Introduction
Colon cancer was the third most common type of
cancer diagnosed and the third most common cause of cancer-related
mortality in the United States in 2015 (1). Colorectal cancer was the third most
commonly diagnosed cancer in males and the second most common in
females worldwide in 2012 according to Global Cancer Statistics
(2). The five-year survival rate for
colon cancer is only 10% in patients with metastases (3), potentially due to the development of
drug resistance during therapy. Oxaliplatin (OX), a third
generation platinum-based antineoplastic agent, is a commonly used
chemotherapeutic agent for the clinical treatment of advanced colon
cancer (4). Although the clinical
application of OX has resulted in a significant improvement in
response rate and progression-free survival in advanced colon
cancer (5), ~40% of cases of colon
cancer continue to develop resistance (6). Therefore, the development of novel
therapeutic strategies is required to overcome the current OX
resistance in advanced colon cancer.
Autophagy is a dynamic cellular protective process
of cells that occurs in response to stress and an abnormal
microenvironment (7). Recently,
increasing evidence has indicated the importance of autophagy in
human cancer, with autophagy exhibiting a dual function in cancer
development. In healthy cells, autophagy acts as a tumor suppressor
by clearing damaged proteins and organelle accumulation to prevent
tumorigenesis (8). However, autophagy
in cancer cells may promote cell survival by sustaining the
cellular metabolism necessary for survival under hypoxic conditions
and drug treatment, resulting in tumor growth and therapeutic
resistance (8–10). In colon cancer, autophagy appears to
favor cancer cell survival by protecting from tumor cell death
caused by chemotherapy and radiotherapy (11–15). For
example, it has been demonstrated that autophagy is responsible for
the resistance of colon cancer cells to 5-fluorouracil (FU)
treatment, as inhibition of autophagy enhances 5-FU-induced tumor
cell apoptosis in vitro (11,12,15). In
addition, OX can activate cell autophagy via endoplasmic reticulum
(ER) stress and the reactive oxygen species (ROS) pathway in human
colon cancer cells to induce their resistance to OX treatment
(13). Although the inhibition of
autophagy can increase the sensitivity of colon cancer cells to OX
treatment in vitro, the in vivo therapeutic effects
of autophagy inhibition on tumor growth has yet to be investigated
in animal models treated with OX.
Therefore, the aim of the present study was to
observe the effect of the autophagy inhibitor 3-methyladenine
(3-MA) combined with OX on murine CT26 cell growth in vitro
and in vivo. In addition, the potential mechanism of the
combined effect induced by this combination therapy was
investigated.
Materials and methods
Cells, reagents and antibodies
The CT26 mouse colon carcinoma cell line (CRL-2638;
American Type Culture Collection, Manassas, VA, USA) was maintained
in RPMI-1640 medium (Invitrogen Life Technologies, Carlsbad, CA,
USA) supplemented with 10% heat-inactivated fetal bovine serum and
100 µg/ml kanamycin sulfate at 37°C in a 5% CO2
humidified incubator. The following reagents were used in present
study: OX (Eloxatin®; Sanofi, Paris, France), 3-MA (M9281;
Sigma-Aldrich, St. Louis, MO, USA) and ProLong® Gold antifade
reagent with 4′,6-diamidino-2-phenylindole (DAPI; Cell Signaling
Technology, Inc., Danvers, MA, USA). In addition, the antibodies
used in current study included, Beclin1 (Abcam, Cambridge, UK; cat
no. ab62557), microtubule-associated protein light chain 3 (LC3;
Abcam; cat no. ab58610), autophagy related 5 (ATG5; Abcam; cat no.
ab108327), Bcl-2-associated X protein (Bax; Abcam; cat no.
ab32503), caspase-3 (Santa Cruz Biotechnology, Inc., Dallas, TX,
USA; cat no. sc-7148) and p53 (Abcam; cat no. ab1431).
Immunofluorescence
A total of 2×104 CT26 cells were seeded
into an 8-well chamber slide and treated with phosphate-buffered
saline (PBS), OX (4 mM), 3-MA (5 nM) or OX plus 3-MA for 48 h.
Cells were then washed with PBS and fixed using 4% formaldehyde.
