Introduction
Helicobacter pylori infection is associated
with an increased risk of gastric cancer (1) and results inchanges in the expression of
inflammatory molecules, including cytokines and other immune
mediators (2). Immune mediators
activated by H. pylori have been demonstrated to promote
neoplastic transformation (3).
MicroRNAs (miRNAs/miRs) are small noncoding RNAs
that have been implicated in a number of physiological and
pathological responses as post-transcriptional repressors of gene
expression (4). miRNAs can
specifically bind to the 3′ untranslated region (UTR) of target
cellular mRNAs, in turn triggering mRNA degradation or inhibition
of translation (4). Previous studies
have suggested an association between miRNAs and H.
pylori-induced gastric carcinogenesis; Zhang et al
(5) demonstrated that miR-21 was
significantly upregulated in human gastric cancer tissues and H.
pylori-infected gastric mucosa, and that this upregulation
enhanced cell proliferation and invasion in a gastric cancer cell
line. Miao et al (6)
demonstrated that miR-375 inhibits H. pylori-induced gastric
carcinogenesis by blocking the Janus kinase 2-signal transducer and
activator of transcription 3 signaling pathway.
Autophagy is an important cellular function that
enables the recycling of proteins or damaged organelles (7). Previous studies have revealed that H.
pylori can induce autophagy in gastric epithelial cells
(8), and autophagy serves an
important functionin the development and progression of cancer
(9). Therefore H.
pylori-dependent autophagy maybe carcinogenic; however, the
molecular mechanisms underlying the association between autophagy
and H. pylori-induced gastric carcinogenesis remain
unclear.
Mammalian target of rapamycin (mTOR) is an inhibitor
of autophagy (8–10). Inhibitors of mTOR and miRNAs that
target mTOR have been demonstrated to promote autophagy and
therefore suppress the proliferation of a number of types of cancer
cell (10). In the present study,
miR-99b enhanced autophagy by targeting mTOR in gastric epithelial
cells and promoted H. pylori-induced gastric
carcinogenesis.
Materials and methods
Antibodies and reagents
The GFP-microtubule-associated protein 1A/1B light
chain 3 (LC3) plasmid was kindly provided by Dr Di Wang (Department
of Clinical Laboratory, The People's Liberation Army No. 309
Hospital, Beijing, China). Rapamycin (Rapa; cat. no. R8781),
bafilomycin A1 (cat. no. b1793) and 3-methyladenine (3-MA; cat. no.
5142-23-4) were purchased from Sigma-Aldrich; Merck KGaA,
Darmstadt, Germany. Antibodies against mTOR (cat. no. 2972), LC3
(cat. no. 4108) and GAPDH (cat. no. 5174) were obtained from Cell
Signaling Technology, Inc., Danvers, MA, USA. Anti-rabbit (cat. no.
sc-2054) and anti-mouse (cat. no. sc-358914) secondary antibodies
were purchased from Santa Cruz Biotechnology, Inc., Dallas, TX,
USA. ELISA kits for tumor necrosis factor-α (TNF-α; cat. no.
MTA00B) and interleukin-8 (IL-8; cat. no. D8000C) were purchased
from R&D Systems, Inc., Minneapolis, MN, USA.
Cell and bacterial culture
The human embryonic kidney cell line HEK-293T and
human gastric cancer BGC-823 cell line were purchased from the
American Type Culture Collection (Manassas, VA, USA). HEK-293T was
cultured in Dulbecco's modified Eagle's medium supplemented with
10% fetal bovine serum (FBS; Gibco; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA) in a humidified incubator at 37°C with 5%
CO2. The human gastric cancer cell line BGC-823 was
cultured in RPMI-1640 medium (Invitrogen; Thermo Fisher Scientific,
Inc.) supplemented with 10% FBS and 100 U/ml penicillin in a
humidified incubator at 37°C with 5% CO2. The wild-type
H. pylori strain 26695 was obtained from American Type
Culture Collection (Manassas, VA, USA) and grown as previously
described (11). Subsequently, cells
were seeded inthe wells of a 12-well plate and grown to 80%
confluency. The medium was then replaced with antibiotic-free
medium. H. pylori was added to cells at a multiplicity of
infection (MOI) of 100:1. The infection model was monitored by the
release of IL-8 and TNF-α, as measured by the DuoSet®
ELISA Development System (R&D Systems, Inc., Minneapolis, MN,
USA).
Cell transfection
All oligonucleotides were synthesized byShanghai
GenePharma Co., Ltd. (Shanghai, China). Sequences of all the
oligonucleotides were as follows: miR-99b mimic,
5′-CACCCGUAGAACCGACCUUGCG-3′; miR-99b inhibitor,
5′-CACCCGUAGAACCGACCUUGCG-3′; and scrambled miR-control,
5′-CAGUACUUUUGUGUAGUACAA-3′. Transfections were performed using
Lipofectamine® 2000 (Invitrogen; Thermo Fisher
Scientific, Inc.), according to the manufacturer's protocol. Cells
were transfected with 50 nM miRNA mimics, inhibitors, or scrambled
miR-control (negative control) for 24 h prior to subsequent
experiments.
Clinical samples
Patients undergoing gastrointestinal endoscopy at
The People's Liberation Army No. 309 Hospital (Beijing, China)
between January 1, 2014 and December 30, 2015, were enrolled. In
total, 38 patients with H. pylori+ gastric cancer
(28 male and 10 female; age range, 33–64 years), 10 patients with
H. pylori− gastric cancer (6 male and 4 female;
age range, 27–63 years), 22 patients with H.
pylori+ non-gastric cancer (17 male and 5 female;
age range, 36–66 years) and 9 healthy controls (6 male and 3
female; age range, 26–60 years) were included in the present study.
Gastric cancer tissues from the patients and gastric mucosa
tissuefrom non-cancer controls were retrieved from all the subjects
who received endoscopic sub-mucosal dissection and stored at −80°C
prior to subsequent experiments. The diagnoses of all the specimens
were histopathologically confirmed. The present study was approved
by the Ethics Committee of Dalian Medical University. Written
informed consent was obtained from all patients.
