Introduction
Gastric cancer is one of the most common epithelial
malignant types of cancer, and is a serious threat to human health
(1). Due to specific eating habits,
climate and geographical position, China is one of the countries
with the highest incidence of gastric cancer (2). Numerous factors have been reported to
contribute to the occurrence of gastric cancer, including
helicobacter pylori infection (3), lifestyle (4), socioeconomic status (5), environmental (6) and genetic factors (7–9). For
gastric cancer in the early stages of disease, surgical resection
is the primary therapeutic strategy, whereas the conventional
treatment for advanced gastric cancer is surgical resection
combined with chemotherapy (10,11).
However, chemotherapy drugs do not only destroy tumor cells, but
also attack normal cells, which can result in severe side effects
for the patient (12). Therefore,
efforts should be made to develop safe tumor-targeting therapeutic
strategies.
Previous studies have focused on using
ultrasound-triggered microbubble destruction (UTMD) for the
treatment of cancer (13,14). Lipid microbubbles, which are widely
used as acoustic contrast agents, are also considered to function
as good carriers for drug delivery (15–17). The
diameter of a nanoscale lipid microbubble is shorter than that of a
red blood cell, therefore, it can freely flow with the blood into
the pulmonary circulation without blocking it (18). In addition, a nanoscale lipid
microbubble can pass through the vascular endothelial cell gap to
reach the tissues outside the vessels (18). Drugs loaded lipid microbubbles
(DLLMs) can be monitored dynamically by ultrasound (19). Once the microbubbles gather in a
tumor-containing organ, relatively low-dose ultrasound was used to
irradiate the target organ to destroy the microbubble and release
the drugs (19). Following
ultrasound irradiation, the loaded drug was rapidly released to the
target region to form a relatively high drug concentration
(19,20). Furthermore, ultrasound-induced
mechanical stress resulting in an enlarged cell gap and increased
permeability of the cell membrane has been shown to further
increase the intracellular diffusion of the drug (21–24).
Therefore, UTMD combined with DLLD may serve as an effective
tumor-targeting strategy.
Docetaxel (DOC), a well-known anti-cancer drug, has
been demonstrated to be effective for the treatment of advanced
gastric cancer (25–27). In the present study, lipid
microbubbles containing DOC were prepared, and the effects of
DOC-loaded microbubbles combined with UTMD on the growth of a
gastric cell line were investigated.
Materials and methods
Preparation of DLLD
The DOC-loaded lipid microbubble (DLLD) was prepared
as previously described (28).
Briefly, 1,2-Dipalmitoyl-sn-glycero-3-phosphocholine,
Distearoylphosphatidylcholine, Dipalmitoyl phosphatidylethanolamine
(all from Sigma-Aldrich, Darmstadt, Germany) and DOC
(MedChemExpress, Monmouth Junction, NJ, USA) were mixed to a mass
ratio of 1:5:2:2. The mixture was dissolved in chloroform and
methanol (1:1, v:v) solution. Following rotary vacuum evaporation,
glycerol/PBS (1:9, v:v) was added to form DOC/lipid solution (20
mg/ml). Following perfusion with perfluoropropane gas and
mechanical vibration, DLLD was obtained. The unembedded DOC was
removed by washing in PBS for 15 min at 4°C. The entrapment
efficiency of DLLD was determined by Reverse-Phase High Performance
Liquid Chromatography (RP-HPLC; Dalian Elite Analytical Instruments
Co., Ltd,). The reverse-phase SinoChrom ODS-BP column (200 × 4.6 mm
i.d., pore size 5 µm; Dalian Elite Analytical Instruments Co.,
Ltd.,) was used at a temperature of 30°C. The mobile phase was
composed of methanol/acetonitrile/water (50:30:20; v/v) at a flow
rate of 1 ml/min. UV absorbance detection was set at 230 nm. The
sample quantity was 20 µl. A series of dilutions of DOC (0.1, 0.5,
2.5, 10, 25, 50 and 100 µg/ml) were made to detect the area under
the curve, and a linear calibration curve correlating the area
under the curve and concentration of DOC was constructed. The
concentration of free DOC was calculated according to the linear
calibration curve.
Cell culture and treatment
The gastric cancer cell line BGC-823 was purchased
from the Shanghai Institute of Cell Biology (Shanghai, China) and
maintained in DMEM medium (Thermo Fisher Scientific, Inc., Waltham,
MA, USA) containing 10% FBS (Thermo Fisher Scientific, Inc.)
supplemented with 100 U/ml penicillin and 100 µg/ml streptomycin.
In the present study, BGC-823 cells were divided into 4 groups:
Control, DOC, DLLD and DLLD + UTMD. In the control group, BGC-823
cells were treated with PBS. In the DOC group, BGC-823 cells were
treated with 4 µM DOC. In the DLLD group, DLLD (21.3 mg/l) which
was equal to 4 µM DOC was used. In the DLLD plus UTMD group,
DLLD-treated cells received ultrasound irradiation (0.5
W/cm2, 1 MHz) for 30 sec. Cells were treated with PBS,
DOC or DLLD for 48 h at 37°C.
Cell viability assay
BGC-823 cells were seeded on a 96-well plate
at a density of 3×103 per well and cultured for 24, 48
and 72 h, respectively. A Cell Counting Kit 8 (CCK8;
MedChemExpress) was used for cell viability detection. Briefly,
cells were incubated with CCK8 (10 µl/well) for 3 h at 37°C.
