Introduction
Malignant bowel obstruction (MBO) is a common
complication of advanced cancer of gastrointestinal or
gynaecological origin and can result in a potentially
life-threatening emergency, including rupture of the intestine,
sepsis and multi-organ failure, without timely and effective
treatment (1,2). However, due to colonic distension with
faecal loading, dehydration, electrolyte imbalance, oedema of the
intestinal dissepiment, localised tumours and a poor general
condition in elderly patients, emergency colonic surgery for acute
obstruction is associated with a high mortality rate of 15–34%,
which is significantly higher than the mortality rates following
elective surgery (3,4).
Patients with MBO are commonly at a late stage of
cancer, and a number are unable to tolerate surgery (2). In addition, due to the potentially
distant obstruction position and severe bowel stenosis, it is
difficult to achieve crossing of the obstruction site and
sufficient drainage using the traditional nasogastric tube and
gastroscope-assisted catheterization treatment method (5–7).
Long intestinal tube decompression can alleviate the
symptoms of obstruction effectively by aspiration of the intestinal
contents. In addition, in certain cases, the long intestinal tube
can pass through the severe obstruction of the intestine and result
in a correction of intestinal kinking, thus improving quality of
life (2,5). The aim of the present study was to
investigate the safety and efficacy of long intestinal tube
decompression under fluoroscopic guidance for the treatment of
MBO.
Patients and methods
Patients
The cases of 74 patients with small intestinal MBO
