Introduction
Current recommendations concerning the respective
roles of sun exposure and dietary intake in the supply of vitamin D
presently remain a subject of endless debate. No less than 20
studies were recently published on this issue. These deal with
items such as: the calculated UV exposure levels for a healthy
vitamin D status (1); the high
prevalence of vitamin D insufficiency (2); the vitamin D supplement doses and
serum 25-hydroxyvitamin D in the range associated with cancer
prevention (3); the knowledge and
attitudes concerning vitamin D and impact of sun protection
practices among urban office workers (4); the need for future sun protection
campaigns to address the issue of vitamin D and present strategies
to achieve sufficient vitamin D levels in countries with high UV
radiation throughout the year (5);
the attitudes, practices and knowledge of general practitioners
with regard to vitamin D in relation to prescribing sunshine
(6); the impact of public health
messages in terms of vitamin D and sun protection, as well as
protection against skin cancer (7);
the hazard of UV radiation for children and adolescents (8); the evaluation, treatment and
prevention of vitamin D deficiency considered in a clinical
practice guideline (9); the effects
of ambient sunlight and photoprotection on vitamin D status
(10); the common genetic
determinants of vitamin D insufficiency (11); an overview analysis of the time
individuals spend outdoors (12);
the effectiveness of casual exposure to summer sunlight for
maintaining adequate vitamin D status (13); the possible reduction of vitamin D
production to insufficient levels resulting from the widespread use
of sun creams, particularly those with high sun protection factors
(14); the optimal exposure to
sunlight in order to both maximise vitamin D synthesis and minimise
undesirable damages (15); and
another position statement on the risks and benefits of sun
exposure (16).
In Germany, the matter under consideration was also
far from being ignored. The following publications attest, in a far
from exhaustive manner, of such a concern. In 2008, Reinhold et
al drew attention to the measurements of circulating
25-hydroxyvitamin D concentrations in 97 German cancer patients.
The authors proposed that an abnormally low serum 25(OH)D
concentration represents a preferential risk factor, in middle-aged
females, for breast cancer, as compared with other neoplastic
manifestations in female subjects (17). A report from the Robert
Koch-Institute (Berlin, Germany) dealt with several questions
concerning vitamin D status (18).
The dietary source of vitamin D was first briefly mentioned. The
percentage of young (3–17 year-old) and older (18–79 year-old) male
and female subjects presenting a severe, moderate or mild
deficiency in vitamin D were also provided with consideration of
both seasonal and geographical (for example, subjects with a
migration background) differences. Recommendations were offered on
both the dietary uptake of vitamin D, according to gender and age,
and exposure to UV. For instance, a daily exposure to outside
sunshine of 15–20 min between spring and winter with uncovered face
and arms was recommended, with care to avoid sunburn. The potential
consequences and risks of vitamin D deficiency were also discussed.
The correlation between vitamin D status and health was the further
theme of a study published in 2008 by Hintzpeter et al
(19). Up to 81% of male subjects
and 89% of female subjects were found to have a 25(OH)D intake
below the recommended level of 5.0 μg per day. The seasonal
variation in the serum concentration of 25(OH)D was highlighted.
The female subjects aged between 65 and 79 years were considered to
have a higher risk of vitamin D deficiency. Lastly, and most
importantly, a ‘consensus article’ was recently published (20). It reflects the opinion of the
Ernährungs-kommission der Deutschen Gesellschaft für Kinder und
Jugendmedizin (DGKJ) in collaboration with the Arbeitsgemeinschaft
Pädiatrische Endokrinologie (APE). It concerns such items as the
photoproduction and metabolism of active vitamin D and its
biological function in calcium and phosphate homeostasis, as well
as in bone mass regulation. It stresses the suboptimal vitamin D
status currently prevailing in all age groups. It aims to
summarise, from available literature in national and international
publications, the reference values for vitamin D supply and
consumption. It defines recommendations for infants, children and
adolescents living in Germany in order to achieve improved vitamin
D status. These recommendations include protected sunlight
exposure, intense physical activity (at least one hour daily)
outside and increased vitamin D intake via supplements. In these
respects, special attention is given to risk groups, including
children nourished on a vegetarian diet, migrants, individuals with
limited sunlight exposure and chronically ill individuals.