Bacterial colony-forming unit (CFU)
determination
Following infection, the cell bacterium co-culture
was washed three times with 1 ml of warm PBS per well to remove
non-adherent bacteria. To determine the CFU count corresponding to
intracellular bacteria, the cell monolayers were treated with
gentamicin (100 µg/ml; Sigma-Aldrich; Merck KGaA; G1272) at 37°C in
5% CO2 for 1 h, washed three times with warm PBS, and
then incubated with 1 ml of 0.5% saponin (Sigma-Aldrich; Merck
KGaA; 47036) in PBS at 37°C for 15 min. The treated monolayers were
homogenized and viable bacteria were grown on Mueller-Hinton agar
(BD Biosciences, Franklin Lakes, NJ, USA) containing sterile
defibrinated sheep blood (Shanghai YIJI industries Co., Ltd.,
Shanghai, China; cat. no. P0041) (5% v/v) and enumerated by the
pour plate method following serial dilution (11).
Bioinformatics approach
The Target Scan database (http://www.targetscan.org) was used to identify
putative human target genes for miR-99b by their 3′UTRs.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was extracted from cells using TRIzol
reagent (Invitrogen; Thermo Fisher Scientific, Inc.) in accordance
with the manufacturer's protocol. RT-qPCR analysis for miRNAs was
performed using TaqMan miRNA assays (Ambion; Thermo Fisher
Scientific, Inc.) and has-miR-99b RT-PCR primer set (cat. no.,
abx096835; Abbexa Ltd., Cambridge, UK) in an iQ5 Real-Time PCR
Detection System (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Reverse transcription reactions were performed using
TAQMAN® microRNA RT kit (Ambion; Thermo Fisher
Scientific, Inc.) under the following conditions: 16°C for 30 min,
42°C for 30 min and 84°C for 5 min. PCR reactions were performed
using the following conditions: 95°C for 2 min followed by 40
cycles of 95°C for 15 sec and 60°C for 30 sec. U6 small nuclear RNA
was used as an endogenous control for data normalization. Relative
expression was calculated using the 2−ΔΔCq method
(12).
Western blot analysis
Cells were washed with PBS and then lysed with
protein lysis buffer (Pierce; Thermo Fisher Scientific, Inc.).
Following centrifugation at 5,000 × g for 15 min at 4°C, the
protein concentration was measured with a bicinchoninic acid
protein assay kit (Pierce; Thermo Fisher Scientific, Inc.). A total
of 50 µg protein was loaded per lane and run on a 10% SDS-PAGE gel.
The proteins were transferred to polyvinylidene difluoride
membranes. The membranes were blocked with 5% non-fat dry milk in
Tris-buffered saline (pH 7.4) containing 0.05% Tween-20 at room
temperature for 1 h, and were incubated with primary antibodies
(1:200; Cell Signaling Technology, Inc.) and horseradish
peroxidase-conjugated secondary antibodies (1:5,000; Santa Cruz
Biotechnology, Inc.) at 4°C overnight in accordance with the
manufacturer's protocol. The protein of interest was visualized
using an enhanced chemiluminescence western blotting substrate
(Pierce; Thermo Fisher Scientific, Inc.) and the Chemidoc XRS Gel
Documentation System (Bio-Rad Laboratories, Inc.). Image J (version
2.1.4.7; National Institutes of Health, Bethesda, MD, USA) was used
for quantification of the results.
Cell proliferation assay
An MTT assay, which tests for cell proliferation and
viability, was used in this study as previously described (13). Cells were seeded at a density of
5×103/well and incubated in 96-well culture plates for
72 h at 37°C. A total of 50 µl MTT solution was added to each well
prior to incubation at 37°C for 4 h. Following incubation, the MTT
reagent was aspirated and 150 µl/well of DMSO was added to each
well to dissolve the formazan precipitate. Subsequently, the
DuoSet® ELISA Development System (R&D Systems, Inc.,
Minneapolis, MN, USA) was used to measure the optical densities of
the plates at 570 nm. Cell number was calculated as follows: Cell
numbertarget=(ODtarget-ODblank)/(ODcontrol-ODblank)
× cell numbercontrol.
Confocal microscopy
Cells were grown on collagen-precoated glass cover
slips in 24-well plates at a density of 105 cells/well.
Cells were transfected with control, miR-99b mimics or inhibitor,
together with GFP-LC3 using Lipofectamine® 2000. Cells
were washed three times for 3 min with PBS, fixed with 4%
paraformaldehyde at 37°C for 15 min and further washed with PBS.
The cells were then mounted with vecta-shield reagent (Vector
Laboratories, Inc., Burlingame, CA, USA). A Radiance 2000 laser
scanning confocal microscope was used for confocal microscopy,
followed by analysis with Laser Sharp 2000 software (Bio-Rad
Laboratories, Inc.). Images were captured in the sequential
scanning mode.
Plasmid constructs and luciferase
reporter assay
To construct the luciferase report vector, mTOR
3′UTR and its flanking sequence were PCR-amplified using primers:
5′-CGGGGTACCAGATGTGCCCATCACGTTTT-3′ (forward) and
5′-CCGGAATTCTGGTGTCTAGACATGGCTACACTT-3′ (reverse). The amplified
fragment was cloned into the PGL3 vector (Promega Corporation,
Madison, WI, USA). Similarly, a mutated mTOR 3′UTR fragment, in
which the miR-99b (5′-UACGGGU-3′ to 5′-AUGCCCA-3′) binding site was
mutated, was PCR-amplified using primers:
5′-CCATAACTTTAGAAAGCTACACTTTGACTTAACTCAC-3′ (forward) and
5′-GTGAGTTAAGTCAAAGTGTAGCTTTCTAAAGTTATGG-3′ (reverse). The PCR
product was cloned into the vector PGL3. Luciferase activity assay
was performed according to the instruction manual (Promega
Corporation).
Statistical analysis
All data are expressed as the mean ± standard
deviation from ≥3 independent experiments performed in triplicate.
Statistically significant differences between groups were
determined using a two-tailed Student's t-test using SPSS software
(version 17.0; SPSS, Inc., Chicago, IL, USA). P<0.05 was
considered to indicate a statistically significant difference.