who were treated at The Sixth Affiliated Hospital of Sun Yat-Sen
University (Guangzhou, China) during the period between June 2015
and October 2017 were reviewed. All the patients were diagnosed by
clinical and pathological diagnostic methods, as well as plain
X-ray radiography and abdominal computed tomography (CT) scans.
The inclusion criteria were as follows: Definite
diagnosis of small intestinal obstruction by abdominal CT scan or
plain X-ray radiography, obstruction caused by a
histologically-confirmed malignant tumour, refractory nausea and
vomiting, and absence of dysphagia, suffocation and other symptoms.
Patients with any of the following characteristics were excluded:
Unconsciousness, severe nasopharyngeal or oesophageal diseases,
multiple organ dysfunction, including of the heart, liver or lungs,
gastrointestinal perforation and active bleeding.
Approval for the study protocol was obtained from
the Institutional Ethics Review Board of The Sixth Affiliated
Hospital of Sun Yat-Sen University. Written informed consent for
the treatment was obtained from each patient prior to long
intestinal tube placement.
Instruments
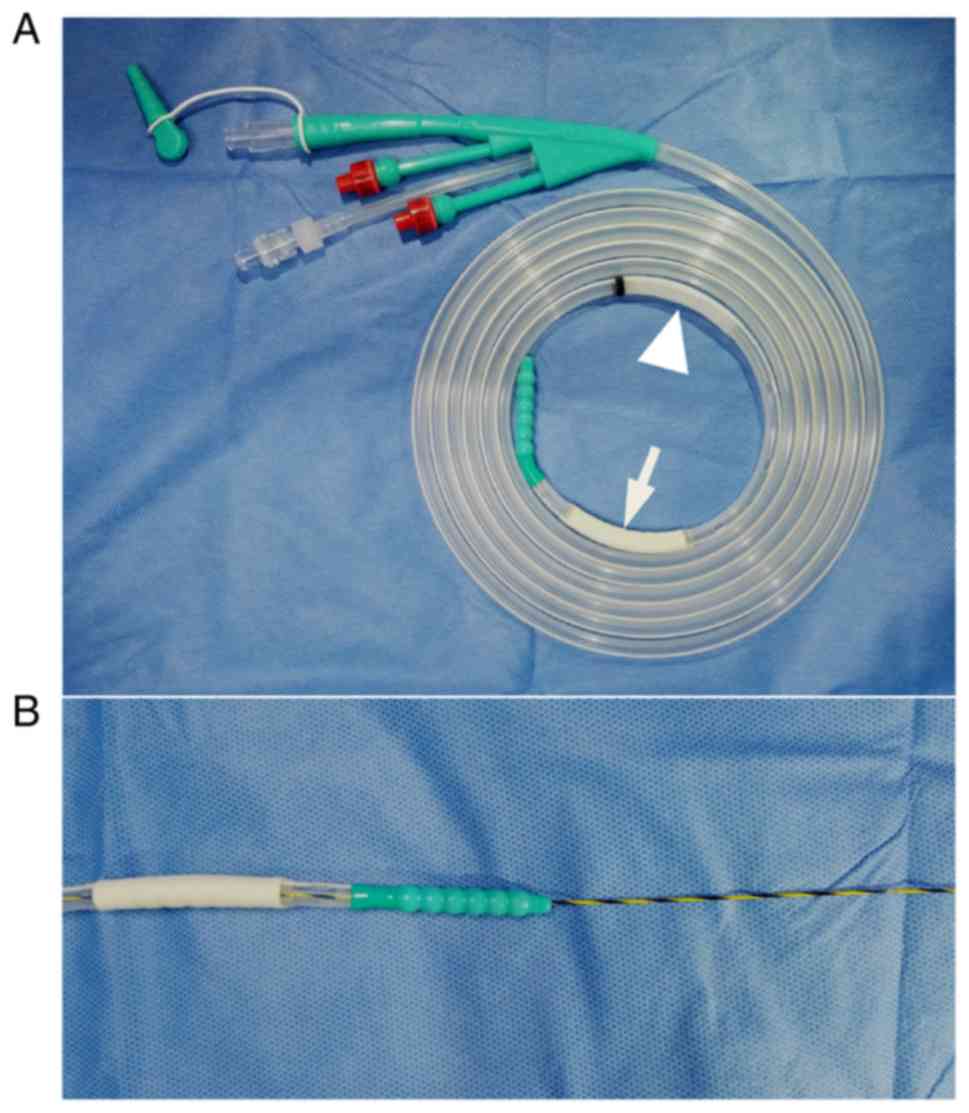
A hydrophilic long intestinal tube (Create Medic,
Dalian, China) was used (Fig. 1).
The tube had an outer diameter of 16 or 18 French, a working length
of 300 cm, an anterior balloon and a posterior balloon at its tip,
an injection channel with an anti-reflux valve and a drainage
channel. In addition to the hole at the tip, there were 7 side
holes near the distal end of the tube. The self-contained guide
wire was 1.24 mm in diameter and 350 cm long. Additionally, liquid