Taking into account these considerations, the main
aims of the present study were to present the information recently
gained from an inquiry conducted among 448 general practitioners
(Hausärzten) and to deal with the issue of vitamin D
deficiency.
Materials and methods
The list of 10 questions submitted to general
practitioners working in different regions of Germany is given in
Table I. All results are expressed
as mean values (± SEM). The statistical significance of differences
between mean values was assessed by use of a Student’s t-test.
P<0.05 was considered to indicate a statistically significant
result.
 | Table I.List of 10 questions distributed to
general practitioners. |
Table I.
List of 10 questions distributed to
general practitioners.
| Number | Question | Answers |
|---|
| 1 | How high do you
estimate the percentage of your patients with a vitamin D
deficiency warranting treatment? | A) Light
B) Moderate
C) Severe |
| 2 | What do you advise
to your patients with a vitamin D deficiency? |
-
- Intake of vitamin D preparation
-
- Increased exposure to sunlight
-
- Exposure to artificial radiation
-
- No recommendation
|
| 3 | How much direct
sunlight exposure do you believe is adequate to restore sufficient
vitamin D synthesis? |
-
- 10 min
-
- 20 min
-
- 30 min
-
- 40 min
-
- More
|
| 4 | How do you judge in
general the recommendation of creams protecting against
sunlight? |
-
- Iudicious
-
- Unnecessary
-
- No opinion
|
| 5 | How do you judge
the recommendation of creams protecting against sunlight in your
patients with vitamin D deficiency? |
-
- Judicious
-
- Unnecessary
-
- No opinion
|
| 6 | Do you recommend to
