Ovarian cancer is one of the most lethal
gynecological tumor types with 22,440 new cases and 14,080
associated mortalities reported in 2017 in the USA (1). Surgery is the optimal treatment for
early-stage ovarian cancer, whereas platinum-based chemotherapy
followed by debulking surgery is the standard therapy for advanced
ovarian cancer (2). Although
developments in surgery and chemotherapy have enhanced clinical
outcomes, improvement of the 5-year survival rate of <30% is
required (3). In recent decades, as
the concepts of synthetic lethality and immune escape have emerged
(4,5),
several targeted drugs that differentiate from conditional
chemotherapy have been applied to ovarian cancer treatment. Ovarian
cancer cells, particularly high-grade serious ovarian cancer
(HGSOC) cells, exhibit a high mutation rate of BRCA1 DNA
repair-associated (BRCA1)/BRCA2, which is responsible for
error-free repair of DNA double-strand breaks (DSB), leading to a
homologous recombination defect (HRD) (6). Olaparib, the first inhibitor of the
enzyme poly (ADP-ribose) polymerase (PARP) to be approved by the
USA Food and Drug Administration, was demonstrated to be effective
in BRCA mutation-positive ovarian cancer and was shown to kill HRD
cells via tumor-selective synthetic lethality (7). Bevacizumab, an anti-angiogenic agent
against vascular endothelial growth factor (VEGF), was reported to
successfully improve progression-free survival (PFS) time among
patients with recurrent ovarian cancer. However, no significant
change in the overall survival (OS) time was identified (8). Another class of drugs that attract
attention in cancer treatment are the immunotherapeutic agents,
particularly drugs that inhibit the programmed death-ligand 1
(PD-L1)/programmed death-1 (PD-1) or B7/cytotoxic
T-lymphocyte-associated protein 4 (CTLA-4) pathways. Clinical
studies have suggested that checkpoint blockades can stimulate an
immune response against tumors (9).
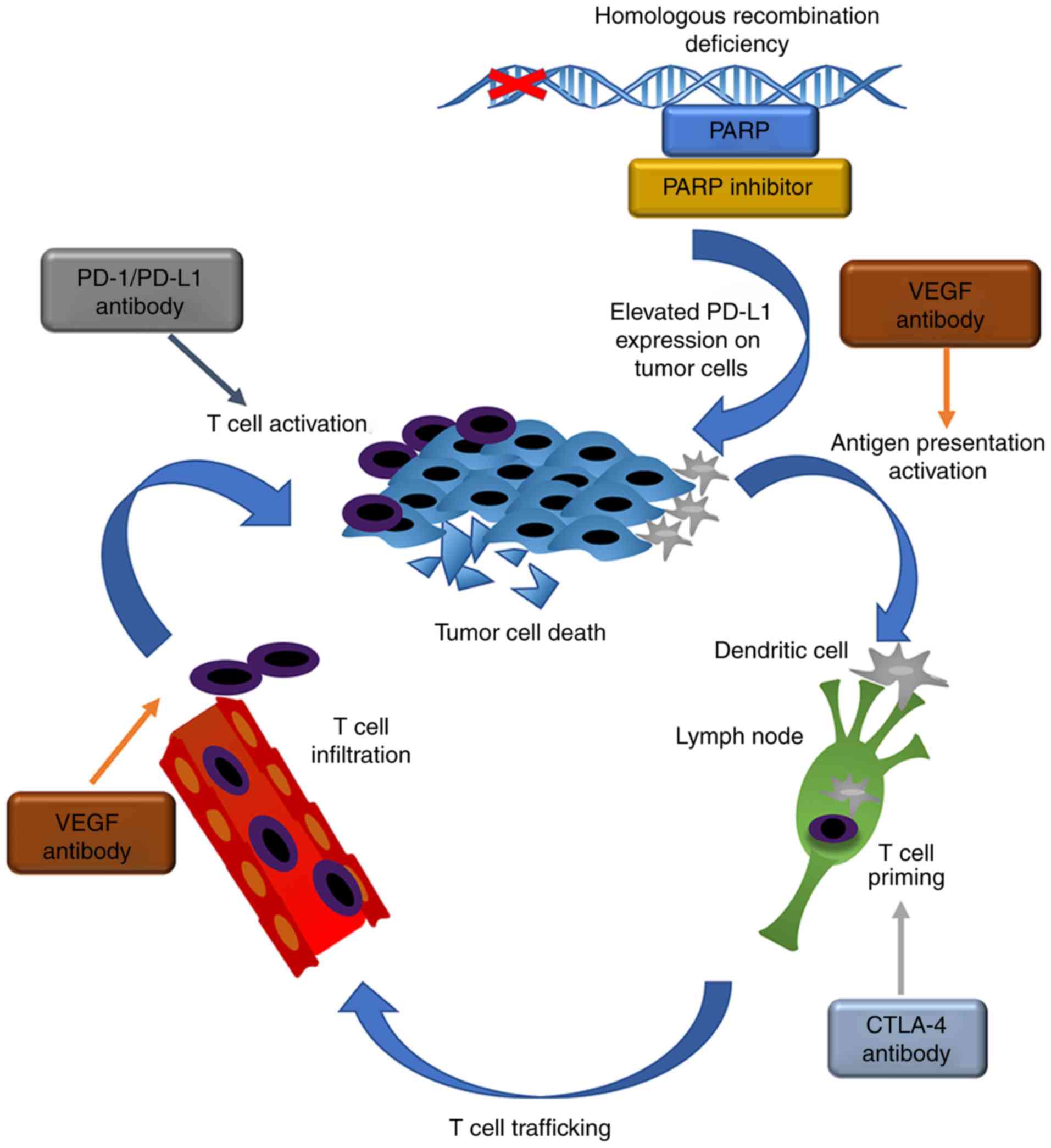
Targeted and checkpoint therapies are associated with the action of
the immune system against the tumor, as presented in Fig. 1. Based on their complementary and
non-overlapping immune responses, the current review outlines novel
combined therapies for the treatment of ovarian cancer (10).