Results
Expression of miR-99b is increased in
H. pylori+cancer samples compared with H.
pylori− cancer samples
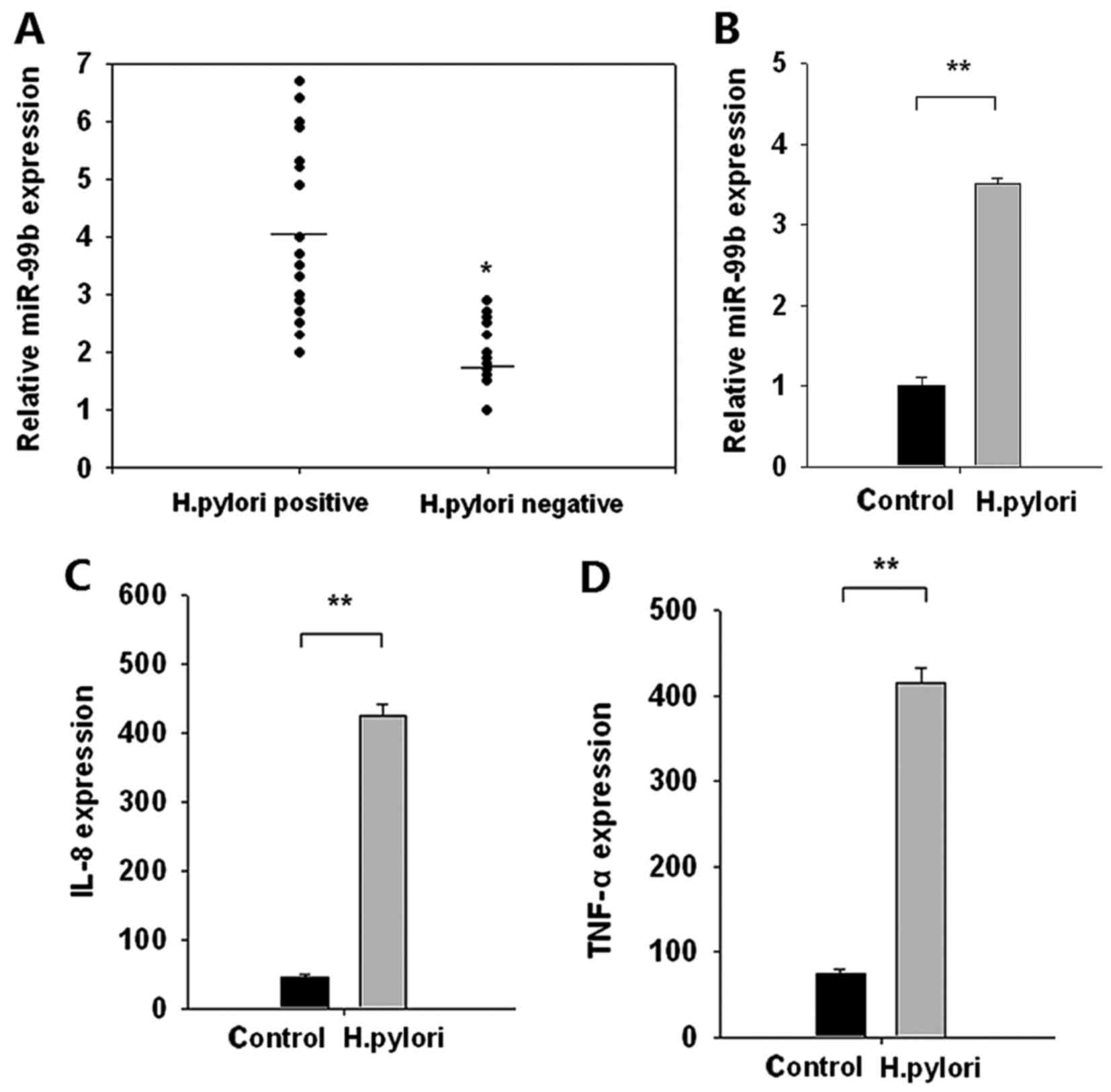
The expression of miR-99b was evaluated in 38 H.
pylori+ and 10 H. pylori−gastric
cancer samples. The expression of miR-99b was significantly
increased in H. pylori+ gastric cancer samples
compared with that in H. pylori− gastric cancer
samples (P<0.05; Fig. 1A). To
confirm these clinical findings, miR-99b expression was evaluated
in H. pylori-infected BGC-823 human gastric carcinoma cells.
Expression of miR-99b was significantly increased following H.
pylori infection compared with control cells (P<0.01;
Fig. 1B). Simultaneously, the
expression of the pro-inflammatory cytokines IL-8 and TNF-α was
significantly increased following H. pylori infection
compared with the control (both P<0.01; Fig. 1C and D). These data suggested that
H. pylori infection promoted the upregulation of miR-99b,
which may be implicated in neoplastic transformation.
miR-99b enhances intracellular H.