Optical density (OD) was read at 450 nm using a microplate reader.
Cell inhibition was calculated according to the formula
1-ODexpremental group/ODcontrol group.
BrdU incorporation assay
A BrdU cell proliferation ELISA kit (Abcam,
Cambridge, MA, USA) was used to quantify cells in DNA synthesis.
Briefly, cells were incubated with fresh medium containing BrdU
solution for 12 h at 37°C. After removing the medium and being
washed in PBS for 5 min at room temperature (RT), cells were fixed
in 4% paraformaldehyde solution for 10 min at RT and incubated with
primary BrdU antibody for 1 h at RT. Cells were subsequently
incubated with the secondary antibody for 30 min at RT. Following
incubation of cells with TMD and stop solution, the absorbance was
determined at 450 nm using a microplate reader (Thermo Fisher
Scientific, Inc., USA).
Flow cytometric analysis
Cells in the different experimental groups were
digested using 0.25% trypsin and homogenized by pipetting. For cell
cycle analysis, cells were centrifuged at 1,000 × g for 5 min at RT
and re-suspended in 70% cold ethanol and stored at 4°C overnight.
The ethanol was removed by centrifugation (1,000 × g for 5 min at
RT) and cells were washed in PBS for 5 min at RT. Cells were then
incubated with propidium iodide (PI; Thermo Fisher Scientific, Inc,
USA) for 30 min at 4°C in the dark. Immediately following this
incubation, the samples were detected using a flow cytometer
(Becton-Dickinson, Heidelberg, Germany). The data were analyzed by
FlowJo 7.6 software (Stanford University, California, USA).
For cell apoptosis detection, an Annexin V-FITC
Apoptosis Detection kit (Vazyme Biotech, Co., Ltd., Nanjing, China)
was used. Following staining with Annexin V and PI for 15 min in
the dark, samples were immediately detected using a flow cytometer
(Becton, Dickinson and Company). The data were analyzed using
FlowJo 7.6.1 software (FlowJo LLC).
For mitochondrial membrane potential (MMP)
detection, a JC-1 MMP detection kit (Beyotime Institute of
Biotechnology, Haimen, China) was used. Cells treated with carbonyl
cyanide 3-chlorophenylhydrazone were set as the positive control.
Cells were incubated with JC-1 (5 mg/l) for 1 h at 37°C. The
unbound JC-1 was removed by washing in PBS. Samples were
immediately detected using a flow cytometer (Becton, Dickinson and
Company). The data were analyzed by Flow Jo 7.6 software (Stanford
University, California, USA). When the MMP is high, JC-1 aggregates
to form a polymeric compound (red fluorescence) in the matrix of
mitochondria. On the contrary, JC-1 cannot aggregate and exists as
a JC-1 monomer (green fluorescence) (29). Therefore, the MMP was calculated as
the ratio of red fluorescence intensity to green fluorescence
intensity.
Western blot analysis
BGC-823 cells were harvested and lysed in
RIPA solution (Beyotime Institute of Biotechnology) containing
phenylmethanesulfonyl fluoride (PMSF) and phosphatase inhibitor.
Following centrifugation (13,000 × g for 15 min at 4°C), the
supernatant was collected. The protein content for each sample was
determined using the bicinchoninic acid assay method. The protein
(25 µg/lane) was separated by sodium dodecyl sulfate polyacrylamide
gel electrophoresis using a 10% gel. The fractioned proteins in the
gel were transferred onto a PVDF membrane. Following immersion in
5% milk/PBST for 1 h at RT, the membrane was incubated with the
primary antibodies, including p53 (dilution 1:500; cat. no. ab26),
p21 (dilution 1:1,000; cat. no. ab109520), Bcl-2 (dilution 1:1,000;
cat. no. ab32124) and Bax (dilution 1:1,000; cat. no. ab32503; all
Abcam) at 4°C overnight. The unbound primary antibodies in the
membranes were removed by washing in PBS for 15 min at RT. The
membranes were then incubated with the corresponding HRP-conjugated
goat anti-rabbit (dilution 1:3,000; cat. no. ab6721) and goat anti
mouse (dilution 1:3,000; cat. no. ab205719; all from Abcam)
secondary antibodies at room temperature for 1 h. Protein bands in
the membrane were visualized following staining with enhanced
chemiluminescence solution.
Statistical analysis
Data are expressed as the mean ± SD. One-way ANOVA
was used for statistics among groups. When ANOVA was significant,
it was followed by a post-hoc Fishers least significant difference
test. P<0.05 was considered to indicate a statistically
significant difference. The SPSS 19.0 software package was used to
perform statistical analyses (IBM Corp.).
