Introduction
Alzheimer's disease (AD) is an age-associated
neurodegenerative disease that causes dementia, and severely
affects the health and quality of life of elderly individuals
(1). AD interrupts various brain
functions, including memory, intelligence, judgment and learning
(2). A previous study demonstrated
that the etiology and pathogenesis of AD involves a variety of
factors, including environmental elements, genetic factors and
aging (3). The accumulation of
pathological amyloid β (Aβ) peptide fragments serve a specific role
in AD by inducing neuronal apoptosis and subsequent cognitive
dysfunction (4,5). Models involving Aβ peptide deposition
are widely used to simulate AD in animals (6–8). At
present, modern medicine lacks an effective treatment for the core
symptoms of AD, which includes progressive cognitive decline.
Therefore, it is important to identify novel therapeutic approaches
to counteract AD-associated cognitive impairment.
The flavonoid compound scutellarin (Scu) is
ubiquitous in nature, particularly in the genus Erigeron
(Asteraceae) and Scutellaria (Lamiaceae), and has been widely used
in traditional Chinese medicine for a number of millennia (9–11).
Recently, studies have made significant progress assessing the
benefits of Scu, which exhibited neuroprotective effects, including
anti-oxidant, anti-inflammatory and anti-apoptotic activities in
numerous diseases (12–14). Additionally, previous studies
demonstrated the beneficial effects of Scu in vascular endothelial
dysfunction (15,16), myocardial infarction (17), colorectal cancer (18,19) and
other types of cancer (20,21). Scutellarein (5,6,7,4′-tetrahydroxy
flavone; Scue) is the hydrolyzed product of Scu in perennial herbs,
including Scutellaria baicalensis, Scutellaria lateriflora
and Scutellaria barbata (22,23).
Previous studies demonstrated that Scue is absorbed more easily
following oral administration compared with Scu, when administered
in equal doses (22,24). Recent studies additionally
demonstrated that Scu/Scue may prevent neuronal injury and the
protective effects of Scue were determined to be superior to Scu
(25–27). However, it remains to be determined
whether Scue may affect Aβ-induced cell apoptosis and
neurotoxicity, which are important pathogenic mechanisms of AD.
Therefore, the present study aimed to examine whether Scue is able
to exert therapeutic activity through protein kinase B/nuclear
factor-κB (NF-κB) signaling in AD.
In the present study, a cellular model and a rodent
model of Aβ-induced AD were used to evaluate the ability of Scue;
the results demonstrated that Scue may inhibit neuro-inflammation,
and ameliorate the cognitive and cellular effects of Aβ toxicity
through inhibition of the NF-κB signaling pathway. The present data
provided evidence for the use of Scue as a novel therapeutic to
treat patients with AD.
Materials and methods
Extraction of Scue
A Scutellaria baicalensis root was provided
from Jilin Northeast Asia Pharmaceutical Co., Ltd. (Yanji, China).
Extract standards were obtained from the Jilin Institutes for Food
and Drug Control (China). The Scutellaria baicalensis root
was dried and crushed, soaked for 1.5 h in a 10-fold water volume
(w/v), and subsequently refluxed three times for 30 min. Polyamide
column chromatography was used to separate Scue and monitored using
high-performance liquid chromatography (HPLC). Measurements were
performed using HPLC U3000 with a Corona® charged
aerosol detector (Thermo Fisher Scientific, Inc., Waltham, MA,
USA). A XB-C18 (250×4.6 mm; 5 µm) column (Welch Materials, Inc.,
Hurst, TX, USA) was used for sample separation at 30°C. A 10 µl
injection volume with 20:80 gradient was used with acetonitrile as
mobile phase A and 0.1% (v/v) formic acid in water as mobile phase
B. The flow rate was set to 0.8 ml/min.
Cell culture
Rat pheochromocytoma (PC12) cells were purchased
from The Type Culture Collection of The Chinese Academy of Medical
Sciences (Shanghai, China). Cells were cultured in Dulbecco's
modified Eagle's medium (DMEM; Gibco, Thermo Fisher Scientific,
Inc.) supplemented with 8% fetal bovine serum and 8% horse serum
(Gibco; Thermo Fisher Scientific, Inc.), and maintained at 37°C in
a humidified atmosphere of 5% CO2. For the experimental
treatments, cells were pre-incubated with different concentrations
(0, 5, 10, 15 and 30 µg/ml) of the test compound (Scue) and (0, 5,
10, 15 and 30 µg/ml) of the test compound (Scu) dissolved in 0.2%
dimethyl sulfoxide (DMSO) in DMEM for 4 h and subsequently treated
with 2 µg/ml Aβ for 24 h (7).
MTT assay
Cell viability was determined using a MTT assay.
Cells were seeded in 96-well microplates at a density of
2×103 cells/well and incubated for 24 h to allow the
cells to adhere. Subsequently, MTT (Sigma-Aldrich; Merck KGaA,
Darmstadt, Germany) at a final concentration of 0.2 mg/ml was added
to each well and incubated at 37°C for 72 h. Following incubation,
the cell supernatants were removed and the remaining formazan
crystals were dissolved in 200 µl DMSO for 15 min. The optical
density of each well was determined using an ELX-800
spectrophotometer (BioTek Instruments, Inc., Winooski, VT, USA) at
490 nm.
Flow cytometry analysis of
apoptosis
A flow cytometer (FACSCalibur; BD Biosciences, San
Jose, CA, USA) and an apoptosis detection kit (Biogot Technology
Co., Ltd., Nanjing, China) were used according to the
manufacturer's protocol to detect apoptotic cells. Cells were
harvested, centrifuged at 2–8°C for 10 min at 1,500 × g), washed
and subsequently resuspended in 400 µl binding buffer. A total of 5
µl Annexin V-fluorescein isothiocyanate was added to each cell
suspension and the suspension was incubated at 2–8°C for 15 min in
the dark. Subsequently, 10 µl propidium iodide was added and the
suspension was incubated at 2–8°C for 5 min in the dark. Flow
cytometry was performed within 1 h of the final step. FlowJo
software (version 7.6; FlowJo LLC, Ashland, OR, USA) was used for
analysis.
Immunofluorescence staining
Cells were fixed in 4% paraformaldehyde for 15 min
at room temperature and subsequently gently rinsed in PBS. To
permeabilize the cells, they were incubated for 30 min in PBS
containing 0.1% Triton X-100. Cells were blocked with 8% goat serum
(Gibco; Thermo Fisher Scientific, Inc.) for 15 min at room
temperature and each slide was incubated with NF-κB p65 primary
antibody (1:100; cat. no. bs-3543R; BIOSS, Beijing, China)
overnight at 4°C, and Cy3-labeled goat anti-rabbit secondary
antibody (1:200; cat. no. A0516; Beyotime Institute of
Biotechnology, Haimen, China) in the dark at room temperature for
60 min. The cells were counterstained with DAPI for 10 min at room
temperature. Cells were viewed under a fluorescent microscope
(Olympus Corporation, Tokyo, Japan; magnification, ×400) subsequent
to adding anti-fading reagent.
Animal model construction
Healthy male Wistar rats (n=24; age, 6–8 weeks;
weight, 200 g) were purchased from the Laboratory Animal Center of
Jilin University (Changchun, China). Animals were housed in
laboratory facilities under the following conditions: Temperature,
21.0–25.0°C; relative humidity, 40.0–70.0%; complete air
replacement 15 times/h; and 12-h light/dark cycle. Prior to the
experiments, the rats were group-housed in a pathogen-free grade
animal room with ad libitum access to food and water and
allowed to acclimate for 1 week. The Animal Ethics Committee of
Jilin University approved the experimental protocol.
Each rat was randomly assigned to one of four
groups: Control, Aβ, Scue (50 mg/kg; intragastrically) or Scu (50
mg/kg; intraperitoneally). Non-control rats were anesthetized with
sodium pentobarbital (60 mg/kg; intraperitoneally) and injected in
the deep frontal cortex (3.2 mm anteroposterior, 2 mm dorsoventral
relative to bregma; depth 3 mm) with 3 µl Aβ (10 ng/µl) (28), whereas, control rats received an
injection of 3 µl saline. Following these injections, rats were
subjected to treatment and testing over a period of 4 weeks.
All the mice were sacrificed with CO2
(the displacement rate of CO2 was 10% chamber
volume/min) for 0.5 h subsequent to behavioral testing (7 days),
and hippocampal tissues were dissected. Subsequently, one-half of
the hippocampal tissues were frozen in liquid nitrogen and stored
at −70°C for future protein analyses. The other tissues were fixed
for 12 h in 4% paraformaldehyde at room temperature, and embedded
in paraffin for sectioning and staining.
Morris water maze (MWM) testing
The MWM test includes an acquisition period and a
special probe trial, and is a well-established method for the
evaluation of learning and memory in animals (29). In the present study, the acquisition
period lasted for 6 days, with two training sessions per day and a
15 min interval between sessions. Each animal was placed at a
designated starting point in a different quadrant of the maze,
facing the tank wall. In one quadrant, a platform was hidden just
below the surface of the water. If a rat identified and climbed
onto the platform, and remained there for >3 sec, the swimming
time was documented as the latency to locate the platform. If a rat
failed to locate the platform within 120 sec, it was manually
placed onto the platform for 30 sec and the latency was recorded as
120 sec.