PD-1 is a member of the cluster of differentiation
(CD)28 family and is expressed on the surface of activated T cells,
B cells, dendritic cells and macrophages. PD-L1, a ligand of PD-1,
is a member of the B7 family and is highly expressed in a broad
range of malignant tumor types. It has been demonstrated that the
interaction between PD-1 and PD-L1 negatively regulates T-cell
proliferation, tumor killing and cytokine secretion, and enhances
the number of regulatory T cells (Tregs), resulting in the
maintenance of self-tolerance, as well as cancer progression
(11–14). In a mouse ovarian model, compared with
ovarian cells overexpressing PD-L1, a PD-L1-deleted ovarian cell
line exhibited a higher number of cytotoxic lymphocytes and an
improved prognosis (15). Several
studies have demonstrated that ovarian cancer is an immunogenic
tumor. It was shown that patients with increased intraepithelial
CD8+ T-cell infiltration and a higher
CD8+/CD4+ T-cell ratio exhibited improved OS,
with a median survival time of 55 months, compared with that in
patients with lower frequencies of T cells (26 months) (16). Poor OS and PFS in patients are
associated with high expression levels of PD-L1 in tumor cells
(17). Small interfering RNA has been
utilized to downregulate PD-L1 expression in dendritic cells, which
significantly increases the proportion of memory-like T cells in
mouse bone, as well as tumor specific CD8+ T cells,
demonstrating that the PD-1/PD-L1 pathway influences the immune
system directly (18).
In 2010, the first phase I clinical trial of the
anti-PD-1 antibody nivolumab (a fully human immunoglobulin G4
monoclonal antibody), with a dose ranging from 0.3 to 10 mg/kg, was
administered to 39 patients with solid tumors, including advanced
melanoma, non-small cell lung cancer, renal cell carcinoma (RCC),
prostate cancer and colorectal cancer (19). The response rate was 7.7%, and
nivolumab demonstrated good tolerance, as only one serious adverse
event of inflammatory colitis occurred in a patient with melanoma
who received five doses at 1 mg/kg. In 2012, a phase Ib study of
anti-PD-L1 antibody in patients with advanced solid tumors
demonstrated clinical benefit against ovarian cancer (20). Among 17 patients with ovarian cancer,
16 patients receiving 10 mg/kg exhibited a partial response, of the
16 patients, one patient exhibited a partial response, and 3
patients demonstrated stable disease for ≥24 weeks. On the basis of
the aforementioned clinical data, the first clinical trial to
explore the effects of nivolumab against ovarian cancer was
conducted by Hamanishi et al (21). Among 20 patients with
platinum-resistant ovarian cancer, 2 patients exhibited a durable
complete response (in the 3 mg/kg cohort) and 1 patient exhibited a
partial response (in the 1 mg/kg cohort). The disease control rate
in all 20 patients was 45% and the median PFS time was 3.5 months.
However, drug-associated treatment-emergent adverse events (TEAEs)
occurred in 19 of the 20 patients (95%). Among them, 8 patients
(40%) experienced adverse events of grade 3 or 4, including
hypothyroidism, lymphocytopenia, fever, arrhythmia, arthralgia, and
increased alanine aminotransferase and aspartate aminotransferase
levels. In an ongoing phase Ib study of avelumab, an anti-PD-L1
antibody, data from 23 patients with recurrent or refractory
ovarian cancer were analyzed (22). A
total of 4 patients experienced a partial response, 2 patients
exhibited >30% tumor remission and the median PFS was 11.9
weeks. TEAEs occurred in 18 patients (78.3%) and 2 patients (8.7%)
experienced grade ≥3 drug-associated TEAEs, including increased
lipase and creatine kinase levels, and autoimmune myositis, which
led to treatment discontinuation. No patient experienced serious
drug-associated TEAEs. The most commonly reported drug-associated
TEAEs included fatigue, nausea and diarrhea. In one previous case
report, a patient with radiation- and chemotherapy-resistant HGSOC
demonstrated a notable complete response to the anti-PD1 immune
checkpoint inhibitor pembrolizumab (23).
PD-1/PD-L1 pathway inhibitors are commonly used for
patients with advanced ovarian cancer, or for patients where
chemotherapy or radiotherapy failed to demonstrate an effect.
However, a major limitation of immunotherapy is the extent of
disease burden, which keeps the antitumor efficacy in check
(24). Therefore, a combination of
agents targeting the PD-1/PD-L1 pathway and other cancer pathways,
may offer a promising novel therapy against ovarian cancer in the
future.
In the process of tumor killing, B7-1 (CD80) and
B7-2 (CD86) on antigen-presenting cells bind to CD28 on T cells and
serve a crucial role in the activation of the T cells, When the two
molecules bind together, it evokes the proliferation of the T cells
(24). CTLA-4 is a CD28 homolog with
stronger binding affinity to B7 and is expressed predominantly on T
cells, including Tregs (25). In
contrast to initiating immune activation, CTLA-4 binding to B7
produces a negative signal that suppresses the immune system
(26). The proportion of CD28:B7
binding compared with CTLA-4:B7 binding regulates whether the T
cells undergo activation or suppression (27). The use of CTLA-4 inhibitors to reverse
T-cell suppression is a promising therapy to promote the activation
of immune cells against tumors. As demonstrated in an in
vivo experiment, CTLA-4 inhibitors exhibit a capacity to
improve the effect of chemotherapy and reverse the tumor
suppressive environment in mice (28). In 2003, a CTLA-4-blocking antibody,
ipilimumab, was administered to 7 patients with melanoma and 2
patients with ovarian carcinoma who had previously accepted
therapeutic vaccine (29). Of the 2
patients with ovarian carcinoma, 1 patient exhibited a 43%
reduction in the ovarian tumor marker cancer antigen (CA)-125 in
the blood, beginning 2 months after treatment. However, this effect
was not sustained. The other patient demonstrated a rapid increase
in CA-125 levels upon treatment, but achieved a plateau 1 month
after the infusion.
In order to acquire more information regarding the
toxicity and antitumor effects of the CTLA-4 antibody ipilimumab, 9
patients with stage IV ovarian carcinoma were recruited (30). Each patient had received the same
therapeutic vaccine and the same dose of ipilimumab. The data
demonstrated that 3 patients achieved stable disease for 2, 4 or
>6 months. Among the patients, 1 patient who was treated with an
initial dose of ipilimumab achieved a significant drop in CA-125
level. Although the level was not maintained, a second infusion led
to a more rapid decrease in CA-125 level. Furthermore, hepatic
metastasis regressed gradually and CA-125 was sustained at a low
level when an additional nine infusions of ipilimumab were
administered over almost 4 years. The occurrence of a grade 1 rash
was the only adverse event in this patient, whereas grade 3
diarrhea was observed in 2 other patients (22.2%) and 1 patient
(11.1%) developed Sweet's syndrome accompanied with tumor
progression.
Due to the involvement of different ligands and
functions, combinatorial targeting of PD-1/PD-L1 and CTLA-4
exhibited synergistic antitumor activity in a mouse model of colon
adenocarcinoma (31). In a clinical
trial, accumulating evidence revealed that patients with combined
therapy demonstrated a higher overall response rate (ORR) and
longer PFS time. However, the number of TEAEs that occurred
following combined therapy increased significantly compared with
that following single therapy (32,33).
