| 0.315 |
|
Femur | 27 | 16 (59.3) |
| 18 (66.7) |
|
| Tibia
fibula | 9 | 6 (66.7) |
| 6 (66.7) |
|
|
Humerus | 7 | 4 (57.1) |
| 4 (57.1) |
|
|
Others | 5 | 2 (40.0) |
| 1 (20.0) |
|
| Enneking stage |
|
| 0.003 |
| <0.001 |
|
IB-IIA | 17 | 5 (29.4) |
| 4 (23.5) |
|
|
IIB-III | 31 | 23 (74.2) |
| 25 (80.6) |
|
| Tumor diameter,
cm |
|
| 0.007 |
| 0.047 |
| ≤5 | 30 | 13 (43.3) |
| 16 (53.3) |
|
|
>5 | 18 | 15 (83.3) |
| 13 (72.2) |
|
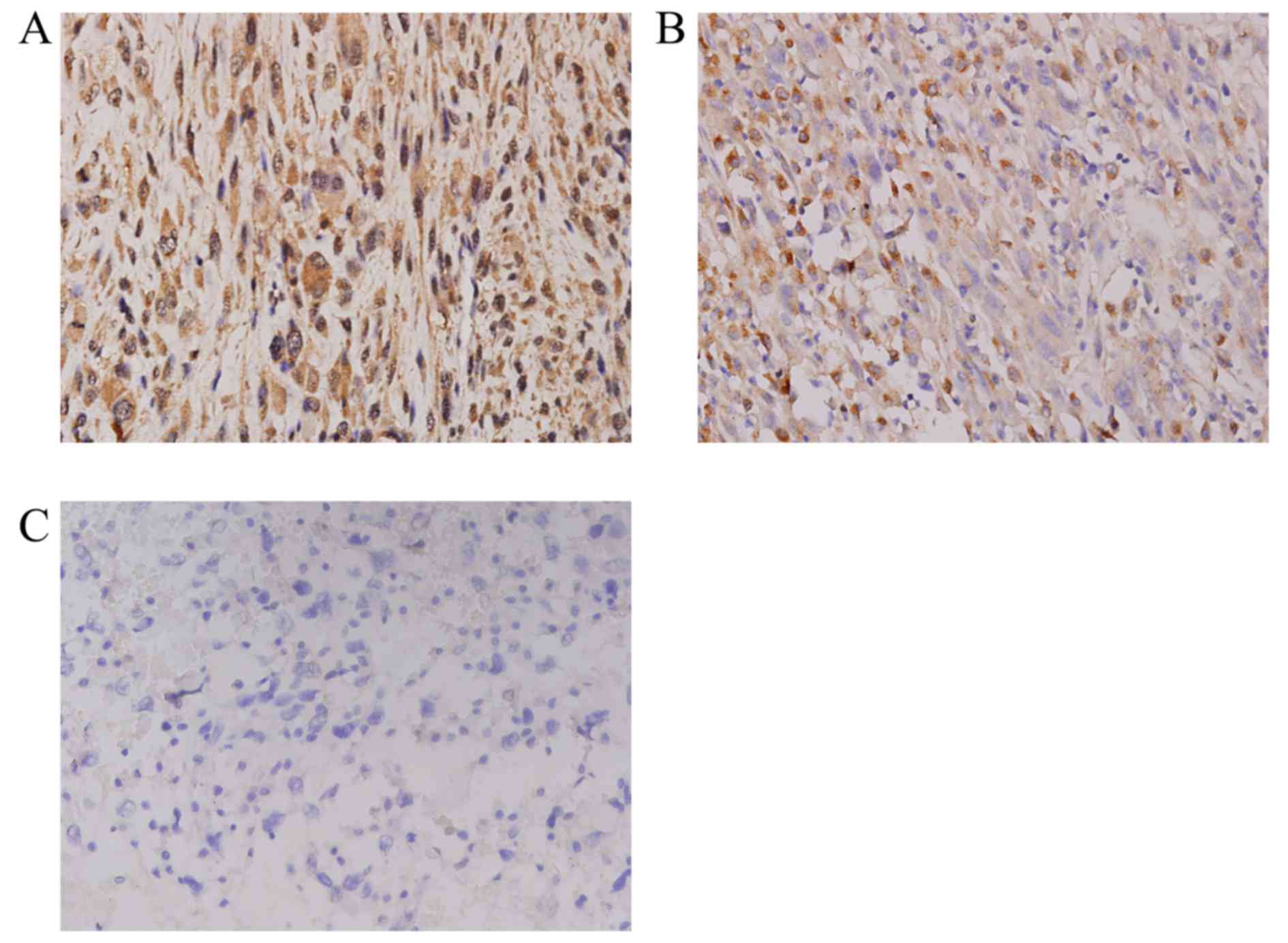
Immunohistochemistry (IHC)
All samples were decalcificated prior to IHC. The
expression of Livin and PlGF was determined by IHC. Sections were
stained with rabbit polyclonal anti-human Livin (PAB12872) and PlGF
(PAB8004) primary antibodies (1:100 dilutions; Abnova, Taipei,
Taiwan) for 12 h at 4°C and then horseradish peroxidase-conjugated
goat polyclonal anti-rabbit secondary antibody (31460; 1:5,000
dilution; Thermo Fisher Scientific, Inc.) for 20 min at 37°C,
according to the manufacturer's protocol. Bone samples were used as
negative controls for Livin and PlGF staining. The expression was
evaluated independently by two pathologists and the data from the
two investigators were averaged. Under the light microscope,
positive cells were observed as cells containing brown granules in
the nucleus or cytoplasm. For each section, a charge-coupled device
camera was used to capture at least five fields of view at
magnification ×400 (Olympus BX51 CCD; P70; Olympus Corporation,
Tokyo, Japan). Image-Pro Plus software (version 5.0; Media
Cybernetics, Inc., Rockville, MD, USA) was used to quantitatively
analyze the images. The score was calculated by summing the
intensity score and the proportion score, providing a score between
0 and 9. The proportion score was calculated as follows: 0, no
positivity; +1, ≤25% tumor cell positivity; +2, 26–50% tumor cell
positivity; and +3, >50% tumor cell positivity. The intensity
score was calculated as follows: 0, no staining; +1, weak staining;
+2, intermediate staining; and +3, strong staining. Specimens were
additionally divided into a low or high expression group, according
to their score as follows: Specimens with score ≤2 were regarded as
low expression; and specimens with scores >2 were regarded as
high expression (17).