The spatial probe trial was only performed once. The
platform was removed from the pool and the rat was placed at any
starting point that was not adjacent to the platform. The number of
times that each rat swam across the original location of the
platform within 120 sec was documented.
Western blotting
Cells [cytoplasmic and nuclear NF-κB were separated
by the membrane protein separation method (30)] were lysed in
nonyl-phenoxypolyethoxylethanol-40 lysate (Beyotime Institute of
Biotechnology), and total protein and nucleoproteins from the
hippocampal tissues were extracted using radioimmunoprecipitation
assay lysis buffer (Beyotime Institute of Biotechnology). Protein
concentrations were determined using the bicinchoninic acid method
(Beyotime Institute of Biotechnology). For each sample, 40 µg total
protein was run on an SDS-PAGE gel (15%), followed by transfer to a
polyvinylidene fluoride membrane (EMD Millipore, Billerica, MA,
USA). Membranes were blocked for 1.5 h in 5% BSA (cat. no. A8806;
Sigma-Aldrich; Merck KGaA) at 2–8°C. The membranes were incubated
with primary antibodies against nuclear factor of κ-light
polypeptide gene enhancer in B cells inhibitor α [IκBα; cat. no.
YS-(kt)-0907, phospho (p)-IκBα (cat. no. YS-KT1551) (Shanghai
Yansheng Biochemical Reagent Co., Ltd., Shanghai, China), NF-κB,
cleaved caspase-3 (cat. no. bs-0081R), B cell lymphoma-2 (Bcl-2;
cat. no. bs-20351R), apoptosis regulator BAX (Bax; cat. no.
bs-4564R), β-actin (cat. no. bs-0061R) and lamin-A (cat. no.
bs-1839R) (1:1,000; BIOSS) overnight at 4°C. Subsequently, the
membranes were incubated with goat anti-rabbit immunoglobulin
G-horseradish peroxidase antibodies (1:5,000; cat. no. A0208;
Beyotime Institute of Biotechnology) at room temperature for 1 h,
followed by chromogenic detection using an enhanced
chemiluminescence reagent (cat. no. WP20005; Thermo Fisher
Scientific, Inc.) Films were scanned and analyzed using
Gel-Pro-Analyzer 4.0 software (Media Cybernetics, Inc., Rockville,
MD, USA), and the optical densities of the target bands were
quantified relative to β-actin.
Nissl staining
Paraffin-embedded hippocampal tissues were cut into
5 µm sections, processed with conventional Nissl staining (31), and examined under a light microscope
(magnification, ×400).
ELISA
Commercially available ELISA kits were used to
detect interleukin-6 (IL-6; cat. no. ml002293), tumor necrosis
factor-α (TNF-α; cat. no. ml002095), interferon-γ (IFN-γ; cat. no.
ml027464), superoxide dismutase (SOD; cat. no. ml643059),
malondialdehyde (MDA; cat. no. ml077384), acetylcholine (Ach; cat.
no. ml401805) (Shanghai Enzyme-linked Biotechnology Co., Ltd.,
Shanghai, China) and Aβ (cat. no. JL14446-48T; Shanghai Jianglai
Industrial Ltd., Shanghai, China) expression levels in the
hippocampal tissues, according to the manufacturer's protocols.
Statistical analysis
Data are presented as the mean ± standard deviation.
In vitro experiments were repeated three times, whereas
in vivo experiments were conducted in six rats. Comparisons
between groups were performed using one-way analysis of variance
and Bonferroni post hoc tests. GraphPad Prism 5.0 (GraphPad
Software, Inc., La Jolla, CA, USA) was used to analyze all the data
and images. P<0.05 was considered to indicate a statistically
significant difference.
Results
Extraction, separation and
purification of Scue
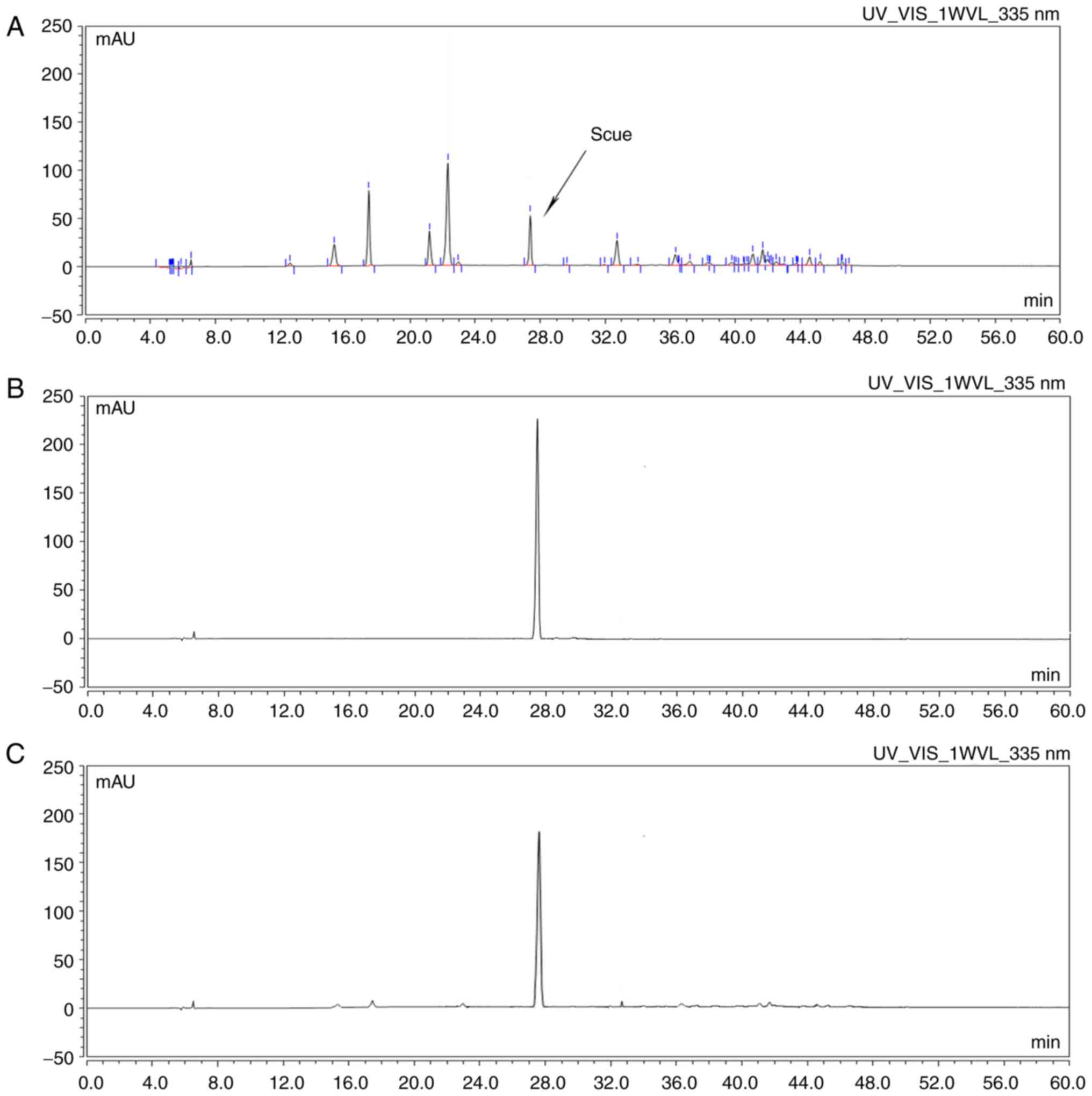
Scue was obtained as described above. The results
demonstrated that a single symmetrical peak was identified by HPLC;
the shape of the peak was sharp and steep, and the retention time
was the same as the reference substance (Fig. 1).