Therefore, there is a requirement to identify agents that exhibit a
synergistic effect with checkpoint pathway inhibitors, but do not
increase the number or severity of TEAEs.
PARP inhibitors have been widely studied in HGSOCs
with either germline or somatic mutations of BRCA1/BRCA2. Clinical
trial data have suggested that olaparib, 400 mg twice daily, can
exhibit a significant antitumor effect in patients who are
confirmed to be either platinum-sensitive or platinum-resistant
(34,35). Compared with those patients who
received a placebo and experienced a median PFS time of 5.5 months,
the patients undergoing olaparib treatment experienced a
significantly increased PFS time, with a median of 19.1 months. The
most common adverse events were anemia, abdominal pain and
intestinal obstruction. Certain patients with HGSOC undergoing
olaparib maintenance therapy attained a long-term (LT) response
that lasted >2 years. Germline or somatic BRCA1/BRCA2 mutations
were correlated with LT response (36). However, even for patients with
wild-type BRCA, the median PFS time improved moderately compared
with that in the placebo group (7.4 vs. 5.5 months) (37). In another study, niraparib, a
selective inhibitor of PARP-1/2, was administered to patients with
platinum-sensitive, recurrent ovarian cancer by maintenance therapy
(38). Those receiving niraparib
exhibited a longer PFS time compared with those receiving placebo,
regardless of the presence or absence of BRCA mutations or the HRD
status. However, there remains a substantial number of patients
with mutations that resist this agent (39).
With advancements in preclinical and clinical
trials, the mechanisms involved in PARP inhibitor resistance have
been partly uncovered (40). The most
common mechanism of resistance is non-homologous end-joining
(NHEJ), which competes with homologous recombination (HR) in the
process of DSB repair (41).
MicroRNA-622 (miR-622) serves a pivotal role in the modulation of
the competing association between HR and NHEJ. As demonstrated in
an in vitro experiment, miR-622 mitigates the effect of PARP
inhibition and platinum in BRCA1-mutant cells (42). Furthermore, data from The Cancer
Genome Atlas suggests that overexpression of miR-622 is associated
with PFS and OS among patients with BRCA1 mutation and BRCA1
hypermethylation (42). In certain
cases, BRCA-2 mutant cells can undergo a secondary mutation and
restore the capacity of the BRCA-2 functional protein that repairs
DNA damage in PARP, which results in tolerance to PARP inhibitors
(43).
Although significant clinical benefits have been
achieved using PARP inhibitor therapy for BRCA1/BRCA2-mutated
ovarian cancer, associated resistance remains the main challenge to
overcome. Therefore, the combination of PARP inhibitors with other
agents may be a useful strategy to overcome this problem.
Angiogenesis has been confirmed as an effective
target for therapy in several tumor types, including ovarian
cancer, renal cell carcinoma and pancreatic cancer (44). The VEGF family and their cognate
receptors, the angiopoietin family of ligands, are the main
elements that contribute to tumor angiogenesis (45,46). VEGF
serves a critical role in the progression of ovarian cancer,
ascites formation and the metastasis of tumor cells (47). Increasing evidence indicates that
ovarian cancer cells exhibit high expression of VEGF and VEGF
receptor (VEGFR), which are associated with ovarian cancer
development and progression (48).
Bevacizumab, a humanized recombinant anti-VEGF monoclonal antibody
has been applied in the treatment of recurrent ovarian cancer.
Clinical data revealed no significant difference in the median PFS
time of patients treated by chemotherapy compared with the median
PFS time of patients treated with a combination of chemotherapy and
bevacizumab followed by maintenance chemotherapy (10.3 vs. 11.2
months) (8,49). However, the bevacizumab-treatment
group exhibited a prolonged median PFS time of 14.1 months. The
benefit is greater with respect to patients at high risk for
disease progression. Patients with platinum-sensitive and
-resistant cancer exhibited improved PFS and ORR times when treated
with bevacizumab therapy (50,51).
Cediranib, an oral inhibitor of VEGFR1-3 and c-Kit7, when combined
with chemotherapy and followed by a maintenance therapy, yielded a
significant improvement in PFS time among women with recurrent,
platinum-sensitive ovarian cancer. The predominant cause for
discontinuation of the therapy was an increase in dose-associated
toxicity (52).
Although the target of anti-angiogenic agents is
genetically stable, drug tolerance cases have been observed in
pre-clinical and clinical settings. The most common drug resistance
mechanisms are associated with the evasion of anti-angiogenic
agents, as well as pre-existing indifference to anti-angiogenic
agents (44,53). In addition, the immune situation
appears to be associated with the anti-angiogenic effect. Groups
with immune gene upregulation have been demonstrated to repress
angiogenesis-associated gene expression and exhibit an improved OS
time (54).
An increasing number of studies have indicated that
targeted therapies are able to stimulate the immune response of the
host. Therefore, acknowledging the immunological effect of targeted
drugs, as well as the crosslink between immunotherapy and targeted
therapy, may provide improved combined therapy for patients with
cancer (55). Ovarian cancer with
BRCA1/2 mutation has been identified as a rational candidate for
immunotherapy and targeted therapy (56). In HGSOC, tumors harboring
HR-deficient/BRCA1/2 mutations demonstrated a higher neoantigen
load and increased numbers of CD3+ and CD8+
tumor-infiltrating lymphocytes (TILs) (57). Elevated levels of PD-1 and PD-L1
expression on tumor-infiltrating immune cells was also observed
compared with that in HR-proficient tumors, which indicated that
BRCA1/2-mutated HGSOCs may be more sensitive to PD-1/PD-L1
inhibitors compared with HR-proficient HGSOCs. It has been
suggested that increased expression levels of PD-1/CTLA-4
attenuates cytotoxic T lymphocytes. Cisplatin treatment coupled
with dual PD-L1 antibody and CTLA-4 antibody therapy substantially
augmented antitumor immunity in BRCA1-deficient mice, producing a
systemic immune response (57). This
response consisted of enhanced dendritic cell activation and
reduced number of suppressive forkhead box P3+ Tregs,
and was augmented in the activation of tumor-infiltrating cytotoxic
CD8+ and CD4+ T cells. A previous study
demonstrated that melanoma patients with somatic mutations and
higher levels of tumor neoantigen are more susceptible to
anti-CTLA-4 treatment (58). Higuchi
et al (59) identified that a
combination of CTLA-4 antibody and PARP inhibitors can enhance
T-cell function and increase the amount of novel lymphocyte clones,
resulting in a lasting and improved anti-ovarian cancer effect. In
addition, increased levels of interferon-γ (IFN-γ) induced by
combined therapy, amplified the therapeutic benefit. Another
checkpoint inhibitor, anti-PD-1 antibody, did not demonstrate any
significant effect on survival when co-administrated with PARP
inhibitor. This unexpected result may be due to a lack of
activation of lymphocytes, rather than the reversal of T-cell
suppression. An in vivo study revealed that incorporation
with PD-L1 blockade can sensitize patients to PARP inhibitor
therapy (60). Furthermore, in
contrast to each treatment alone, no increase in serious
complications occurred. Jiao et al (60) identified that when the breast cancer
MDA-MB-231 cell line was exposed to PARP inhibitor, the surface
expression level of PD-L1 was upregulated, as expected. PARP
inhibitors led to an increased level of PD-L1 expression through
deactivation of glycogen synthase kinase 3β (GSK3β), and elevated
PD-L1 expression attenuated T-cell function and weakened the effect
of PARP inhibitors against cancer.