Results
Effect of DLLD combined with UTMD on
BGC-823 cell growth
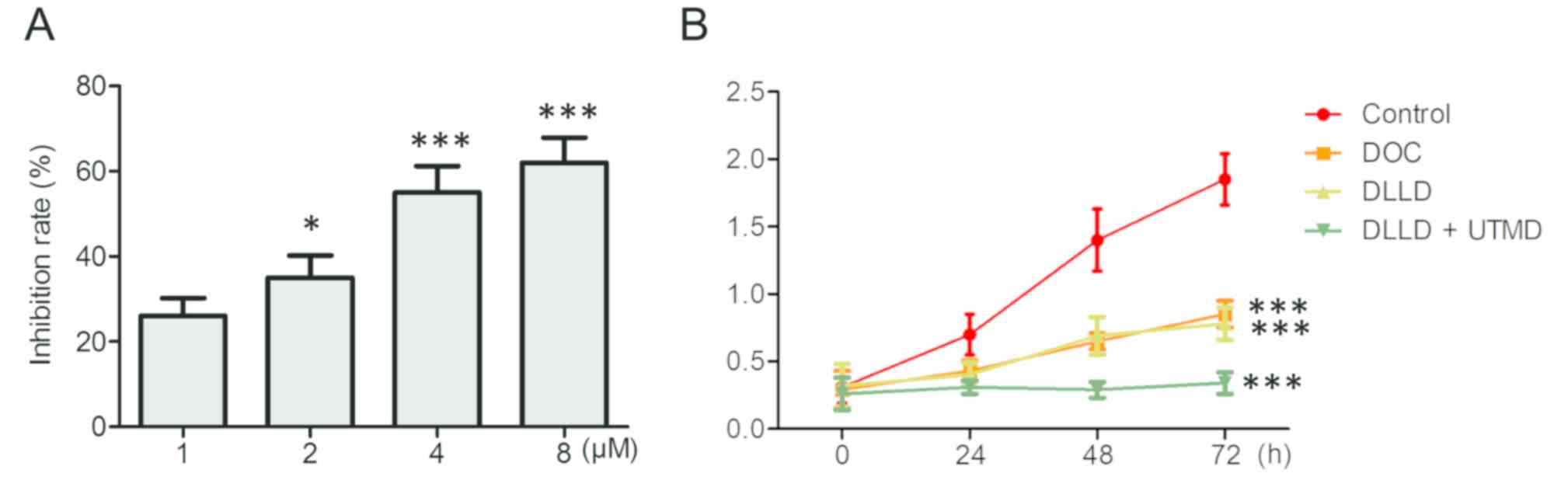
To identify an optimal inhibitory dose of DOC on the
growth of BGC-823 cells, BGC-823 cells were treated with serial
concentrations of DOC (1, 2, 4 and 8 µM) for 48 h. The results
demonstrated that DOC significantly inhibited the growth of BGC-823
in a dose-dependent manner, and the optimum inhibition was observed
at a dose of 4 µM (Fig. 1A). As a
result, 4 µM DOC was subsequently used in the present study.
Cells were treated with vehicle, DOC, DLLD
(capsulation efficiency, 76±3.5%) and DLLD plus UTMD for 0, 24, 48
and 72 h respectively. The results demonstrated that treatment with
DLLD plus UTMD significantly inhibited the growth of BGC-823 cells
compared with DOC or DLLD treatment alone (Fig. 1B). The inhibitory effect of DOC and
DLLD alone were similar (Fig.
1B).
Effect of DLLD combined with UTMD on
BGC-823 cell cycle
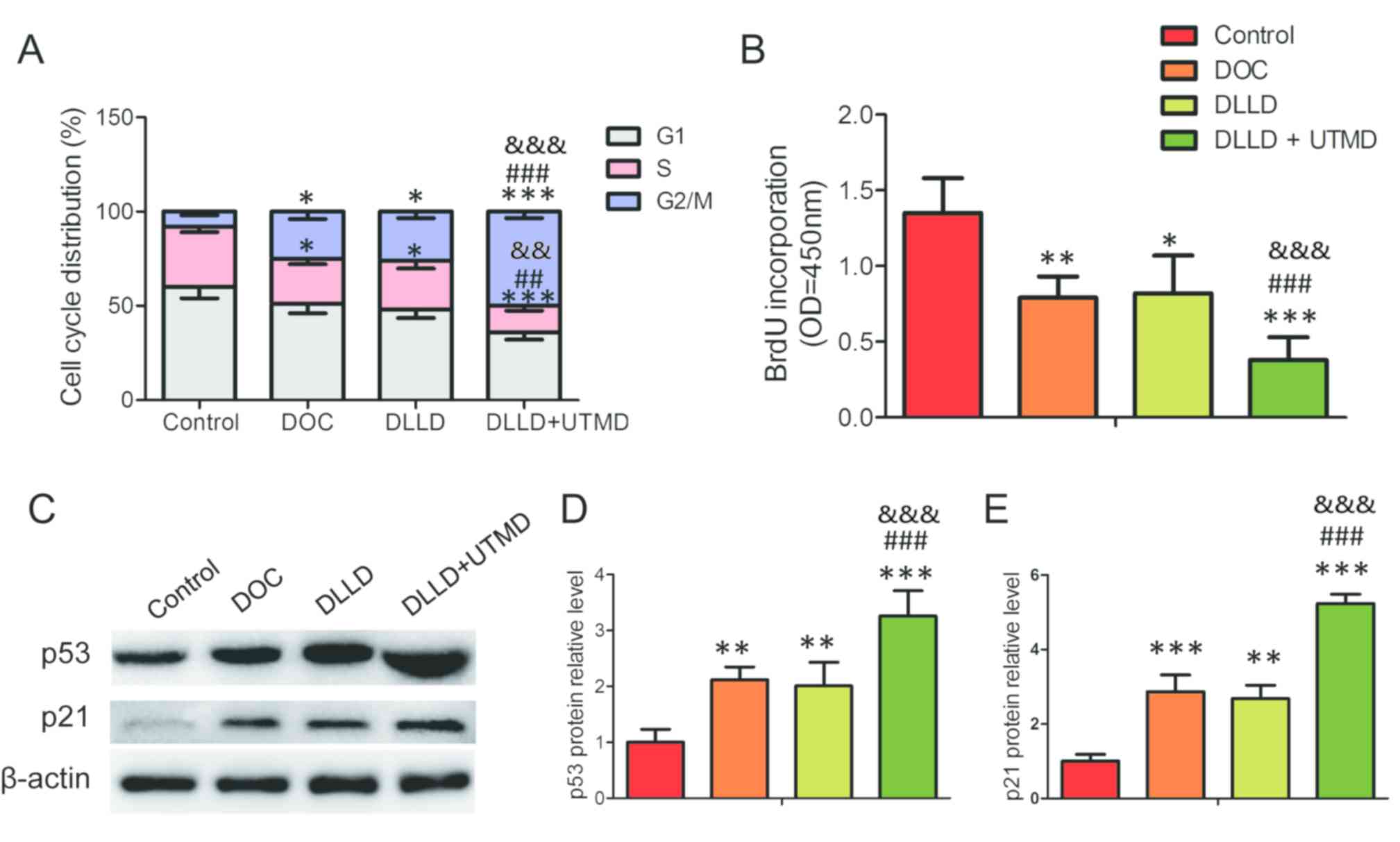
Cell cycle analysis revealed that DOC, DLLD and DLLD
plus UTMD could significantly decrease the proportion of cells in
the S phase and increase it in the G2/M phase when
compared with the control (Fig. 2A).