Scue attenuates Aβ-induced cell death
in PC12 cells
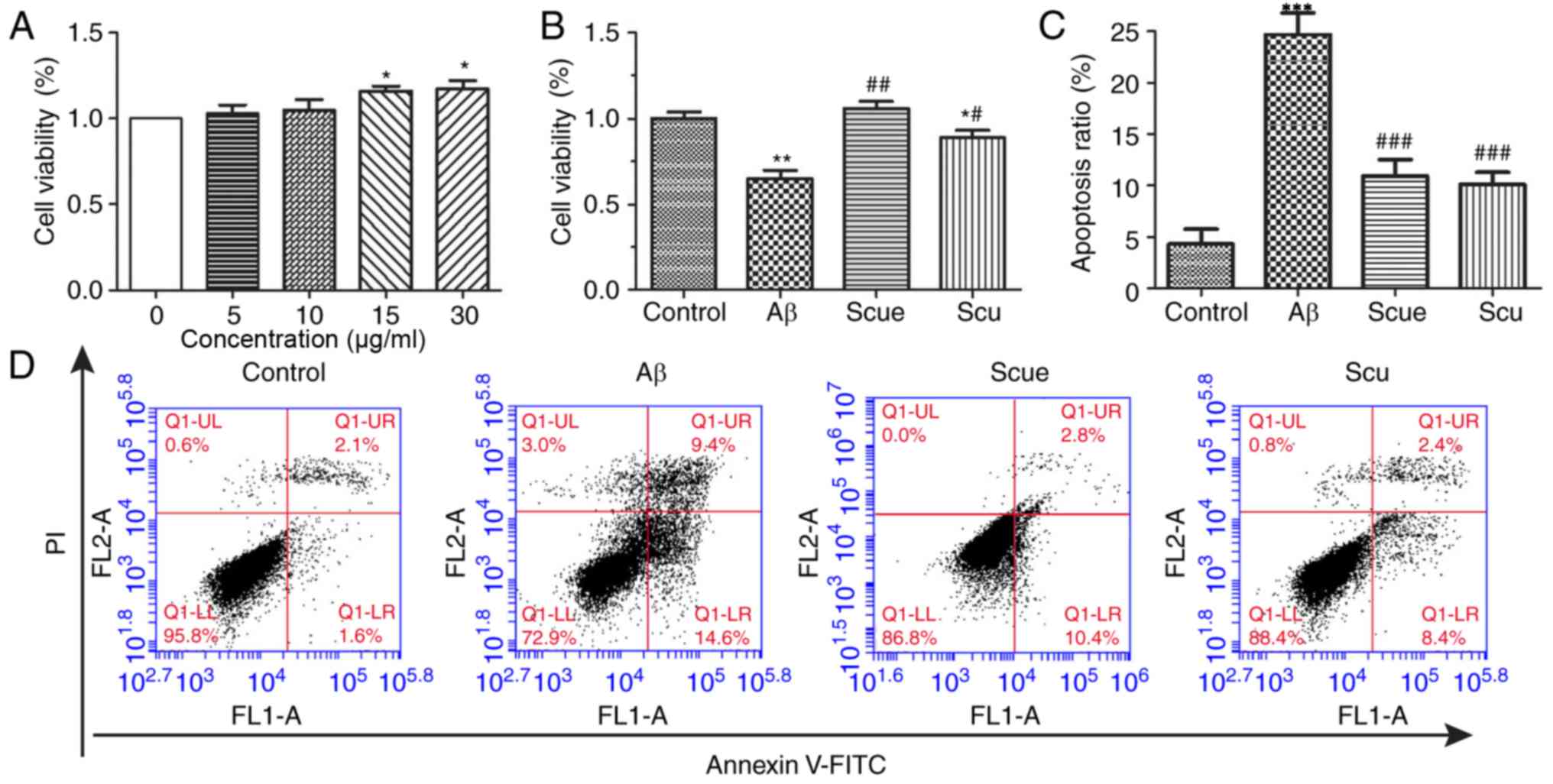
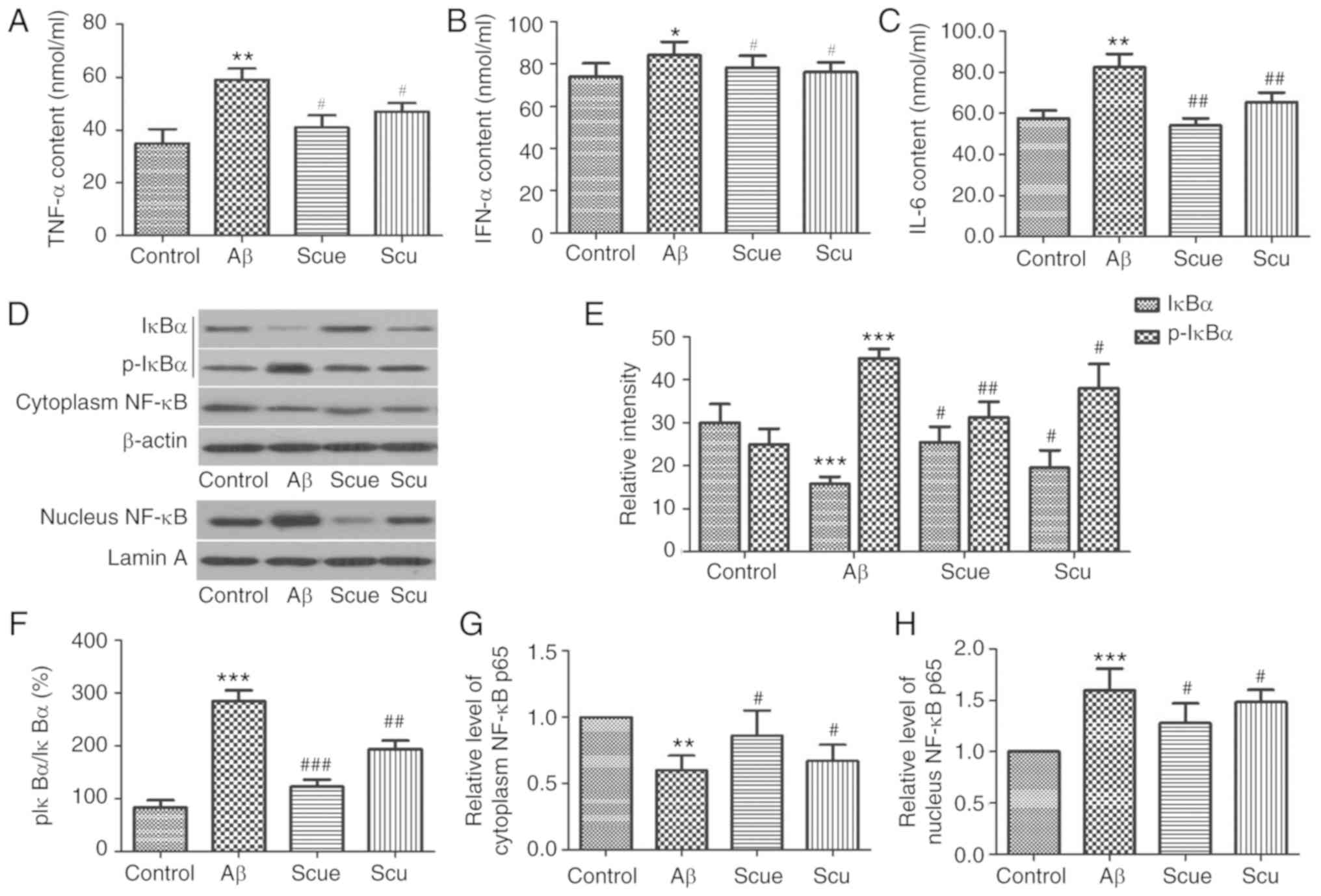
Cell viability was assessed by an MTT assay in order
to determine the effects of Scue on Aβ-induced cell death. To
determine the proper concentration ranges for the study of
neuroprotective effects, the cytotoxicity of each test compound was
evaluated using PC12 cells. Scue did not demonstrate any detectable
toxicity at any of the concentrations tested (Fig. 2A). The protective effects of Scue on
Aβ-induced cell death were measured. Treatment with 2 µg/ml Aβ for
24 h decreased cell viability by 31%, whereas, pretreatment with
Scue (30 µg/ml) significantly attenuated Aβ-induced cell death
(Fig. 2B; P<0.01). Aβ-induced
cell death was further investigated by flow cytometry. Treatment
with Aβ (2 µg/ml) significantly increased apoptosis compared with
the control group; however, pretreatment with Scue (30 µg/ml)
significantly decreased the number of apoptotic cells compared with
treatment with Aβ alone (P<0.001). Apoptotic ratios with respect
to the control group were as follows: 24.0% in the Aβ (2 µg/ml)
treatment group; 13.4% in the Scue (30 µg/ml) treatment group;
10.8% in the Scu (30 µg/ml) treatment group. Therefore, Scue and
Scu decreased the apoptotic ratios (Fig.