After washing, the cells were treated with 0.1% Triton X-100
containing 1% bovine serum albumin for 1 h at room temperature,
followed by incubation with the LC3 antibody (dilution, 1:200) for
24 h at 4°C in a humidified chamber. Cells were washed with PBS and
incubated with horseradish peroxidase (HRP)-conjugated secondary
antibody for 2 h at room temperature. After rinsing with PBS, the
cells were placed on a coverslip by ProLong® Gold antifade reagent
with DAPI and examined using an IX70 inverted fluorescence
microscope (Olympus Corporation, Tokyo, Japan).
Acridine orange (AO) and
monodansylcadaverine (MDC) staining
A total of 5×104 CT26 cells were seeded
into a 4-well chamber slide and treated with PBS, OX (4 mM), 3-MA
(5 nM) or OX plus 3-MA for 48 h. The treated cells were washed with
PBS, stained with medium containing 1 µg/ml AO (Polysciences, Inc.,
Warrington, PA, USA) or 10 mM MDC (Sigma-Aldrich) in PBS for 15
min, washed with PBS and immediately examined under a fluorescence
microscope.
Western blot analysis
Proteins were extracted from the treated CT26 cells
using RIPA buffer (50 mM Tris-base, 1.0 mM EDTA, 150 mM NaCl, 0.1%
SDS, 1% Triton X-100, 1% sodium deoxycholate and 1 mM
phenylmethylsulfonyl fluoride) and the protein concentration was
determined using a DC™ protein assay kit (Bio-Rad Laboratories,
Hercules, CA, USA). Equal amounts of the protein samples were
loaded and separated on a 12% SDS-PAGE and transferred onto
polyvinylidene difluoride membranes (GE Healthcare Life Sciences,
Chalfont, UK). After blocking with 5% non-fat milk in Tris-buffered
saline with 0.1% Tween-20 (TBST) for 1 h, the membranes were
incubated with the indicated primary antibodies overnight at 4°C.
After washing with TBST, the blots were incubated with
HRP-conjugated secondary antibody for 1 h at room temperature and
the target proteins were detected using enhanced chemiluminescence
reagents (Amersham Pharmacia Biotech, Inc., Piscataway, NJ,
USA).
Quantitative assessment of apoptosis
using flow cytometry
After trypsinization and washing with PBS,
1×106 CT26 cells were stained in 0.5 ml hypotonic
fluorochrome solution (50 mg/ml propidium iodide in 0.1% sodium
citrate containing 0.1% Triton X-100) overnight at 4°C.
Subsequently, flow cytometric analysis was performed using a flow
cytometer (EPICS Elite ESP; Beckman Coulter, Brea, CA, USA) to
assess the number of apoptotic cells with hypodiploid DNA
content.
Cell viability assays
CT26 cells were seeded at a concentration of
5×103 cells per well in a 96-well plate. After culturing
overnight, the cells were incubated with fresh medium containing
PBS, OX (4 mM), 3-MA (5 nM) or OX plus 3-MA for the indicated time
periods. The number of viable cells was then estimated using an MTT
assay by measuring absorbance at a wavelength of 570 nm using a
microplate reader (Multiskan MK3; Bio-Rad Laboratories). The data
are expressed as the mean ± standard deviation (SD) from a minimum
of three independent experiments.
In vivo tumor growth
In total, 40 female BALB/c mice (age, 6–7 weeks)
were purchased from the Animal Center at Sichuan University
(Chengdu, China). CT26 cells (5×105 cells in 100 µl PBS)
were subcutaneously injected into the BALB/c mice at the dorsal
flank. After injection, the mice were randomly separated into four
groups of 10 mice (control group; 3-MA group; OX group;3-MA plus OX
groups). Each mouse received an intraperitional (i.p.) injection of
PBS (1 ml; control and OX groups) or 3-MA (1 ml; 24 mg/kg; 3-MA and
3-MA plus OX groups) and an intravenous (i.v.) injection of PBS
(100 µl; control and 3-MA groups) or OX (100 µl; 10 mg/kg; OX and
3-MA plus OX groups). The i.p. injections were performed on days 5,
10, 15, 20 and 25 after tumor cell inoculation, and the i.v.
injections were administered on days 10 and 24 after tumor cell
inoculation. Tumor growth was monitored by measuring the tumor
diameter using a vernier caliper every two days until day 27, when
the mice were sacrificed, and the tumor volume was calculated using
the following equation: Length × width2 × 0.52 (16).
