Introduction
Teratomas are congenital tumors consisting of
derivatives from the ectoderm, endoderm and mesoderm germ cell
layers (1,2). A teratoma is considered to be a
non-seminomatous germ cell tumor and is typically located in either
the sacrococcygeal region or in the gonads. Malignant mature cystic
teratomas (0.2–2% of cases) have the potential to metastasize to
sites such as the retroperitoneal lymph nodes and lung parenchyma
(2,3). Retroperitoneal teratomas are commonly
identified in early childhood, but are rarely reported in adults
(1,2). Giant retroperitoneal teratomas in
adults are even rarer, with only a few cases previously described
in the literature. The current study presents the case of a giant
retroperitoneal teratoma in a 55-year-old female. The teratoma was
considered unresectable at the first exploratory laparotomy and was
finally treated successfully with surgical resection in the second
surgery. A review of the current clinical literature on this topic
supports our management of this case. Written informed consent was
obtained from the patient.
Case report
Clinical presentation and diagnosis
A 55-year-old female (gravida 4, para 3) was
referred to the First Affiliated Hospital (Hangzhou, China) with a
11-month history of an abdominal palpable mass and no previous
history of routine health examinations. The patient was diagnosed
with a right retroperitoneal tumor and severe hydronephrosis, and
consequently underwent an exploratory laparotomy for the purpose of
excision at Yiwu Central Hospital on August 10, 2006. The tumor was
not completely removed due to a severe hemorrhage during the
surgery. However, a small section of the tumor was resected and a
nephrostomy was performed for the hydronephrosis. The pathology
report resulted in a diagnosis of a mature retroperitoneal
teratoma. At 11 months after the first surgery, the patient was
admitted to The First Affiliated Hospital, College of Medicine,
Zhejiang University (Hangzhou, Zhejiang, China) for a whole tumor
resection.
A physical examination revealed a 25-cm mobile and
solid mass with regular contours in the abdomen. A 20-cm vertical
incision scar and a nephrostomy catheter were present on the right
upper abdomen. The catheter drained ∼200 ml clear urine/day.
Routine laboratory tests, including those for serum α-fetoprotein
(AFP), were all within normal ranges. Abdominal ultrasonography
revealed a parenchymatous irregular hypoechoic tumor in the right
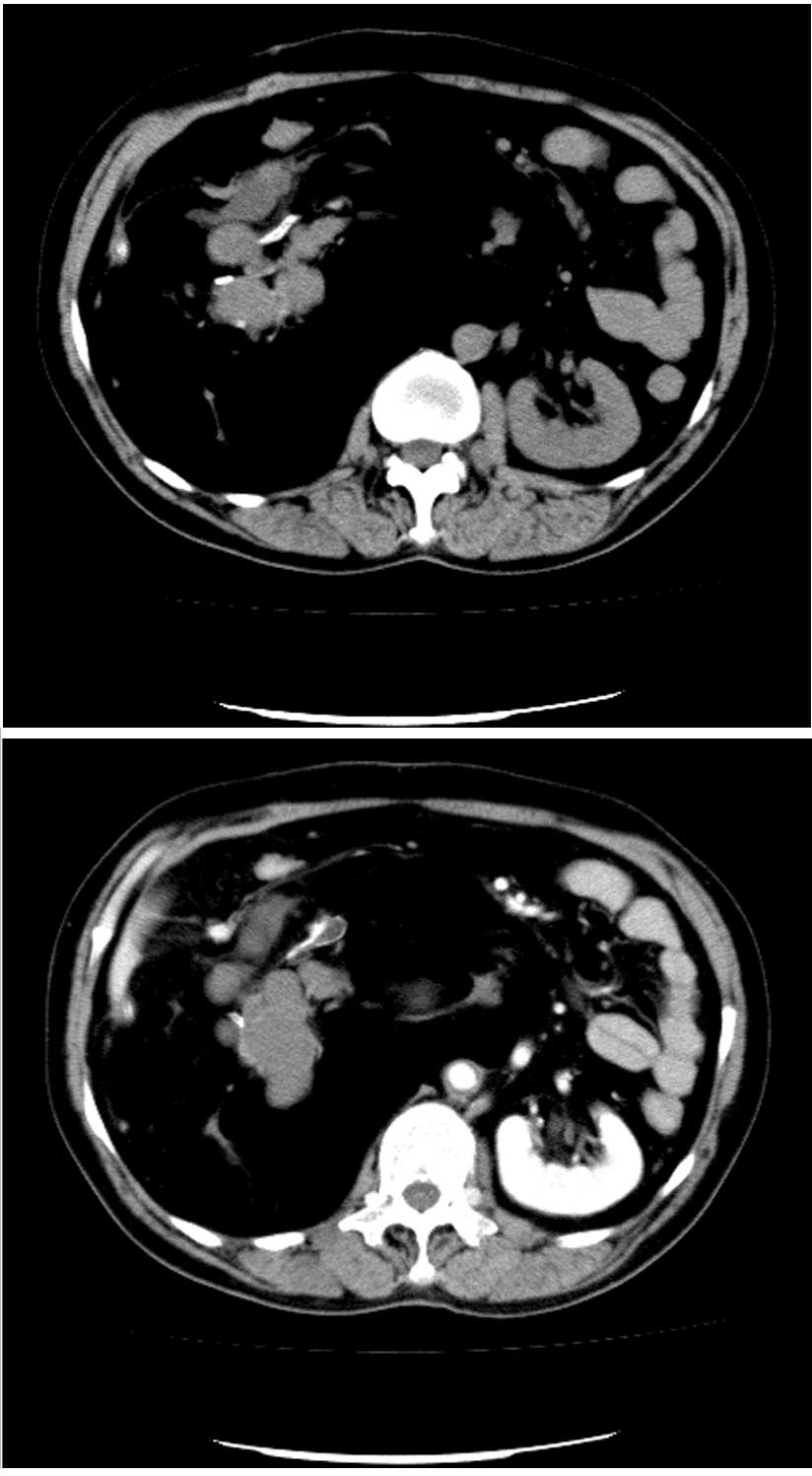
retroperitoneum. Abdominal spiral computed tomography demonstrated
a large complex mass composed of multiloculated cystic components,