2C and D).
 | Figure 2.Scue alleviates Aβ-induced PC12 cell
death. (A) Cell viability following treatment with Scue at a range
of concentrations. P<0.05 vs. 0 µg/ml. (B) Cell viability
following treatment with Aβ and pretreatment with 30 µg/ml
Scu/Scue. (C) Cultured cells were double-stained with
FITC-conjugated anti-Annexin V antibody and PI, and subjected to
flow cytometry analysis of apoptotic cells. (D) Representative flow
cytometry plots are presented. Data are presented as the mean ±
standard deviation. n=3. *P<0.05, **P<0.01, ***P<0.001 vs.
control group; #P<0.05, ##P<0.01,
###P<0.001 vs. Aβ group. Aβ, amyloid β; PI, propidium
iodide; Scu, scutellarin; Scue, scutellarein; FITC, fluorescein
isothiocyanate; UL, upper left; UR, upper right; LL, lower left;
LR, lower right; FL1-A/FL2-A, area of fluorescence; Q,
quadrant. |
Scue suppresses NF-κB activation in
PC12 cells
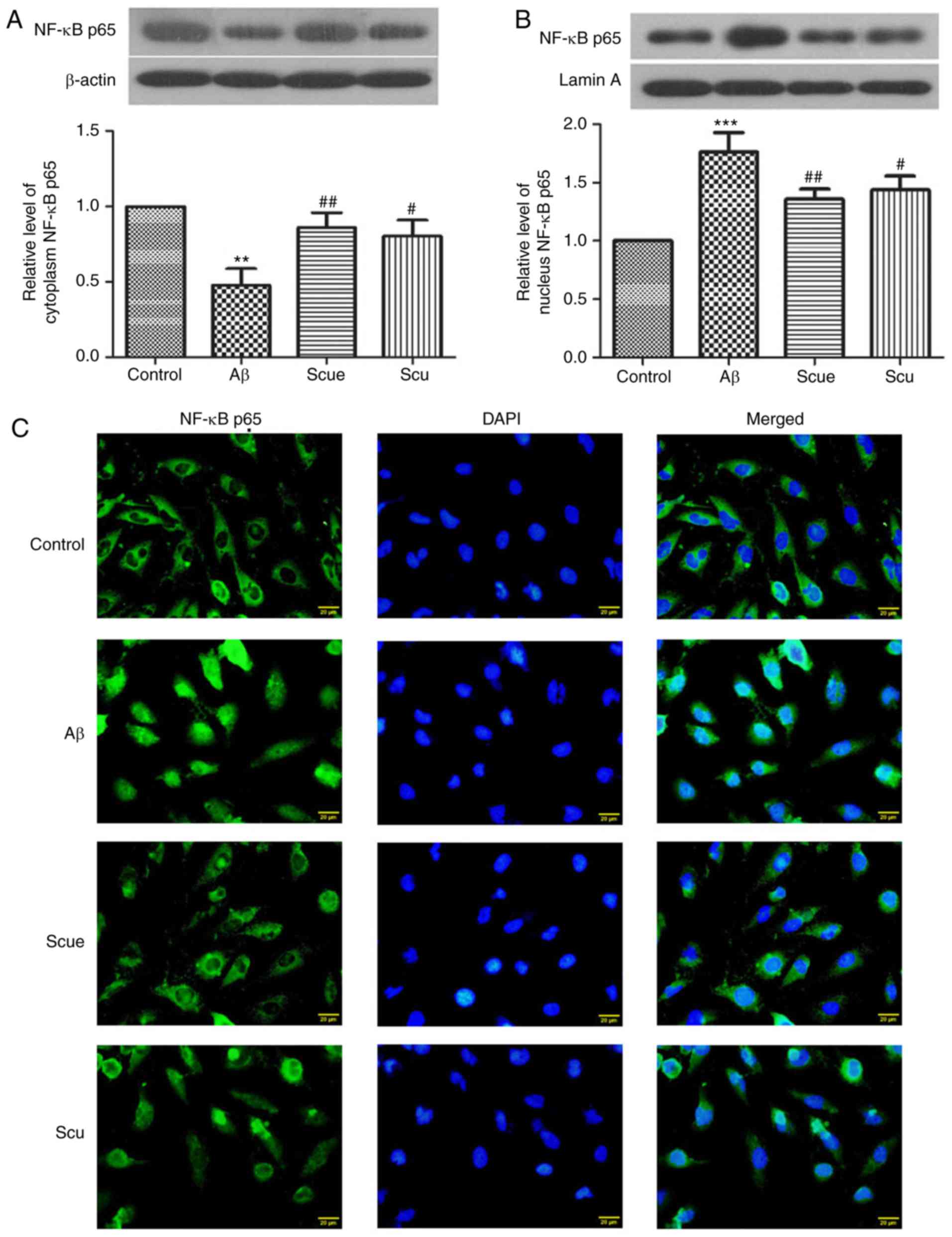
Western blotting was used to evaluate the expression
of NF-κB p65 in cells. Compared with the control group, cytoplasmic
NF-κB was significantly decreased by 54% (P<0.01; Fig. 3A) and nuclear NF-κB was significantly
increased by 1.549-fold (P<0.001; Fig. 3B) in the Aβ group. Scue and Scu
increased the expression level of cytoplasmic NF-κB compared with
the Aβ group (P<0.01 and P<0.05, respectively; Fig. 3A), and decreased the expression level
of nuclear NF-κB compared with the Aβ group (P<0.01 and
P<0.05, respectively; Fig. 3B).
This suggested that Scu and Scue inhibited the NF-κB signaling
pathway.
Immunofluorescence staining demonstrated that NF-κB
p65 was primarily expressed in the cytoplasm of the cells, and the
NF-κB p65 expression in the nucleus was increased in the Aβ group
compared with the control group (Fig.
3C). Treatment with Scu and Scue reversed the Aβ-induced
alterations in NF-κB p65 localization. These results suggested that
Scue may inhibit activation of the NF-κB signaling pathway in
Aβ-induced injury of PC12 cells.
Scue attenuates Aβ-induced cognitive
impairment and hippocampal alterations in rats
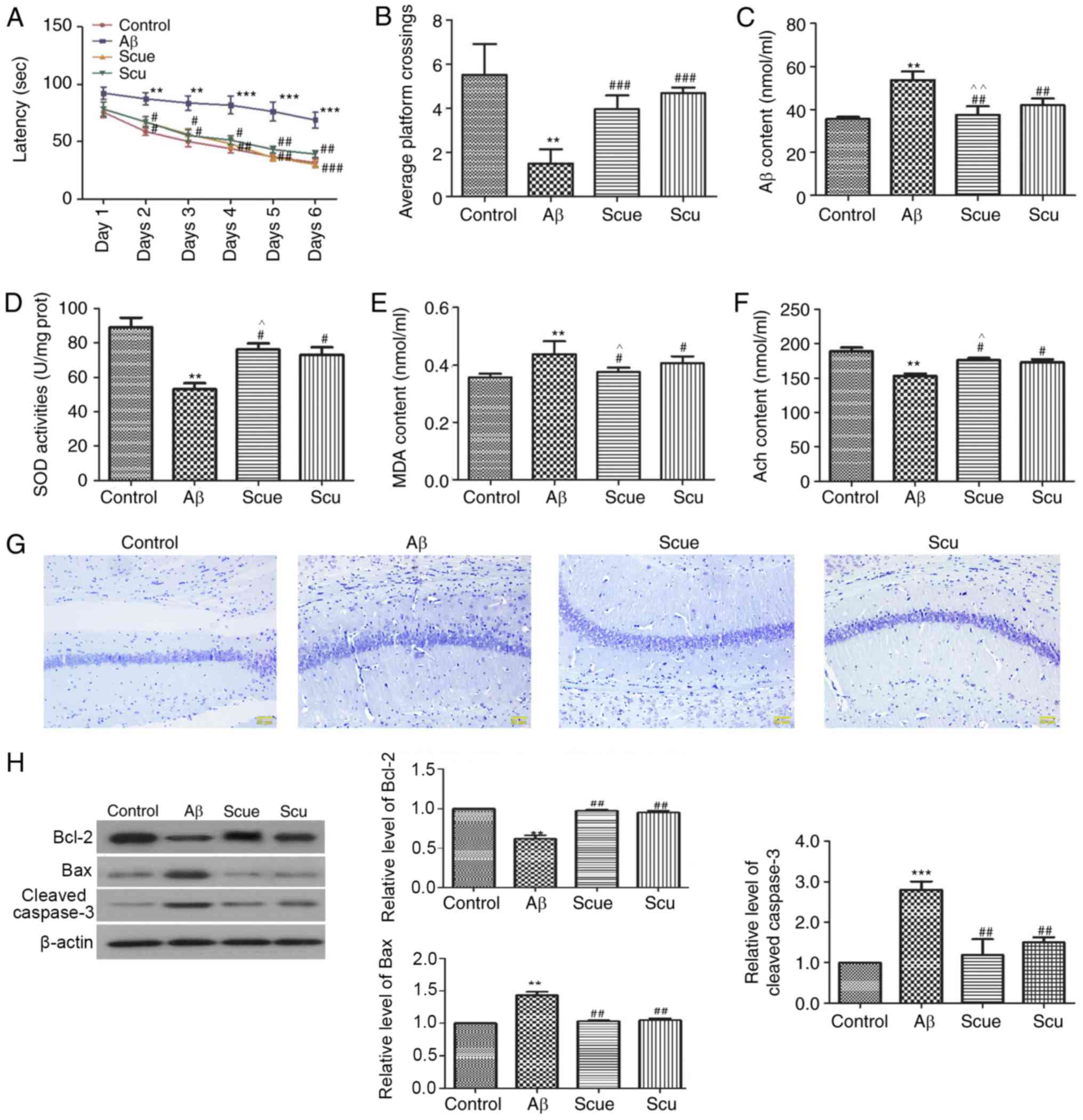
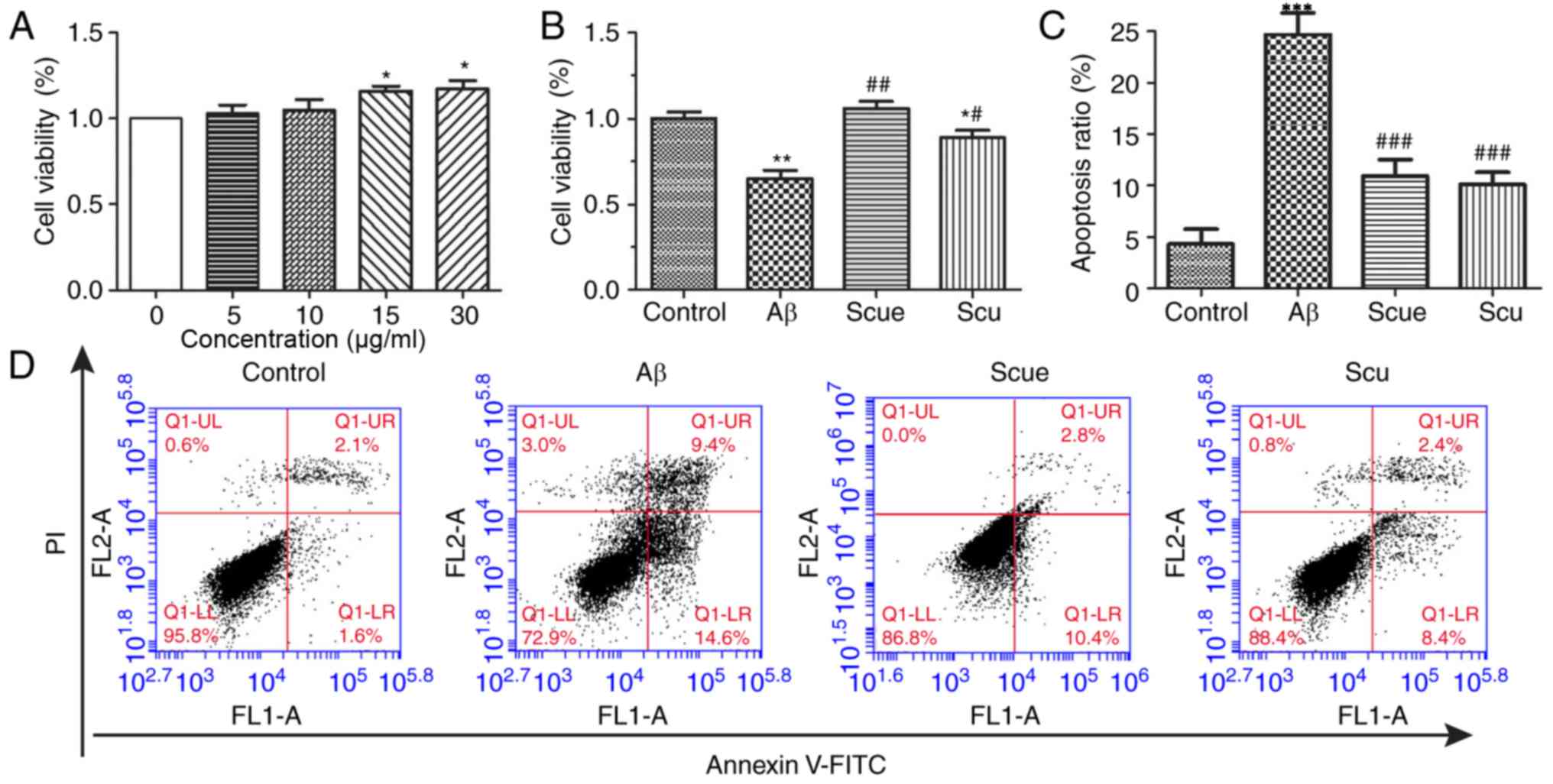
The MWM task was used to investigate the effects of
Scue on Aβ-induced spatial memory impairments. Rats in the Aβ group
at day 6 demonstrated significantly longer latencies to locate the
platform (68.25±8.67 sec) compared with the control group
(31.90±5.68 sec; P<0.001; Fig.
4A). Treatment with Scue significantly attenuated the effects
of Aβ-induced latency to locate the platform during the acquisition
period and increased the number of platform crossings in the
spatial probe trial (Fig. 4B;
P<0.001).
 | Figure 4.Scue attenuates Alzheimer's
disease-like pathology in rats. (A) Latency of crossings and (B)