your pateints with vitamin D deficiency the use of creams
protecting against sunlight? |
-
- No, due to the resulting blockade in vitamin D
synthesis in skin
-
- Yes, all year to prevent light and sun damage to
the skin
-
- Yes, but only in summer to prevent light and sun
damage to the skin
|
| 7 | Which measures do
you recommend during winter to your patients with vitamin D
deficiency? |
-
- Intake of vitamin D preparations
-
- Increased exposure to sunligh
-
- Whenever possible, travel to more sunny regions
to improve vitamin D status
-
- Exposure to artificial radiation
-
- No special recommendation
|
| 8 | How do you judge
the behaviour of individuals who protect themselves intensively
against UV radiation by measures such as the use of anti-light
creams or special textiles? |
|
| 9 | What would be your
opinion on a less strict protection against UV in order to improve
care of vitamin D status in the population? |
-
- Judicious
-
- Unnecessary
-
- No opinion
|
| 10 | Which of the
following do you have a greater concern for in your patients in
general? |
|
Results
Question 1
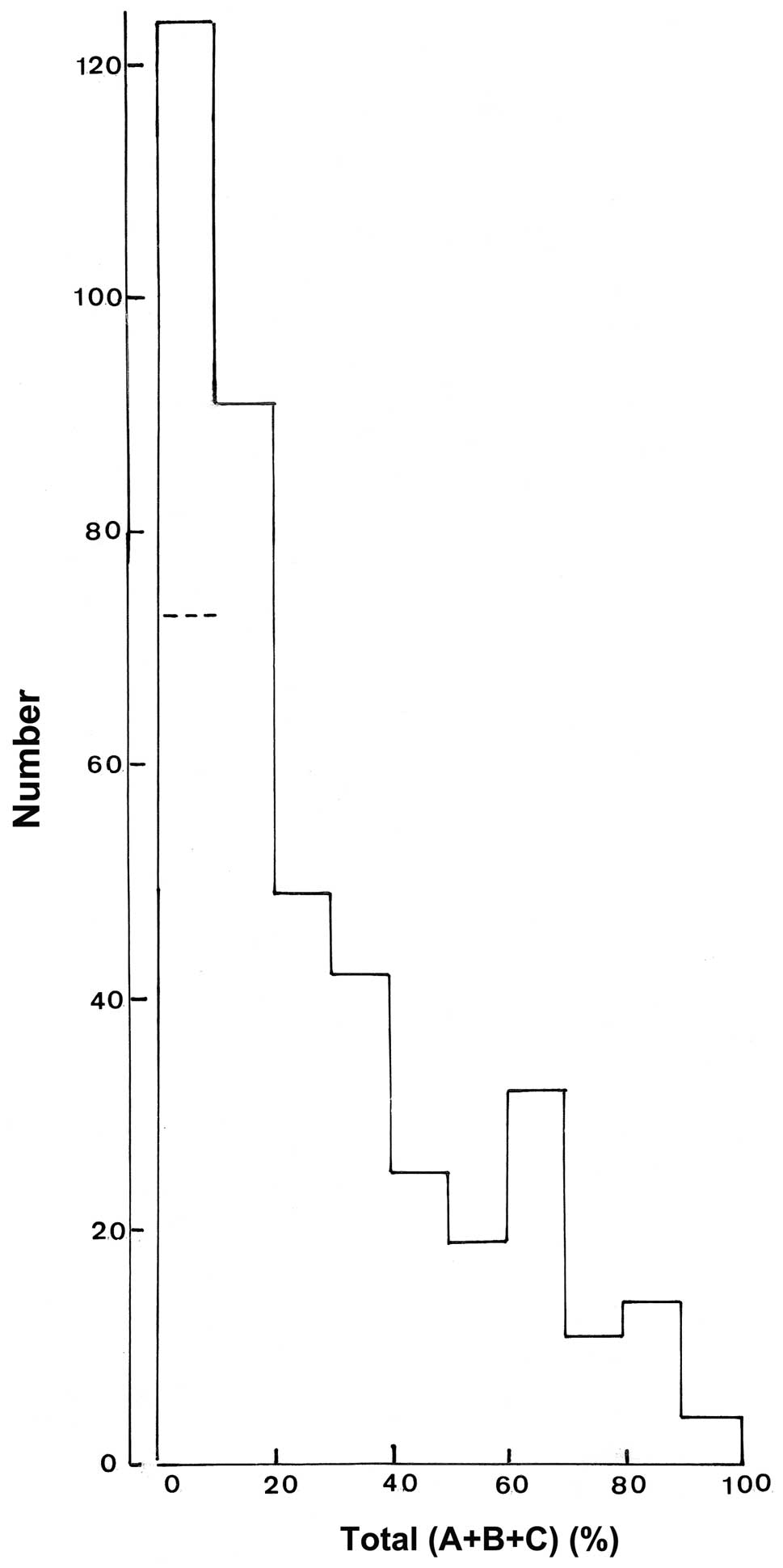
As indicated in the addendum and as based on 411
answers (Fig. 1), the consulted
physicians considered that, on average, 25±1% of their patients
suffer from a vitamin D deficiency. Based on 397 out of a total of
448 answers, such a deficiency was estimated as being light in
∼54±2% of the affected patients, whilst considered as severe in
only ∼10±1% and as intermediate in ∼37±2% of the affected patients
(Table II).
 | Table II.Relative frequency of replies A, B
and C to question 1. |
Table II.
