Introduction
Cervical anterior corpectomy and fusion (ACF), which
involves direct removal of the compressive abnormality with
stabilization obtained by anterior arthrodesis, has been used as a
standard treatment option for cervical disc disease with excellent
clinical outcomes (1). However, there
are some limitations to ACF. First of all, for 25% of the patients
undergoing cervical fusion, the symptoms will reappear within 10
years (2). It has been well
documented that the rate of pseudarthrosis increases with each
segmental level added to an anterior decompression and fusion
(3). Secondly, although ACF has been
employed to treat cervical myelopathy caused by soft disc
herniation with stable outcomes (4),
complications related to bone grafting, such as dislodgement,
fracture, and nonunion of the grafted bone (5), and recurrence of myelopathy due to
adjacent segment degeneration (6)
have been reported. So in some cases, more than three-levels of ACF
(7) or cervical disc replacement have
to be performed to avoid secondary myelopathy.
The complications associated with ACF could
potentially be minimized by combining ACF with other treatments,
such as cervical artificial disc replacement (C-ADR). Analysis of
the strain distribution of intervertebral discs after ACF showed an
increase in longitudinal strain, most frequently at the levels
immediately adjacent to the fused level (8). On the other hand, it has been
demonstrated that C-ADR maintains motion at the operated level and
decreases strain on the adjacent segments for prevention of
adjacent-segment disease (ASD) (9).
Therefore, ACF and C-ADR could potentially be combined together to
treat multilevel cervical myelopathy (MCM) with reduced risk of
ASD. Since the clinical outcomes of two levels C-ADR are not well
defined, in this study we only performed one level C-ADR on the
patients. Our current study aimed to evaluate the clinical and
radiographic outcomes of patients undergoing this hybrid
technique.
Patients and methods
Patient data
All patients with MCM undergoing this hybrid
technique in the authors' clinic over a 3-year period were
assessed. This study was approved by the Ethics Committee of
Jiangyin People's Hospital (Jiangyin, China) and Changzheng
Hospital (Shanghai, China). Signed written informed consents were
obtained from all participants before the study. Inclusion
criteria: patients with three or four consecutive level
degenerative disc disease between C3 and C7 and with a
radiculopathy or myelopathy that was not responding to conservative
treatments. Exclusion criteria: facet syndrome, patients with
stenosis caused by posterior compression, osteoporosis,
ossification of posterior longitudinal ligament (OPLL), tumor,
severe degenerative scoliosis or kyphosis and infection, which are
considered as the standard contraindications for ACF and C-ADR
techniques. Hybrid technique was not performed if the first or the
last segment was spondylotic and not mobile. A total of 23 patients
(14 females and 9 males) were included in the study. The mean age
at surgery was 48.3±8.5 years. The target levels were consecutive
in all cases, including C3-6 (n=9), C3-7 (n=6), C4-7 (n=8). C-ADR
was performed in the segment that had greater physiologic motion
(C6/7>C3/4) when the first or the last segment was mobile and
non-spondylotic.
Surgical procedure
A standard Smith-Robinson approach was used to
expose the symptomatic levels in all patients. Subtotal corpectomy
with strut graft was performed by removing discs, vertebral bodies,
and posterior longitudinal ligament (10). Operative levels were determined based
on preoperative radiographic results. Extensive decompression was
performed to expose the dura throughout the length of the
corpectomy and discectomy via removal of the osteophytes, herniated
nucleus pulposus and posterior longitudinal ligament. Titanium mesh
(DePuy Synthes Spine, Inc., Raynham, MA, USA) filled with the bone
dust of the resected vertebra was placed in the anterior cervical
plate (Slim-Loc; DePuy Synthes Spine, Inc.). Preparation of the
endplates for arthroplasty was accomplished following the standard
procedure. Sizing of the Prestige® Cervical Disc
(Medtronic, Memphis, TN, USA) was determined by comparing the
preoperative radiographic results including computed tomography
(CT) scan to the templates. Insertion of the C-ADR (Discover™;
DePuy Synthes Spine, Inc.) was accomplished under lateral
fluoroscopy to ensure adequate depth. Correct placement of a C-ADR
was confirmed by anteroposterior (AP) and lateral fluoroscopic
imaging before closure of the incision. All patients were allowed
to sit up within a few days after surgery and wore a plastic
cervical collar without a chin support for 2 months.