paraffin oil and a flat panel Innova 3100 digital subtraction
angiography system (GE Healthcare, Chicago, IL, USA) were used.
Procedure
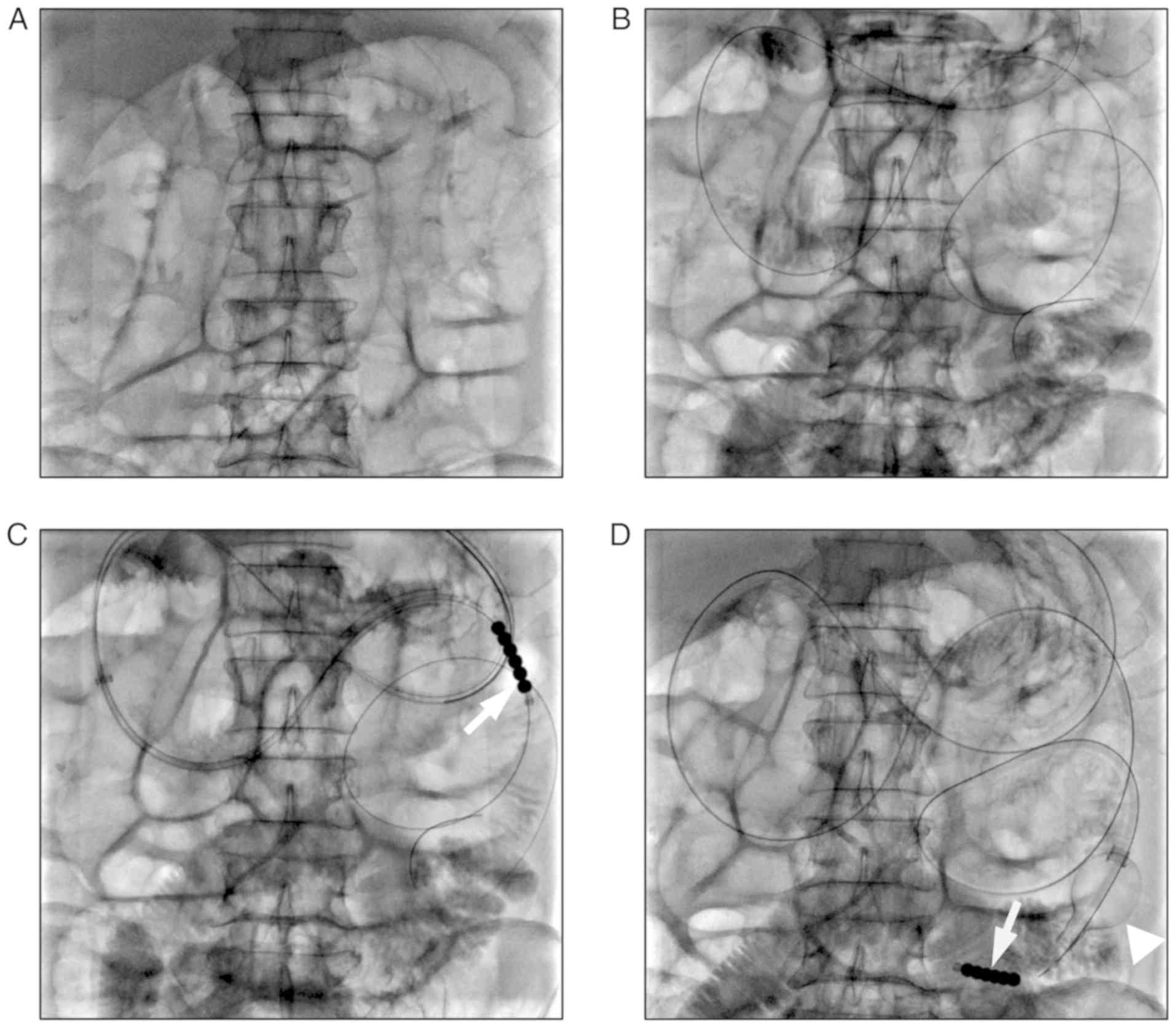
With the patient in the supine position, a 0.90-mm
wide, 150-cm long Terumo guidewire (Terumo Corporation, Tokyo,
Japan) and a 5 French DAV catheter (Cook Medical, Bloomington, IN,
USA) via an 8 French guiding catheter (Boston Scientific,
Marlborough, MA, USA) were placed via the nostril, oesophagus and
stomach into the descending duodenum under fluoroscopic guidance.
The guide wire was removed, and iodinated contrast medium
(meglumine diatrizoate or iopromide) was injected through the DAV
catheter to confirm the catheter location in the duodenum, as well
as the shape of the jejunum. Following this, a 0.90-mm wide, 450-cm
long Zebra guidewire (Boston Scientific) was inserted into the
upper jejunum. The DAV catheter and guiding catheter were removed,
and the long intestinal tube was placed in the jejunum via the
prepositioned Zebra guidewire (Fig.
2).
To aid the passing of the long intestinal tube
through the stomach and duodenum more easily, the self-contained
guide wire, 1.24 mm in diameter, was also inserted into the tube.
In addition, liquid paraffin oil was applied to lessen the friction
between the tube and the enteric wall, and to reduce the patients'
discomfort.
Finally, 20 ml iodinated contrast medium was
injected into the tube to evaluate the extent of small intestine
expansion. The anterior balloon of the tube was filled with 20 ml
sterilised distilled water to promote intestinal peristalsis and to
assist the gradual movement of the tube to the distal end of the
small intestine.
