Introduction
As the largest endocrine organ in the human body,
thyroid plays an important role in regulating the metabolic process
of human body (1). Thyroid nodule
(TN), is the most common thyroid disease in clinical practice. TN
is a disease caused by abnormal growth of thyroid follicles in
patients, most of which are benign lesions such as goiter and
thyroid adenoma, but TN can also lead to malignant lesions such as
thyroid carcinoma and lymphoma (2,3). It has
been reported (4) that the main
reason for the significant increase of the incidence of thyroid
cancer in the past 30 years is that there are no obvious clinical
manifestations before the onset of thyroid cancer and it is very
easy to have missed diagnosis. After thyroidectomy, the impairment
of body function is accompanied by a variety of complications,
which has a serious impact on the quality of life and safety of
patients (5). Therefore, the
diagnosis and differentiation of TN is particularly important.
There was a survey showing (6) that the diagnosis rate of diagnosing TN
patients was <10% in clinical palpation, but the detection rate
of TN patients could be significantly improved by imaging
examination. At present, the diagnosis of TN is mainly
ultrasound-guided fine needle puncture, but the hardness of lesion
tissue cannot be obtained by ultrasound imaging, while ultrasound
elastography makes up for this defect, and it is being popularized
to clinic gradually (7,8).
The present study aimed to find a better diagnostic
method and to provide reference for clinical practice by comparing
the difference between ultrasound-guided fine needle puncture and
elastic ultrasound in the diagnosis of TN.
Patients and methods
In the present study, 194 patients with TN, admitted
from June 2014 to June 2015, were selected to be treated with
ultrasound elastography and ultrasound-guided fine needle puncture
biopsy and all patients had definite diagnosis after surgical or
ultrasound follow-up for 12 months. Among the 194 patients, 79 were
male and 115 were female, and the age of the patients was 29–64
years, with an average age of 44.95±6.82 years. The benign nodules
were 129 and the malignant nodules were 88. The clinical data are
shown in Table I. This study was
approved by the Medical Ethics Committee of Liaocheng People's
Hospital (Liaocheng, China) and all patients and their families
were informed and signed the informed consent.
 | Table I.Clinical data of patients. |
Table I.
Clinical data of patients.
| Groups | Clinical information
(n) |
|---|
| Sex |
|
| Male | 79 |
|
Female | 115 |
| Age (years) |
|
|
>45 | 105 |
| ≤45 | 89 |
| Benign lesion
(n=129) |
|
|
Adenomatous goiter | 82 |
|
Follicular adenoma | 25 |
|
Proliferative nodule | 22 |
| Malignant lesion
(n=88) |
|
| Papillary
thyroid carcinoma | 81 |
|
Follicular thyroid
carcinoma | 6 |
| Medullary
carcinoma | 1 |
Inclusion and exclusion criteria
Inclusion criteria: The patient was older than 18
years. The pathological diagnosis of TN after operation was clear
and the size and location of the lesion could be described in
detail. The course of the disease was half a year, and there was no
recent drug treatment and no other hereditary diseases.
Exclusion criteria: Respiratory diseases, blood
relationship between patients, no recent blood transfusion
treatment, uncoordinated follow-up and incomplete clinical
information.
Detection methods
Ultrasound elastography
In this experiment, Hi Vision Ascendus (Hitachi
color ultrasound diagnostic instrument; Hitachi, Ltd., Tokyo,
Japan) was used to detect 194 patients, and real-time elastic
ultrasonic detection was performed on patients with real-time
linear array high-frequency probe, with a probe frequency of 6–13
MHz. The patient presented supine position and exposed the neck.
The diameter, shape, perimeter, and blood supply of the thyroid
gland were detected by conventional ultrasound. Then, ultrasound
elastography was used to detect the lesion and the vertical
pressure was placed at the lesion. The pressure was adjusted to the
range of 3–4 and the obtained images were observed (9). The ratings are shown in Table II. In this study, the patients with 1
and 2 score of elasticity were classified as benign nodules and
those with elastic score >3 were classified as malignant nodules
(10).
 | Table II.Elastic ultrasound ratings. |
Table II.