average number of crossings in the Morris water maze spatial probe
test of memory. Hippocampal expression of (C) Aβ, (D) SOD, (E) MDA
and (F) Ach. (G) Nissl staining in the hippocampus. Scale bar, 50
µm. The expression levels of (H) Bcl-2, Bax and cleaved-caspase-3
were detected by western blotting. Densitometry analyses were
conducted using β-actin as an internal reference. Representative
results from repeated experiments are presented and data are
presented as the mean ± standard deviation. n=6. **P<0.01,
***P<0.001 vs. the control group; #P<0.05,
##P<0.01, ###P<0.001 vs. the Aβ group.
^P<0.05, ^^P<0.01 vs. the Scu group.
Aβ, amyloid β; Scu, scutellarin; Scue, scutellarein; SOD,
superoxide dismutase; MDA, malondialdehyde; Ach, acetylcholine;
Bcl-2, B cell lymphoma-2; Bax, apoptosis regulator BAX. |
ELISA was used for the analysis of hippocampal
tissues from each of the groups. The Aβ content was increased
1.45-fold in the Aβ group relative to the control group (Fig. 4C; P<0.01), and decreased 0.05-fold
in the Scue group compared with in the Scu group (P<0.01). SOD
expression was decreased 0.35-fold in the Aβ group (Fig. 4D; P<0.01), and increased 0.04-fold
in the Scue group compared with in the Scu group (P<0.05).
The MDA content in the hippocampal tissues was
significantly increased in the Aβ group by 118% relative to the
control (P<0.01; Fig. 4E), and
decreased 0.05-fold in the Scue group compared with in the Scu
group (P<0.05). Hippocampal Ach content was significantly
decreased by 79% relative to the control (P<0.01; Fig. 4F), and increased 0.06-fold in the
Scue group compared with in the Scu group (P<0.05). These
observations were significantly reversed by treatment with
Scu/Scue, with Scue presenting more prominent effects
(P<0.05).
Nissl staining was used to assess neurons in the
hippocampus. Fewer neurons were labeled in the Aβ group compared
with the control group. Furthermore, numerous cells demonstrated an
irregular arrangement and loss of cytomorphology in samples from
the Aβ group. Treatment with Scu/Scue improved the cytomorphology
of the hippocampal neurons (Fig.
4G).
Western blotting was used to evaluate the
hippocampal expression of proteins associated with apoptosis,
including Bcl-2, Bax and cleaved caspase-3. The expression level of
Bcl-2 in the Aβ group was reduced to 57% of that in the control
group (P<0.01; Fig. 4H), whereas,
expression levels of Bax (1.34-fold; P<0.01; Fig. 4H) and cleaved caspase-3 (2.60-fold;
P<0.001; Fig. 4H) were increased.
In the Scue 50 mg/kg group, expression levels of Bcl-2, Bax and
cleaved caspase-3 were similar to those observed in the control
group (Fig. 4H). In general,
treatment with Scu/Scue attenuated the Aβ-induced alterations in
the hippocampus, with Scue presenting more prominent effects
compared with Scu.