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was isolated from osteosarcoma cells
(MG-63, Saos-2 and U-OS) with TRIzol reagent (Thermo Fisher
Scientific, Inc.) and reverse-transcribed to synthesize cDNA using
a PrimeScript 1st Strand cDNA Synthesis kit (Takara Biotechnology
Co., Ltd., Dalian, China) according to the manufacturer's protocol.
qPCR assay was conducted using a TaqMan® One-Step PCR
Master Mix (Applied Biosystems; Thermo Fisher Scientific, Inc.),
according to the following protocol: 40 cycles consisting of
denaturation at 95°C for 5 sec, annealing at 60°C for 30 sec, and
extension at 72°C for 30 sec. A standard curve was generated on the
basis of a linear association between the first cycle number at
which the fluorescence signal significantly increased
[quantification cycle (Cq) value] and the logarithm of the initial
value. The quantity of target mRNA in unknown samples was
determined from the Cq value using a standard curve. A control
without template was included in each experiment. Non-template and
DNA controls, standard dilutions, and samples were assayed in
duplicate. The expression levels of Livin and PlGF mRNA were
normalized to that of GAPDH mRNA, and divided into high and low
expression groups. GAPDH primers were as follows: Forward,
5′-GCACCGTCAAGGCTGAGAAC-3′; and reverse, 5′-TGGTGAAGACGCCAGTGGA-3′.
Equal volumes of complementary DNA from each sample were amplified
using the following primers: Livin forward,
5′-AAGGAAGAGACTTTGTCCACAGTGT-3′; Livin reverse,
5′-GGCTGCGTCTTCCGGTT-3′; PlGF forward, 5′-TCAGAGGTGGAAGTGGTA-3′;
and PIGF reverse, 5′-ACACAGTGCAGATTCTCA-3′. Two independent
experiments were performed in triplicate, and the PCR products were
measured using an ABI PRISM 7700 Sequence Detection System (Applied
Biosystems; Thermo Fisher Scientific, Inc.) and analyzed with ABI
PRISM 7000 SDS v.1.2.3 RQ software (Applied Biosystems; Thermo
Fisher Scientific, Inc.).
Statistical analysis
For survival analysis, overall survival (OS) time
was defined as the interval between the date of diagnosis and the
date of mortality or the last follow-up. All statistical analyses
were performed using SPSS software (v.18; SPSS, Inc., Chicago, IL,
USA). To analyze the prognostic significance of Livin and PlGF
expression, the χ2 test was used to test the association
between Livin and PlGF expression level and other prognostic
factors. The Kaplan-Meier method was used to estimate curves for OS
for the subgroups of potential prognostic factors, and comparisons
were conducted using the log-rank test. Univariate and multivariate
regression analyses according to the Cox's proportional hazards
regression model, with OS as the dependent variable, were used to
evaluate Livin and PlGF expression as potential independent
prognostic factors. The Cox proportional hazard model was used to
analyze data for Livin and PlGF expression against OS time (in
months) and patient status (deceased vs. alive). Covariates
included Livin and PlGF expression level (as a continuous
variable), age at diagnosis, tumor stage (low stages IB-IIA vs.
advanced stages IIB-III), and tumor size. Outcome data were derived
from a detailed review of patient medical records and oncology
clinical chart, and were supplemented by contact with the treating
physician, patient and patient family. P<0.05 was considered to
indicate a statistically significant difference.