Data collection
Preoperative demographic, surgical, and outcome data
were collected from all patients. Clinical outcomes were assessed
by arm and neck VAS scores, neck disability index (NDI) scores and
range of motion (ROM). ROM of the cervical spine was measured on
plain radiographs. Data from patients who had completed the
follow-up examination scheduled at 6 weeks, 3 and 24 months after
surgery were analyzed.
Statistical analysis
Statistical Package for the Social Sciences (SPSS)
program (version 11.0; SPSS, Inc., Chicago, IL, USA) was used for
the statistical analyses. Results are expressed as mean ± standard
deviation (SD). Comparison between multiple groups was made using
one-way ANOVA followed by a post-hoc test (Least Significant
Difference). P<0.05 was considered to indicate a statistically
significant difference.
Results
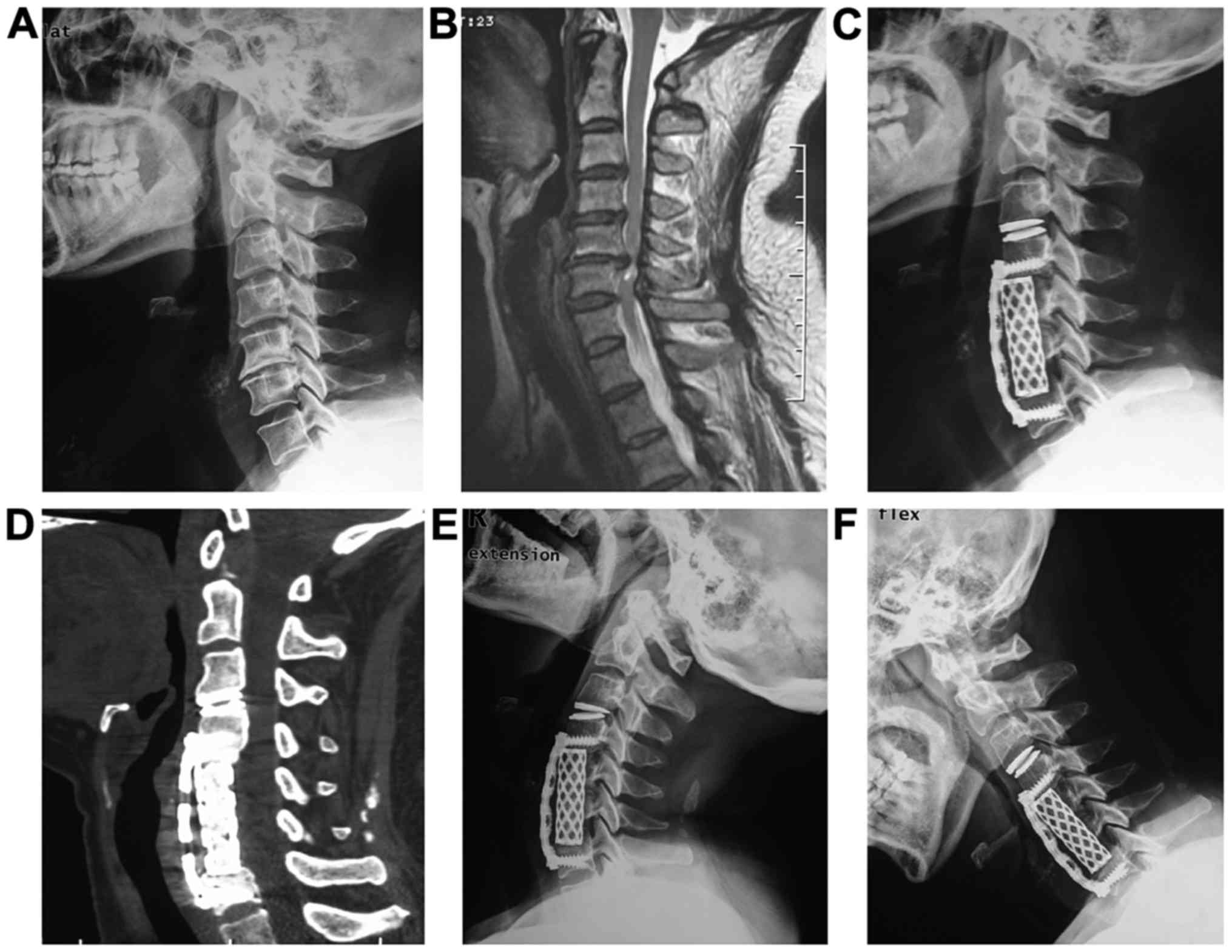
Correct placement of C-ADR
To make sure that C-ADR was correctly placed during
the surgery, lateral fluoroscopic images were taken as shown in
Fig. 1A. No hardware complications
were observed in this study as shown in Fig. 1C. Bone fusion was achieved in all
patients at 6 months after operation (Fig. 1D). ROM was calculated by the
difference in Cobb angles between full flexion and extension in
lateral cervical radiographs (Fig.