Following insertion of the long intestinal tube,
intermittent negative pressure drainage was performed to reduce the
intraluminal pressure of the small intestine. A plain X-ray
radiograph of the abdomen was taken every few days to evaluate the
progress of the tube and the degree of decompression.
Observation of efficacy
The following clinical data were reviewed to
retrospectively assess the safety and efficacy of the treatment:
Age, tumour type, procedure duration, insertion depth of the long
intestinal tube, daily drainage, changes in abdominal pain and
bloating, plain X-ray radiographs of the abdomen prior to and
following long tube insertion, and any complications, including
gastrointestinal perforation, bleeding, nasal mucosal injury,
laryngeal oedema and aspiration pneumonia.
Results
Clinical characteristics
A total of 74 patients were included for analysis in
the present study. There were 50 men and 24 women (mean age,
56.5±12.4 years; range, 31–82 years). The primary cancer types of
the patients with MBO are shown in Table
I. The mean time required for placement of the long intestinal
tube guided by fluoroscopy was 31.09±16.25 min (range, 10.00–65.00
min). The mean insertion depth of the tube was 153±39 cm (range,
85–260 cm). The characteristics of the treatment with a long
intestinal tube in the 74 patients with MBO are shown in Table II.
 | Table I.Primary tumour type of 74 patients
with malignant bowel obstruction. |
Table I.
Primary tumour type of 74 patients
with malignant bowel obstruction.
| Tumour type | Patients, n (%) |
|---|
| Carcinoma of sigmoid
colon | 19 (25.7) |
| Rectal cancer | 17 (23.0) |
| Carcinoma of
descending colon | 12 (16.2) |
| Gastric cancer | 11 (14.9) |
| Carcinoma of
ascending colon | 6
(8.1) |
| Cervical
carcinoma | 3
(4.1) |
| Ovarian cancer | 2
(2.7) |
| Carcinoma of urinary
bladder | 2
(2.7) |
| Lung cancer | 1
(1.4) |
| Cholangiocellular
carcinoma | 1
(1.4) |
 | Table II.Clinical parameters of treatment with
long intestinal tube in 74 patients with malignant bowel
obstruction. |
Table II.
Clinical parameters of treatment with
long intestinal tube in 74 patients with malignant bowel
obstruction.
| Clinical
parameters | Mean ± SD |
|---|
| Insertion depth of
tube, cm | 153.00±39.00 |
| Procedure duration,
min | 31.09±16.25 |
| Drainage on the first
day, ml | 708.38±554.30 |
| Drainage on the
second day, ml | 706.55±624.70 |
| Drainage on the third
day, ml | 527.50±475.20 |
Clinical outcomes
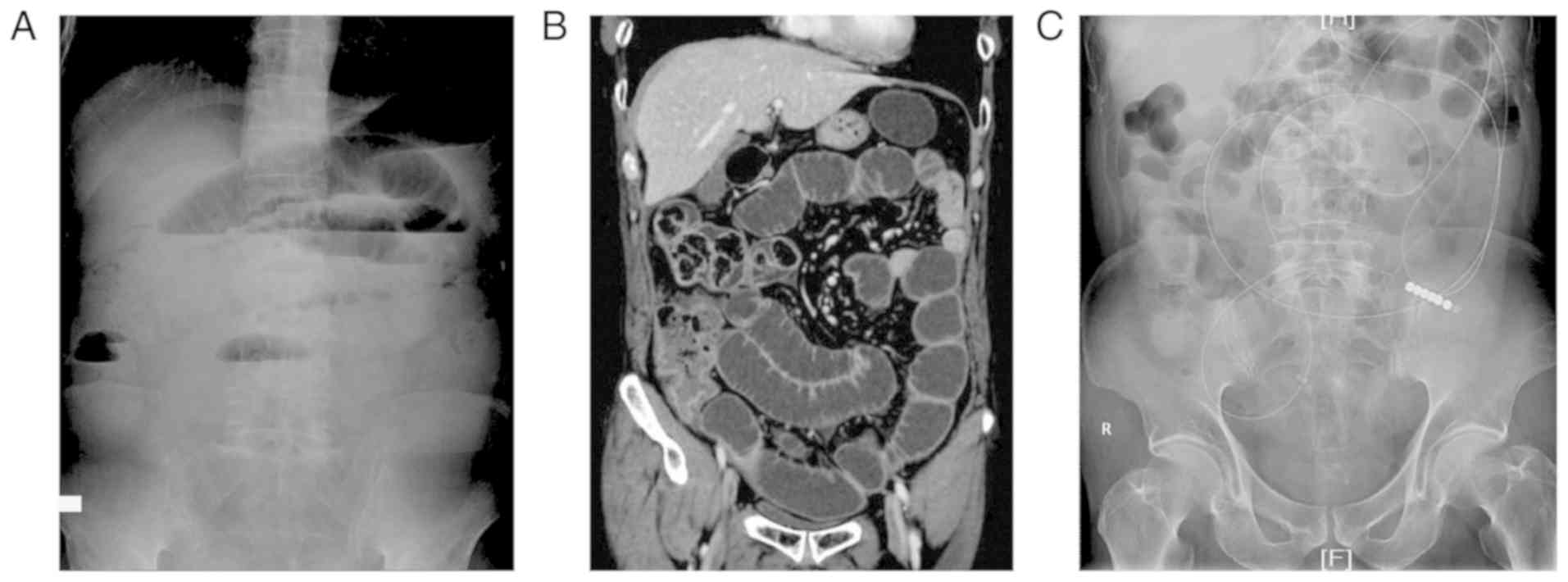