Results
Expression of Livin or PlGF is
increased in osteosarcoma specimens
The associations between the clinicopathological
factors and the expression of Livin or PlGF in 48 osteosarcoma
tissues are shown in Table I. The
expression levels of Livin and PlGF in osteosarcoma specimens were
significantly increased, compared with those in normal bone tissues
(P<0.01). Livin and PlGF proteins were consistently detected in
28 (58.3%) and 29 (60.4%) of the 48 osteosarcoma specimens,
respectively, but in none of the normal bone tissues (Fig. 1). Livin and PlGF were predominantly
identified in a granular pattern in the cytoplasm. In 17 cases
(35.4%), the two proteins were present in the cytoplasm and in 8
cases (16.7%) there was no detection of either protein. In
addition, using Spearman's correlation coefficient analysis, no
association was identified between the expression of Livin and PlGF
(P=0.960).
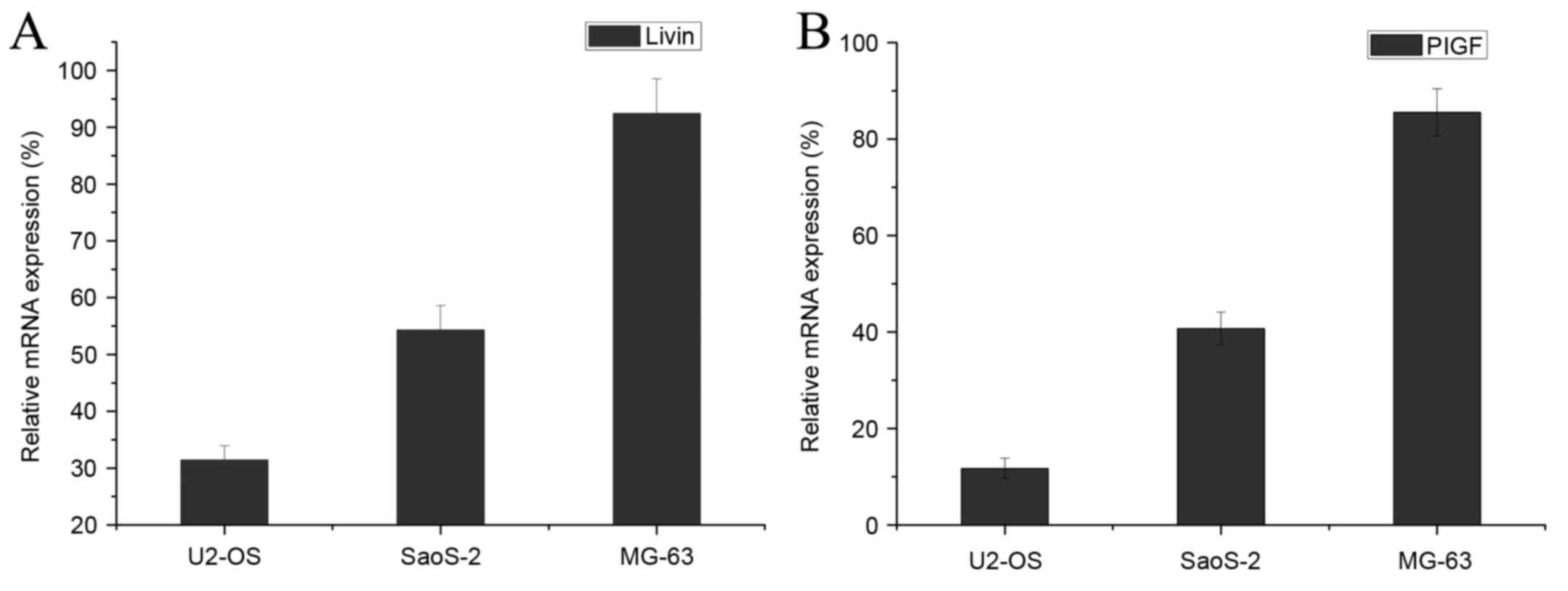
Expression of Livin or PlGF is
increased in OS cell lines
qPCR was performed to determine the mRNA expression
levels of Livin and PlGF in three osteosarcoma cell lines (SaOS-2,
MG-63 and U2OS). The expression levels of Livin and PlGF genes were
determined in three osteosarcoma cell lines, and were markedly
increased in MG-63 cells, compared with those in U2OS and SaOS-2
cells (Fig. 2).
Expression of Livin or PlGF is
associated with advanced stage osteosarcoma and tumor diameter
The IHC results demonstrated that the expression
levels of Livin and PlGF were associated with pathological stage
and tumor diameter (Table I). The
expression levels of Livin and PlGF in patients between stages IB
and IIA were significantly decreased, compared with those in
patients between stages IIB and III (P=0.003 and P<0.001,
respectively). Patients were divided into two groups according to
tumor diameter (≤5 cm and >5 cm), and the expression levels of
Livin and PlGF were compared. There were 30 cases with a tumor
diameter ≤5 cm, and the positive expression rate of Livin and PlGF
was 43.3% (13 cases) and 53.3% (16 cases), respectively. A total of
18 cases exhibited a tumor diameter >5 cm, and the positive
expression rate of Livin and PIGF was 83.3% (15 cases) and 72.2%
(13 cases), respectively. A significant association was identified
between the expression levels of Livin or PlGF and tumor diameter
(P=0.007 and P=0.047, respectively). However, there was no
significant association between the expression levels of Livin and
PlGF and sex, age or site of tumor (Table
I).