1).
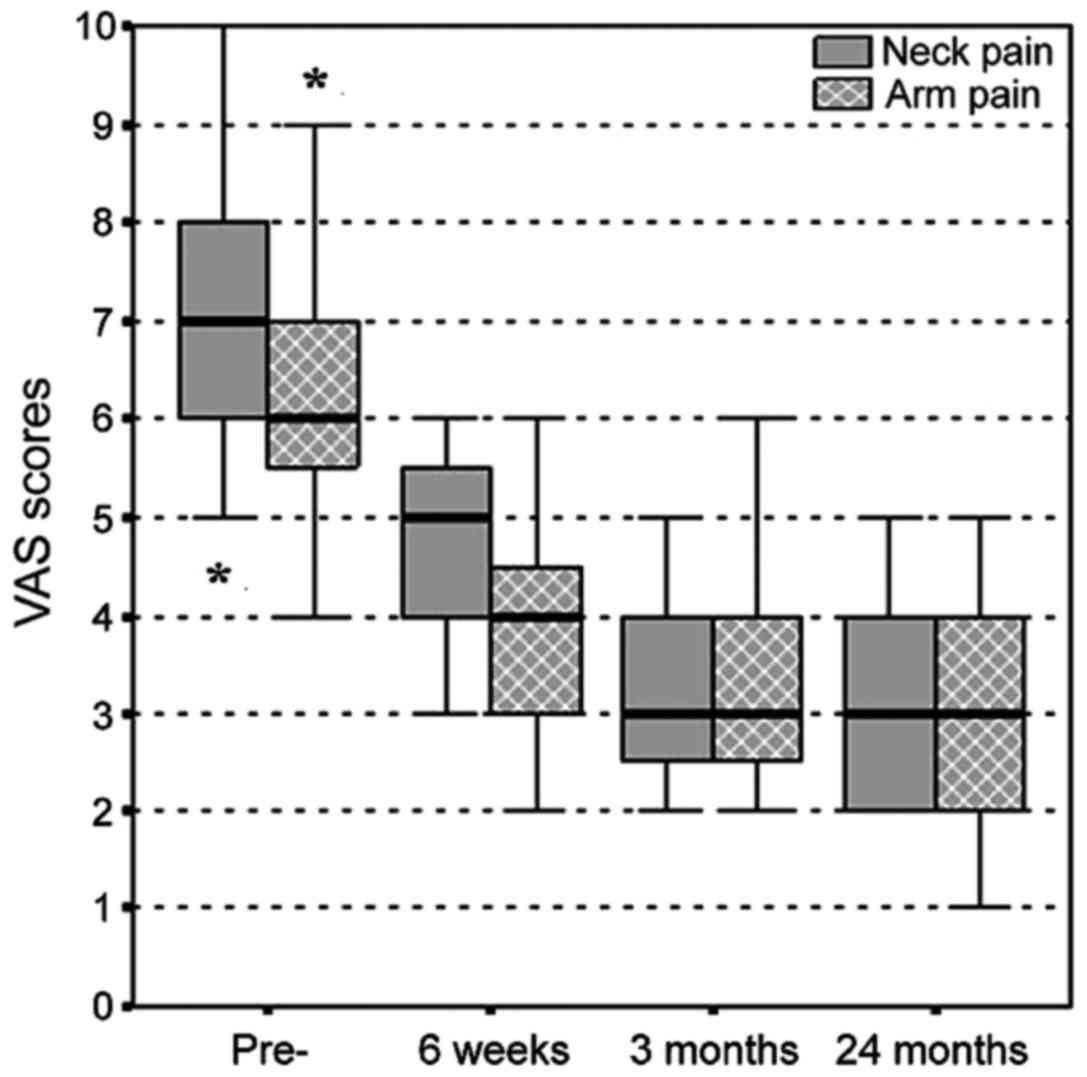
Clinical outcomes
As shown in Fig. 2,
the neck-pain VAS score before surgery was 6.96±1.77, and decreased
gradually over the follow-up period (4.65±1.03 at 6 weeks;
3.30±1.06 at 3 months and 3.09±0.95 at 24 months). The same trend
was observed for arm-pain VAS score, which was 6.35±1.61 before
surgery and decreased to 4.00±1.13 at 6 weeks; 3.30±1.11 at 3