To determine the survival time of the mice, 100 mice
received a subcutaneous inoculation of CT26 cells (5×105
cells/mouse) prior to being randomly separated into four groups of
25 mice per group. The four groups received treatment with PBS, OX,
3-MA or OX plus 3-MA, as described above, and the survival times of
the mice were recorded for seven weeks after cell inoculation, at
which point the experiment was terminated. All mouse experiments
were reviewed and approved by the Animal Care and Use Committee of
the Animal Center at Sichuan University.
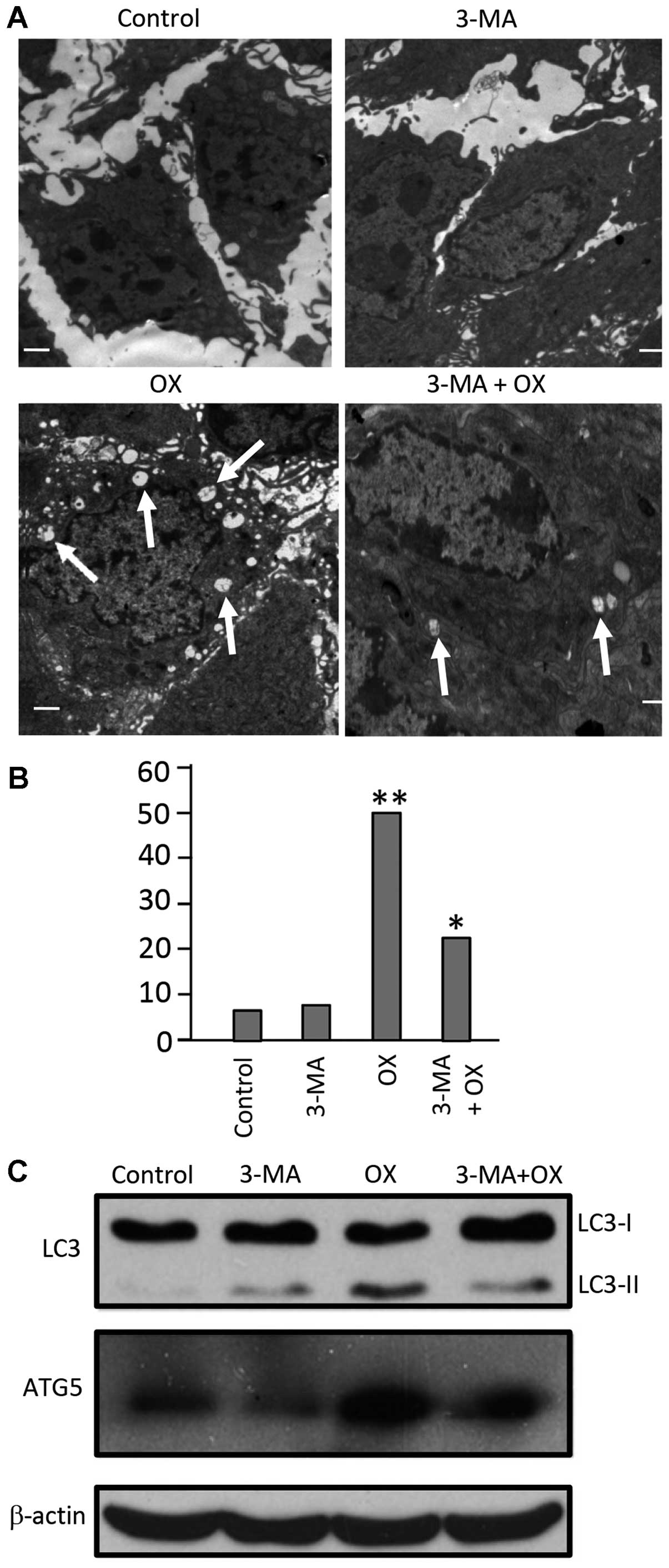
Electron microscopy
Tumor tissues were obtained from three
randomly-selected mice from each of the four groups (control, 3-MA,
OX and OX + 3-MA) (n=12) that were sacrificed on day 27 after tumor
cell inoculation. Tumor tissues were sliced into 1 mm3
sections and fixed with 2.5% glutaraldehyde in 0.1 M sodium
cacodylate buffer (SCB) for 1 h. After washing with SCB, the
tissues were incubated with 1% osmium tetroxide in 0.1 M SCB for 1
h at room temperature, followed by washing three times with SCB.