However, treatment with DLLD plus UTMD could further decrease the
proportion of cells in the S phase and increase it in the
G2/M phase when compared with treatment with DOC or DLLD
alone (Fig. 2A). No significant
differences were observed between the DOC and DLLD groups (Fig. 2A). This result was further confirmed
by analysis of BrdU incorporation and the expression of cell
cycle-regulating proteins. Among the four groups, BrdU
incorporative cells were the lowest and the expression of p53 and
p21 the highest in the DLLD plus UTMD group (Fig. 2B-E).
Effect of DLLD combined with UTMD on
BGC-823 cell apoptosis
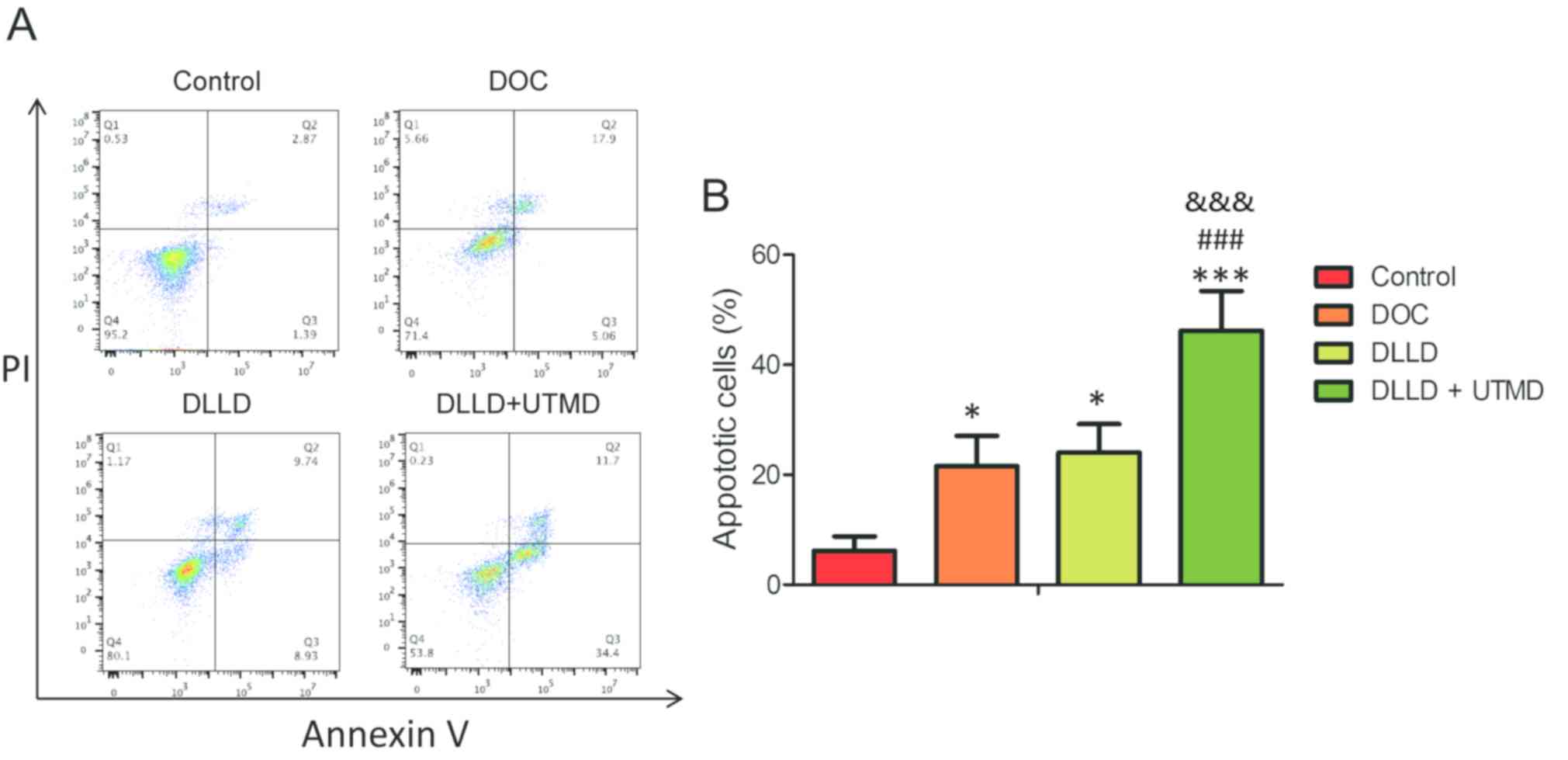
The cell apoptosis assay revealed that DOC, DLLD and
DLLD plus UTMD could significantly induce apoptosis in BGC-823
cells when compared with the control (Fig. 3A and B). However, treatment with DLLD
plus UTMD could further promote cell apoptosis when compared with
treatment with DOC or DLLD alone (Fig.