Relative frequency of replies A, B
and C to question 1.
| Reported total %
(A+B+C) | Number of
cases | Reply A (%) | Reply B (%) | Reply C (%) |
|---|
| 100 | 32 | 48.3±5.3 | 38.4±5.1 | 13.2±2.2 |
| >100 | 5 | 55.6±5.6 | 36.5±5.4 | 7.9±2.5 |
| ≥100 | 37 | 49.3±4.7 | 38.2±4.5 | 12.5±2.0 |
| 1–95 | 360 | 54.2±2.0 | 36.5±1.9 | 9.4±0.9 |
| All | 397 | 53.7±1.9 | 36.7±1.8 | 9.7±0.8 |
Question 2
The majority of consulted physicians (94.2%) would
recommend the intake of vitamin D preparations. An increase in
exposure to sunlight was also considered as appropriate by 63.0% of
the physicians. By contrast, the exposure to artificial sources of
radiation was advised by only 1.6% of the consulted physicians,
whilst no specific recommendation was only mentioned by 2.5%. It
should be stressed that both the intake of vitamin D and increased
exposure to sunlight were mentioned by 264 out of 448 answers
(58.9%).
Question 3
In order to restore a sufficient vitamin D
production in patients with a vitamin D deficiency, the unprotected
exposure to sunlight (for example, at midday in spring and summer)
was recommended for 10 min in 19.0% of the provided answers, for 20
min in 30.5%, for 30 min in 32.6%, for 40 min in 6.3% and for
longer in 11.6% of the answers. An average of ∼26 min exposure to
sunlight emerged from these recommendations. Eight consulted
physicians made no recommendation in this respect and were,
therefore, not taken into account in the above computation.
Question 4
The majority (91.3%) of consulted physicians
considered in general, i.e. in all subjects, the use of creams
protecting against sunlight as judicious, whilst only 4.9%
considered it unnecessary. Of the consulted physicians, 3.8% did
not provide a positive or negative answer to this question.
Question 5
The use of creams protecting against sunlight by the
patients with a vitamin D deficiency was considered to make sense
by 353/448 (78.8%) of consulted physicians, whilst not being
considered so by only 12.5%. No opinion was expressed by the
remaining 8.7% of consulted physicians.
Question 6
Consistent with the answer to question 5, only 7.3%
of the consulted physicians would not advise the use of creams
protecting against sunlight in their patients with a vitamin D
deficiency as it may suppress the synthesis of vitamin D by the
skin. The other 92.6% of consulted physicians would be in favour of
the use of these creams in their patients with a vitamin D
deficiency. Approximately 30% of the latter physicians (26.9% of
all physicians) would recommend the use of such creams throughout
the year to prevent sunlight damage to the skin. However, the other
physicians also providing positive advice (65.7% of all physicians)
would restrict the use of such creams in their patients with
vitamin D deficiency to the summer period (to prevent sunlight
damage to the skin).
Question 7
Question 7 refers to the measures to be adopted
during the winter period in patients with a vitamin D deficiency.
Five approaches were listed in this question. Up to three of these
approaches were, on occasion, considered advisable. In order of
decreasing advisability, such approaches entailed: the intake of
vitamin D preparations (90.6% of positive replies); an increased
exposure to sunlight (47.0% of positive replies); whenever possible
to travel to sunny regions in order to improve the vitamin D status
(17.8% of positive replies); and the exposure to artificial
radiation (2.4% of positive replies). Only 3.8% of the consulted
physicians failed to make a recommendation in this respect.
Question 8
Question 8 concerns the consulted physicians’
opinions with regard to the behaviour of individuals who protect
themselves intensively against UV radiation, by measures such as
the use of anti-light creams or special textiles. The majority of
physicians (53.9%) considered such behaviour as worthwhile.
Nevertheless 38.1% of the physicians considered such behaviour to
be of limited value, as it could lead to a vitamin D deficiency. Of
the consulted physicians, 4.0% advised against this behaviour in
view of the increased risk of vitamin D deficiency. The remaining
4.7% of the physicians expressed no opinion on this matter.
Incidentally, out of 448 consulted physicians, four provided a dual
answer on these questions.
Question 9
The majority of physicians (68.2%) considered it
unnecessary to restrict less severely the protection against UV;
for example, by an increase in midday exposure to sunlight. Only
18.9% of the physicians provided an opposite view, whilst 12.9% did
not express any opinion on this matter.