months and 3.00±0.95 at 24 months after surgery. Therefore, our
results showed that both the neck- and arm-pain VAS scores were
significantly improved after surgery (P<0.05).
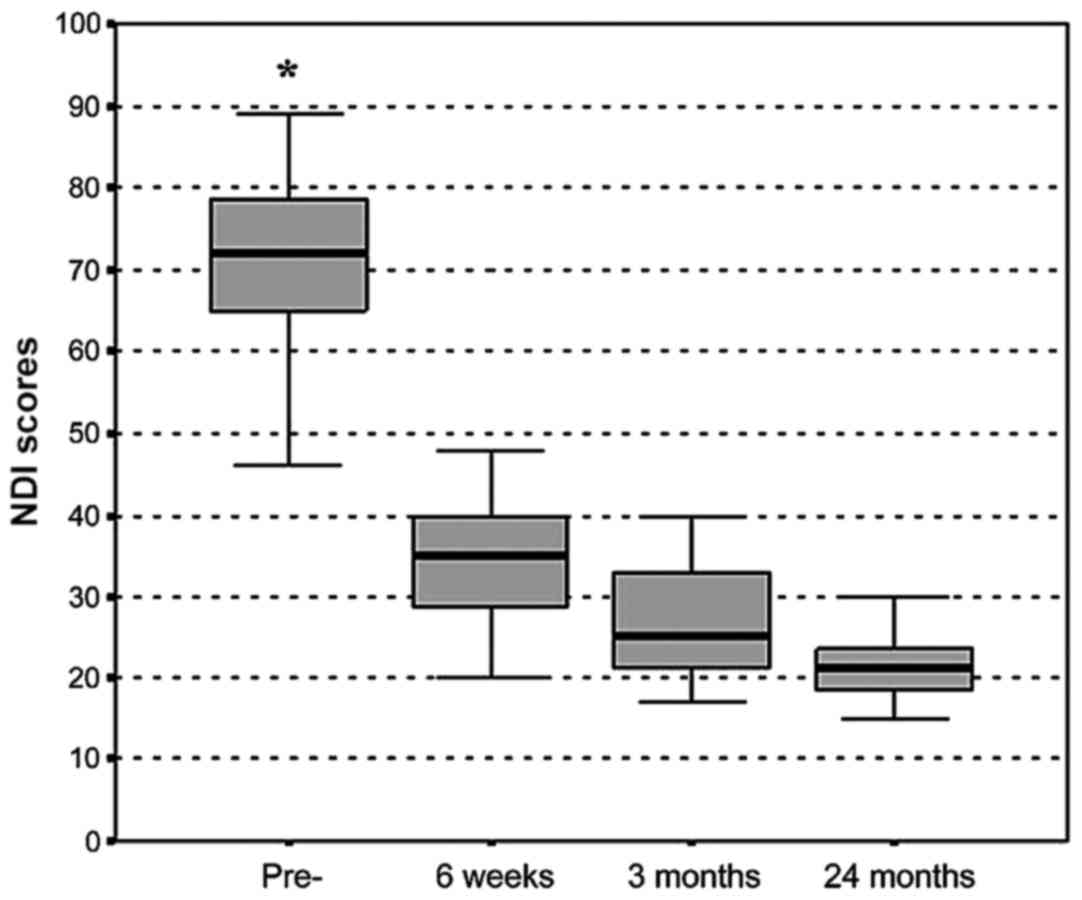
Reduction of NDI scores was also observed after
surgery at all follow-up time-points (70.39±10.68 before surgery
vs. 37.65±13.59 at 6 weeks; 26.65±6.87 at 3 months and 21.35±4.09
at 24 months after surgery) (Fig. 3).