Elastic ultrasound ratings.
| Ratings | Standards |
|---|
| 1 point | The nodules and
surrounding tissues are green |
| 2 points | The nodules were
mixed with blue and green, but mostly green |
| 3 points | The nodules were
mixed with blue and green, but mostly blue |
| 4 points | The nodule is
blue |
| 5 points | The nodules and
surrounding tissues are blue |
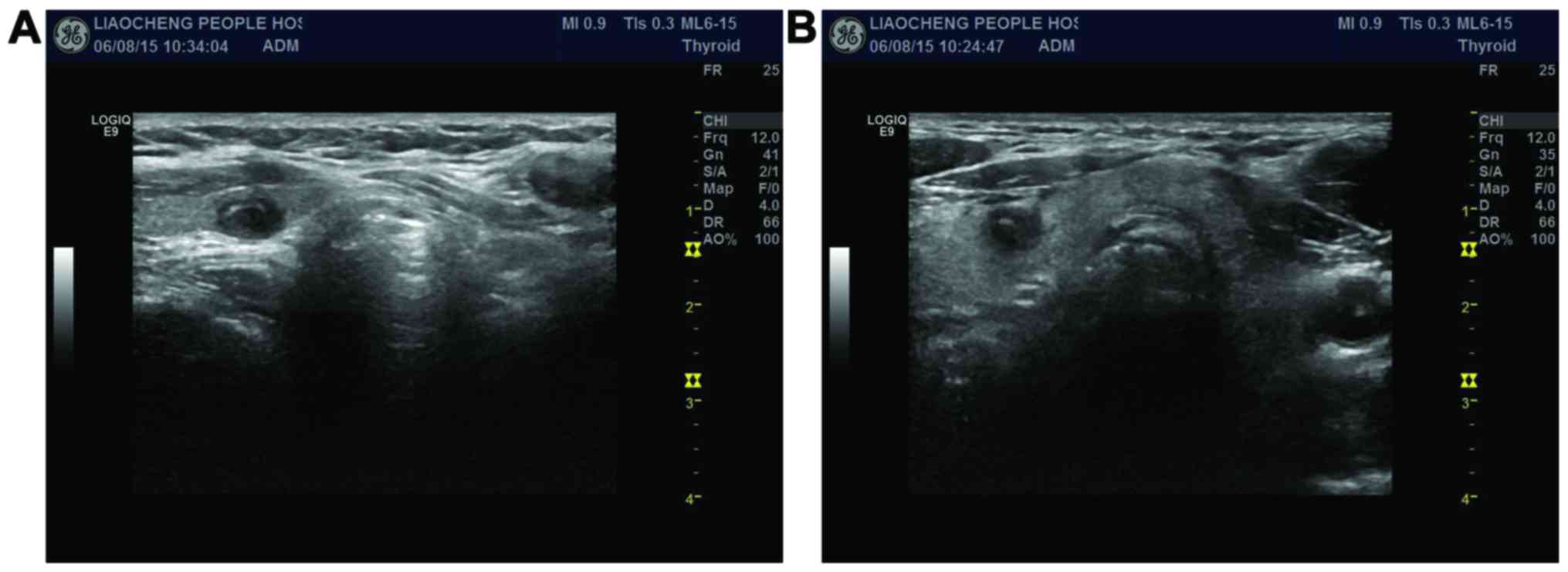
Ultrasound-guided fine needle
puncture
In the present study, 16G automatic biopsy needle
was used for ultrasound-guided puncture performed on patients. The
patient presented supine position and exposed the neck. Routine
disinfection was done and towels were held. The fixed converter was
adjusted and fixed, the lesion was placed in the center of
ultrasound image and the direction of the needle was inclined along
the scanning plane. When the puncture reached the location of the
lesion, the tissue of the lesion was sucked and biopsy was carried
out. Results of cytological test referred to the literature
(11): Benign: cytological detection
was benign; malignant: cytological detection was malignant;
uncertain: uncertain, suspicious as malignant nodules. An image of
ultrasound puncture is shown in Fig.
1.