Question 10
Lastly, 77.3% of the consulted physicians considered
skin cancer and sun damage to be a concern for their patients,
whilst only 19.4% were concerned by the morbid manifestations of
vitamin D deficiency. Both concerns were mentioned by 7.8% of the
physicians. No opinion on this matter was formulated by 11.4% of
the consulted physicians.
Discussion
The mean percentages listed in the Results in answer
to the list of 10 questions submitted to the consulted physicians
should not mask the considerable dispersion of individual answers
in some instances. This is best illustrated in Fig. 1, which depicts the far from
negligible variability in assessing the relative number of patients
presenting with a vitamin D deficiency (question 1).
With this reservation in mind, another notable
finding from the present study is the prevailing concern on skin
cancer and sun damage, as distinct from morbid manifestations of
vitamin D deficiency (question 10).
In a prevention perspective, the majority of
consulted physicians were not in favour of a less strict protection
against UV (question 9) and, on the contrary, considered the
behaviour of individuals protecting themselves intensively against
UV radiation as worthwhile (question 8). However, 54% of physicians
considered the behaviour of individuals who protect themselves
intensively against UV radiation to be worthwhile (question 8).
The recommendations for patients with a vitamin D
deficiency were mainly in terms of vitamin D intake and/or an
increased exposure to sunlight (question 2). In this respect an
average of approximately 26 min exposure to sunlight emerged from
the present inquiry (question 3). This period of sun exposure is
associated with a significantly increased risk of severe sun burn
in people with certain skin types as well as in most children
(21). This result suggests that
there is some confusion about the level of sun exposure and vitamin
D production that may result in an increased risk of skin damage
and skin cancer. During the winter period, emphasis was placed on
the intake of vitamin D and, to a lesser extent, to increased
exposure to sunlight (question 7). The exposure to artificial
sources of radiation was not found advisable, whether in patients
with vitamin D deficiency (question 2) or during the winter period
(question 7).
Lastly, the use of creams protecting against
sunlight was found to be particularly judicious whether in patients
with vitamin D deficiency (questions 5 and 6) or in all individuals
(question 4).
In conclusion, despite the fact that priority was
evidently given to the damaging consequences of uncontrolled sun
exposure, there remains the need to focus communication regarding
this issue specifically on the risk of skin cancer, whilst not
ignoring suitable recommendations to prevent or correct vitamin D
deficiency.
Acknowledgements
We are grateful to Mrs. C Demesmaeker
for secretarial assistance. We would also like to thank the
companies MSD and Meda for their support.
References
|
1.
|
AR WebbO EngelsenCalculated ultraviolet
exposure levels for a healthy vitamin D statusPhotochem
Photobiol8216971703200610.1562/2006-09-01-RA-67016958558
|
|
2.
|
IA van der MeiAL PonsobyO EngelsenJA
PascoJJ McGrathDW EylesL BlizzardT DwyerR LucasG JonesThe high
prevalence of vitamin D insufficiency across Australian populations
is only partly explained by season and latitudeEnviron Health
Perspect11511321139200717687438
|
|
3.
|
CF GarlandCB FrenchLL BaggerlyRP
HeaneyVitamin D supplement doses and serum 25-hydroxyvitamin D in
the range associated with cancer preventionAnticancer
Res31617622201121378345
|
|
4.
|
LH VuJC van der PolsDC WhitemanMG KimlinRE
NealeKnowledge and attitudes about vitamin D and impact on sun
protection practices among urban office workers in Brisbane,
AustraliaCancer Epidemiol Biomarkers
Prev1917841789201010.1158/1055-9965.EPI-10-012720570906
|
|
5.
|
M JandaM KimlinD WhitemanJ AitkenR
NealeSun protection and low levels of vitamin D: are people
concerned?Cancer Causes
Control1810151019200710.1007/s10552-007-9042-417641980
|
|
6.