A BR5-AKT (BRCA1-deficient) tumor model exhibited a
high level of Akt activation that inhibited GSK3β (61), which may have masked the function of
PARP inhibitor. Therefore, a suitable ovarian cancer model is
critical to identify the synergistic effect of PD-L1 blockade and
PARP inhibitor. In a case report, a 38-year-old woman with
platinum-refractory advanced ovarian adenosquamous carcinoma, who
failed to respond to prior multiline chemotherapies and
anti-angiogenic agents, received significant clinical benefit from
a combination of targeted therapy (olaparib and pazopanib) and PD-1
inhibitors (pembrolizumab and nivolumab). The patient survived for
>15 months and took nivolumab as maintenance therapy (62). A phase I study to evaluate the safety
and efficacy of the combination of PARP inhibitor and anti-CTLA-4
antibody was conducted in women with BRCA mutation-associated
recurrent ovarian cancer (63). No
dose-limiting toxicities were identified and grade 1/2 toxicities
were almost consistent with prior studies that used immune
checkpoint inhibitors. Furthermore, all patients who received the
combined therapy demonstrated a decrease in tumor size and CA-125
levels.
Based on the aforementioned discussion, the
combination of PARP inhibitor and PD-L1 blockade can enhance the
antitumor effect without an increase in serious complications. This
supports the power of combined therapy by maximizing treatment
response while minimizing toxicity.
Combinational therapy of bevacizumab and cisplatin
was applied to a xenograft ovarian cancer model, and the antitumor
efficacy of cisplatin was demonstrated to be amplified (64). In addition to possessing proangiogenic
properties, VEGF-A serves a critical role in the immunosuppressive
tumor environment, as it is associated with an inhibition of
dendritic cell maturation, an accumulation of myeloid-derived
suppressor cells (MDSCs) and an induction of Tregs (65,66).
Furthermore, PD-1 and CTLA-4 have been verified to be expressed by
these cells in the tumor microenvironment (67).
Previous studies have observed that VEGF enhances
the expression of PD-1 expression on intratumoral CD8+ T
cells, which could be downregulated via VEGF antibody (68,69).
Combined application of anti-PD-1 and VEGF-A blockade produces a
stronger and synergistic antitumor effect in tumors with high
expression of VEGF, compared with sole therapy (70). In patients with metastatic RCC who
received VEGF-targeting agents, an inverse correlation was
identified between high PD-L1 expression level and poor survival
time (71). In addition, VEGF can
upregulate other inhibitory receptors, including T-cell
immunoglobulin and mucin domain 3, CTLA-4 and lymphocyte-activation
gene 3, in a dose-dependent manner (68). CTLA-4 is highly associated with tumor
angiogenesis. Following treatment with ipilimumab, patients with
high serum levels of VEGF experience a poor prognosis (72).
The tumor vascular structure also inhibits the
expression of adhesion molecules, including E-selectin,
intracellular adhesion molecule 1 (ICAM1) and vascular cell
adhesion protein 1 (VCAM1), which limits the transmigration of TILs
(73). Administering ipilimumab in
combination with bevacizumab was revealed to increase T-cell
infiltration and the expression levels of ICAM1 and VCAM1 in
patients with advanced melanoma, in addition to enhancing T-cell
accumulation, furthermore, specific cytokines that are critical to
tumor inhibition, including C-C-C motif chemokine 10, tumor
necrosis factor-α (TNF-α) and interleukin 1-α, were significantly
increased following combined ipilimumab and bevacizumab therapy
(74). Certain subgroups of patients
with combined therapy even developed increased levels of antibody
against Gal-1, which is known to promote tumor growth and
progression, patients with elevated antibodies to Gal-1 exhibit
favorable overall survival and improved clinical outcomes (74,75).
In a phase I trial, high serum levels of
angiopoietin-2 (ANGPT2) contributed to tumor angiogenesis
correlated with a poor survival and reduced response in patients
who underwent immunotherapy (76).
ANGPT2 was revealed to induce PD-L1 expression in tumor-associated
macrophages and weaken the efficiency of immunotherapy.
Furthermore, ipilimumab plus bevacizumab treatment downregulated
ANGPT2 expression in sera and in tumors (77). The close association between
angiogenesis ability and checkpoint protein expression suggests
that the combination of anti-angiogenic and checkpoint treatment
may complement each other's limitations and provide novel treatment
strategies for ovarian cancer. In 2017, Lee et al (78) initiated a clinical trial to evaluate
the antitumor effect of the PD-1 inhibitor durvalumab in
combination with endothelial growth factor receptor 1–3 inhibitor
cediranib or PARP inhibitor olaparib in women with cancer. A total
of 9 patients with ovarian cancer were recruited to the durvalumab
plus cediranib arm, in addition to 14 patients with gynecological
or breast cancer types. The data suggested that 6 patients with
ovarian cancer achieved a partial response for >5 to >8
months and a 50% ORR, which is higher compared with that recorded
for PD-L1 pathway inhibition (ORR range, 10–20%) (21) or cediranib treatment alone (23% ORR)
(79). However, treatment with
durvalumab plus cediranib was associated with a higher frequency of
TEAEs. A total of 7 patients suffered from grade 2–4 adverse events
and 1 patient experienced grade 3 pulmonary hypertension and
eventually succumbed.
In the context of the immune microenvironment, a
combined treatment of VEGF blockade and checkpoint blockade is a
double-edged sword, as it may increase the tumor-killing effect and
the associated adverse events. Therefore, the safety of combined
therapy in ovarian cancer should be confirmed in larger clinical
trials.