The long intestinal tube was successfully inserted
in all patients. Following 1–3 days of tube decompression, the
symptoms of abdominal pain, abdominal bloating and vomiting were
greatly improved in 58 patients (78.38%) (Fig. 3). Among the 58 patients, following
3–7 days of tube decompression, the symptoms of MBO were further
improved or remained stable. Within 1 month of treatment, the
symptoms of MBO were completely resolved and the long intestinal
tube was removed in 13 cases. Tumour resection or enterostomy was
performed for 19 patients. A total of 20 patients kept the long
intestinal tube for >1 month and the symptoms of MBO did not
deteriorate. Of the 74 patients, 4 were lost to follow-up, and 2
patients succumbed to multiple organ failure and end-stage
cancer.
The symptoms of the remaining 16 patients were not
effectively relieved following decompression. Of the 16 patients,
10 required surgical treatment for rectal cancer (n=3), carcinoma
of the sigmoid colon (n=3), carcinoma of the descending colon
(n=2), gastric cancer (n=1) and carcinoma of the ascending colon
(n=1). The remaining 6 patients received conservative treatment for
carcinoma of the sigmoid colon (n=3), carcinoma of the descending
colon (n=2) and gastric cancer (n=1). No serious complications,
including gastrointestinal bleeding, perforation, laryngeal oedema
and aspiration pneumonia, or serious nasal mucosal injury (nasal
cavity bleeding, oedema and asphyxia) were observed in these
patients.
Discussion
Although the small intestine accounts for at least
75% of the length of the gastrointestinal tract, small intestinal
malignant tumours are unusual and account for only 1–5% of all
gastrointestinal tract malignancies (8–10). The
incidence of intestinal malignant tumours is significantly lower
compared with that of colonic malignancies (11,12). The
progression of the majority of advanced colonic and gynaecological
malignancies is characterised by multiple segmental obstructions,
including small intestinal obstructions (13).
The occurrence of MBO results in a series of
pathological and physiological changes, including bowel ischaemia
and anoxia, oedema of the intestinal dissepiments, and bacterial
translocation and infection, which aggravate the increase in
vascular permeability and destroy the liquid secretion absorption
equilibrium in the intestinal canal, ultimately resulting in
intestinal wall necrosis, perforation, haemorrhage, infection and
septic shock (2–5,14,15).