The differences between pre- and postoperative NDI scores were
statistically significant (P<0.05).
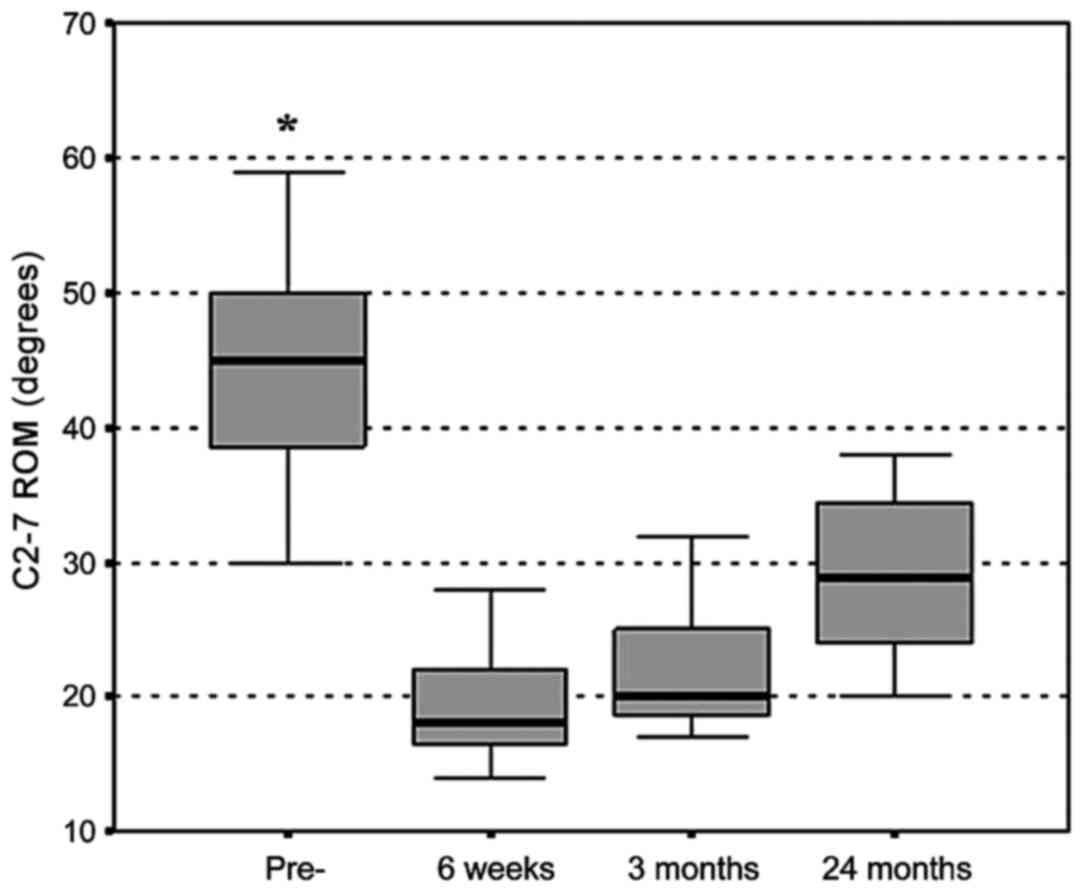
Changes in C2-7 ROM were also notable (Fig. 4). We observed a 56% of reduction in
ROM at 6 weeks after surgery (43.96±8.19 vs. 19.17±3.55,
P<0.05). The reduction rate of ROM was less as the follow-up
prolonged (50% at 3-month follow-up and 34% at 24-month follow-up),
but the statistical significance remained (P<0.05). The C2-7 ROM
degrees achieved by our hybrid technique were compared to the data
from some of the published studies which assessed anterior or
posterior approach in MCM (Table I)
(10–12). Studies (10–12) showed
that the rate of the ROM decrease was greater than those obtained
by this hybrid technique.