pylori elimination and decreases BGC-823 cell proliferation
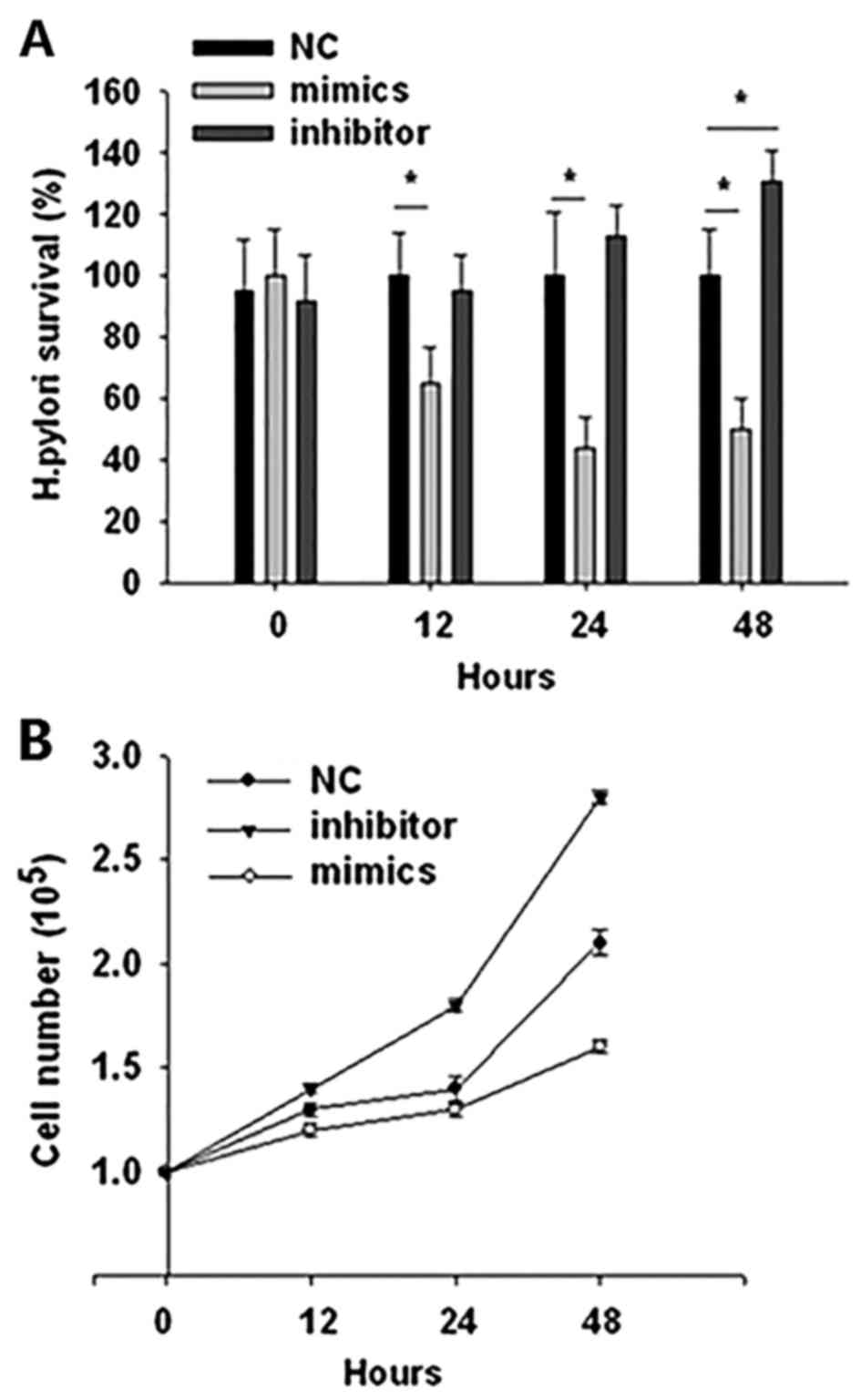
BGC-823 gastric cancer cells were transiently
transfected with miR-99b mimics, inhibitors, or negative control
and then challenged with H. pylori at an MOI of 100. The
intracellular survival rate of H. pylori was examined at
different time points. The results demonstrated that transfection
with miR-99b mimics significantly reduced the survival rate of
intracellular H. pylori compared with the negative control
(P<0.05; Fig. 2A). Transfection
with a miR-99b inhibitor had no significant effect on H.
pylori survival, with the exception of at 48 h following
infection, when the survival rate of H. pylori was
significantly increased compared with the negative control
(P<0.05; Fig. 2A). To verify
whether miR-99b serves a rolein tumor initiation, the effects
miR-99b on cell proliferation were assessed. An MTT analysis
demonstrated that the BGC-823 cell number was markedly decreased
following transfection with miR-99b mimics compared with the
negative control group, whereas transfection with an miR-inhibitor
markedly increased the cell number compared with the control group
at 12, 24 and 48 h post-infection (Fig.
2B).
miR-99b induces intracellular H.
pylori elimination and BGC-823 cell death through autophagy
upregulation
It has previously been demonstrated that H.
pylori-induced cell proliferation was acarcinogenic factor
(6), and autophagy serves a critical
role in intracellular H. pylori elimination and regulation
of cell proliferation and carcinogenesis (8). Therefore miR-99b may mediate H.
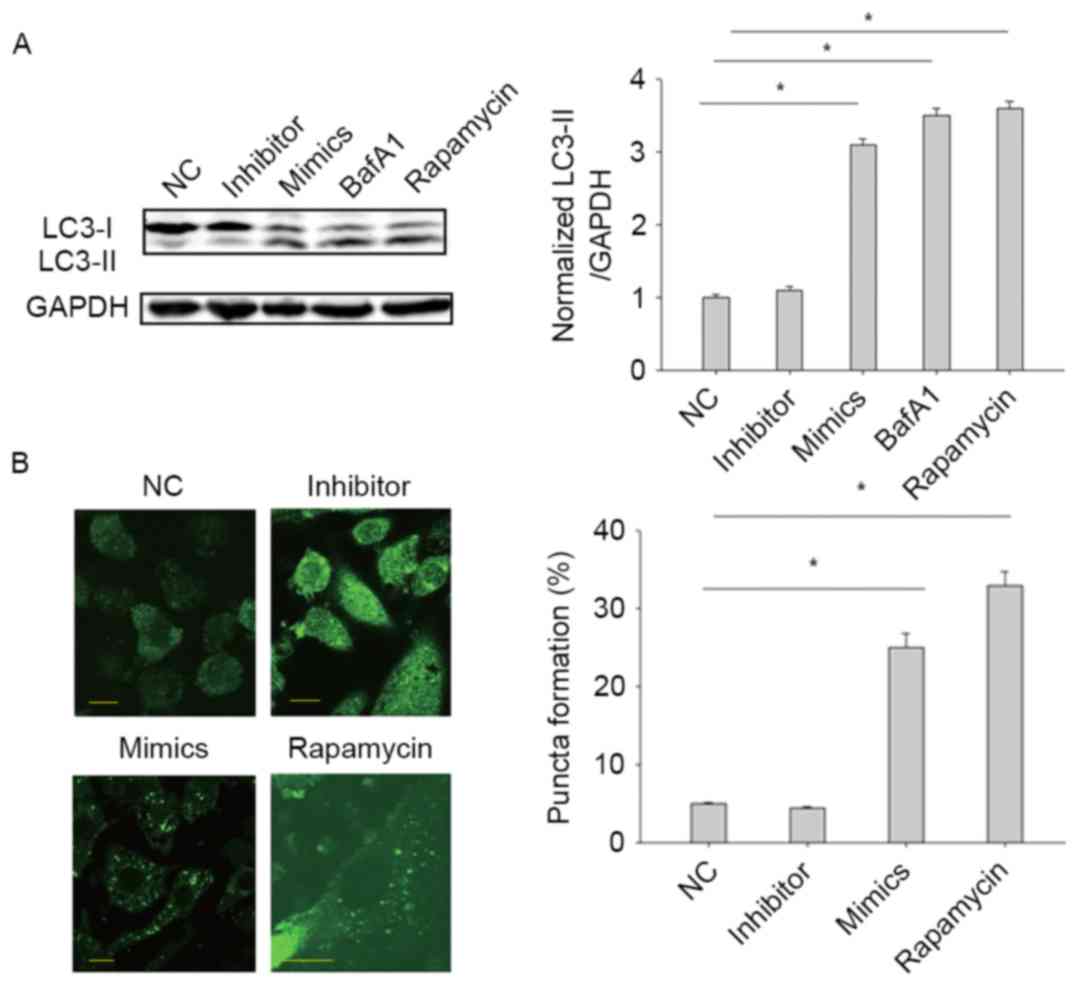
pylori-induced cell proliferation by regulating autophagy. LC3
conversion from LC3-I to LC3-II indicates activation of autophagy
(8,9).