soft tissue elements, inhomogeneous fatty tissue and calcifications
in the right upper retroperitoneum. The remnant right kidney was
encased by the tumor (Fig. 1).
Magnetic resonance imaging (MRI) of the pelvis revealed a large
25×18×10-cm non-enhanced cystic mass in the retroperitoneum,
distorting the abdomen severely at the level of the umbilicus and
lifting the liver vessels from behind. The abdominal aorta was
crushed to the left and the inferior vena cava was narrowed. The
ascending lumbar, azygos and hemi-azygos veins were distended and
twisted markedly (Fig. 2).
Treatment and clinical course
The patient underwent a second laparotomy for the
purpose of resection of the tumor on July 11, 2007. During the
surgical procedure, a 25-cm long subcostal incision was made and
the mass was found located in the retroperitoneal cavity, with
adhesion to the adjacent structures. The tumor was resected
successfully with a right nephrectomy. During surgery, the
diaphragmatic muscle ruptured due to the adhesion of the mass, and
thoracic closed drainage was performed. The patient had an
uneventful post-operative recovery and was well at follow-up. The
surgical specimen was a large tumor mass measuring 22×18×10 cm in
size and weighing 6 kg. The specimen contained a hydronephrotic and
distended kidney. The tumor consisted of fat, fiber and
cartilage-like tissue (Fig. 3).
Histological sections revealed mature, differentiated elements
consistent with a mature teratoma. The kidney exhibited chronic
pyelonephritis and atrophy, and pyelectasis was observed in the
majority of the renal parenchyma.
Discussion
Teratomas have been identified in individuals from
every age group, however, the peak incidence is reported at between
20 and 40 years old (3). The
majority of cases of malignant transformation are detected at 30–70
years old (4,5). Teratomas are generally divided into 2
histological types, mature and immature. A mature teratoma is an
adult-type tumor consisting of differentiated elements, while an
immature teratoma consists of elements with only partial somatic
differentiation, similar to that observed in an embryo or fetus. In
cases of retroperitoneal teratomas, ∼75% are benign and 25% are
malignant. With regard to the histological subtypes, mature
teratomas are generally benign, but may undergo malignant
transformation into non-germ cell malignancies, including sarcomas
and carcinomas (2,6). Immature teratomas have inherent
malignant potential, but which percentage of immature teratomas in
the retroperitoneum behaves in a malignant fashion is unclear.
The diagnosis of a retroperitoneal teratoma is often
made on the basis of investigative imaging (2,7,8).