The current review provided a perspective regarding
the co-administration of targeted therapy and immunotherapy in
ovarian cancer treatment. Targeted therapy is capable of initiating
T-cell activation and infiltration, which serves a central role in
immunotherapy. High PD-L1 expression is closely associated with a
poor prognosis in targeted therapy. PARP inhibitor has been proven
to modulate the immune response against an ovarian cancer model
with BRCA1 mutation (80). In
particular, the amount of peritoneal CD8+ T cells, NK
cells, and their production of IFN-γ and TNF-α increases
significantly, whereas the percentage of immunosuppressive MDSCs
and Tregs decreases following PARP inhibitor therapy. These results
conclude that a synergic effect of immune checkpoint blockade in
combination with PARP inhibitor is promising. Potent
anti-angiogenic treatment also can promote PD-L1 expression and
hypoxia, which disables antigen-presenting cells and weakens the
activation of T cells. By contrast, elevated serum levels of CTLA-4
have been reported to promote a higher risk of invasive and
metastatic potential, a poor response to anti-VEGF therapy, a poor
prognosis and a shorter overall survival time (81).
There are clear advantages of combined
administration, including the generation of a regime where targeted
therapy improves positive immune activation that could further
accelerate checkpoint blockade. One additional consideration is
whether adding checkpoint inhibition may reverse the
immunosuppressive condition of targeted therapy. In certain in
vivo experiments with BRCA1 mutation, only the concurrent
administration of CTLA-4 antibody and PAPP inhibitor elicited dual
antitumor effectiveness, and PD-1 antibody failed to demonstrate
the same effect as CTLA-4 antibody (59). Combination therapy with two agents
attracts research into the potential mechanisms involved. Testing
various combinations of targeted treatment with immunotherapy has
been performed in numerous clinical trials. The main challenge of
combinational therapy is the potential of dual toxicity.
Furthermore, the biological and immune system in a mouse model does
not completely mimic human cancer. Therefore, there is a lack of
evidence on the response to many different combined therapies
(82). Understanding
immune-associated mechanisms of the targeted pathways may benefit
the development of safer combined therapies. Additionally, there
are a number of ongoing clinical trials that are evaluating the
effect of combined targeted therapy and immunotherapy in ovarian
cancer (Table I).
In conclusion, the potential adverse effects of
combination therapy and the choice of targeted therapy that may be
most effective with a checkpoint antibody requires consideration
when applying in a clinical setting.
Not applicable.
This study was supported by the National Natural
Science Funds (grant no. 81571455) the Projects of the Ministry of
Science and Technology (grant nos. 2015DFR31070 and 2012DFA30490),
the Special Plan of Clinical Medicine Development of Beijing
Medical Administration Bureau (grant no. ZYLX201713) and the
Ministry of Science and Technology (grant nos. 2017YFC1001204 and
2016YFC1000100).
Not applicable.
GZ and ZZ analyzed and interpreted the review. GZ
collected the references and wrote the review and CL revised the
article. The authors Hb, GC and RC contribute to the acquisition of
data and ZZ designed the review. All authors read and approved the
final manuscript.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2017. CA Cancer J Clin. 67:7–30. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Orr B and Edwards RP: Diagnosis and
treatment of ovarian cancer. Hematol Oncol Clin North Am.
32:943–964. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ashworth A: A synthetic lethal therapeutic
approach: Poly(ADP) ribose polymerase inhibitors for the treatment
of cancers deficient in DNA double-strand break repair. J Clin
Oncol. 26:3785–3790. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Beatty GL and Gladney WL: Immune escape
mechanisms as a guide for cancer immunotherapy. Clin Cancer Res.
21:687–692. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Eskander RN and Tewari KS: PARP inhibition
and synthetic lethality in ovarian cancer. Expert Rev Clin
Pharmacol. 7:613–622. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lord CJ and Ashworth A: PARP inhibitors:
Synthetic lethality in the clinic. Science. 355:1152–1158. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Burger RA, Brady MF, Bookman MA, Fleming
GF, Monk BJ, Huang H, Mannel RS, Homesley HD, Fowler J, Greer BE,
et al: Incorporation of bevacizumab in the primary treatment of
ovarian cancer. N Engl J Med. 365:2473–2483. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Postow MA, Callahan MK and Wolchok JD:
Immune checkpoint blockade in cancer therapy. J Clin Oncol.
33:1974–1982. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hughes PE, Caenepeel S and Wu LC: Targeted
therapy and checkpoint immunotherapy combinations for the treatment
of cancer. Trends Immunol. 37:462–476. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zou W and Chen L: Inhibitory B7-family
molecules in the tumour microenvironment. Nat Rev Immunol.
8:467–477. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hamid O, Robert C, Daud A, Hodi FS, Hwu
WJ, Kefford R, Wolchok JD, Hersey P, Joseph RW, Weber JS, et al:
Safety and tumor responses with lambrolizumab (anti-PD-1) in
melanoma. N Engl J Med. 369:134–144. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Freeman GJ, Long AJ, Iwai Y, Bourque K,
Chernova T, Nishimura H, Fitz LJ, Malenkovich N, Okazaki T, Byrne
MC, et al: Engagement of the PD-1 immunoinhibitory receptor by a
novel B7 family member leads to negative regulation of lymphocyte
activation. J Exp Med. 192:1027–1034. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Francisco LM, Salinas VH, Brown KE,
Vanguri VK, Freeman GJ, Kuchroo VK and Sharpe AH: PD-L1 regulates
the development, maintenance, and function of induced regulatory T
cells. J Exp Med. 206:3015–3029. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Abiko K, Mandai M, Hamanishi J, Yoshioka
Y, Matsumura N, Baba T, Yamaguchi K, Murakami R, Yamamoto A, Kharma
B, et al: PD-L1 on tumor cells is induced in ascites and promotes
peritoneal dissemination of ovarian cancer through CTL dysfunction.
Clin Cancer Res. 19:1363–1374. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sato E, Olson SH, Ahn J, Bundy B,
Nishikawa H, Qian F, Jungbluth AA, Frosina D, Gnjatic S, Ambrosone
C, et al: Intraepithelial CD8+ tumor-infiltrating lymphocytes and a
high CD8+/regulatory T cell ratio are associated with favorable
prognosis in ovarian cancer. Proc Natl Acad Sci USA.