To test our hypothesis, LC-3 expression was measured in BGC-823
cells following transfection with miR-99b mimics, inhibitors or a
negative controlfor 24 h. Transfection with miR-99b mimics
significantly increased the expression of LC3-II compared with the
negative control (P<0.05), whereas transfection with miR-99b
inhibitor had no clear effect on the expression of LC-II (Fig. 3A). As a positive control, treatment
with rapamycin (200 nM; autophagy inducer) significantly increased
the expression of LC3-II compared with the control (P<0.05). In
addition, treatment with bafilomycin A1 (200 nM; LC3-II degradation
inhibitor) resulted in a significant increase in LC3-II expression
compared with the control, indicating that the autophagic flux was
unobstructed (P<0.05; Fig. 3A). To
confirm that miR-99b triggers autophagy, a GFP-LC3-II puncta
formation assay was used to monitor autophagy. Transfection with
miR-99b significantly increased the percentage of cells with
GFP-LC3-II-positive puncta compared with the control cells
(P<0.05), whereas transfection with miR-99b inhibitor had no
effect (Fig. 3B). Taken together,
these results demonstrated that miR-99b promotes autophagy in
gastric cancer cells.
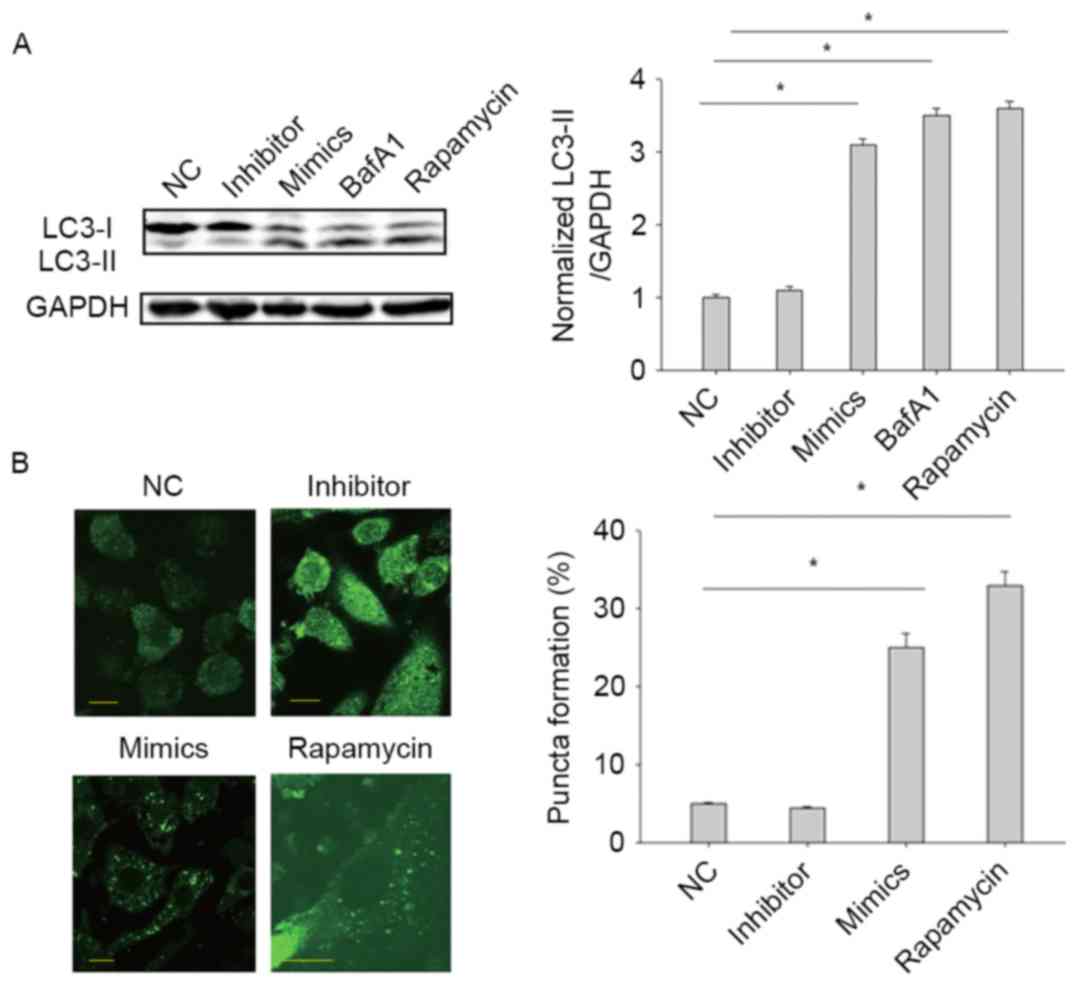 | Figure 3.miR-99b promotes autophagy. (A)
BGC-823 cells were treated with rapamycin, BafA1, miR-99b mimics or
miR-99b inhibitor. The LC3-II/GAPDH level was determined by western
blot analysis. (B) BGC-823 cells were transfected with plasmid
expressing GFP-LC3B, together with either negative control, miR-99b
mimics or miR-99b inhibitor. After 24 h, following fixation, cells
were immediately visualized using confocal microscopy (scale bar=10
µm). The number of GFP-LC3B puncta in each cell was counted.