|
B BoneskiA GirgisP MaginG HortonI BrozekB
ArmstrongPrescribing sunshine: a cross-sectional survey of 500
Australian general practitioners’ practices and attitudes about
vitamin DInt J Cancer13021382145201221647876
|
|
7.
|
PH YoulM JandaM KimlinVitamin D and sun
protection: the impact of mixed public health messages in
AustraliaInt J Cancer1519631970200910.1002/ijc.2415419123471
|
|
8.
|
SJ BalkCouncil on Environmental
HealthSection on Dermatology: Ultraviolet radiation: a hazard to
children and
adolescentsPediatrics127791817201110.1542/peds.2010-3502
|
|
9.
|
MF HolickNC BinkleyHA Bischoff-FerrariCM
GordonDA HanleyRP HeaneyH MuradCM WeaverEndocrine
SocietyEvaluation, treatment, and prevention of vitamin D
deficiency: an Endocrine Society clinical practice guidelineJ Clin
Endocrinol Metab9619111930201110.1210/jc.2011-038521646368
|
|
10.
|
JW DiehlMW ChiuEffects of ambient sunlight
and photoprotection on vitamin D statusDermatol
Ther234860201010.1111/j.1529-8019.2009.01290.x20136908
|
|
11.
|
TJ WangF ZhangJB RichardsB KestenbaumJB
van MeursD BerryDP KielEA StraetenC OhlssonDL KollerCommon genetic
determinants of vitamin D insufficiency: a genome-wide association
studyLancet376180188201010.1016/S0140-6736(10)60588-020541252
|
|
12.
|
BL DiffeyAn overview analysis on the time
people spend outdoorsBr J
Dermatol164848854201110.1111/j.1365-2133.2010.10165.x21128911
|
|
13.
|
BL DiffeyIs casual exposure to summer
sunlight effective at maintaining adequate vitamin D
status?Photodermatol Photoimmunol
Photomed26172176201010.1111/j.1600-0781.2010.00518.x20626818
|
|
14.
|
M NorvalHC WulfDoes chronic sunscreen use
reduce vitamin D production to insufficient levels?Br J
Dermatol161732736200910.1111/j.1365-2133.2009.09332.x19663879
|
|
15.
|
AR WebbR KiftJL BerryLE RhodesThe vitamin
D debate: translating controlled experiments into reality for human
sun exposure timesPhotochem
Photobiol87741745201110.1111/j.1751-1097.2011.00898.x21517886
|
|
16.
|
P CallisterJ GaltryR DidhamThe risks and
benefits of sun exposure: should skin colour and ethnicity be the
main variable for communicating health promotion messages in New
Zealand?Ethn
Health165771201110.1080/13557858.2010.52792521213156
|
|
17.
|
U ReinholdB SchmitzC KurbacherW NagelM
SchmidtWJ MalaisseCirculating 25-hydroxyvitamin D concentration in
German cancer patientsOncol Rep2015391543200819020739
|
|
18.
|
B HintzpeterGBM MensinkMJ MüllerC
Scheidt-NaveVitamin D status and health correlates among German
adultsEur J Clin
Nutr6210791089200810.1038/sj.ejcn.160282517538533
|
|
19.
|
B HintzpeterGBM MensinkW ThierfelderMJ
MüllerC Scheidt-NaveVitamin D status and health correlates among
German adultsEur J Clin
Nutr6210791089200810.1038/sj.ejcn.160282517538533
|
|
20.
|
M WabitschB KoletzkoA
MoßVitamin-D-Versorgung im Säuglings-, Kindes- und
JugendalterMonatsschr Kinderheilkd87667742011(In German)
|
|
21.
|
MA PathakSunscreens: topical and systemic
approaches for protection of human skin against harmful effects of
solar radiationJ Am Acad
Dermatol7285312198210.1016/S0190-9622(82)70117-36752223
|