102:18538–18543. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hamanishi J, Mandai M, Iwasaki M, Okazaki
T, Tanaka Y, Yamaguchi K, Higuchi T, Yagi H, Takakura K, Minato N,
et al: Programmed cell death 1 ligand 1 and tumor-infiltrating CD8+
T lymphocytes are prognostic factors of human ovarian cancer. Proc
Natl Acad Sci USA. 104:3360–3365. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cubillos-Ruiz JR, Engle X, Scarlett UK,
Martinez D, Barber A, Elgueta R, Wang L, Nesbeth Y, Durant Y,
Gewirtz AT, et al: Polyethylenimine-based siRNA nanocomplexes
reprogram tumor-associated dendritic cells via TLR5 to elicit
therapeutic antitumor immunity. J Clin Invest. 119:2231–2244.
2009.PubMed/NCBI
|
|
19
|
Brahmer JR, Drake CG, Wollner I, Powderly
JD, Picus J, Sharfman WH, Stankevich E, Pons A, Salay TM, McMiller
TL, et al: Phase I study of single-agent anti-programmed death-1
(MDX-1106) in refractory solid tumors: Safety, clinical activity,
pharmacodynamics, and immunologic correlates. J Clin Oncol.
28:3167–3175. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Taneja SS: Re: Safety and activity of
Anti-PD-L1 antibody in patients with advanced cancer. J Urol.
188:2148–2149. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hamanishi J, Mandai M, Ikeda T, Minami M,
Kawaguchi A, Murayama T, Kanai M, Mori Y, Matsumoto S, Chikuma S,
et al: Safety and antitumor activity of anti-PD-1 antibody,
nivolumab, in patients with platinum-resistant ovarian cancer. J
Clin Oncol. 33:4015–4022. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Disis ML, Patel MR, Pant S, Infante JR,
Lockhart AC, Kelly K, Beck JT, Gordon MS, Weiss GJ, Ejadi S, et al:
Avelumab (MSB0010718C), an anti-PD-L1 antibody, in patients with
previously treated, recurrent or refractory ovarian cancer: A phase
Ib, open-label expansion trial. J Clin Oncol. 5509:2015.
|
|
23
|
Bellone S, Buza N, Choi J, Zammataro L,
Gay L, Elvin J, Rimm DL, Liu Y, Ratner ES, Schwartz PE and Santin
AD: Exceptional response to pembrolizumab in a metastatic,
chemotherapy/radiation-resistant ovarian cancer patient harboring a
PD-L1-genetic rearrangement. Clin Cancer Res. 24:3282–3291. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tse BW, Collins A, Oehler MK, Zippelius A
and Heinzelmann-Schwarz VA: Antibody-based immunotherapy for
ovarian cancer: Where are we at? Ann Oncol. 25:322–331. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chen L and Flies DB: Molecular mechanisms
of T cell co-stimulation and co-inhibition. Nat Rev Immunol.
13:227–242. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chambers CA, Kuhns MS, Egen JG and Allison
JP: CTLA-4-mediated inhibition in regulation of T cell responses:
Mechanisms and manipulation in tumor immunotherapy. Annu Rev
Immunol. 19:565–594. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Krummel MF and Allison JP: CD28 and CTLA-4
have opposing effects on the response of T cells to stimulation. J
Exp Med. 182:459–465. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lesterhuis WJ, Salmons J, Nowak AK, Rozali
EN, Khong A, Dick IM, Harken JA, Robinson BW and Lake RA:
Synergistic effect of CTLA-4 blockade and cancer chemotherapy in
the induction of anti-tumor immunity. PLoS One. 8:e618952013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hodi FS, Mihm MC, Soiffer RJ, Haluska FG,
Butler M, Seiden MV, Davis T, Henry-Spires R, MacRae S, Willman A,
et al: Biologic activity of cytotoxic T lymphocyte-associated
antigen 4 antibody blockade in previously vaccinated metastatic
melanoma and ovarian carcinoma patients. Proc Natl Acad Sci USA.
100:4712–4717. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hodi FS, Butler M, Oble DA, Seiden MV,
Haluska FG, Kruse A, Macrae S, Nelson M, Canning C, Lowy I, et al:
Immunologic and clinical effects of antibody blockade of cytotoxic
T lymphocyte-associated antigen 4 in previously vaccinated cancer
patients. Proc Natl Acad Sci USA. 105:3005–3010. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Korman A, Chen B, Wang C, Wu L, Cardarelli
P and Selby M: Activity of Anti-PD-1 in murine tumor models: Role
of ‘host’ PD-L1 and synergistic effect of anti-PD-1 and
anti-CTLA-4. J Immunol. 178:2007.
|
|
32
|
Postow MA, Chesney J, Pavlick AC, Robert
C, Grossmann K, McDermott D, Linette GP, Meyer N, Giguere JK,
Agarwala SS, et al: Nivolumab and ipilimumab versus ipilimumab in
untreated melanoma. N Engl J Med. 372:2006–2017. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Larkin J, Chiarion-Sileni V, Gonzalez R,
Grob JJ, Cowey CL, Lao CD, Schadendorf D, Dummer R, Smylie M,
Rutkowski P, et al: Combined nivolumab and ipilimumab or
monotherapy in untreated melanoma. N Engl J Med. 373:23–34. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Audeh MW, Carmichael J, Penson RT,
Friedlander M, Powell B, Bell-McGuinn KM, Scott C, Weitzel JN,
Oaknin A, Loman N, et al: Oral poly(ADP-ribose) polymerase
inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and
recurrent ovarian cancer: A proof-of-concept trial. Lancet.
376:245–251. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Pujadelauraine E, Ledermann JA, Selle F,
Gebski V, Penson RT, Oza AM, Korach J, Huzarski T, Poveda A,
Pignata S, et al: Olaparib tablets as maintenance therapy in
patients with platinum-sensitive, relapsed ovarian cancer and a
BRCA1/2 mutation (SOLO2/ENGOT-Ov21): A double-blind, randomised,
placebo-controlled, phase 3 trial. Lancet Oncol. 18:1274–1284.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Lheureux S, Lai Z, Dougherty BA, Runswick
S, Hodgson DR, Timms KM, Lanchbury JS, Kaye S, Gourley C, Bowtell
D, et al: Long-term responders on olaparib maintenance in
high-grade serous ovarian cancer: Clinical and molecular
characterization. Clin Cancer Res. 23:4086–4094. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ledermann J, Harter P, Gourley C,
Friedlander M, Vergote I, Rustin G, Scott CL, Meier W,
Shapira-Frommer R, Safra T, et al: Olaparib maintenance therapy in
patients with platinum-sensitive relapsed serous ovarian cancer: A
preplanned retrospective analysis of outcomes by BRCA status in a
randomised phase 2 trial. Lancet Oncol. 15:852–861. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Mirza MR, Monk BJ, Herrstedt J, Oza AM,
Mahner S, Redondo A, Fabbro M, Ledermann JA, Lorusso D, Vergote I,
et al: Niraparib maintenance therapy in platinum-sensitive,
recurrent ovarian cancer. N Engl J Med. 375:2154–2164. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Lim JSJ and Tan DSP: Understanding
resistance mechanisms and expanding the therapeutic utility of PARP
inhibitors. Cancers (Basel). 9:E1092017. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Bouwman P and Jonkers J: Molecular
pathways: How can BRCA-mutated tumors become resistant to PARP
inhibitors? Clin Cancer Res. 20:540–547. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Deriano L and Roth DB: Modernizing the
nonhomologous end-joining repertoire: Alternative and classical
NHEJ share the stage. Annu Rev Genet. 47:433–455. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Choi YE, Meghani K, Brault ME, Leclerc L,
He YJ, Day TA, Elias KM, Drapkin R, Weinstock DM, Dao F, et al:
Platinum and PARP inhibitor resistance due to overexpression of
MicroRNA-622 in BRCA1-mutant ovarian cancer. Cell Rep. 14:429–439.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Lord CJ and Ashworth A: Mechanisms of
resistance to therapies targeting BRCA-mutant cancers. Nat Med.