Retroperitoneal teratomas are predominantly cystic or completely
solid in appearance. Ultrasonography represents an important tool
for making an early diagnosis and performing post-operative
monitoring. Computed tomography (CT) scans or MRI are used to
identify various components of these neoplasms, including
soft-tissue density structures, adipose tissue and sebaceous and
serous-type fluids. These imaging techniques are also able to
indicate the precise location, morphology and adjacent structures
of the tumor, enabling improved pre-operative planning and a more
complete removal of the tumor with less damage (7). In addition, MRI, compared with CT, is
more suitable for the determination of the association between the
teratoma and celiac great vessels and the degree of tumor
infiltration (8). AFP is produced
by malignant retroperitoneal teratomas and functions as a specific
tumor marker for laboratory diagnosis (6). Abnormal elevations in serum levels of
carcinoembryonic antigen (CEA) and carbohydrate antigen (CA)19-9
have been reported in primary retroperitoneal teratomas (9). In the present case, all tumor markers
were within the normal range.
The primary treatment of retroperitoneal teratomas
is surgical resection (6,10). The most important structures in the
abdomen are the aorta, vena cava, superior mesenteric vessels,
celiac trunk and duodenum. Damage to these structures may cause
overwhelming hemorrhaging, severe post-operative complications and
even fatalities. Imaging of the tumor is critical for developing an
effective pre-operative strategy and performing a safe surgical
excision (6,9,10). As
observed in the present patient, the benign teratoma expands and
presses against, rather than encases, the surrounding structures
and therefore may be dissected away from these adjacent structures.
As with other abdominal surgeries, pre-operative imaging and the
development of an appropriate strategy are essential for the
excision of a retroperitoneal tumor. A malignant teratoma that
invades the adjacent structures requires more extensive resection
and may include the major vessels or organs. Unresectable or
marginally resectable retroperitoneal teratomas may be shrunk
following an initial course of chemotherapy (10).
Acknowledgements
The present case study was supported
by grants from the National Natural Science Foundation of China
(no. 30772176) and the National Key Clinical Specialty Construction
Project of China.
References
|
1.
|
Luo CC, Huang CS and Chu SM:
Retroperitoneal teratomas in infancy and childhood. Pediatr Surg
Int. 21:536–540. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Gatcombe HG, Assikis V and Kooby D:
Primary retroperitoneal teratomas: a review of the literature. J
Surg Oncol. 86:107–113. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Lakkis WG, Martin MC and Gelfand MM:
Benign cystic teratoma of the ovary: A 6-year review. Can J Surg.
28:444–446. 1985.PubMed/NCBI
|
|
4.
|
Ayhan A, Bukulmez O, Genc C, Karamursel BS
and Ayhan A: Mature cystic teratomas of the ovary: Case series from
one institution over 34 years. Eur J Obstet Gynecol Reprod Biol.
88:153–157. 2000.PubMed/NCBI
|
|
5.
|
Singh P, Yordan EL, Wilbanks GD, Miller AW
and Wee A: Malignancy associated with benign cystic teratomas
(dermoid cysts) of the ovary. Singapore Med J. 29:30–34.
1988.PubMed/NCBI
|
|
6.
|
Gatcombe HG, Assikis V and Kooby D:
Primary retroperitoneal teratomas: a review of the literature. J
Surg Oncol. 86:107–113. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Yang DM, Jung DH and Kim H:
Retroperitoneal cystic masses: CT, clinical and pathologic findings
and literature review. Radiographics. 24:1353–1365. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Choi BI, Chi JG and Kim SH: Case report:
MRI of Retroperitoneal Teratoma: correlation with CT and Pathology.
J Comput Assist Tomoger. 13:1083–1086. 1989. View Article : Google Scholar
|
|
9.
|
Lin M, Ng KK, Hung CF, Tseng JH, Cheung YC
and Wan YL: Dyspnea as a clinical manifestation in primary
retroperitoneal teratoma. Zhonghua Fang She Xue Za Zhi. 26:141–145.
2001.(In Chinese).
|
|
10.
|
Leandros E, Alexakis N and Konstadoulakis
M: Postchemotherapy resection of a primary mature malignant
retroperitoneal teratoma in an adult: report of a case. Surg Today.
35:965–967. 2005. View Article : Google Scholar : PubMed/NCBI
|