 | Table I.The C2-7 ROM decrease for anterior
surgery in each study. |
Table I.
The C2-7 ROM decrease for anterior
surgery in each study.
|
|
|
|
| Cervical ROM
(degree) |
|
|---|
|
|
|
|
|
|
|
|---|
| Sources | Approach | Follow-up time | No. of patients | Pre- | Post- | Mean decrease rate of
ROM (%) |
|---|
| Edwards et al
(10) | Corpectomy and fusion
with instrumentation | 49 months | 13 | 37.00 | 16.00 | 56.76 |
| Wada et al
(11) | Corpectomy and fusion
without instrumentation | 15 years | 23 | 39.40 | 19.20 | 51.27 |
| Lee et al
(12) | Corpectomy and fusion
with instrumentation | 21.8 months | 20 | 37.30 | 17.70 | 52.55 |
Surgical outcomes and
complications
During the follow-up period, there were no
complications related to the surgical procedures, such as device
migration, infection, neurologic compromise, pseudoarthrosis, or
heterotopic ossification. No other adjacent segment degeneration
was detected either radiographically or clinically.
Discussion
The primary goals of the surgical treatment of MCM
are the relief of neurological compression, stabilization of
cervical spine and restoration of lordotic alignment. Posterior
procedures, such as laminectomy and laminoplasty, which are
associated with significant postoperative axial pain and high
incidence of postoperative kyphosis, have become less preferred
treatments of MCM (2,13,14). For
patients with cervical myelopathy involving only one or two motion
segments, ACF has been the preferred surgical treatment which is
performed with high success rate and less complications (15). However ACF is not the best treatment
option for MCM involving three or more levels, as it is associated
with less predictable outcomes and a higher frequency of
complications (16,17). So, currently, the most commonly used
technique for MCM with three or more levels is contiguous
corpectomies and fusion. However, the incidence of complications
resulting from this surgical modality, such as graft displacement,
non-union and hardware-related complications, is increased as more
levels are decompressed (8,18–20). It
has been demonstrated that a two-level fusion substantially
increases intradiscal pressure as compared to single-level fusion.
Hilibrand et al (21) have
recommended that all degenerated adjacent segments should be fused
with the target level. It has been demonstrated that C-ADR
maintains motion at the operated level and decreases strain on the
adjacent segments for prevention of ASD (22–24). If
the level at which surgery was performed still maintains mobility,
compensatory hypermobility may not occur in adjacent levels
(2). In MCM with sufficient cervical
motion at one or two levels, hybrid technique combining C-ADR at
the mobile level, with ACDF at the spondylotic level, may be a
reasonable alternative to contiguous corpectomies and fusion.