19:1381–1388. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Jayson GC, Kerbel R, Ellis LM and Harris
AL: Antiangiogenic therapy in oncology: Current status and future
directions. Lancet. 388:518–529. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Ferrara N and Kerbel RS: Angiogenesis as a
therapeutic target. Nature. 438:967–974. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Monk BJ, Poveda A, Vergote I, Raspagliesi
F, Fujiwara K, Bae DS, Oaknin A, Ray-Coquard I, Provencher DM,
Karlan BY, et al: Anti-angiopoietin therapy with trebananib for
recurrent ovarian cancer (TRINOVA-1): A randomised, multicentre,
double-blind, placebo-controlled phase 3 trial. Lancet Oncol.
15:799–808. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Bekes I, Friedl TW, Köhler T, Möbus V,
Janni W, Wöckel A and Wulff C: Does VEGF facilitate local tumor
growth and spread into the abdominal cavity by suppressing
endothelial cell adhesion, thus increasing vascular peritoneal
permeability followed by ascites production in ovarian cancer? Mol
Cancer. 15:132016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Graybill W, Sood AK, Monk BJ and Coleman
RL: State of the science: Emerging therapeutic strategies for
targeting angiogenesis in ovarian cancer. Gynecol Oncol.
138:223–226. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Perren TJ, Swart AM, Pfisterer J,
Ledermann JA, Pujade-Lauraine E, Kristensen G, Carey MS, Beale P,
Cervantes A, Kurzeder C, et al: A phase 3 trial of bevacizumab in
ovarian cancer. N Engl J Med. 365:2484–2496. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Moore KN, Di Silvestro P, Lowe ES, Garnett
S and Pujade-Lauraine E: SOLO1 and SOLO2: Randomized phase III
trials of olaparib in patients (pts) with ovarian cancer and a
BRCA1/2 mutation (BRCAm). J Clin Oncol. 32:2014. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Aghajanian C, Blank SV, Goff BA, Judson
PL, Teneriello MG, Husain A, Sovak MA, Yi J and Nycum LR: OCEANS: A
randomized, double-blind, placebo-controlled phase III trial of
chemotherapy with or without bevacizumab in patients with
platinum-sensitive recurrent epithelial ovarian, primary
peritoneal, or fallopian tube cancer. J Clin Oncol. 30:2039–2045.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Ledermann JA, Embleton AC, Raja F, Perren
TJ, Jayson GC, Rustin GJS, Kaye SB, Hirte H, Eisenhauer E, Vaughan
M, et al: Cediranib in patients with relapsed platinum-sensitive
ovarian cancer (ICON6): A randomised, double-blind,
placebo-controlled phase 3 trial. Lancet. 387:1066–1074. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Bergers G and Hanahan D: Modes of
resistance to anti-angiogenic therapy. Nat Rev Cancer. 8:592–603.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Gourley C, Mccavigan A, Perren T, Paul J,
Michie CO, Churchman M, Williams A, McCluggage WG, Parmar M, Kaplan
RS, et al: Molecular subgroup of high-grade serous ovarian cancer
(HGSOC) as a predictor of outcome following bevacizumab. J Clin
Oncol. 32:55022014. View Article : Google Scholar
|
|
55
|
Galluzzi L, Buque A, Kepp O, Zitvogel L
and Kroemer G: Immunological effects of conventional chemotherapy
and targeted anticancer agents. Cancer Cell. 28:690–714. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
McAlpine JN, Porter H, Köbel M, Nelson BH,
Prentice LM, Kalloger SE, Senz J, Milne K, Ding J, Shah SP, et al:
BRCA1 and BRCA2 mutations correlate with TP53 abnormalities and
presence of immune cell infiltrates in ovarian high-grade serous
carcinoma. Mod Pathol. 25:740–750. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Nolan E, Savas P, Policheni AN, Darcy PK,
Vaillant F, Mintoff CP, Dushyanthen S, Mansour M, Pang JB, Fox SB,
et al: Combined immune checkpoint blockade as a therapeutic
strategy for BRCA1-mutated breast cancer. Sci Transl Med.
9:eaal49222017. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Snyder A, Makarov V, Merghoub T, Yuan J,
Zaretsky JM, Desrichard A, Walsh LA, Postow MA, Wong P, Ho TS, et
al: Genetic basis for clinical response to CTLA-4 blockade in
melanoma. N Engl J Med. 371:2189–2199. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Higuchi T, Flies DB, Marjon NA,
Mantia-Smaldone G, Ronner L, Gimotty PA and Adams SF: CTLA-4
blockade synergizes therapeutically with PARP inhibition in
BRCA1-deficient ovarian cancer. Cancer Immunol Res. 3:1257–1268.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Jiao S, Xia W, Yamaguchi H, Wei Y, Chen
MK, Hsu JM, Hsu JL, Yu WH, Du Y, Lee HH, et al: PARP inhibitor
upregulates PD-L1 expression and enhances cancer-associated
immunosuppression. Clin Cancer Res. 23:3711–3720. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Xing D and Orsulic S: A mouse model for
the molecular characterization of brca1-associated ovarian
carcinoma. Cancer Res. 66:8949–8953. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Li A, Sun S, Song T, Li X, Cheng W, Yao R,
Zhang D, Cai Z, Zhang J, Zhai D and Yu C: Targeted therapy and
immunotherapy for platinum-refractory advanced ovarian
adenosquamous carcinoma: A case report. OncoTargets Ther.