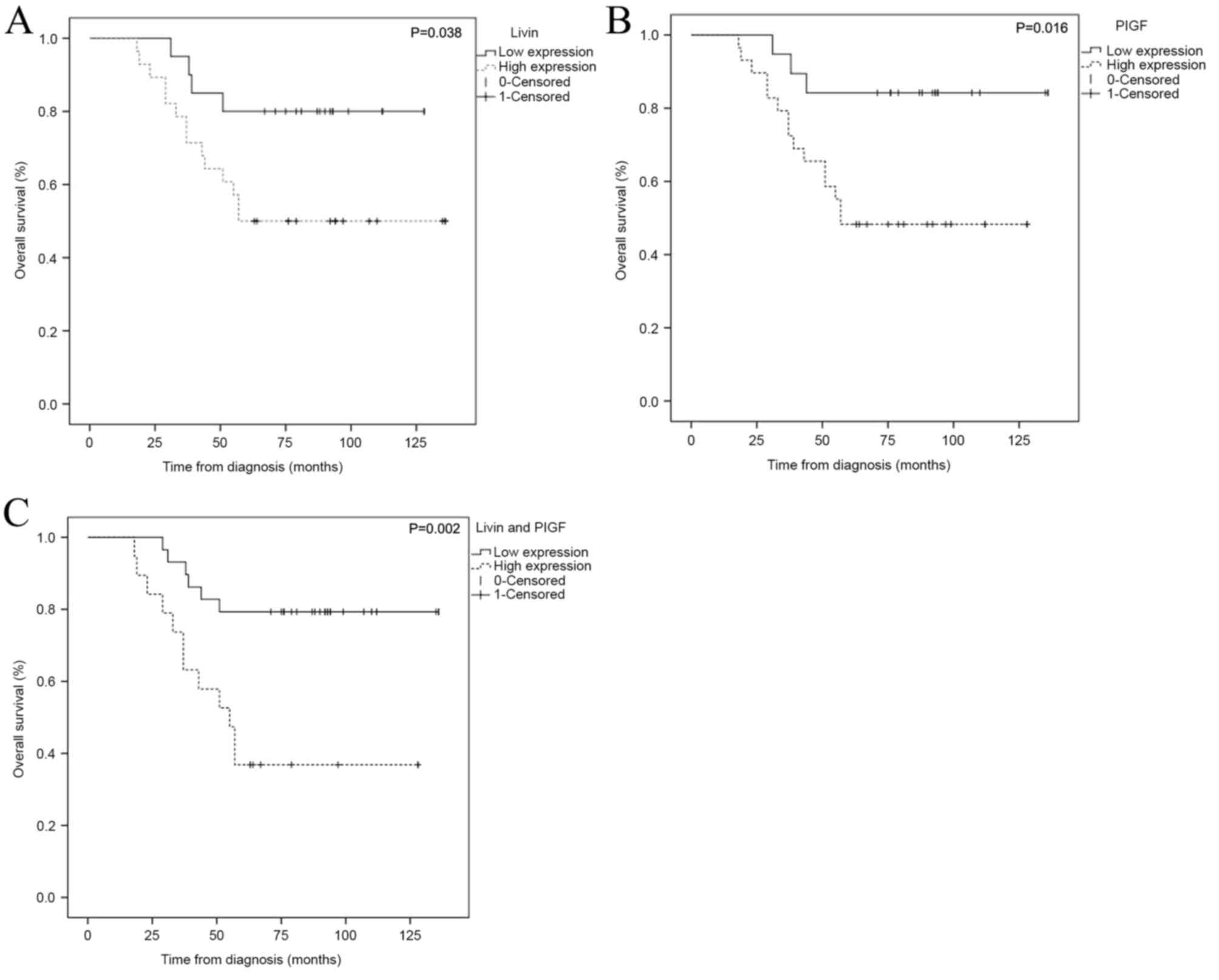
Expression of Livin or PlGF is
associated with 5-year OS rate
For all of patients in the present study, the median
OS time was 73.9 months (range, 18.3–136.5 months) and the 5-year
OS rate of the Livin and PlGF high expression group (7 cases,
23.3%) was significantly decreased, compared with that of the Livin
and PlGF low expression group (23 cases, 66.7%) (P=0.003). Analysis
of the 5-year OS rate revealed a significant difference between
patients with tumors exhibiting expression of Livin (n=28) and
those with tumors that did not exhibit expression of Livin (n=20)
(P=0.034). For the 29 patients exhibiting PlGF expression, the
survival analysis differed significantly from that of patients who
did not express PIGF (P=0.012) (Table
II). Patients with osteosarcoma with low Livin or PlGF
expression exhibited a significantly increased survival time,
compared with that of patients with high Livin or PlGF expression
(Fig. 3).
 | Table II.Expression of Livin and PlGF in
osteosarcoma and its association with 5-year OS. |
Table II.