Therefore, it is essential to reduce the pressure of the intestinal
cavity and drain intestinal contents effectively, as well as to
improve the blood supply of the intestinal wall in a timely
manner.
Conservative treatments of MBO include fast
nasogastric tube decompression, anti-infection treatments,
inhibition of the secretion of digestive juice by somatostatin and
restoration of the electrolyte balance (16). Nasogastric tube decompression is
commonly used for MBO. While traditional nasogastric tube
decompression can decompress and drain the gastral cavity fully,
the location of the nasogastric tube makes it difficult to
effectively drain small intestinal contents and relieve the
symptoms of intestinal obstruction, including abdominal pain and
abdominal bloating (17–19). More importantly, traditional
nasogastric tube decompression may not achieve the restoration of
early enteral nutrition (2).
Long-tube decompression is a useful alternative
treatment for patients with bowel obstructions (20,21).
Several studies report the superiority of decompression tubes in
aspects of decompression and drainage (2,3,5–7).
However, it is often difficult to insert a long intestinal tube
into the small bowel, which results in longer procedure times and a
poor postoperative outlook.
Currently, in the majority of patients with MBO, the
long intestinal tube is placed with the assistance of endoscopy.
However, the preparation for endoscopy, which includes bowel
cleaning and gas injection during insertion, can lead to marked
discomfort and pain (9,22). In addition, under endoscopical
guidance, the tip of the long intestinal tube is often placed in
the horizontal segment of the duodenum or just across the Treitz
ligament, and the tube is then advanced by gastrointestinal
peristalsis. However, due to weak intestinal peristalsis in certain
elderly or weak patients, the tube cannot be pushed forward to the
jejunum. In the present study, a 450-cm long Zebra guidewire was
inserted into the upper jejunum under fluoroscopic guidance,
and the long intestinal tube was placed directly into the jejunum
via the Zebra guidewire without the aid of intestinal peristalsis.
The long intestinal tube was placed successfully in all 74
patients, with a mean insertion depth of 153 cm. Due to the high
success rate and good tolerance, patients more readily accepted the
fluoroscopy-guided, long intestinal tube placement for the
treatment of malignant bowel obstruction. Following 1–3 days of
tube decompression, 58 patients (78.38%) improved substantially.
The other 16 patients were in the advanced stage of cancer, with
multiple metastases in the intestinal tract and multiple severe
obstructions. Therefore, they were not effectively relieved
following decompression. Of the 16 patients, 10 required surgical
treatment and the remaining 6 received conservative treatment. No
serious complications, including gastrointestinal bleeding,
perforation, laryngeal oedema, aspiration pneumonia and serious
nasal mucosalinjury, were observed in the present study.
Another treatment modality for the treatment of MBO,
particularly for malignant colorectal obstruction, is the use of a
self-expanding stent (23–25). However, the existence of
stent-related complications, including perforation, infection,
active bleeding, stent migration and re-obstruction, should be
emphasised (26). Due to the long
distance from the anus, it is often difficult to implant the stent
in the hepatic flexure of the colon, the ascending colon or the
ileum. In addition, there are often multiple sites of obstruction
in MBO patients, which makes it difficult to relieve all of the
obstructions using the self-expanding stent (21,27).
Long intestinal tube decompression can alleviate the symptoms of
obstruction effectively from the proximal bowel, which may
partially overcome the difficulties caused by multiple sites of
obstruction.
The present study has several limitations. Firstly,
a retrospective analysis of the data was performed, and, as such,
the study is subject to the inherent limitations of retrospective
studies. Secondly, the cost-effectiveness of the treatment has not
been assessed, and treatment complications have not been compared
with those of the conventional nasogastric tube decompression.
Therefore, a multicentre randomised controlled trial between
fluoroscopy-guided long intestinal tube placement and the existing
invasive therapies may be required to confirm the safety and
efficacy of this treatment.