Subsequently, the tissues were dehydrated with alcohol in a graded
ethanol series and then embedded in paraffin. A Reichert EM UC7
Ultramicrotome (Leica Microsystems GmbH, Wetzlar, Germany) was used
to cut ultrathin sections of the tissue block. After
counterstaining with 0.3% lead citrate, the ultrathin sections were
examined on a Philips EM420 transmission electron microscope
(Philips, Eindhoven, The Netherlands). Autophagic cells were
defined as cells that had five or more autophagic vacuoles.
Furthermore, the areas occupied by autophagic vacuoles within the
cytoplasm were calculated using Image-Pro Plus software (version
3.0; Media Cybernetics, Inc., Silver Spring, MD, USA) and used for
indexing the cytoplasmic area occupied by autophagic vacuoles.
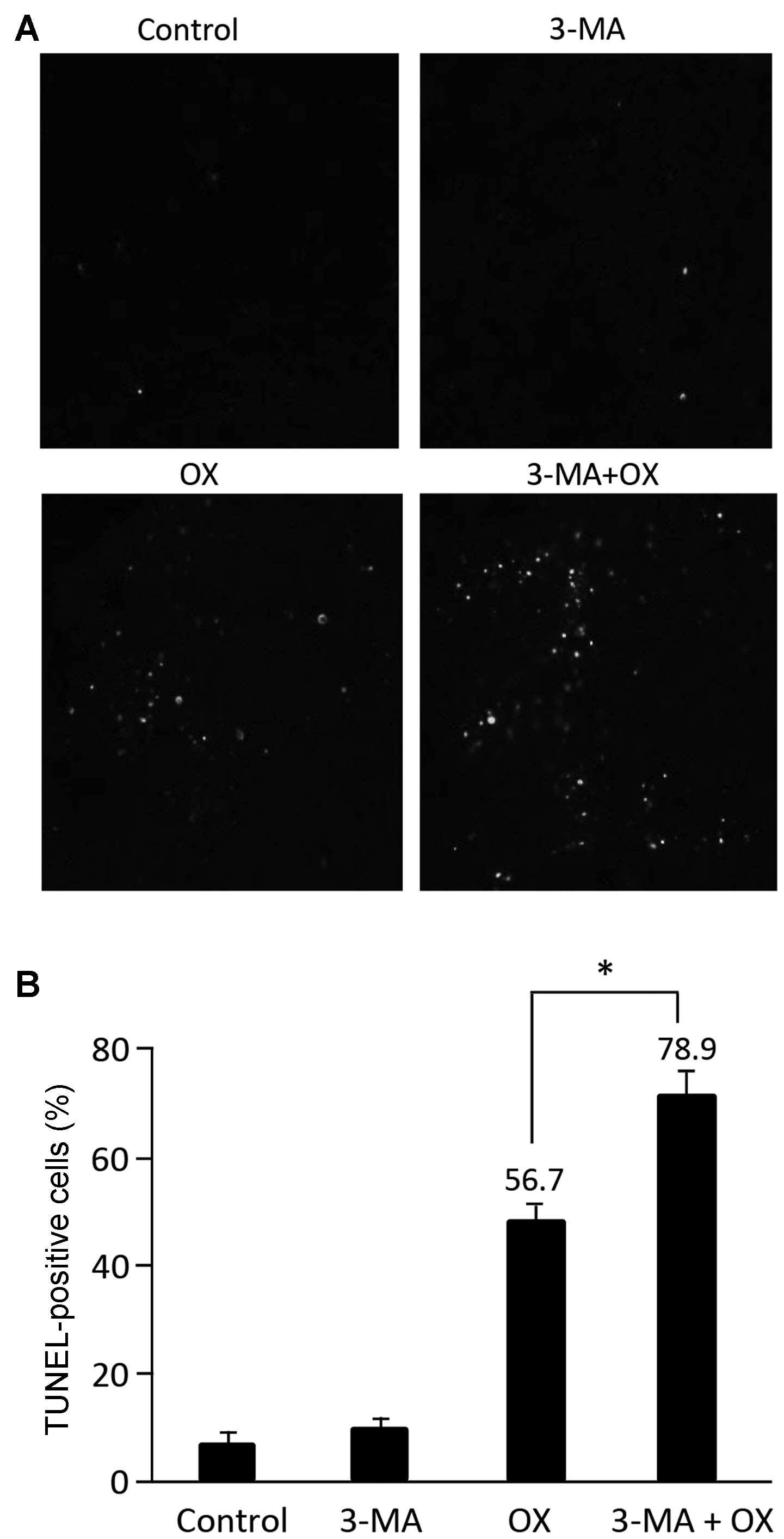
Terminal
deoxynucleotidyltransferase-mediated dUTP nick-end labeling (TUNEL)
assay
Apoptotic cells within the tumor sections were
detected by performing a TUNEL assay using the DeadEnd™
Fluorometric TUNEL system (Promega Corporation, Madison, WI, USA),
according to the manufacturer's instructions. The mean percentage
of apoptotic cells in tumor tissues was determined by counting the
number of apoptotic cells in a field and dividing this number by
the total number of cells counted in the same field, selecting five
high power fields for each slide.