Statistical method. In this experiment, SPSS 20.0
statistical software package (IBM Corp., Armonk, NY, USA) was used
to analyze the collected data, and GraphPad software was used to
draw the histogram. The sensitivity was equal to true malignancy
divided by pathological diagnosis of malignancy, the specificity
was equal to true benign divided by pathologic diagnosis of benign,
and the accuracy was equal to true malignancy plus true benign and
then divided by total number of nodules. The counting data were
expressed by rate (%), and analyzed by the Chi-square test.
P<0.05, was considered as statistically significant.
Results
Diagnostic results of the two
methods
In this study, 194 patients were detected and it was
found that the number of nodules diagnosed through surgical or
ultrasound follow-up for 12 months was 217, including 129 benign
nodules and 88 malignant nodules. Through ultrasound elastography,
it was diagnosed that there were 75 benign nodules and 142
malignant nodules, and through ultrasound-guided puncture, it was
diagnosed that there were 112 benign nodules, 78 malignant nodules
and 27 uncertain nodules (Tables
III and IV).
 | Table III.Results of ultrasound imaging. |
Table III.
Results of ultrasound imaging.
|
| Results of ultrasonic
diagnosis |
|
|---|
|
|
|
|
|---|
| Results of
pathological diagnosis | Malignant | Benign | Total |
|---|
| Malignant | 61 | 48 | 109 |
| Benign | 81 | 27 | 108 |
| Total | 142 | 75 | 217 |
 | Table IV.Results of ultrasound-guided
puncture. |
Table IV.
Results of ultrasound-guided
puncture.
|
| Results of
ultrasound-guided puncture |
|
|---|
|
|
|
|
|---|
| Results of
pathological diagnosis | Malignant | Benign | Uncertain | Total |
|---|
| Malignant | 57 | 4 | 27 | 88 |
| Benign | 21 | 108 | 0 | 129 |
| Total | 78 | 112 | 27 | 217 |
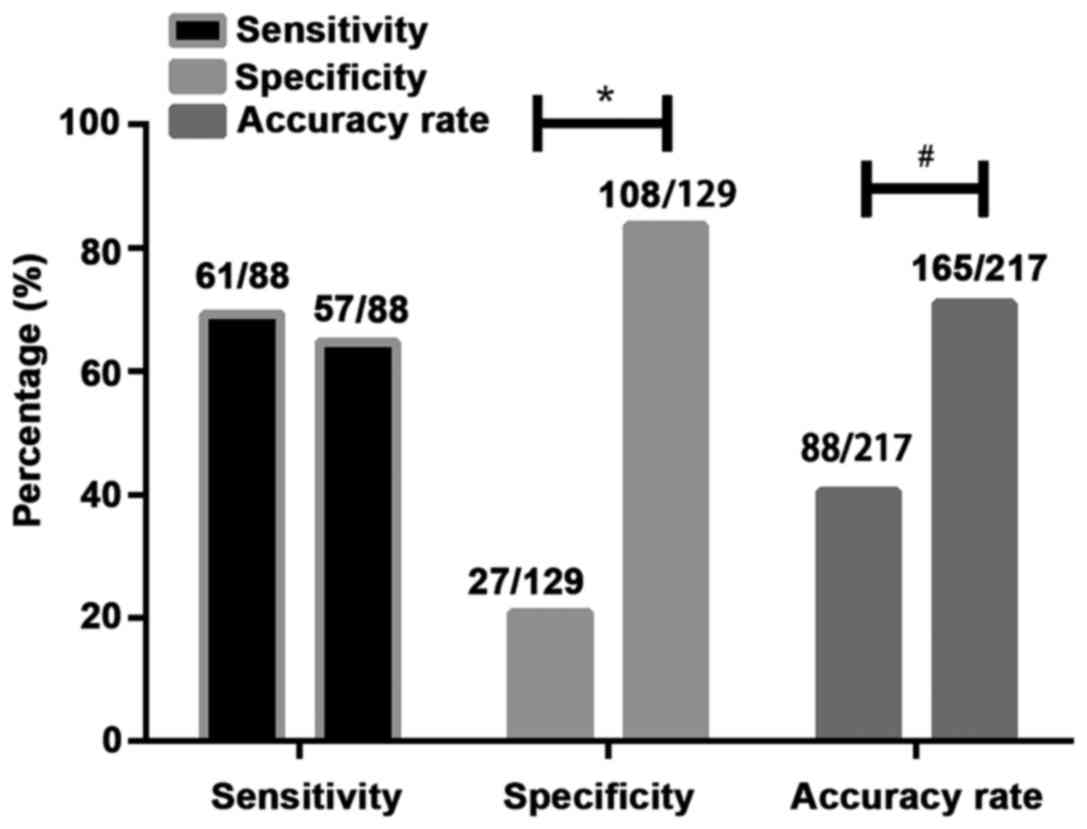
Comparison of diagnostic values of the
two methods
Through the calculation of the sensitivity,
specificity and accuracy by the two detection methods, it was found
that there was no statistically significant difference (P>0.05)
between the sensitivity of ultrasound elastography (69.32%) and
that of ultrasound-guided fine needle puncture (64.77%). By
contrasting the specificity of ultrasound elastography, it was
found that there was a significant difference (P<0.05) between
the specificity of ultrasound elastography (20.93%) and that of
ultrasound-guided fine needle puncture (83.7%). Besides, through
the calculation of accuracy, it was found that the accuracy of
ultrasound elastography (40.55%) was significantly lower than that
of ultrasound-guided fine needle puncture (76.04%; P<0.05)
(Fig. 2).
Discussion
Nowadays, TN is a common endocrine system disease in
clinic. There was a survey showing that the incidence of TN was
only 4–8% and the incidence of malignant lesions was <1%, while
the diagnostic rate of TN was very unsatisfactory (12). Statistics showed (13) that the diagnostic rate of TN before
clinical operation was ≤50%, and most of the patients were found to
be middle and late stage after diagnosis, which brought great
difficulties to the treatment and prognosis of the patients.
Therefore, the early diagnosis of TN plays a very important guiding
role in clinical treatment. At present, with the increasing
awareness of self-protection and safety of the masses, a large
number of people conduct regular physical examination every year,
and thyroid detection has been paid more and more attention.
The diagnosis of TN is mainly based on ultrasound
and palpation puncture and the advantages and disadvantages of