3A and B). The levels of cell apoptosis in the DOC and DLLD
treatment groups were similar (Fig. 3A
and B).
Effect of DLLD combined with UTMD on
the MMP of BGC-823 cells
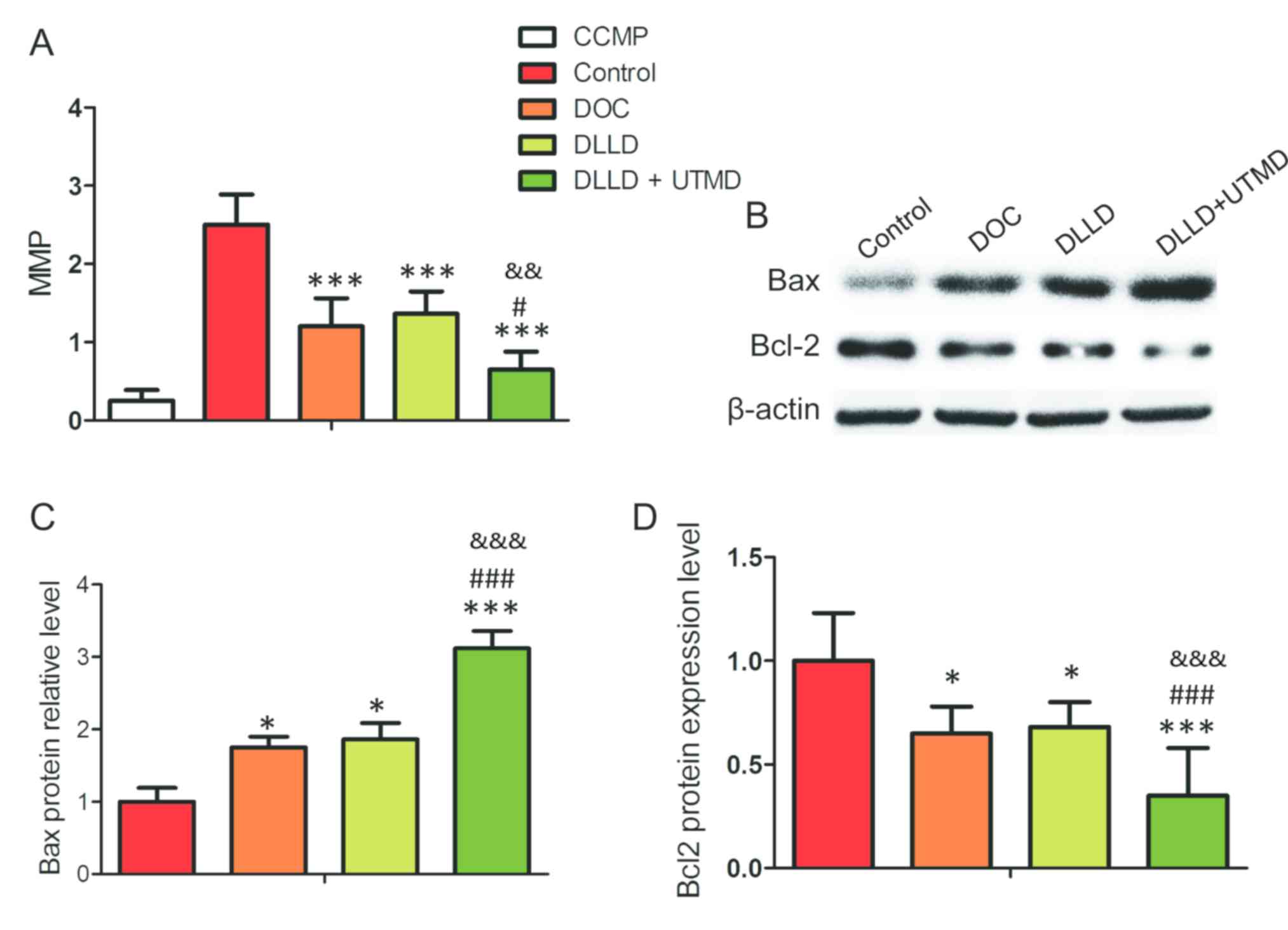
The results of MMP analysis revealed that treatment
with DLLD plus UTMD significantly decreased the MMP level of
BGC-823 cells when compared with treatment with DOC or DLLD alone
(Fig. 4A). It was also demonstrated
that the expression of Bcl-2 was lowest and the expression of Bax
highest in the DLLD plus UTMD group (Fig. 4B-D).