Expression of Livin and PlGF in
osteosarcoma and its association with 5-year OS.
|
| Expression |
|---|
|
|
|
|---|
|
| Livin | PlGF | Livin and PlGF |
|---|
|
|
|
|
|
|---|
| Variables | Positive, n
(%) | Negative, n
(%) | P-value | Positive, n
(%) | Negative, n
(%) | P-value | Positive, n
(%) | Negative, n
(%) | P-value |
|---|
| 5-year OS,
n=48 | 14 (46.7) | 16 (53.3) | 0.034 | 14 (46.7) | 16 (53.3) | 0.012 | 7 (23.3) | 23 (76.7) | 0.003 |
| Mean survival time,
months | 87.00 | 110.35 | 0.038 | 81.72 | 120.47 | 0.016 | 71.32 | 115.86 | 0.002 |
To assess whether the prognostic value of Livin or
PlGF was attributable to prognosis, Cox's regression analysis was
performed with all variables including Livin expression, PlGF
expression, Livin and PlGF expression, age at diagnosis, tumor
stage (low stages IB-IIA vs. advanced stages IIB-III), and tumor
size. Univariate analysis revealed that pathological stage and
tumor diameter were significant factors influencing the OS time of
patients with osteosarcoma. The OS time in patients with stages
IB-IIA and a tumor diameter ≤5 cm was significantly increased,
compared with that of patients with stages IIB-III and a tumor
diameter >5 cm. Patients exhibiting low Livin and PlGF
expression had a markedly longer OS time when compared with that of
patients with high Livin and PlGF expression. No significant
differences in OS time were observed in any other
clinicopathological parameters, including sex, age and tumor
site.
Factors that demonstrated prognostic significance by
univariate analysis were subsequently examined in a multivariate
analysis. A poor OS was identified in patients with high expression
of Livin [P=0.023; hazard ratio (HR), 0.274; 95% confidence
interval (CI), 0.089–0.839] and PlGF (P=0.014; HR, 0.209; 95% CI,
0.060–0.728) (P=0.001; HR, 0.193; 95% CI, 0.094–0.511 for Livin and
PlGF) (Table III). These results
suggested that high Livin and PlGF expression are independent
prognostic factor for OS in patients with osteosarcoma.
 | Table III.Multivariate analysis of Livin and
PlGF expression for the prognosis of osteosarcoma. |
Table III.
Multivariate analysis of Livin and
PlGF expression for the prognosis of osteosarcoma.
| Variables | HR | P-value | 95% CI |
|---|
| Livin high
expression | 0.274 | 0.023 | 0.089–0.839 |
| PlGF high
expression | 0.209 | 0.014 | 0.060–0.728 |
| Livin and PlGF high
expression | 0.001 | 0.193 | 0.094–0.511 |
Discussion
With the development of neoadjuvant chemotherapy,
the long-term survival of patients with osteosarcoma of the
extremity without metastatic disease has improved from 10–15% to
50–70% (18). However, patients with
metastatic disease at diagnosis exhibit a poor prognosis due to
chemotherapy resistance. Resistance to chemotherapy is a hallmark
of osteosarcoma (19). The reduction
of anti-apoptotic factors may provide a rational basis for the
development of novel therapeutic strategies target in cancer
osteosarcoma (20). IAPs are the only
known endogenous proteins that regulate the activity of initiator
and effector caspases (21).
Overexpression of XIAP and survivin has been identified in
osteosarcoma, indicating that IAP-mediated inhibition of apoptosis
may participate in tumorigenesis (21). Livin is one of the novel human IAP
family members, which was first described in melanoma. It has been
demonstrated that Livin was expressed in a number of types of tumor
cell and several fetal tissues, but not in normal adult tissues.
Livin is not detectable in the majority of types of normal
differentiated tissue, with the exception of the placenta, testes,
spinal cord and lymph node; however, it is present in a number of
types of cancer including carcinomas of the breast and prostate,
osteosarcoma, melanoma and lymphoma cells (21).
A previous study revealed that Livin antagonized the
death receptor and mitochondria-based apoptosis signaling pathways
via the inhibition of downstream caspases including caspase-3,
caspase-7 and caspase-9, leading to their inactivation and
degradation (22). The anti-apoptotic
potential of Livin and its preferential expression in osteosarcoma,
at very low or undetectable levels in the corresponding normal
tissue, suggest that the manipulation of Livin expression could
represent a novel and tumor-specific molecular target for cancer
therapy (23). Zhuang et al
(24) demonstrated that long-term
silencing of Livin expression inhibited the proliferation of
Livin-expressing non small-cell lung cancer cells and increased the
chemosensitivity of NSCLC cells.
Consistent with a previous study (25), the results of the present study
identified that a substantial proportion of primary osteosarcoma
tissues expressed Livin (58.3%) and the positive expression of
Livin was significantly associated with advanced staged
osteosarcoma. In the present study, the expression levels of Livin
in the osteosarcoma specimens were significantly increased,
compared with those in normal bone tissue. The high expression of
Livin was significantly associated with OS, clinical Enneking stage
and tumor diameter, but not with other clinicopathological factors.