Scue suppresses Aβ-induced hippocampal
neuroinflammation and NF-κB activation
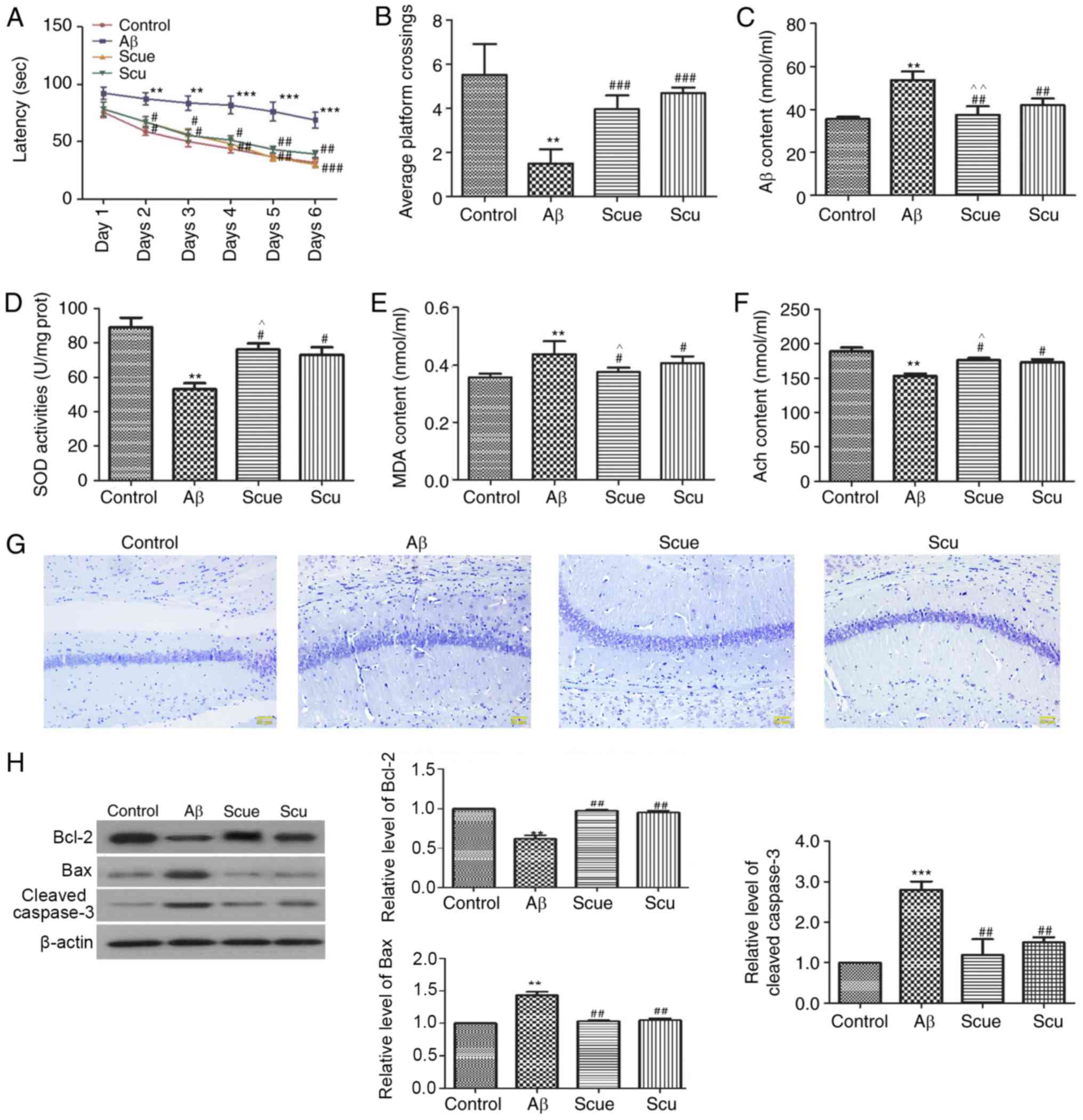
To assess the mechanism of the effects of Scue on
Aβ-induced alterations in the hippocampus, the expression levels of
TNF-α, IFN-γ and IL-6 were determined by ELISA. Compared with the
control group, the expression levels of TNF-α (P<0.01; Fig. 5A), IFN-γ (P<0.05; Fig. 5B) and IL-6 (P<0.01; Fig. 5C) in the hippocampi of Aβ-treated
rats were significantly increased; however, these increases were
significantly decreased by treatment with Scue (all P<0.05;
Fig. 5A-C) compared with treatment
with Aβ alone. Subsequently, the NF-κB signaling pathway was
investigated: Hippocampal expressions levels of IκBα and p-IκBα in
addition to expression levels of NF-κB in the cytoplasm and the
nucleus were determined by western blotting. Compared with the
control group, in the Aβ group, the phosphorylation of IκBα level
was significantly increased and the expression of hippocampal IκBα
was significantly decreased (P<0.001; Fig. 5D and E). The ratio of p-IκBα/IκBα was
83.3% in the control group and 300% in the Aβ group (P<0.001;
Fig. 5F), and cytoplasmic NF-κB was
reduced to 64% of control (P<0.01; Fig. 5G). Nuclear NF-κB was significantly
increased by 1.54-fold (P<0.01; Fig.
5H). Scue significantly increased the expression of IκBα
(P<0.05) and decreased the phosphorylation of IκBα (P<0.01;
Fig. 5D and E). Scue additionally
increased the cytoplasmic NF-κB (P<0.05; Fig. 5G) and decreased the nuclear NF-κB
(P<0.05; Fig. 5H) compared with
the Aβ group. Aβ-associated alterations in NF-κB were significantly
attenuated by treatment Scue, suggesting that Scue decreased the
phosphorylation of IκBα and subsequently inhibited activation of
NF-κB signaling in the hippocampus.
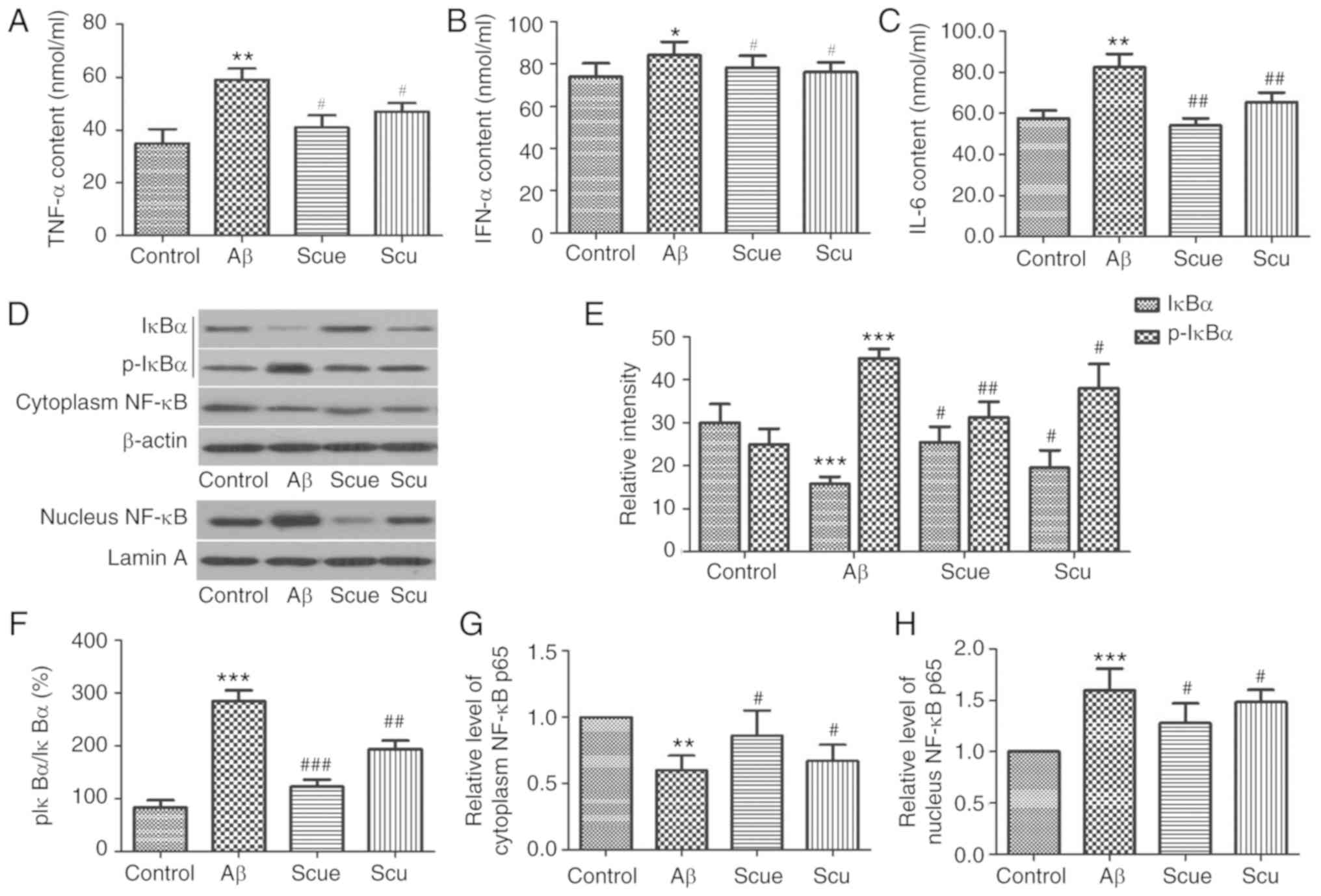 | Figure 5.Scue suppresses Aβ-induced
hippocampal inflammation and NF-κB activation in rats. Hippocampal
expression of (A) TNF-α, (B) IFN-α and (C) IL-6. (D) Hippocampal
expression of IκBα, p-IκBα, nuclear NF-κB p65 and cytoplasmic NF-κB
p65 as detected by western blotting. Densitometry analyses of (E)
IκBα, (F) ratio of p-IκBα to IκBα, (G) cytoplasmic NF-κB p65 and
(H) nuclear NF-κB p65 using β-actin and lamin A as internal
controls. Representative results of a number of experimental
replicates are presented and data are presented as the mean ±
standard deviation. n=6. *P<0.05, **P<0.01, ***P<0.001 vs.
the respective control group; #P<0.05,
##P<0.01, ###P<0.001 vs. the respective
Aβ group. Aβ, amyloid β; Scu, scutellarin; Scue, scutellarein;
TNF-α, tumor necrosis factor-α; IFN-α, interferon-α; IL-6,
interleukin-6; NF-κB, nuclear factor κ-light-chain-enhancer of
activated B cells p65; IκBα, nuclear factor of κ-light polypeptide
gene enhancer in Bcells inhibitor α; p, phospho. |
Discussion
The diverse biological effects of traditional
Chinese medicines are attracting an increasing amount of attention
in modern therapeutics. In previous studies, Scu exhibited
therapeutic effects in a variety of diseases (32–34). In
the present study, the possibility for the use of Scue in the
treatment of AD was investigated using in vitro and in
vivo models of cell death and Aβ-associated pathology.