Discussion
DOC can bind and stabilize intracellular
microbubbles, thus disrupting the dynamic balance of microtubule
assembly and disassembly, resulting in cell death (30). Due to this property, DOC has been
widely used for the treatment of several types of cancer, including
gastric cancer (31). However, as a
cell cycle inhibitor, DOC is toxic to normal cells, which can
result in numerous side effects, including hair loss, neutropenia
and anemia (32). Therefore, more
tumor-targeting strategies need to be developed. Due to its ability
to deliver drugs to the target area, while minimizing dose and
toxicity, DLLD combined with UTMD has attracted attention in the
field of solid tumor treatment (33–37). In
the present study, the effect of DLLD in combination with UTMD on
the growth of a cultured gastric cancer cell line, BGC-823, was
investigated. The results demonstrated that combination treatment
with DLLD and UTMD exhibited the maximum inhibitory effect on tumor
cell growth, primarily by arresting the cell cycle in the
G2/M phase, inhibiting cell DNA synthesis, promoting
cell apoptosis and disrupting MMP, when compared with treatment
with DOC or DLLD alone.
A previous study by Kang et al (35) reported that DLLD combined with UTMD
could effectively inhibit the growth of VX2 rabbit liver tumors by
deferring proliferation and promoting apoptosis. Studies
investigating the effect of DLLD combined with UTMD on the growth
of other tumors, such as H22 HCC or MHCC-H hepatocellular carcinoma
xenografts and prostate carcinoma xenografts, have also
demonstrated that DLLD combined with UTMD was the most effective
strategy for the inhibition of tumor cell proliferation and the
promotion of apoptosis (28,38,39).
Consistent with the aforementioned results, the results of the
present study indicated that DLLD combined with UTMD could
significantly inhibit DNA synthesis, promote cell accumulation in
the G2/M phase and stimulate cell apoptosis.
The underlying molecular mechanism of DOC-induced
cell cycle arrest and apoptosis may be associated with the high
expression of p53, a well-characterized molecule that mediates cell
cycle arrest and cell apoptosis (40). An increasing amount of evidence has
suggested that p53 serves a critical role in sensitizing tumor
cells to DOC. A previous study demonstrated that activating p53
sensitized colorectal cancer to treatment with DOC (41). Another study demonstrated that the
p53 pathway was responsible for mediating tumor cell cycle arrest
and cell apoptosis in response to combination treatment with DOC
and resveratrol (42). In addition,
a recent clinical study demonstrated that the nanocomplex carrying
the p53 gene in combination with DOC could significantly block
solid tumor development (43). The
present study identified that DLLD combined with UTMD induced the
highest expression level of p53 and its downstream effector, p21,
in the BGC-823 cell line. Therefore, it was concluded that the
tumor-destroying effect of DLLD combined with UTMD was at least
partly mediated by promoting the expression of p53.
It has previously been reported that ultrasound
combined with microbubbles induces cavitation, resulting in
mitochondrial damage and subsequently mitochondria-dependent cell
apoptosis (44,45). Cavitation is associated with inducing
the opening of the mitochondrial permeability transition pore
(44). The present study found that
DLLD combined with UTMD could significantly lower MMP levels of
BGC-823 cells. Furthermore, the expression of Bcl-2 (anti-apoptotic
factor) was significantly inhibited and Bax (which is pro-apoptotic
factor) was significantly promoted, following combination treatment
with DLLD and UTMD. Bcl-2 and Bax are mitochondrial membrane
proteins, and the ratio of Bcl-2 to Bax determines whether cells
undergo apoptosis (46). A previous
study using DOC-loaded human serum albumin nanoparticles for the
treatment of breast cancer cells observed that the nanoparticles
could significantly increase the expression of Bax, thereby
elevating the ratio of Bax to Bcl-2, leading to cell apoptosis
(47). A different study has also
demonstrated that taxotere could abrogate the pro-apoptotic
function of Bcl-2 (48). Therefore,
we speculate that the cavitation-induced instability of the
mitochondrial membrane by UTMD may be further enhanced by DOC,
resulting in strong cell apoptosis.
In conclusion, the results of the present study
demonstrated that combination treatment with DLLD and UTMD could
more effectively inhibit the growth of a gastric cell line, through
cell cycle arrest, promotion of apoptosis and disruption of MMP,
when compared with treatment with DOC or DLLD alone. To the best of
our knowledge, this is the first study that focused on
investigating the effect of combination treatment with DLLD and
UTMD on the growth of a gastric cancer cell line. The findings
suggested that DLLD plus UTMD could be a promising novel strategy
for the treatment of gastric cancer.
Acknowledgements
Not applicable.
Funding
This project was supported by the Key Research and
Development Plan from the Jiangxi Provincial Science and Technology
Department (grant no. 20171BBG70062).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JWW conceived and designed this study. BL, PZ, HLL
and LH performed all of the experiments and data analysis. BL and
PZ wrote the manuscript. JWW reviewed the manuscript. All the
authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Torre LA, Siegel RL, Ward EM and Jemal A:
Global cancer incidence and mortality rates and trends-an update.
Cancer Epidemiol Biomarkers Prev. 25:16–27. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dadashzadeh K, Peppelenbosch MP and Adamu
AI: Helicobacter pylori pathogenicity factors related to
gastric cancer. Can J Gastroenterol Hepatol. 2017:79424892017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Buckland G, Travier N, Huerta JM,
Bueno-de-Mesquita HB, Siersema PD, Skeie G, Weiderpass E, Engeset
D, Ericson U, Ohlsson B, et al: Healthy lifestyle index and risk of
gastric adenocarcinoma in the EPIC cohort study. Int J Cancer.