*P<0.05 vs. NC. miR, microRNA; LC3, microtubule-associated
protein 1A/1B light chain 3; NC, negative control; BafA1,
bafilomycin A1. |
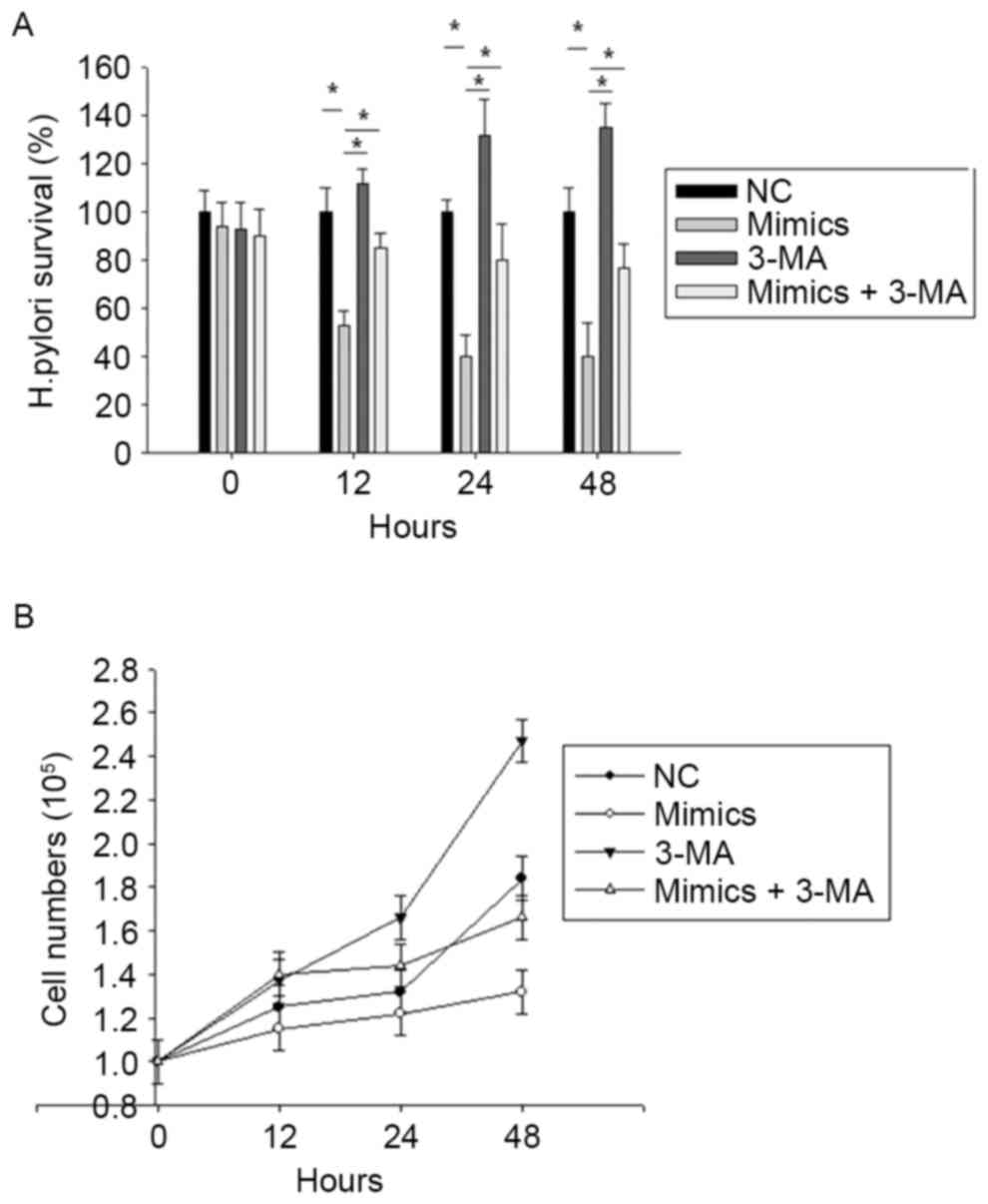
It was further investigated whether miR-99b induces
intracellular H. pylori elimination and gastric carcinoma
cell death through autophagy upregulation. BGC-823 cells were
pre-treated with miR-99b mimics or not, and either left untreated
or pre-treated with the autophagy inhibitor 3-MA (5 mM), followed
by exposure to H. pylori for 12, 24 and 48 h. Treatment with
3-MA reversed the effect of miR-99b mimics on the H. pylori
survival rate (Fig. 4A) and BGC-823
cell number (Fig. 4B). These data
demonstrate that miR-99b decreases the survival of intracellular
H. pylori and BGC-823 cell numberby inducing autophagy.
miR-99b promotes autophagy by
targeting mTOR
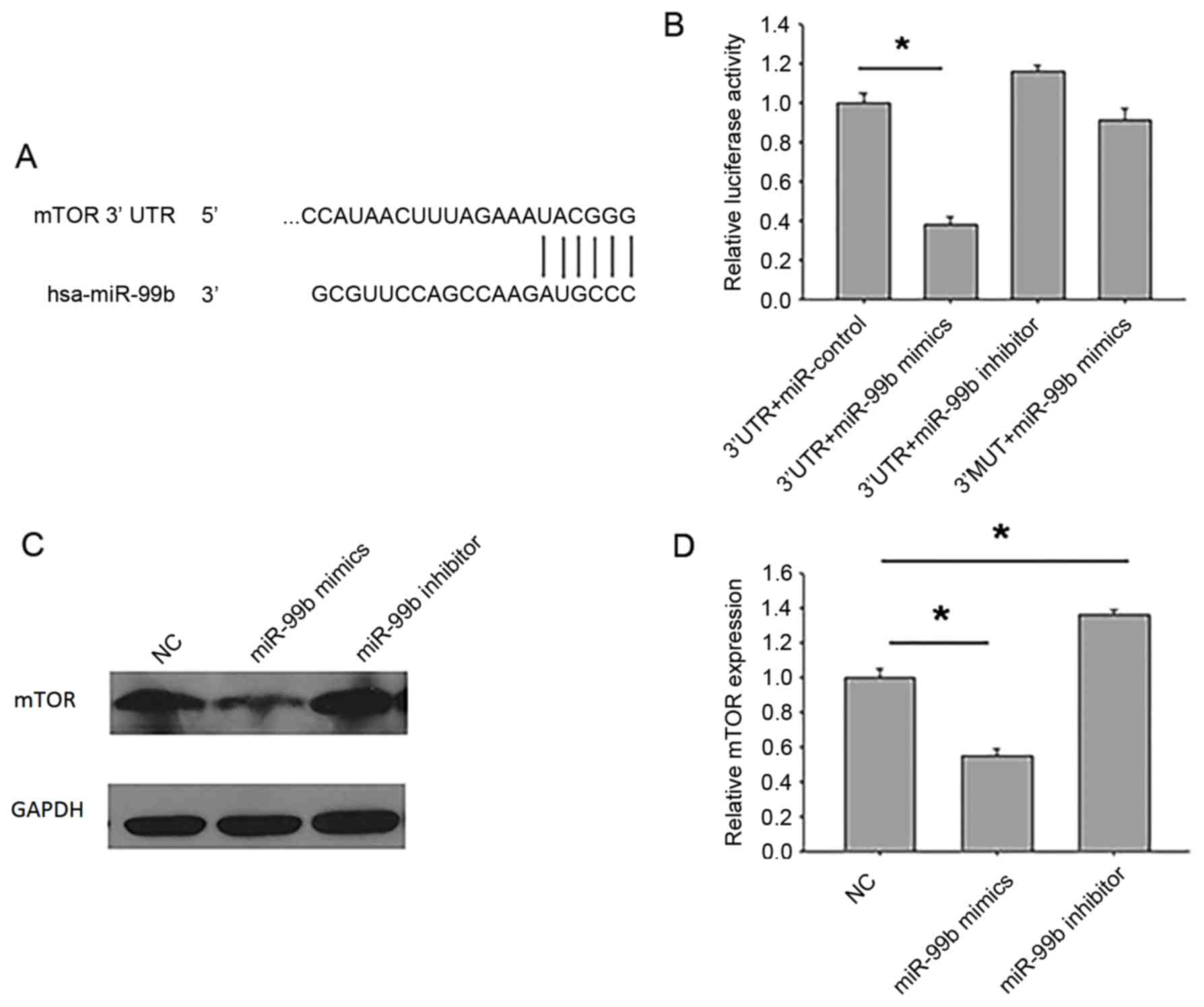
To determine the mechanism underlying the effect of
miR-99b on autophagy, a bioinformatics approach was used to
identify potential miR-99b targets, and miRNA target identification
quality was improved through theuse of prediction programs. mTOR
was identified as a putative miR-99b target gene (Fig. 5A). To directly address whether miR-99b
binds to the 3′UTR of target mRNAs, luciferase report vectors were
constructed that contained the putative miR-99b binding sites
within the mTOR 3′UTR. In addition, a vector containing the mTOR
3′UTR mutated within the putative miR-99b binding site (3′MUT) was
generated. A significant reduction in luciferase activity was
observed in HEK-293T cells following transfection with the mTOR
3′UTR luciferase vector and miR-99b mimics compared with cells
transfected with the luciferase vector alone (P<0.05; Fig. 5B). However, no significant difference
in luciferase activity was observed in cells transfected with 3′MUT
and miR-99b mimics compared with cells transfected with 3′MUT
alone.
Next, the protein expression of mTOR inBGC-823 cells
transfected with miR-99b mimics or inhibitors was measured.
Treatment with miR-99b mimics significantly reduced the protein
expression of mTOR (P<0.05), whereas treatment with miR-99b
inhibitor significantly increased the protein expression of mTOR