One of the open questions regarding the hybrid
technique as used in this study is whether or not combination of
ACF with C-ADR leads to firm fusion. In the present study, our
radiographic evaluation demonstrated a 100% fusion rate in the
segments. This hybrid technique was effective in eliminating
radicular pain and had a favorable recovery of NDI scores. At 6
weeks, the C2-7 ROM decreased immediately after surgery because of
patients' fear and residual pain. As the fear and residual pain
alleviated, the C2-7 ROM showed a better recovery at 3 and 24
months. On the other hand, we assumed that preserved ROM may be the
basis for a better clinical outcome. Our results are in close
agreement with previous research comparing clinical and
radiological outcomes between artificial disc replacement and
fusion. Also incidences of complications and secondary operations
in the current study are low, suggesting the functional success of
this hybrid technique. Hilibrand et al (21) have reported that each year ~2.9% of
the patients has to go through surgery due to symptomatic ASD after
ACF. In our present study, we did not observe any cases of ASD. We
hypothesize that the hybrid technique can reduce ASD by reducing
hypermobility in adjacent segments, or the small sample size and
the short follow-up periods are responsible for this result. Shin
et al (25) have reported that
in two consecutive level cervical disc disease, the hybrid
technique is superior to the two-level ACDF in terms of better NDI
recovery, less postoperative neck pain, faster C2-7 ROM recovery,
and less adjacent ROM. But these benefits of hybrid technique are
similar to those of 2-ACDF with 5 years of follow-up (26).
Further studies are required to determine the
underlying etiology of adjacent segment degeneration which might be
due to the type of instrumentation used or the natural history of
the disease itself. Also, it would be beneficial to understand the
ideal biomechanical properties of this hybrid technique, which
would enable us to make better use of this hybrid technique in
treating MCM patients.
High hospitalization expenses, small sample size,
short follow-up period and lack of a control group are the few
limitations of the present study.
In conclusion, the results in this study indicate
that this hybrid technique treatment combining ACDF with C-TDR is
both technically feasible and effective for surgical treatment of
MCM. This study demonstrates the benefits of developing a treatment
specific for the needs of the patient and each vertebral segment.
However, future comparative studies will be required to determine
the potential pros and cons of the hybrid technique. Long-term
follow-up studies are also required to assess the clinical and
functional outcome, and reoperation rates of the hybrid
technique.
Acknowledgements
Not applicable.
Funding
This study was supported by the Young Medical
Talents of Jiangsu Province (QNRC2016132), and the Major Program of
Wuxi Municipal Commission of Health and Family Planning
(201708).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
YZhu and YZhang designed the study and performed the
experiments; JF, GX and XY collected the data; JF and GX analyzed
the data; YZhu and XY prepared the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Jiangyin People's Hospital (Jiangyin, China) and Changzheng
Hospital (Shanghai, China). Signed written informed consents were
obtained from all participants before the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bose B: Anterior cervical fusion using
Caspar plating: Analysis of results and review of the literature.
Surg Neurol. 49:25–31. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hilibrand AS, Carlson GD, Palumbo MA,
Jones PK and Bohlman HH: Radiculopathy and myelopathy at segments
adjacent to the site of a previous anterior cervical arthrodesis. J
Bone Joint Surg Am. 81:519–528. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Farey ID, McAfee PC, Davis RF and Long DM:
Pseudarthrosis of the cervical spine after anterior arthrodesis.
Treatment by posterior nerve-root decompression, stabilization, and
arthrodesis. J Bone Joint Surg Am. 72:1171–1177. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kokubun S and Sato T: (ⅱ) Cervical
myelopathy and its management. Curr Orthop. 12:7–12. 1998.
View Article : Google Scholar
|
|
5
|
Yonenobu K, Fuji T, Ono K, Okada K,
Yamamoto T and Harada N: Choice of surgical treatment for
multisegmental cervical spondylotic myelopathy. Spine. 10:710–716.