palpation puncture are obvious. The failure rate of puncture is
high and it is difficult to obtain materials for degenerative and
small nodules, which leads to the failure of the later examination
(14). The traditional grayscale
supergrowth and color Doppler ultrasound have a good judgment on
the tissue morphology, the perimeter, the internal echo of the
tissue, the blood flow in and around the tissue and the
calcification of the tissue, but the hardness of the tissue cannot
be judged very well (15). Ultrasound
elastography is an ultrasound imaging method first proposed by
scholar Ophir et al (16).
Ultrasound elastography is to compare the difference of elastic
coefficient between different tissues and after compression by
external force, the tissue changes in different forms. The
amplitude of signal movement before and after compression is
contrasted and transformed into a real-time image, so as to judge
the hardness of the tissue through it. The greater the hardness is,
the higher the degree of malignancy is, and vice versa (17).
In this study, through the diagnosis of TN patients
by ultrasound elastography, it was found that the sensitivity of
ultrasound elastography was 69.32%, which was slightly higher than
that of ultrasound-guided puncture (64.77%), but there was no
statistically significant difference. However, in the study of Li
et al (18), the accuracy of
detecting TN by ultrasound elastography was as high as 92.5%
(74/80), which was very different from our study, and we speculated
that it might be caused by the differences of equipment. Compared
with ultrasound-guided puncture, the specificity and accuracy were
significantly lower, which might be due to the internal hemorrhage,
necrosis and calcification in some benign TN, so that the hardness
of tissue increased, resulting in a lot of false-positive results
(19). When TN diameter was >3 cm
and at the lower pole position, the detection results would also be
affected, leading to the diagnosis deviation (20). Compared with palpation-guided puncture
biopsy, ultrasound-guided high-frequency puncture had obvious
advantages. First of all, the depth and the orientation of the
needle were more clearly grasped. Secondly, the ultrasound-guided
puncture wound was smaller, faster and safer, and the failure rate
could be reduced and the efficiency could be improved through
ultrasound guidance (21). In this
experiment, the results of ultrasound-guided puncture in the
diagnosis of TN showed that the sensitivity, specificity and
accuracy of puncture TN under ultrasound guidance were satisfactory
and the specificity and accuracy were significantly higher than
that of ultrasound elastography. Nevertheless, in the case of
multiple advantages, ultrasound-guided puncture is still an
invasive detection method. If the patient has small nodules and
more lesions, it may result in limited safety during the
examination. Moreover, the ultrasound-guided fine needle puncture
will have a small number of sucked cells, and the small number of
sucked cells will result in unsatisfactory results under
post-staining microscope (22). We
speculated that in this ultrasound-guided fine needle puncture,
uncertain patients might be the result of a small number of sucked
cells. Both methods had advantages and disadvantages. Through
consulting the literature, it was found (23,24) that
the detection rate of TN could be improved by ultrasound
elastography combined with ultrasound-guided puncture and the
screening of patients by ultrasound elastography could reduce the
number of puncture and false-positive results and increase the
early diagnosis rate.