(P<0.05; Fig. 5C and D). As the
mTOR inhibitor rapamycin significantly enhanced autophagy in
gastric cancer cells (Fig. 3), taken
together these results indicate that miR-99b decreases
intracellular bacterial load and gastric cancer cell proliferation
by promoting autophagy through the inhibition of mTOR
expression.
Discussion
H. pylori promotes inflammation of the
gastric mucosa, which can then lead to gastric atrophy and
intestinal metaplasia, resulting in the development of gastric
cancer. H. pylori may therefore represent acritical risk
factor for gastritis and gastric cancer transformation. Previous
studies have indicated that cell proliferationis an important
indicator of gastric carcinogenesis; therefore controlling cell
proliferation may be an effective method to prevent and treat
gastric cancer (6).
Among the mediators induced in response to H.
pylori infection, miRNAs may serve a major rolein the outcome
of the bacteria-host interaction by acting as immune mediators that
link inflammatory responses with gastric carcinogenesis; Li et
al (14) demonstrated that H.
pylori may function as an initiator in the process of
carcinogenesis by up-regulating miR-222, which promotes cell
proliferation and inhibits the expression of
reversion-inducing-cysteine-rick protein with kazal motifs. Ma
et al (15) demonstrated that
miR-223 contributes to cancer cell proliferation and migration
during H. pylori infection. In addition, Chang et al
(16) identified a series of miRNAs
(miR-99b-3p, −564 and −638) that are aberrantly expressed in
gastric cancer in a H. pylori-dependent manner, further
demonstrating that certain miRNAs are differentially expressed
between H. pylori+ and H.
pylori− gastric cancer tissues.
miR-99b has been demonstrated to serve as a tumor
suppressor by inhibiting cancer cell proliferation by targeting a
number of proteins, including homeobox-A1, SWI/SNF-related
matrix-associated actin-dependent regulator of chromatin subfamily
A member 5 (SMARC) subfamily A member 5, SMARC subfamily D member 1
and mTOR (17). mTOR serves a crucial
role in cancer biology and has emerged as a potential target for
drug development (18).