Livin expression levels in patients exhibiting stages I–IIA were
significantly decreased, compared with those in patients exhibiting
stages IIB-III. In addition, analysis of the 5-year OS rate
identified a significant difference between patients with
osteosarcoma in the Livin positive-expression group and patients
who did not express Livin. Livin was primarily identified as a
granular pattern in the cytoplasm in the present study.
Additionally, the gene expression of Livin was determined in three
different osteosarcoma cell lines (SaOS-2, MG-63 and U2OS) and
identified to be increased in MG-63 cells, compared with that in
the two other cell lines. Therefore, the results of the present
study demonstrated that Livin may serve a function in osteosarcoma
development, which is similar to the findings of a previous report,
which identified the function of Livin in other types of malignancy
(26).
A previous study demonstrated that angiogenesis
serves a key function in cancer growth, and was regarded as a
marker for invasiveness and metastasis in osteosarcoma (27). VEGF has been extensively studied and
is considered to be the most important pro-angiogenic factor in
osteosarcoma (28). PlGF, which
exhibits 42% amino acid sequence identity with VEGF, was initially
cloned from the placenta and cooperated with VEGF in the formation
of vasculature (29). A previous
study has demonstrated the prognostic implication of high PlGF
expression in a number of types of cancer (30). PlGF serves a key function in tumor
angiogenesis by affecting endothelial cells via VEGF receptor
(VEGFR)-1 (31). Actions of PIGF in
tumor angiogenesis include the following: Separating VEGF from
VEGFR-1, enabling VEGF to activate VEGFR-2; acting as a stimulator
via binding to VEGFR-1, which in turn would increase cell
sensitivity to VEGF acting via VEGFR-2; recruiting
monocytes/macrophages, which affects vessel growth; and mobilizing
hematopoietic progenitor cells from the bone marrow (31). Previous studies have demonstrated that
increased PlGF expression was associated with tumor progression and
the invasiveness of cancer cells was inhibited by the anti-PlGF
antibody (32,33). However, the level of PlGF protein
expression and its significance in osteosarcoma remain unknown.
To the best or our knowledge, the present study was
the first study to quantitate the PlGF expression in human
osteosarcoma tissues and cell lines in order to evaluate the
association between PlGF expression and the prognosis of
osteosarcoma. The results of the present study revealed that
positive expression of PlGF is significantly associated with
advanced tumor stage and a tumor diameter >5 cm. Increased
expression of PlGF was observed in advanced stage osteosarcoma,
compared with that in early stage osteosarcoma, and high PIGF
expression was indicative of a poor prognosis for the patient. The
results of the present study validated that PlGF was significantly
upregulated in osteosarcoma specimens, compared with that in normal
bone tissues. In addition, the association between PlGF and
prognosis was of increased significance in stage IIB-III patients,
compared with that in stage IB-IIA patients. The results of the
present study indicated that PlGF may not be involved in the early
development and growth of osteosarcoma. The effect of Livin and
PlGF expression was additionally studied in three human
osteosarcoma cell lines. MG-63, an osteoblast-derived osteosarcoma
cell line derived from a 14-year-old Caucasian male, is considered
to be representative of osteoblast precursors or early
undifferentiated osteoblast-like cells (34). SaOS-2 is a non-transformed
osteoblast-like cell line derived from the primary osteosarcoma of
an 11-year-old Caucasian female (35)
and U2OS was derived from a moderately differentiated sarcoma of
the tibia of a 15-year-old female (36). The expression levels of Livin and PlGF
in MG-63 cells were markedly increased, compared with those in U2OS
and SaOS-2 cell lines; this result may be because MG-63 cells are
phenotypically more differentiated than U2OS and SaOS-2 cells
(37,38). Therefore, it has been suggested by the
present study that PlGF may serve a function in the rapid
restoration of tumor blood supply following treatment and thus may
enhance the possibility of cancer recurrence. PlGF may be a
therapeutic target in patients with cancer recurrence.
The present study has demonstrated that Livin is
positively expressed in osteosarcoma and may be an important
prognostic marker for the survival of patients with osteosarcoma.
In addition, the results of the present study revealed that
increased levels of PlGF are significantly associated with poorly
differentiated osteosarcoma and a poor outcome for the patient.
Anti-angiogenic therapy exhibits potential in combination with
conventional chemotherapy for patients with osteosarcoma and
additional studies are required to validate this. Therefore, the
present study identified that Livin and PlGF may be potential
treatment targets for human osteosarcoma. However, as the size of
the present sample is limited, additional validation is
required.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant no. 81660443), the
Natural Science Foundation of Jiangxi Province (grant no.
20122BBG70107-3) and the Foundation of Shanghai Health Bureau
(grant no. 2010061).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
KS conducted the molecular genetic studies,
participated in the sequence alignment performed the statistical
analysis and drafted the manuscript. ZC performed the immunoassays.
TC participated in the design of the study. JZ and QL conceived the
study, participated in its design and coordination and assisted in
drafting the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the ethical
committee of Zhongshan Hospital, Fudan University and had been
performed in accordance with the ethical standards laid down in the
1964 Declaration of Helsinki. Due to the present study being
retrospective, the ethics committee specifically approved that not
informed consent was required due to data being analyzed
anonymously; therefore, informed consent was not required, but the
patients or their guardians signed in informed consent for the
surgery.