11:3705–3711. 2018. View Article : Google Scholar
|
|
63
|
Adams SF, Rixe O, McCance D, Lee H,
Eberhardt S, Westgate S, Rutledge T and Muller C: Phase I study
combining PARP-inhibition with immune checkpoint blockade in women
with BRCA-deficient recurrent ovarian cancer. Gynecol Oncol. 145
Suppl 1:S99–S100. 2017. View Article : Google Scholar
|
|
64
|
Mabuchi S, Terai Y, Morishige K,
Tanabe-Kimura A, Sasaki H, Kanemura M, Tsunetoh S, Tanaka Y, Sakata
M, Burger RA, et al: Maintenance treatment with bevacizumab
prolongs survival in an in vivo ovarian cancer model. Clin Cancer
Res. 14:7781–7789. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Terme M, Pernot S, Marcheteau E, Sandoval
F, Benhamouda N, Colussi O, Dubreuil O, Carpentier AF, Tartour E
and Taieb J: VEGFA-VEGFR pathway blockade inhibits tumor-induced
regulatory T-cell proliferation in colorectal cancer. Cancer Res.
73:539–549. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Huang Y, Chen X, Dikov MM, Novitskiy SV,
Mosse CA, Yang L and Carbone DP: Distinct roles of VEGFR-1 and
VEGFR-2 in the aberrant hematopoiesis associated with elevated
levels of VEGF. Blood. 110:624–631. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Buchbinder EI and Desai A: CTLA-4 and PD-1
pathways: Similarities, differences, and implications of their
inhibition. Am J Clin Oncol. 39:98–106. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Voron T, Colussi O, Marcheteau E, Pernot
S, Nizard M, Pointet AL, Latreche S, Bergaya S, Benhamouda N,
Tanchot C, et al: VEGF-A modulates expression of inhibitory
checkpoints on CD8+ T cells in tumors. J Exp Med. 212:139–148.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Tada Y, Togashi Y, Kotani D, Kuwata T,
Sato E, Kawazoe A, Doi T, Wada H, Nishikawa H and Shitara K:
Targeting VEGFR2 with Ramucirumab strongly impacts
effector/activated regulatory T cells and CD8(+) T cells in the
tumor microenvironment. J Immunother Cancer. 6:1062018. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Wallin JJ, Bendell JC, Funke R, Sznol M,
Korski K, Jones S, Hernandez G, Mier J, He X, Hodi FS, et al:
Atezolizumab in combination with bevacizumab enhances
antigen-specific T-cell migration in metastatic renal cell
carcinoma. Nat Commun. 7:126242016. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Choueiri TK, Figueroa DJ, Fay AP,
Signoretti S, Liu Y, Gagnon R, Deen K, Carpenter C, Benson P, Ho
TH, et al: Correlation of PD-L1 tumor expression and treatment
outcomes in patients with renal cell carcinoma receiving sunitinib
or pazopanib: Results from COMPARZ, a randomized controlled trial.
Clin Cancer Res. 21:1071–1077. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Yuan J, Zhou J, Dong Z, Tandon S, Kuk D,
Panageas KS, Wong P, Wu X, Naidoo J, Page DB, et al: Pretreatment
serum VEGF is associated with clinical response and overall
survival in advanced melanoma patients treated with ipilimumab.
Cancer Immunol Res. 2:127–132. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Peske JD, Woods AB and Engelhard VH:
Control of CD8 T-cell infiltration into tumors by vasculature and
microenvironment. Adv Cancer Res. 128:263–307. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Wu X, Giobbie-Hurder A, Liao X, Lawrence
D, McDermott D, Zhou J, Rodig S and Hodi FS: VEGF neutralization
plus CTLA-4 blockade alters soluble and cellular factors associated
with enhancing lymphocyte infiltration and humoral recognition in
melanoma. Cancer Immunol Res. 4:858–868. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Wu X, Li J, Connolly EM, Liao X, Ouyang J,
Giobbie-Hurder A, Lawrence D, McDermott D, Murphy G, Zhou J, et al:
Combined anti-VEGF and anti-CTLA-4 therapy elicits humoral immunity
to galectin-1 which is associated with favorable clinical outcomes.
Cancer Immunol Res. 5:446–454. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Goede V, Coutelle O, Neuneier J,
Reinacher-Schick A, Schnell R, Koslowsky TC, Weihrauch MR, Cremer
B, Kashkar H, Odenthal M, et al: Identification of serum
angiopoietin-2 as a biomarker for clinical outcome of colorectal
cancer patients treated with bevacizumab-containing therapy. Br J
Cancer. 103:1407–1414. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Wu X, Giobbie-Hurder A, Liao X, Connelly
C, Connolly EM, Li J, Manos MP, Lawrence D, McDermott D, Severgnini
M, et al: Angiopoietin-2 as a biomarker and target for immune
checkpoint therapy. Cancer Immunol Res. 5:17–28. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Lee JM, Cimino-Mathews A, Peer CJ, Zimmer
A, Lipkowitz S, Annunziata CM, Cao L, Harrell MI, Swisher EM,
Houston N, et al: Safety & clinical activity of the programmed
death-ligand 1 inhibitor durvalumab in combination with Poly
(ADP-Ribose) polymerase inhibitor olaparib or vascular endothelial
growth factor Receptor 1–3 Inhibitor Cediranib in Women's Cancers:
A dose-escalation, phase I study. J Clin Oncol. 35:2193–2202. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Hirte H, Lheureux S, Fleming GF, Sugimoto
A, Morgan R, Biagi J, Wang L, McGill S, Ivy SP and Oza AM: A phase
2 study of cediranib in recurrent or persistent ovarian, peritoneal
or fallopian tube cancer: A trial of the Princess Margaret, Chicago
and California Phase II Consortia. Gynecol Oncol. 138:55–61. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Huang J, Wang L, Cong Z, Amoozgar Z, Kiner
E, Xing D, Orsulic S, Matulonis U and Goldberg MS: The PARP1
inhibitor BMN 673 exhibits immunoregulatory effects in a Brca1(−/-)
murine model of ovarian cancer. Biochem Biophys Res Commun.
463:551–556. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Fukuda T, Kamai T, Masuda A, Nukui A, Abe
H, Arai K and Yoshida K: Higher preoperative serum levels of PD-L1
and B7-H4 are associated with invasive and metastatic potential and
predictable for poor response to VEGF-targeted therapy and
unfavorable prognosis of renal cell carcinoma. Cancer Med.
5:1810–1820. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Robert L, Ribas A and Hu-Lieskovan S:
Combining targeted therapy with immunotherapy. Can 1+1 equal more
than 2? Semin Immunol. 28:73–80. 2016.
|