The rat PC12 cell line has been widely used to
evaluate the neuroprotective effects of bioactive reagents.
Furthermore, this cell line is particularly sensitive to Aβ-induced
injury (35–37). Therefore, the PC12 cell line was used
for the therapeutic evaluation of Scue. Similar to previous
studies, 2 µg/ml Aβ induced ~32% cell death, whereas, pretreatment
with Scue inhibited Aβ-induced apoptosis (9,38), thus,
demonstrating that Scue may protect against the pro-apoptotic
cellular effects of Aβ in vitro.
The MWM test is commonly used to study spatial
learning and memory in animals, and is considered to be a reliable
preclinical tool (39,40). In the present study, group
differences in the escape latencies in the training trials and in
the number of passes over the original platform location in the
probe trial demonstrated that Aβ compromised rodent learning and
memory performance, and treatment with Scu/Scue protected against
the Aβ-induced cognitive impairments. It was previously
demonstrated that the deposition of Aβ in the brain represents an
important event in the etiology and pathology of AD (41,42).
According to the free radical theory, oxidative stress additionally
contributes to the pathogenesis of AD (43); furthermore, decreases in Ach are
associated with AD (44). In the
present study, Scue decreased hippocampal Aβ and MDA content whilst
increasing SOD and Ach expression, suggesting that Scutellaria
baicalensis and its constituent Scue exhibit significant
therapeutic potential for the treatment of AD-associated
pathology.
The Nissl body is a structural characteristic of
neurons that is present in neuronal cell bodies and dendrites.
Nissl staining is a widely-used method for observing the
cytomorphology of neurons (45).
Consistent with the results of the present study, it was previously
demonstrated that neuronal damage is a principle cause of AD
(46). Nissl staining of the
hippocampus demonstrated that neurons were arranged in disorderly
patterns in the Aβ group animals, indicative of severe neuronal
damage. Furthermore, it was hypothesized that hippocampal apoptosis
underlies learning and memory deficits in AD (47). The apoptotic suppressor Bcl-2 serves
an important role in apoptosis together with the pro-apoptotic
protein Bax. Specifically, the ratio of Bax to Bcl-2 determines
whether apoptosis occurs (48).
Caspase-3 serves a similarly pivotal role in the apoptosis pathway
(49). The present study
demonstrated that Scue not only protected against apoptosis
associated with Aβ exposure in vitro; however, additionally
counteracted Aβ-induced decreases in the anti-apoptotic protein
Bcl-2 expression level and suppressed the expression of
pro-apoptotic proteins Bax and cleaved caspase-3 in vivo,
suggesting that Scue exhibits neuroprotective and anti-apoptotic
properties in a rodent model of AD.
NF-κB is a dimeric signaling complex that exists
stably in the cytoplasm when bound to IκBα. In response to external
stimuli, IκBα may be phosphorylated, resulting in the dissociation
of IκBα from NF-κB and the nuclear translocation of NF-κB to
initiate the transcription of certain genes that lead to
inflammation and apoptosis (50,51). The
present study demonstrated that Scue inhibited Aβ-induced
phosphorylation of IκBα, thereby restricting the activation and
nuclear translocation of NF-κB. Future studies are required to
determine whether the inhibition of NF-κB activation underlies the
beneficial effects of treatment with Scue in rodent AD, or instead,
whether decreases in NF-κB activation occur as a consequence of the
observed anti-inflammatory and antioxidative effects.
In summary, Scue inhibited Aβ-induced PC12 cell
apoptosis, and protected against AD-associated pathology and
cognitive impairment in rats possibly by decreasing apoptosis in
the hippocampus. These results demonstrated a potential therapeutic
use for Scue in AD.
Acknowledgements
Not applicable.
Funding
The present study was supported by the following
grants: The Scientific Research of Traditional Chinese Medicine
Industry ‘The protection and utilization of traditional Chinese
medicine resources in the representative area of China’ (grant no.
201207002); Protection and Utilization of Traditional Chinese
Medicine Resources on behalf of Jilin Province (grant no.
201207002-05; China). Jilin Province Traditional Chinese Medicine
Science and Technology Project (grant no. 2017014; China); and
Jilin Provincial Health and Family Planning Commission Science and
Technology Project (grant no. 2017Q046; China). Training project
for hundred of young and middle-aged core teachers of Changchun
University of Chinese Medicine.
Availability of data and materials
The datasets used during the present study are
available from the corresponding author upon reasonable
request.
Authors' contributions
XBQ and MHD designed the study. XWH, YX, XS, HL,
JMX, DH, DDY were responsible for experiments. GFL and YXL
conducted experiments and analyzed data.
Ethics approval and consent to
participate
The animal care and treatment protocols were
approved by the Experimental Animal Ethics Committee of Jilin
University (Changchun, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Duits FH, Teunissen CE, Bouwman FH, Visser
PJ, Mattsson N, Zetterberg H, Blennow K, Hansson O, Minthon L,
Andreasen N, et al: The cerebrospinal fluid ‘Alzheimer profile’:
Easily said, but what does it mean? Alzheimers Dement.
10:713–723.e2. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wortmann M: Dementia: A global health
priority-highlights from an ADI and World Health Organization
report. Alzheimers Res Ther. 4:402012.PubMed/NCBI
|
|
3
|
Blennow K, de Leon MJ and Zetterberg H:
Alzheimer's disease. Lancet. 368:387–403. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bagheri M, Joghataei MT, Mohseni S and
Roghani M: Genistein ameliorates learning and memory deficits in
amyloid β(1–40) rat model of Alzheimer's disease. Neurobiol Learn
Mem. 95:270–276. 2011. View Article : Google Scholar : PubMed/NCBIPubMed/NCBI
|
|
5
|
He FQ, Qiu BY, Zhang XH, Li TK, Xie Q, Cui
DJ, Huang XL and Gan HT: Tetrandrine attenuates spatial memory
impairment and hippocampal neuroinflammation via inhibiting NF-κB
activation in a rat model of Alzheimer's disease induced by
amyloid-β(1–42). Brain Res. 1384:89–96. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhou J, Zhou L, Hou D, Tang J, Sun J and
Bondy SC: Paeonol increases levels of cortical cytochrome oxidase
and vascular actin and improves behavior in a rat model of
Alzheimer's disease. Brain Res. 1388:141–147. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Song JX, Lin X, Wong RN, Sze SC, Tong Y,
Shaw PC and Zhang YB: Protective effects of dibenzocyclooctadiene
lignans from Schisandra chinensis against beta-amyloid and
homocysteine neurotoxicity in PC12 cells. Phytother Res.
25:435–443. 2011.PubMed/NCBI
|
|
8
|
Dargahi L, Nasiraei-Moghadam S, Abdi A,
Khalaj L, Moradi F and Ahmadiani A: Cyclooxygenase (COX)-1 activity
precedes the COX-2 induction in Aβ-induced neuroinflammation. J Mol
Neurosci. 45:10–21. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zeng YQ, Cui YB, Gu JH, Liang C and Zhou
XF: Scutellarin mitigates Aβ-induced neurotoxicity and improves
behavior impairments in AD mice. Molecules. 23:E8692018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Baluchnejadmojarad T, Zeinali H and
Roghani M: Scutellarin alleviates lipopolysaccharide-induced
cognitive deficits in the rat: Insights into underlying mechanisms.
Int Immunopharmacol. 54:311–319. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chledzik S, Strawa J, Matuszek K and
Nazaruk J: Pharmacological effects of scutellarin, an active
component of genus scutellaria and erigeron: A systematic review.
Am J Chin Med. 46:319–337. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sun CY, Zhu Y, Li XF, Wang XQ, Tang LP, Su
ZQ, Li CY, Zheng GJ and Feng B: Scutellarin increases
cisplatin-induced apoptosis and autophagy to overcome cisplatin
resistance in non-small cell lung cancer via ERK/p53 and c-met/AKT
signaling pathways. Front Pharmacol. 9:922018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yan WJ and Zhang SQ: Inhibition Mechanism
of Baicalein on the Liver Metastasis of Breast Cancer cell in Vivo.
Pract J Cancer. 33:1915–1919. 2018.
|
|
14
|
Liu W, Liu ZY, Qi HW, et al: Enhancement
role of baicalein used as adjuvant on the immuno-response of
-Tcells in vivo of mice with melanoma. Prac J Med Pharm.
35:1114–1118. 2018.
|
|
15
|
Li Q, Chen Y, Zhang X, Zuo S, Ge H, Chen
Y, Liu X, Zhang JH, Ruan H and Feng H: Scutellarin attenuates
vasospasm through the Erk5-KLF2-eNOS pathway after subarachnoid
hemorrhage in rats. J Clin Neurosci. 34:264–270. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mo J, Yang R, Li F, Zhang X, He B, Zhang
Y, Chen P and Shen Z: Scutellarin protects against vascular
endothelial dysfunction and prevents atherosclerosis via
antioxidation. Phytomedicine. 42:66–74. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Huang H, Geng Q, Yao H, Shen Z, Wu Z, Miao
X and Shi P: Protective effect of scutellarin on myocardial
infarction induced by isoprenaline in rats. Iran J Basic Med Sci.