1985. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Odate S, Shikata J, Soeda T, Yamamura S
and Kawaguchi S: Surgical results and complications of anterior
decompression and fusion as a revision surgery after initial
posterior surgery for cervical myelopathy due to ossification of
the posterior longitudinal ligament. J Neurosurg Spine. 26:466–473.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ikenaga M, Shikata J and Tanaka C:
Long-term results over 10 years of anterior corpectomy and fusion
for multilevel cervical myelopathy. Spine. 31:1568–1574. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schwab JS, Diangelo DJ and Foley KT:
Motion compensation associated with single-level cervical fusion:
Where does the lost motion go? Spine. 31:2439–2448. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yi S, Shin HC, Kim KN, Park HK, Jang IT
and Yoon DH: Modified techniques to prevent sagittal imbalance
after cervical arthroplasty. Spine. 32:1986–1991. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Edwards CC II, Heller JG and Murakami H:
Corpectomy versus laminoplasty for multilevel cervical myelopathy:
An independent matched-cohort analysis. Spine. 27:1168–1175. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wada E, Suzuki S, Kanazawa A, Matsuoka T,
Miyamoto S and Yonenobu K: Subtotal corpectomy versus laminoplasty
for multilevel cervical spondylotic myelopathy: A long-term
follow-up study over 10 years. Spine. 26:1443–1447. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lee SH, Ahn Y and Lee JH: Laser-assisted
anterior cervical corpectomy versus posterior laminoplasty for
cervical myelopathic patients with multilevel ossification of the
posterior longitudinal ligament. Photomed Laser Surg. 26:119–127.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Herkowitz HN: A comparison of anterior
cervical fusion, cervical laminectomy, and cervical laminoplasty
for the surgical management of multiple level spondylotic
radiculopathy. Spine. 13:774–780. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yonenobu K, Hosono N, Iwasaki M, Asano M
and Ono K: Laminoplasty versus subtotal corpectomy. A comparative
study of results in multisegmental cervical spondylotic myelopathy.
Spine. 17:1281–1284. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Saunders RL, Pikus HJ and Ball P:
Four-level cervical corpectomy. Spine. 23:2455–2461. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Vaccaro AR, Falatyn SP, Scuderi GJ,
Eismont FJ, McGuire RA, Singh K and Garfin SR: Early failure of
long segment anterior cervical plate fixation. J Spinal Disord.
11:410–415. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chen Y, Chen D, Guo Y, Wang X, Lu X, He Z
and Yuan W: Subsidence of titanium mesh cage: A study based on 300
cases. J Spinal Disord Tech. 21:489–492. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hee HT, Majd ME, Holt RT, Whitecloud TR
and Pienkowski D: Complications of multilevel cervical corpectomies
and reconstruction with titanium cages and anterior plating. J
Spinal Disord Tech. 16:1–8. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Majd ME, Vadhva M and Holt RT: Anterior
cervical reconstruction using titanium cages with anterior plating.
Spine. 24:1604–1610. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nakase H, Park YS, Kimura H, Sakaki T and
Morimoto T: Complications and long-term follow-up results in
titanium mesh cage reconstruction after cervical corpectomy. J
Spinal Disord Tech. 19:353–357. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hilibrand AS, Yoo JU, Carlson GD and
Bohlman HH: The success of anterior cervical arthrodesis adjacent
to a previous fusion. Spine. 22:1574–1579. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dmitriev AE, Cunningham BW, Hu N, Sell G,
Vigna F and McAfee PC: Adjacent level intradiscal pressure and
segmental kinematics following a cervical total disc arthroplasty:
An in vitro human cadaveric model. Spine. 30:1165–1172. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Emery SE, Bohlman HH, Bolesta MJ and Jones
PK: Anterior cervical decompression and arthrodesis for the
treatment of cervical spondylotic myelopathy. Two to seventeen-year
follow-up. J Bone Joint Surg Am. 80:941–951. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Robertson JT, Papadopoulos SM and
Traynelis VC: Assessment of adjacent-segment disease in patients
treated with cervical fusion or arthroplasty: A prospective 2-year
study. J Neurosurg Spine. 3:417–423. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Shin DA, Yi S, Yoon DH, Kim KN and Shin
HC: Artificial disc replacement combined with fusion versus
two-level fusion in cervical two-level disc disease. Spine.
34:1153–1159. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ji GY, Oh CH, Shin DA, Ha Y, Yi S, Kim KN,
Shin HC and Yoon DH: Artificial disk replacement combined with
fusion versus 2-level fusion in cervical 2-level disk disease with
a 5-year follow-up. Clin Spine Surg. 30:E620–E627. 2017. View Article : Google Scholar : PubMed/NCBI
|