Patient consent for publication
All of the patients or their guardians signed
informed consent for the publication of the present study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Pruksakorn D, Phanphaisarn A, Pongnikorn
D, Daoprasert K, Teeyakasem P, Chaiyawat P, Katruang N and
Settakorn J: Age standardized incidence rates and survival of
osteosarcoma in northern thailand. Asian Pac J Cancer Prev.
17:3455–3458. 2016.PubMed/NCBI
|
|
2
|
Aznab M and Hematti M: Evaluation of
clinical process in osteosarcoma patients treated with chemotherapy
including cisplatin, adriamycin, ifosfamide, and etoposide and
determination of the treatment sequels in a long-term 11-year
follow-up. J Cancer Res Ther. 13:291–296. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
PosthumaDeBoer J, Witlox MA, Kaspers GJ
and van Royen BJ: Molecular alterations as target for therapy in
metastatic osteosarcoma: A review of literature. Clin Exp
Metastasis. 28:493–503. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Du MD, He KY, Qin G, Chen J and Li JY:
Adriamycin resistance-associated prohibitin gene inhibits
proliferation of human osteosarcoma MG63 cells by interacting with
oncogenes and tumor suppressor genes. Oncol Lett. 12:1994–2000.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yoon TM, Kim SA, Lee DH, Lee JK, Park YL,
Lee KH, Chung IJ, Joo YE and Lim SC: Livin enhances chemoresistance
in head and neck squamous cell carcinoma. Oncol Rep. 37:3667–3673.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Li CJ, Cong Y, Liu XZ, Zhou X, Shi X, Wu
SJ, Zhou GX and Lu M: Research progress on the livin gene and
osteosarcomas. Asian Pac J Cancer Prev. 15:8577–8579. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hou Q, Li MY, Huang WT, Wei FF, Peng JP,
Lou MW and Qiu JG: Association between three VEGF polymorphisms and
renal cell carcinoma susceptibility: A meta-analysis. Oncotarget.
8:50061–50070. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liang L, Yue Z, Du W, Li Y, Tao H, Wang D,
Wang R, Huang Z, He N, Xie X, et al: Molecular imaging of inducible
VEGF expression and tumor progression in a breast cancer model.
Cell Physiol Biochem. 42:407–415. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yan B, Kong M, Chen S and Chen YH: VEGF
stimulation enhances Livin protein synthesis through mTOR
signaling. J Cell Biochem. 111:1114–1124. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen L, Ren GS, Li F and Sun SQ:
Expression of livin and vascular endothelial growth factor in
different clinical stages of human esophageal carcinoma. World J
Gastroenterol. 14:5749–5754. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pagani E, Ruffini F, Cappellini Antonini
GC, Scoppola A, Fortes C, Marchetti P, Graziani G, D'Atri S and
Lacal PM: Placenta growth factor and neuropilin-1 collaborate in
promoting melanoma aggressiveness. Int J Oncol. 48:1581–1589. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Babkina IV, Osipov DA, Solovyov YN,
Bulycheva IV, Machak GN, Aliev MD and Kushlinsky NE: Endostatin,
placental growth factor, and fibroblast growth factors-1 and −2 in
the sera of patients with primary osteosarcomas. Bull Exp Biol Med.
148:246–249. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Marrony S, Bassilana F, Seuwen K and
Keller H: Bone morphogenetic protein 2 induces placental growth
factor in mesenchymal stem cells. Bone. 33:426–433. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mahmoodi F and Akrami H: PlGF knockdown
decreases tumorigenicity and stemness properties of spheroid body
cells derived from gastric cancer cells. J Cell Biochem.
118:851–859. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Incio J, Tam J, Rahbari NN, Suboj P,
McManus DT, Chin SM, Vardam TD, Batista A, Babykutty S, Jung K, et
al: PlGF/VEGFR-1 signaling promotes macrophage polarization and
accelerated tumor progression in obesity. Clin Cancer Res.
22:2993–3004. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Enneking WF, Spanier SS and Goodman MA: A
system for the surgical staging of musculoskeletal sarcoma. Clin
Orthop Relat Res. 106–120. 1980.PubMed/NCBI
|
|
17
|
Kawasaki H, Altieri DC, Lu CD, Toyoda M,
Tenjo T and Tanigawa N: Inhibition of apoptosis by survivin
predicts shorter survival rates in colorectal cancer. Cancer Res.
58:5071–5074. 1998.PubMed/NCBI
|
|
18
|
Wang YF, Shen JN, Xie XB, Wang J and Huang
G: Expression change of ezrin as a prognostic factor in primary
osteosarcoma. Med Oncol. 28 Suppl 1:S636–S643. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sampson VB, Vetter NS, Zhang W, Patil PU,
Mason RW, George E, Gorlick R and Kolb EA: Integrating mechanisms
of response and resistance against the tubulin binding agent
Eribulin in preclinical models of osteosarcoma. Oncotarget.