Statistical analysis
All data are presented as the mean ± standard
deviation (SD) and all statistical analyses were performed using a
Student's t-test, unless stated otherwise. P<0.05 was
considered to indicate a statistically significant difference.
Results
OX treatment increases autophagy in
murine CT26 cells
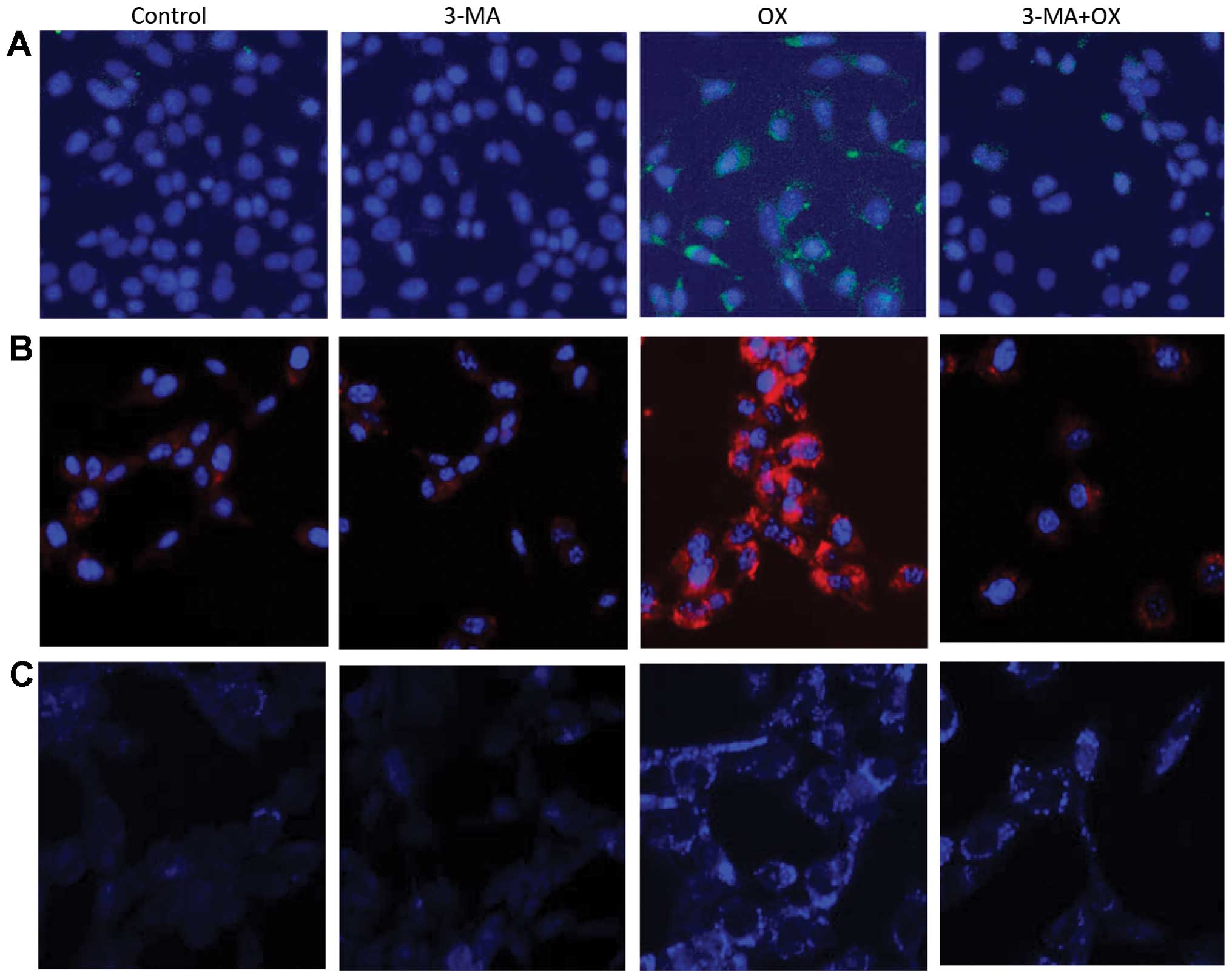
The in vitro treatment of CT26 cells with OX
markedly increased cell autophagy, as indicated by the increased
LC3 staining (green color) observed in Fig. 1A. Furthermore, the autophagy inhibitor
3-MA appeared to block this OX-induced CT26 cell autophagy.