In conclusion, fluoroscopy-assisted long intestinal
tube placement is a safe and effective procedure for intestinal
decompression in patients with MBO. This procedure can greatly
improve quality of life, which is of value to patients and their
families.
Acknowledgements
Not applicable.
Funding
This study was supported by a grant from the
National Natural Science Foundation of China (no. 81301978).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HL and BZ drafted this manuscript. HL, KW and BZ
analyzed the imaging data and collected the data. YL, KW and ZZ
assisted with statistical analysis. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Institutional
Ethics Review Board of The Sixth Affiliated Hospital of Sun Yat-Sen
University (Guangzhou, China). Written informed consent for this
study was obtained from each patient.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Matsuda A, Miyashita M, Matsumoto S,
Sakurazawa N, Takahashi G, Matsutani T, Yamada M and Uchida E:
Comparison between metallic stent and transanal decompression tube
for malignant large-bowel obstruction. J Surg Res. 205:474–481.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Li D, Du H, Shao G, Guo Y, Lu W and Li R:
Application of small intestine decompression combined with oral
feeding in middle and late period of malignant small bowel
obstruction. Oncol Lett. 14:180–184. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Xu YS, Song T, Guo YT, Shao GQ, Du HT, Li
DC and Fu YF: Placement of the decompression tube as a bridge to
surgery for acute malignant left-sided colonic obstruction. J
Gastrointest Surg. 19:2243–2248. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fischer A, Schrag HJ, Goos M, Obermaier R,
Hopt UT and Baier PK: Transanal endoscopic tube decompression of
acute colonic obstruction: Experience with 51 cases. Surg Endosc.
22:683–688. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kanno Y, Hirasawa D, Fujita N, Noda Y,
Kobayashi G, Ishida K, Ito K, Obana T, Suzuki T, Sugawara T, et al:
Long intestinal tube insertion with the ropeway method facilitated
by a guidewire placed by transnasal ultrathin endoscopy for bowel
obstruction. Dig Endosc. 21:196–200. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Amelung FJ, Ter Borg F, Consten EC,
Siersema PD and Draaisma WA: Deviating colostomy construction
versus stent placement as bridge to surgery for malignant
left-sided colonic obstruction. Surg Endosc. 30:5345–5355. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gianotti L, Tamini N, Nespoli L, Rota M,
Bolzonaro E, Frego R, Redaelli A, Antolini L, Ardito A, Nespoli A
and Dinelli M: A prospective evaluation of short-term and long-term
results from colonic stenting for palliation or as a bridge to
elective operation versus immediate surgery for large-bowel
obstruction. Surg Endosc. 27:832–842. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Williamson JM and Williamson RC: Small
bowel tumors: Pathology and management. J Med Assoc Thai.
97:126–137. 2014.PubMed/NCBI
|
|
9
|
Lee BI, Choi H, Choi KY, Byeon JS, Jang
HJ, Eun CS, Cheon JH, Shin SJ, Kim JO, Lee MS and Choi JH: Clinical
characteristics of small bowel tumors diagnosed by double-balloon
endoscopy: KASID multi-center study. Dig Dis Sci. 56:2920–2927.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Schwartz GD and Barkin JS: Small-bowel
tumors detected by wireless capsule endoscopy. Dig Dis Sci.
52:1026–1030. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Imaoka H, Higaki N, Kumagi T, Miyaike J,
Ohmoto M, Yamauchi K, Murakami T, Murakami H, Ikeda Y, Yokota T, et
al: Characteristics of small bowel tumors detected by double
balloon endoscopy. Dig Dis Sci. 56:2366–2371. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Thosani N, Guha S and Singh H: Colonoscopy
and colorectal cancer incidence and mortality. Gastroenterol Clin
North Am. 42:619–637. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Currow DC, Quinn S, Agar M, Fazekas B,
Hardy J, McCaffrey N, Eckermann S, Abernethy AP and Clark K:
Double-blind, placebo-controlled, randomized trial of octreotide in
malignant bowel obstruction. J Pain Symptom Manage. 49:814–821.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li de C, Li RH and Tian Q: Efficacy of
intestinal decompression with long nasointestinal tube and
selective contrast radiography in the treatment of small bowel
obstruction in elderly patients. Minerva Chir. 71:85–90.