7:86594–86607. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Horie R, Nakamura O, Yamagami Y, Mori M,
Nishimura H, Fukuoka N and Yamamoto T: Apoptosis and antitumor
effects induced by the combination of an mTOR inhibitor and an
autophagy inhibitor in human osteosarcoma MG63 cells. Int J Oncol.
48:37–44. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Saleem M, Qadir MI, Perveen N and Ahmad B,
Saleem U, Irshad T and Ahmad B: Inhibitors of apoptotic proteins:
New targets for anticancer therapy. Chem Biol Drug Des. 82:243–251.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Liu GH, Wang C and Ding ZY: Overexpression
of the truncated form of Livin reveals a complex interaction with
caspase-3. Int J Oncol. 42:2037–2045. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lin X, Li HR, Lin XF, Yu ME, Tu XW, Hua
ZD, Lin M, Xu NL, Han LL and Chen YS: Silencing of Livin inhibits
tumorigenesis and metastasis via VEGF and MMPs pathway in lung
cancer. Int J Oncol. 47:657–667. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhuang L, Shen LD, Li K, Yang RX, Zhang
QY, Chen Y, Gao CL, Dong C, Bi Q, Tao JN, et al: Inhibition of
livin expression suppresses cell proliferation and enhances
chemosensitivity to cisplatin in human lung adenocarcinoma cells.
Mol Med Rep. 12:547–552. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Nedelcu T, Kubista B, Koller A, Sulzbacher
I, Mosberger I, Arrich F, Trieb K, Kotz R and Toma CD: Livin and
Bcl-2 expression in high-grade osteosarcoma. J Cancer Res Clin
Oncol. 134:237–244. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Guan HP, Sun JZ, Feng XL, Chen JS, Chen
FJ, Cheng XF, Liu XW and Ni B: Effects of RNA interference-mediated
knockdown of livin and survivin using monomethoxypolyethylene
glycol-chitosan nanoparticles in MG-63 osteosarcoma cells. Mol Med
Rep. 13:1821–1826. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ségaliny AI, Mohamadi A, Dizier B,
Lokajczyk A, Brion R, Lanel R, Amiaud J, Charrier C, Boisson-Vidal
C and Heymann D: Interleukin-34 promotes tumor progression and
metastatic process in osteosarcoma through induction of
angiogenesis and macrophage recruitment. Int J Cancer. 137:73–85.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Liu JQ, Bai X, Duan DC and Dou AX: Role of
five small nucleotide polymorphisms in the VEGF gene on the
susceptibility to osteosarcoma and overall survival of patients.
Oncol Lett. 10:1481–1486. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Autiero M, Waltenberger J, Communi D,
Kranz A, Moons L, Lambrechts D, Kroll J, Plaisance S, De Mol M,
Bono F, et al: Role of PlGF in the intra- and intermolecular cross
talk between the VEGF receptors Flt1 and Flk1. Nat Med. 9:936–943.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ribatti D: The discovery of the placental
growth factor and its role in angiogenesis: A historical review.
Angiogenesis. 11:215–221. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Fischer C, Jonckx B, Mazzone M, Zacchigna
S, Loges S, Pattarini L, Chorianopoulos E, Liesenborghs L, Koch M,
De Mol M, et al: Anti-PlGF inhibits growth of VEGF(R)-inhibitor
resistant tumors without affecting healthy vessels. Cell.
131:463–475. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Meng FJ, Xiao SX, Zhang Y, Wang W, Wang B
and Fan XY: Prognostic significance of placenta growth factor
expression in patients with multiple cancers: A meta-analysis. Int
J Clin Exp Med. 8:12726–12735. 2015.PubMed/NCBI
|
|
33
|
Taylor AP and Goldenberg DM: Role of
placenta growth factor in malignancy and evidence that an
antagonistic PlGF/Flt-1 peptide inhibits the growth and metastasis
of human breast cancer xenografts. Mol Cancer Ther. 6:524–531.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Clover J and Gowen M: Are MG-63 and HOS
TE85 human osteosarcoma cell lines representative models of the
osteoblastic phenotype? Bone. 15:585–591. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Fogh J, Wright WC and Loveless JD: Absence
of HeLa cell contamination in 169 cell lines derived from human
tumors. J Natl Cancer Inst. 58:209–214. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Pontén J and Saksela E: Two established in
vitro cell lines from human mesenchymal tumours. Int J Cancer.
2:434–447. 1967. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Lisignoli G, Toneguzzi S, Cattini L, Pozzi
C and Facchini A: Different expression pattern of cytokine
receptors by human osteosarcoma cell lines. Int J Oncol.
12:899–903. 1998.PubMed/NCBI
|
|
38
|
Cifuentes M, García MA, Arrabal PM,
Martínez F, Yañez MJ, Jara N, Weil B, Domínguez D, Medina RA and
Nualart F: Insulin regulates GLUT1-mediated glucose transport in
MG-63 human osteosarcoma cells. J Cell Physiol. 226:1425–1432.
2011. View Article : Google Scholar : PubMed/NCBI
|