The results from the present study demonstrated that
H. pylori infection induces cell proliferation, which is
regulated by miR-99b. Challenging with miR-99b inhibitor increased
mTOR expression and promoted BGC-823 cell proliferation, the latter
of which was reversed by treatment with the mTOR inhibitor
rapamycin. H. pylori elimination may block cancer cell
proliferation (6), indicating that
miR-99b may suppress carcinogenesis partly through bacterial
elimination. As treatment with miR-99b mimics in the absence of
H. pylori infection also decreased cell proliferation in the
current study, there may be an additional regulatory pathway of
miR-99b that affects carcinogenesis.
mTOR has previously been identified as a key
regulatory factor in the autophagic pathway due to is role as a
sensor for amino acids and ATP depletion, and its role in
integrating hormonal stimuli via the class I phosphoinositide
3-kinase/protein kinase B signaling pathway (8). In the immune system, mTOR is induced by
inflammatory cytokines and growth factors, and inhibits
inflammation-associated gastrointestinal tumorigenesis (19). A previous study suggested that H.
pylori suppresses autophagy, mediates inflammation and
facilitates intracellular survival of the pathogen itself, while
also generating an environment that favors carcinogenesis (20). The results from the present study
suggest that the induction of autophagy by miR-99b negatively
regulates cancer cell proliferation and therefore prevents H.
pylori-induced carcinogenesis. These findings provide a basis
for novel treatments for cancer based on miRNA-dependent induction
of autophagy.
Acknowledgements
The authors of the present study would like to thank
Dr Qi Yu and Dr Chaohui Zhu from The People's Liberation Army No.
309 Hospital (Beijing, China) for providing the clinical tissues
samples of the patients.
References
|
1
|
Lee YC, Chiang TH, Chou CK, Tu YK, Liao
WC, Wu MS and Graham DY: Association between Helicobacter pylori
eradication and gastric cancer incidence: A systematic review and
meta-analysis. Gastroenterology. 150:1113–1124. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wessler S, Krisch LM, Elmer DP and Aberger
F: From inflammation to gastric cancer-the importance of
Hedgehog/GLI signaling in Helicobacter pylori-induced chronic
inflammatory and neoplastic diseases. Cell Commun Signal.
15:152017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Adamsson J, Lundin SB, Hansson LE, Sjovall
H and Svennerholm AM: Immune responses against Helicobacter pylori
in gastric cancer patients and in risk groups for gastric cancer.
Helicobacter. 18:73–82. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bartel DP: MicroRNAs: Genomics,
biogenesis, mechanism, and function. Cell. 116:281–297. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang Z, Li Z, Gao C, Chen P, Chen J, Liu
W, Xiao S and Lu H: MiR-21 plays a pivotal role in gastric cancer
pathogenesis and progression. Lab Invest. 88:1358–1366. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Miao L, Liu K, Xie M, Xing Y and Xi T:
miR-375 inhibits Helicobacter pylori-induced gastric carcinogenesis
by blocking JAK2-STAT3 signaling. Cancer Immunol Immunother.
63:699–711. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fulda S: Autophagy in cancer therapy.
Front Oncol. 7:1282017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yang JC and Chien CT: A new approach for
the prevention and treatment of Helicobacter pylori infection via
upregulation of autophagy and downregulation of apoptosis.
Autophagy. 5:413–414. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhan Z, Li Q, Wu P, Ye Y, Tseng HY, Zhang
L and Zhang XD: Autophagy-mediated hmgb1 release antagonizes
apoptosis of gastric cancer cells induced by vincristine via
transcriptional regulation of mcl-1. Autophagy. 8:109–121. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kim YC and Guan KL: mTOR: A pharmacologic
target for autophagy regulation. J Clin Invest. 125:25–32. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wu K, Yang L, Li C, Zhu CH, Wang X, Yao Y
and Jia YJ: MicroRNA-146a enhance Helicobacter pylori induced cell
apoptosis in human gastric cancer epithelial cell. Asian Pac J
Cancer Prev. 15:5583–5586. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2-ΔΔCt method. Methods. 25:402–408. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang D, Zhu X, Cui C, Dong M, Jiang H, Li
Z, Liu Z, Zhu W and Wang JG: Discovery of novel acetohydroxyacid
synthase inhibitors as active agents against Mycobacterium
tuberculosis by virtual screening and bioassay. J Chem Inf Model.
53:343–353. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li N, Tang B, Zhu ED, Li BS, Zhuang Y, Yu
S, Lu DS, Zou QM, Xiao B and Mao XH: Increased mir-222 in H.
pylori-associated gastric cancer correlated with tumor progression
by promoting cancer cell proliferation and targeting reck. FEBS
Lett. 586:722–728. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ma L, Chen Y, Zhang B and Liu G: Increased
microRNA-223 in Helicobacter pylori-associated gastric cancer
contributed to cancer cell proliferation and migration. Biosci
Biotechnol Biochem. 78:602–608. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chang H, Kim N, Park JH, Nam RH, Choi YJ,
Lee HS, Yoon H, Shin CM, Park YS, Kim JM, et al: Different MicroRNA
expression levels in gastric cancer depending on Helicobacter
pylori infection. Gut Liver. 9:188–196. 2014. View Article : Google Scholar
|
|
17
|
Chen D, Chen Z, Jin Y, Dragas D, Zhang L,
Adjei BS, Wang A, Dai Y and Zhou X: MicroRNA-99 family members
suppress homeobox a1 expression in epithelial cells. PLoS One.
8:e806252013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Francipane MG and Lagasse E: mTOR pathway
in colorectal cancer: An update. Oncotarget. 5:49–66. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Thiem S, Pierce TP, Palmieri M, Putoczki
TL, Buchert M, Preaudet A, Farid RO, Love C, Catimel B, Lei Z, et
al: mTORC1 inhibition restricts inflammation-associated
gastrointestinal tumorigenesis in mice. J Clin Invest. 123:767–781.
2013.PubMed/NCBI
|
|
20
|
Greenfield LK and Jones NL: Modulation of
autophagy by Helicobacter pylori and its role in gastric
carcinogenesis. Trends Microbiol. 21:602–612. 2013. View Article : Google Scholar : PubMed/NCBI
|