2016.PubMed/NCBI
|
|
15
|
Li D, Du H, Shao G, Xu Y, Li R and Tian Q:
Clinical application of transanal ileal tube placement using X-ray
monitoring. Oncol Lett. 13:137–140. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Catena F, Di Saverio S, Kelly MD, Biffl
WL, Ansaloni L, Mandalà V, Velmahos GC, Sartelli M, Tugnoli G, Lupo
M, et al: Bologna guidelines for diagnosis and management of
adhesive small bowel obstruction (ASBO): 2010 evidence-based
guidelines of the world society of emergency surgery. World J Emerg
Surg. 6:52011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sekiba K, Ohmae T, Odawara N, Moriyama M,
Kanai S, Tsuboi M, Saito T, Uchino K, Akamatsu M and Okamoto M: A
new method for insertion of long intestinal tube for small bowel
obstruction: Nonendoscopic over-the-wire method via short
nasogastric tube. Medicine (Baltimore). 95:e54492016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sano N, Yamamoto M, Nagai K, Yamada K and
Ohkohchi N: Nasogastric tube syndrome induced by an indwelling long
intestinal tube. World J Gastroenterol. 22:4057–4061. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Thornblade LW, Truitt AR, Davidson GH,
Flum DR and Lavallee DC: Surgeon attitudes and practice patterns in
managing small bowel obstruction: A qualitative analysis. J Surg
Res. 219:347–353. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim YJ, Yoon CJ, Seong NJ, Kang SG, An SW
and Woo YN: Safety and efficacy of radiological percutaneous
jejunostomy for decompression of malignant small bowel obstruction.
Eur Radiol. 23:2747–2753. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gowen GF: Long tube decompression is
successful in 90% of patients with adhesive small bowel
obstruction. Am J Surg. 185:512–515. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Li RH, Li DC, Tian QZ, Wu P and Zhang XH:
Diagnosis of small bowel obstruction using targeted enterography
during nasointestinal decompression. Cell Biochem Biophys.
72:833–837. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Saito S, Yoshida S, Isayama H, Matsuzawa
T, Kuwai T, Maetani I, Shimada M, Yamada T, Tomita M, Koizumi K, et
al: A prospective multicenter study on self-expandable metallic
stents as a bridge to surgery for malignant colorectal obstruction
in Japan: Efficacy and safety in 312 patients. Surg Endosc.
30:3976–3986. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cirocchi R, Farinella E, Trastulli S,
Desiderio J, Listorti C, Boselli C, Parisi A, Noya G and Sagar J:
Safety and efficacy of endoscopic colonic stenting as a bridge to
surgery in the management of intestinal obstruction due to left
colon and rectal cancer: A systematic review and meta-analysis.
Surg Oncol. 22:14–21. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
van Hooft JE, Bemelman WA, Oldenburg B,
Marinelli AW, Lutke Holzik MF, Grubben MJ, Sprangers MA, Dijkgraaf
MG and Fockens P; collaborative Dutch Stent-In study group, :
Colonic stenting versus emergency surgery for acute left-sided
malignant colonic obstruction: A multicentre randomised trial.
Lancet Oncol. 12:344–352. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
van den Berg MW, Sloothaak DA, Dijkgraaf
MG, van der Zaag ES, Bemelman WA, Tanis PJ, Bosker RJ, Fockens P,
ter Borg F and van Hooft JE: Bridge-to-surgery stent placement
versus emergency surgery for acute malignant colonic obstruction.
Br J Surg. 101:867–873. 2014. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Guo SB and Duan ZJ: Decompression of the
small bowel by endoscopic long-tube placement. World J
Gastroenterol. 18:1822–1826. 2012. View Article : Google Scholar : PubMed/NCBI
|