21:267–276. 2018.PubMed/NCBI
|
|
18
|
Yang N, Zhao Y, Wang Z, Liu Y and Zhang Y:
Scutellarin suppresses growth and causes apoptosis of human
colorectal cancer cells by regulating the p53 pathway. Mol Med Rep.
15:929–935. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yang H, Du Y, Wan S, Trahan GD, Jin Y and
Zhang W: Mesoporous 2D covalent organic frameworks based on
shape-persistent arylene-ethynylene macrocycles. Chem Sci.
6:4049–4053. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Erbele ID, Lin FR, Agrawal Y, Francis HW,
Carey JP and Chien WW: Racial differences of pigmentation in the
human vestibular organs. Otolaryngol Head Neck Surg. 155:479–484.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hou L, Chen L and Fang L: Scutellarin
inhibits proliferation, invasion, and tumorigenicity in human
breast cancer cells by regulating HIPPO-YAP signaling pathway. Med
Sci Monit. 23:5130–5138. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tang H, Tang Y, Li NG, Lin H, Li W, Shi Q,
Zhang W, Zhang P, Dong Z, Shen M, et al: Comparative metabolomic
analysis of the neuroprotective effects of scutellarin and
scutellarein against ischemic insult. PLoS One. 10:e01315692015.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Thirusangu P, Vigneshwaran V, Vijay Avin
BR, Rakesh H, Vikas HM and Prabhakar BT: Scutellarein antagonizes
the tumorigenesis by modulating cytokine VEGF mediated
neoangiogenesis and DFF-40 actuated nucleosomal degradation.
Biochem Biophys Res Commun. 484:85–92. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mamadalieva NZ, Herrmann F, El-Readi MZ,
Tahrani A, Hamoud R, Egamberdieva DR, Azimova SS and Wink M:
Flavonoids in Scutellaria immaculata and S. ramosissima (Lamiaceae)
and their biological activity. J Pharm Pharmacol. 63:1346–1357.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ni G, Tang Y, Li M, He Y and Rao G:
Synthesis of scutellarein derivatives with a long aliphatic chain
and their biological evaluation against human cancer cells.
Molecules. 23:E3102018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Estevez-Garcia IO, Gallegos-Nava S,
Vera-Pérez E, Silveira LH, Ventura-Ríos L, Vancini G,
Hernández-Díaz C, Sánchez-Muñoz F, Ballinas-Verdugo MA, Gutierrez
M, et al: Levels of cytokines and microRNAs in individuals with
asymptomatic hyperuricemia and ultrasonographic findings of gout: A
bench-to-bedside approach. Arthritis Care Res (Hoboken).
70:1814–1821. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Devkota K, Wang YH, Liu MY, Li Y and Zhang
YW: Case report: III° atrioventricular block due to fulminant
myocarditis managed with non-invasive transcutaneous pacing.
Version 2. F1000Res. 7:2392018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
van der Stelt M, Mazzola C, Esposito G,
Matias I, Petrosino S, De Filippis D, Micale V, Steardo L, Drago F,
Iuvone T and Di Marzo V: Endocannabinoids and beta-amyloid-induced
neurotoxicity in vivo: Effect of pharmacological elevation of
endocannabinoid levels. Cell Mol Life Sci. 63:1410–1424. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Yamaguchi Y, Higashi M, Matsuno T and
Kawashima S: Ameliorative effects of azaindolizinone derivative
ZSET845 on scopolamine-induced deficits in passive avoidance and
radial-arm maze learning in the rat. Jpn J Pharmacol. 87:240–244.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ma Y, Wang Q, Liu F, Ma X, Wu L, Guo F,
Zhao S, Huang F and Qin G: KLF5 promotes the tumorigenesis and
metastatic potential of thyroid cancer cells through the NF-κB
signaling pathway. Oncol Rep. 40:2608–2618. 2018.PubMed/NCBI
|
|
31
|
Liao J and Dong W: Effects of donepezil
and verapamilon on learning and memory function in Alzheimer's
disease rat model. China Academica Journal Electronic Publishing
House. 34:58–60. 2012.
|
|
32
|
Hu D, Li C, Han N, Miao L, Wang D, Liu Z,
Wang H and Yin J: Deoxyschizandrin isolated from the fruits of
Schisandra chinensis ameliorates Aβ1−42-induced memory
impairment in mice. Planta Med. 78:1332–1336. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kim SR, Lee MK, Koo KA, Kim SH, Sung SH,
Lee NG, Markelonis GJ, Oh TH, Yang JH and Kim YC:
Dibenzocyclooctadiene lignans from Schisandra chinensis protect
primary cultures of rat cortical cells from glutamate-induced
toxicity. J Neurosci Res. 76:397–405. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yan T, Shang L, Wang M, Zhang C, Zhao X,
Bi K and Jia Y: Lignans from Schisandra chinensis ameliorate
cognition deficits and attenuate brain oxidative damage induced by
D-galactose in rats. Metab Brain Dis. 31:653–661. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Tang YY and Tang XQ: Research progress in
the neurobiological effects of hydrogen sulfide. Sheng Li Ke Xue
Jin Zhan. 48:42–51. 2017.(In Chinese). PubMed/NCBI
|
|
36
|
Hu BL and Guo CY: Advances achievements
about neuroprotective mechanisms of paeoniflorin. Acta
Neuropharmacologica. 5:51–56. 2015.
|
|
37
|
Jang JH and Surh YJ: Protective effect of
resveratrol on beta-amyloid-induced oxidative PC12 cell death. Free
Radic Biol Med. 34:1100–1110. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Qu HM, Liu SJ and Zhang CY: Antitumor and
antiangiogenic activity of Schisandra chinensis polysaccharide in a
renal cell carcinoma model. Int J Biol Macromol. 66:52–56. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Moosavi M, Khales GY, Abbasi L, Zarifkar A
and Rastegar K: Agmatine protects against scopolamine-induced water
maze performance impairment and hippocampal ERK and Akt
inactivation. Neuropharmacology. 62:2018–2023. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Shi J, Liu Q, Wang Y and Luo G:
Coadministration of huperzine A and ligustrazine phosphate
effectively reverses scopolamine-induced amnesia in rats. Pharmacol
Biochem Behav. 96:449–453. 2010.
|
|
41
|
Dong Y, Xu Z, Zhang Y, McAuliffe S, Wang
H, Shen X, Yue Y and Xie Z: RNA interference-mediated silencing of
BACE and APP attenuates the isoflurane-induced caspase activation.
Med Gas Res. 1:52011. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zhang J, Dong Y, Xu Z, Zhang Y, Pan C,
McAuliffe S, Ichinose F, Yue Y, Liang W and Xie Z:
2-Deoxy-D-glucose attenuates isoflurane-induced cytotoxicity in an
in vitro cell culture model of H4 human neuroglioma cells. Anesth
Analg. 113:1468–1475. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Valko M, Leibfritz D, Moncol J, Cronin MT,
Mazur M and Telser J: Free radicals and antioxidants in normal
physiological functions and human disease. Int J Biochem Cell Biol.
39:44–84. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Moreira FTC, Sale MGF and Di Lorenzo M:
Towards timely Alzheimer diagnosis: A self-powered amperometric
biosensor for the neurotransmitter acetylcholine. Biosens
Bioelectron. 87:607–614. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Engblom M, Alexanderson K, Englund L,
Norrmén G and Rudebeck CE: When physicians get stuck in
sick-listing consultations: A qualitative study of categories of
sick-listing dilemmas. Work. 35:137–142. 2010.PubMed/NCBI
|
|
46
|
Knezovic A, Osmanovic-Barilar J, Curlin M,
Hof PR, Simic G, Riederer P and Salkovic-Petrisic M: Staging of
cognitive deficits and neuropathological and ultrastructural
changes in streptozotocin-induced rat model of Alzheimer's disease.
J Neural Transm (Vienna). 122:577–592. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Heo K, Cho YJ, Cho KJ, Kim HW, Kim HJ,
Shin HY, Lee BI and Kim GW: Minocycline inhibits caspase-dependent
and -independent cell death pathways and is neuroprotective against
hippocampal damage after treatment with kainic acid in mice.
Neurosci Lett. 398:195–200. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Bu P, Keshavarzian A, Stone DD, Liu J, Le
PT, Fisher S and Qiao L: Apoptosis: One of the mechanisms that
maintains unresponsiveness of the intestinal mucosal immune system.
J Immunol. 166:6399–6403. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Steinberg I, McCoy HI and Dotter CT:
Angiocardiographic findings in pulmonary tuberculosis. Dis Chest.
19:510–520. 1951. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Gilmore TD and Wolenski FS: NF-κB: Where
did it come from and why? Immunol Rev. 246:14–35. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Yang LP, Zhu XA and Tso MO: Role of
NF-kappaB and MAPKs in light-induced photoreceptor apoptosis.
Invest Ophthalmol Vis Sci. 48:4766–4776. 2007. View Article : Google Scholar : PubMed/NCBI
|