137:598–606. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Laszewicz W, Iwanczak F and Iwanczak B;
Task Force of the Polish Society of Gastroenterology, : Task Force
of the Polish Society of Gastroenterology: Seroprevalence of
Helicobacter pylori infection in Polish children and adults
depending on socioeconomic status and living conditions. Adv Med
Sci. 59:147–150. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ko KP, Shin A, Cho S, Park SK and Yoo KY:
Environmental contributions to gastrointestinal and liver cancer in
the Asia-Pacific region. J Gastroenterol Hepatol. 33:111–120. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zylberberg HM, Sultan K and Rubin S:
Hereditary diffuse gastric cancer: One family's story. World J Clin
Cases. 6:1–5. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yamashita S, Kishino T, Takahashi T,
Shimazu T, Charvat H, Kakugawa Y, Nakajima T, Lee YC, Iida N, Maeda
M, et al: Genetic and epigenetic alterations in normal tissues have
differential impacts on cancer risk among tissues. Proc Natl Acad
Sci USA. 115:1328–1333. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen B, Wang J, Gu X, Zhang J and Feng X:
The DNMT3B −579G>T polymorphism is significantly associated with
the risk of gastric cancer but not lung cancer in chinese
population. Technol Cancer Res Treat. 16:1259–1265. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ajani JA: Evolving chemotherapy for
advanced gastric cancer. Oncologist. 3 (Suppl 10):S49–S58. 2005.
View Article : Google Scholar
|
|
11
|
Menges M and Hoehler T: Current strategies
in systemic treatment of gastric cancer and cancer of the
gastroesophageal junction. J Cancer Res Clin Oncol. 135:29–38.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tripathi PP, Arami H, Banga I, Gupta J and
Gandhi S: Cell penetrating peptides in preclinical and clinical
cancer diagnosis and therapy. Oncotarget. 9:37252–37267. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mullick Chowdhury S, Lee T and Willmann
JK: Ultrasound-guided drug delivery in cancer. Ultrasonography.
36:171–184. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li P, Zheng Y, Ran H, Tan J, Lin Y, Zhang
Q, Ren J and Wang Z: Ultrasound triggered drug release from
10-hydroxycamptothecin-loaded phospholipid microbubbles for
targeted tumor therapy in mice. J Control Release. 162:349–354.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Negishi Y, Endo-Takahashi Y and Maruyama
K: Gene delivery systems by the combination of lipid bubbles and
ultrasound. Drug Discov Ther. 10:248–255. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Elnaggar MA, Subbiah R, Han DK and Joung
YK: Lipid-based carriers for controlled delivery of nitric oxide.
Expert Opin Drug Deliv. 14:1341–1353. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Delalande A, Kotopoulis S, Postema M,
Midoux P and Pichon C: Sonoporation: Mechanistic insights and
ongoing challenges for gene transfer. Gene. 525:191–199. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hynynen K, McDannold N, Sheikov NA, Jolesz
FA and Vykhodtseva N: Local and reversible blood-brain barrier
disruption by noninvasive focused ultrasound at frequencies
suitable for trans-skull sonications. Neuroimage. 24:12–20. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mayer CR, Geis NA, Katus HA and
Bekeredjian R: Ultrasound targeted microbubble destruction for drug
and gene delivery. Expert Opin Drug Deliv. 5:1121–1138. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chen WS, Matula TJ and Crum LA: The
disappearance of ultrasound contrast bubbles: Observations of
bubble dissolution and cavitation nucleation. Ultrasound Med Biol.
28:793–803. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wu W, Cheng Y, Guo BH and Wu Q:
Pharmacokinetics of liver-targeted docetaxel liposomes modified
with 6-O-acyl-D-galactose esters in rabbits. Biomed Rep. 2:545–548.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Deng CX, Sieling F, Pan H and Cui J:
Ultrasound-induced cell membrane porosity. Ultrasound Med Biol.
30:519–526. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhou Y, Kumon RE, Cui J and Deng CX: The
size of sonoporation pores on the cell membrane. Ultrasound Med
Biol. 35:1756–1760. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mehier-Humbert S, Bettinger T, Yan F and
Guy RH: Plasma membrane poration induced by ultrasound exposure:
Implication for drug delivery. J Control Release. 104:213–222.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Uemura N, Kikuchi S, Sato Y, Ohnuma H,
Okamoto K, Miyamoto H, Hirakawa M, Sagawa T, Fujikawa K, Takahashi
Y, et al: A phase II study of modified docetaxel, cisplatin, and
S-1 (mDCS) chemotherapy for unresectable advanced gastric cancer.
Cancer Chemother Pharmacol. 80:707–713. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mitsui Y, Sato Y, Miyamoto H, Fujino Y,
Takaoka T, Miyoshi J, Kagawa M, Ohnuma H, Hirakawa M, Kubo T, et
al: Trastuzumab in combination with docetaxel/cisplatin/S-1 (DCS)
for patients with HER2-positive metastatic gastric cancer:
Feasibility and preliminary efficacy. Cancer Chemother Pharmacol.