However, there are still some limitations in this
study. First of all, this experiment is a retrospective analysis,
lacking contrast. Secondly, the sample size is small, which may be
one of the reasons for the deviation of the results of this study.
Therefore, we hope to increase the number of samples in future
studies and to establish a randomized controlled trial to verify
the correctness of the results of this study.
In summary, ultrasound elastography and
ultrasound-guided fine needle puncture biopsy may lead to different
results, and there are some limitations in a single diagnostic
scheme. Therefore, the two diagnostic schemes need to be combined
to complement each other so as to improve the early diagnosis of
TN.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XP drafted the manuscript. XP and LW performed the
ultrasound elastography and needle puncture. Both authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Liaocheng People's Hospital (Liaocheng, China). Signed informed
consents were obtained from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Tuttle RM, Haugen B and Perrier ND:
Updated American Joint Committee on Cancer/tumor-node-metastasis
staging system for differentiated and anaplastic thyroid cancer
(eighth edition): What changed and why? Thyroid. 27:751–756. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Parsa AA and Gharib H: History and
examination for thyroid nodulesThyroid Nodules. Gharib H: 1st.
Humana Press; Cham: pp. 13–18. 2018, View Article : Google Scholar
|
|
3
|
Alexander EK, Kennedy GC, Baloch ZW, Cibas
ES, Chudova D, Diggans J, Friedman L, Kloos RT, LiVolsi VA, Mandel
SJ, et al: Preoperative diagnosis of benign thyroid nodules with
indeterminate cytology. N Engl J Med. 367:705–715. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lim H, Devesa SS, Sosa JA, Check D and
Kitahara CM: Trends in thyroid cancer incidence and mortality in
the United States, 1974–2013. JAMA. 317:1338–1348. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lee JC, Grodski S, Yeung M and Serpell J:
Response to the letter to the editor regarding ‘Quantitative study
of voice dysfunction after thyroidectomy’. Surgery. 162:692–693.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Paschke R, Cantara S, Crescenzi A, Jarzab
B, Musholt TJ and Sobrinho Simoes M: European Thyroid Association
guidelines regarding thyroid nodule molecular fine-needle
aspiration cytology diagnostics. Eur Thyroid J. 6:115–129. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Middleton WD, Teefey SA, Reading CC,
Langer JE, Beland MD, Szabunio MM and Desser TS: Multiinstitutional
analysis of thyroid nodule risk stratification using the American
College of Radiology Thyroid Imaging Reporting and Data System. AJR
Am J Roentgenol. 208:1331–1341. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Seo H, Na DG, Kim JH, Kim KW and Yoon JW:
Ultrasound-based risk stratification for malignancy in thyroid
nodules: A four-tier categorization system. Eur Radiol.
25:2153–2162. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bae JM, Hahn SY, Shin JH and Ko EY:
Inter-exam agreement and diagnostic performance of the Korean
thyroid imaging reporting and data system for thyroid nodule
assessment: Real-time versus static ultrasonography. Eur J Radiol.