76:375–382. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kim HS, Ryu MH, Zang DY, Ryoo BY, Yang DH,
Cho JW, Lim MS, Kim MJ, Han B, Choi DR, et al: Phase II study of
docetaxel, oxaliplatin, and S-1 therapy in patients with metastatic
gastric cancer. Gastric Cancer. 19:579–585. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhang Y, Chang R, Li M, Zhao K, Zheng H
and Zhou X: Docetaxel-loaded lipid microbubbles combined with
ultrasound-triggered microbubble destruction for targeted tumor
therapy in MHCC-H cells. Onco Targets Ther. 9:4763–4771. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chazotte B: Labeling mitochondria with
JC-1. Cold Spring Harb Protoc 2011. pii:pdb.prot065490. 2011.
|
|
30
|
Tangutur AD, Kumar D, Krishna KV and
Kantevari S: Microtubule targeting agents as cancer
chemotherapeutics: An overview of molecular hybrids as stabilizing
and destabilizing agents. Curr Top Med Chem. 17:2523–2537. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Farha NG and Kasi A: Docetaxel. StatPearls
[Internet]. StatPearls Publishing; Treasure Island, FL: 2019
|
|
32
|
Lyseng-Williamson KA and Fenton C:
Docetaxel: A review of its use in metastatic breast cancer. Drugs.
65:2513–2531. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Haag P, Frauscher F, Gradl J, Seitz A,
Schäfer G, Lindner JR, Klibanov AL, Bartsch G, Klocker H and Eder
IE: Microbubble-enhanced ultrasound to deliver an antisense
oligodeoxynucleotide targeting the human androgen receptor into
prostate tumours. J Steroid Biochem Mol Biol. 102:103–113. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Xing W, Gang WZ, Yong Z, Yi ZY, Shan XC
and Tao RH: Treatment of xenografted ovarian carcinoma using
paclitaxel-loaded ultrasound microbubbles. Acad Radiol.
15:1574–1579. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kang J, Wu X, Wang Z, Ran H, Xu C, Wu J,
Wang Z and Zhang Y: Antitumor effect of docetaxel-loaded lipid
microbubbles combined with ultrasound-targeted microbubble
activation on VX2 rabbit liver tumors. J Ultrasound Med. 29:61–70.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Grainger SJ, Serna JV, Sunny S, Zhou Y,
Deng CX and El-Sayed ME: Pulsed ultrasound enhances nanoparticle
penetration into breast cancer spheroids. Mol Pharm. 7:2006–2019.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Shi F, Yang F, He X, Zhang Y, Wu S, Li M,
Zhang Y, Di W, Dou J and Gu N: Inhibitory effect of
epirubicin-loaded lipid microbubbles with conjugated anti-ABCG2
antibody combined with therapeutic ultrasound on multiple myeloma
cancer stem cells. J Drug Target. 24:34–46. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ren ST, Shen S, He XY, Liao YR, Sun PF,
Wang B, Zhao WB, Han SP, Wang YL and Tian T: The effect of
docetaxel-loaded micro-bubbles combined with low-frequency
ultrasound in H22 hepatocellular carcinoma-bearing mice. Ultrasound
Med Biol. 42:549–560. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Yang Y, Bai W, Chen Y, Nan S, Lin Y, Ying
T and Hu B: Low-frequency ultrasound-mediated microvessel
disruption combined with docetaxel to treat prostate carcinoma
xenografts in nude mice: A novel type of chemoembolization. Oncol
Lett. 12:1011–1018. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kim JH, Yoon EK, Chung HJ, Park SY, Hong
KM, Lee CH, Lee YS, Choi K, Yang Y, Kim K and Kim IH: p53
acetylation enhances Taxol-induced apoptosis in human cancer cells.
Apoptosis. 18:110–120. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Guo J, Yang Y, Linghu E, Zhan Q, Brock MV,
Herman JG, Zhang B and Guo M: RASSF10 suppresses colorectal cancer
growth by activating P53 signaling and sensitizes colorectal cancer
cell to docetaxel. Oncotarget. 6:4202–4213. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Singh SK, Banerjee S, Acosta EP, Lillard
JW and Singh R: Resveratrol induces cell cycle arrest and apoptosis
with docetaxel in prostate cancer cells via a p53/ p21WAF1/CIP1 and
p27KIP1 pathway. Oncotarget. 8:17216–17228. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Pirollo KF, Nemunaitis J, Leung PK, Nunan
R, Adams J and Chang EH: Safety and efficacy in advanced solid
tumors of a targeted nanocomplex carrying the p53 gene used in
combination with docetaxel: A phase 1B study. Mol Ther.
24:1697–1706. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Zhao L, Feng Y, Shi A, Zong Y and Wan M:
Apoptosis induced by microbubble-assisted acoustic cavitation in
K562 cells: The predominant role of the cyclosporin a-dependent
mitochondrial permeability transition pore. Ultrasound Med Biol.
41:2755–2764. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Yang SL, Tang KQ, Bai WK, Zhao YW, Shen E,
Tao JJ and Hu B: Combined low-frequency ultrasound and microbubble
contrast agent for the treatment of benign prostatic hyperplasia. J
Endourol. 27:1020–1026. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Maes ME, Schlamp CL and Nickells RW: BAX
to basics: How the BCL2 gene family controls the death of retinal
ganglion cells. Prog Retin Eye Res. 57:1–25. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kordezangeneh M, Irani S, Mirfakhraie R,
Esfandyari-Manesh M, Atyabi F and Dinarvand R: Regulation of
BAX/BCL2 gene expression in breast cancer cells by docetaxel-loaded
human serum albumin nanoparticles. Med Oncol. 32:2082015.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Haldar S, Basu A and Croce CM: Bcl2 is the
guardian of microtubule integrity. Cancer Res. 57:229–233.
1997.PubMed/NCBI
|