98:14–19. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hong Y, Liu X, Li Z, Zhang X, Chen M and
Luo Z: Real-time ultrasound elastography in the differential
diagnosis of benign and malignant thyroid nodules. J Ultrasound
Med. 28:861–867. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Singh Ospina N, Maraka S, Espinosa DeYcaza
A, O'Keeffe D, Brito JP, Gionfriddo MR, Castro MR, Morris JC, Erwin
P and Montori VM: Diagnostic accuracy of thyroid nodule growth to
predict malignancy in thyroid nodules with benign cytology:
Systematic review and meta-analysis. Clin Endocrinol (Oxf).
85:122–131. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lee YH, Baek JH, Jung SL, Kwak JY, Kim JH
and Shin JH; Korean Society of Thyroid Radiology (KSThR), ; Korean
Society of Radiology, : Ultrasound-guided fine needle aspiration of
thyroid nodules: A consensus statement by the Korean Society of
Thyroid Radiology. Korean J Radiol. 16:391–401. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Haugen BR, Alexander EK, Bible KC, Doherty
GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM,
Schlumberger M, et al: 2015 American Thyroid Association management
guidelines for adult patients with thyroid nodules and
differentiated thyroid cancer: The American Thyroid Association
guidelines task force on thyroid nodules and differentiated thyroid
cancer. Thyroid. 26:1–133. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Carneiro-Pla D: Thyroid nodule
biopsyManagement of Thyroid Nodules and Differentiated Thyroid
Cancer. Roman SA, Sosa JA and Solórzano CC: 1st. Springer
International Publishing; Cham: pp. 47–58. 2017, View Article : Google Scholar
|
|
15
|
Ma JJ, Ding H, Xu BH, Xu C, Song LJ, Huang
BJ and Wang WP: Diagnostic performances of various gray-scale,
color Doppler, and contrast-enhanced ultrasonography findings in
predicting malignant thyroid nodules. Thyroid. 24:355–363. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ophir J, Céspedes I, Ponnekanti H, Yazdi Y
and Li X: Elastography: A quantitative method for imaging the
elasticity of biological tissues. Ultrason Imaging. 13:111–134.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Marticorena Garcia SR, Guo J, Dürr M,
Denecke T, Hamm B, Sack I and Fischer T: Comparison of ultrasound
shear wave elastography with magnetic resonance elastography and
renal microvascular flow in the assessment of chronic renal
allograft dysfunction. Acta Radiol. Jan 1–2017.(Epub ahead of
print). View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li F, Zhang J, Wang Y and Liu L: Clinical
value of elasticity imaging and contrast-enhanced ultrasound in the
diagnosis of papillary thyroid microcarcinoma. Oncol Lett.
10:1371–1377. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Russ G: Risk stratification of thyroid
nodules on ultrasonography with the French TI-RADS: Description and
reflections. Ultrasonography. 35:25–38. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dudea SM and Botar-Jid C: Ultrasound
elastography in thyroid disease. Med Ultrason. 17:74–96. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Levine RA and Interlandi J: The procedure
of ultrasound-guided percutaneous biopsy of thyroid and cervical
lymph nodes: Technical steps, pitfalls, and pearlsAdvanced Thyroid
and Parathyroid Ultrasound. Milas M, Mandel S and Langer JE: 1st.
Springer International Publishing; Cham: pp. 309–321. 2017,
View Article : Google Scholar
|
|
22
|
Kim H, Kim JA, Son EJ and Youk JH:
Quantitative assessment of shear-wave ultrasound elastography in
thyroid nodules: Diagnostic performance for predicting malignancy.
Eur Radiol. 23:2532–2537. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Giovannini M, Thomas B, Erwan B, Christian
P, Fabrice C, Benjamin E, Geneviève M, Paolo A, Pierre D, Robert Y,
et al: Endoscopic ultrasound elastography for evaluation of lymph
nodes and pancreatic masses: A multicenter study. World J
Gastroenterol. 15:1587–1593. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Monpeyssen H, Tramalloni J, Poirée S,
Hélénon O and Correas JM: Elastography of the thyroid. Diagn Interv
Imaging. 94:535–544. 2013. View Article : Google Scholar : PubMed/NCBI
|