OX-induced cell autophagy was also indicated by the increased
presence of acidic vacuoles/autophagosomes identified by AO (red
color; Fig. 1B) and MDC (blue color;
Fig. 1C) staining in the CT26 cells.
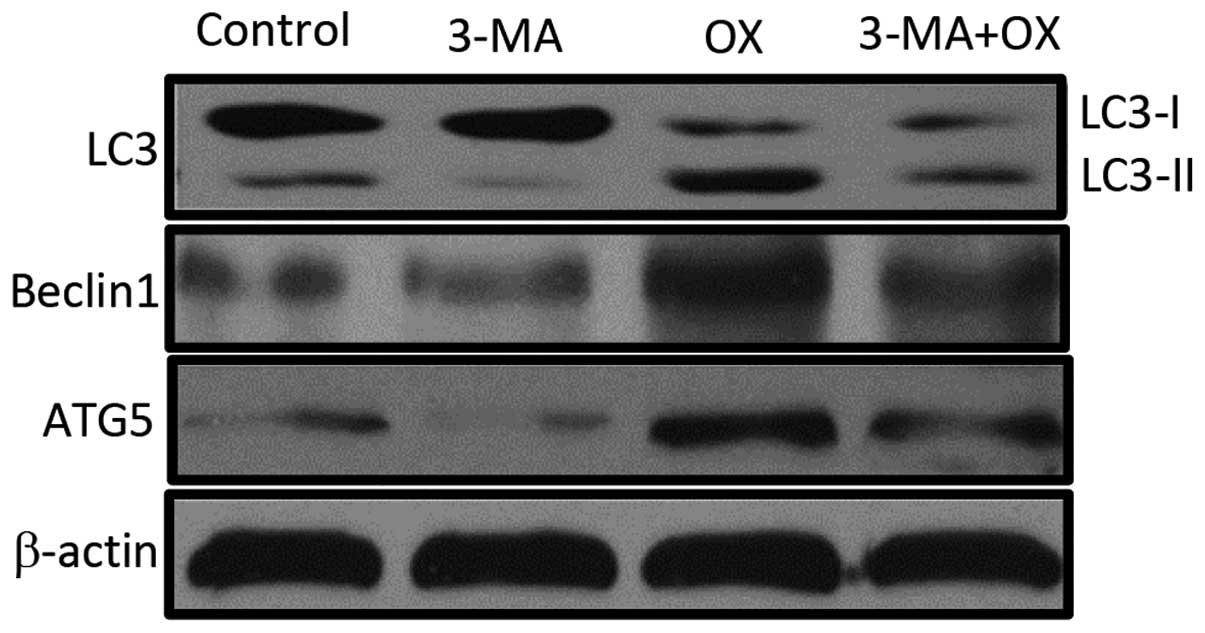
Consistently, OX-treated CT26 cells markedly increased the
expression levels of autophagy-related proteins, such as LC3-II,
Beclin1 and ATG5; however, the increase in the expression levels of
all three proteins was quenched by the administration of 3-MA in
combination with OX (Fig. 2). Taken
together, these data indicate that OX increases cell autophagy and
that the autophagic stimulation effect of OX can be blocked by the
autophagy inhibitor, 3-MA.
OX increases the apoptosis rate of
CT26 cells
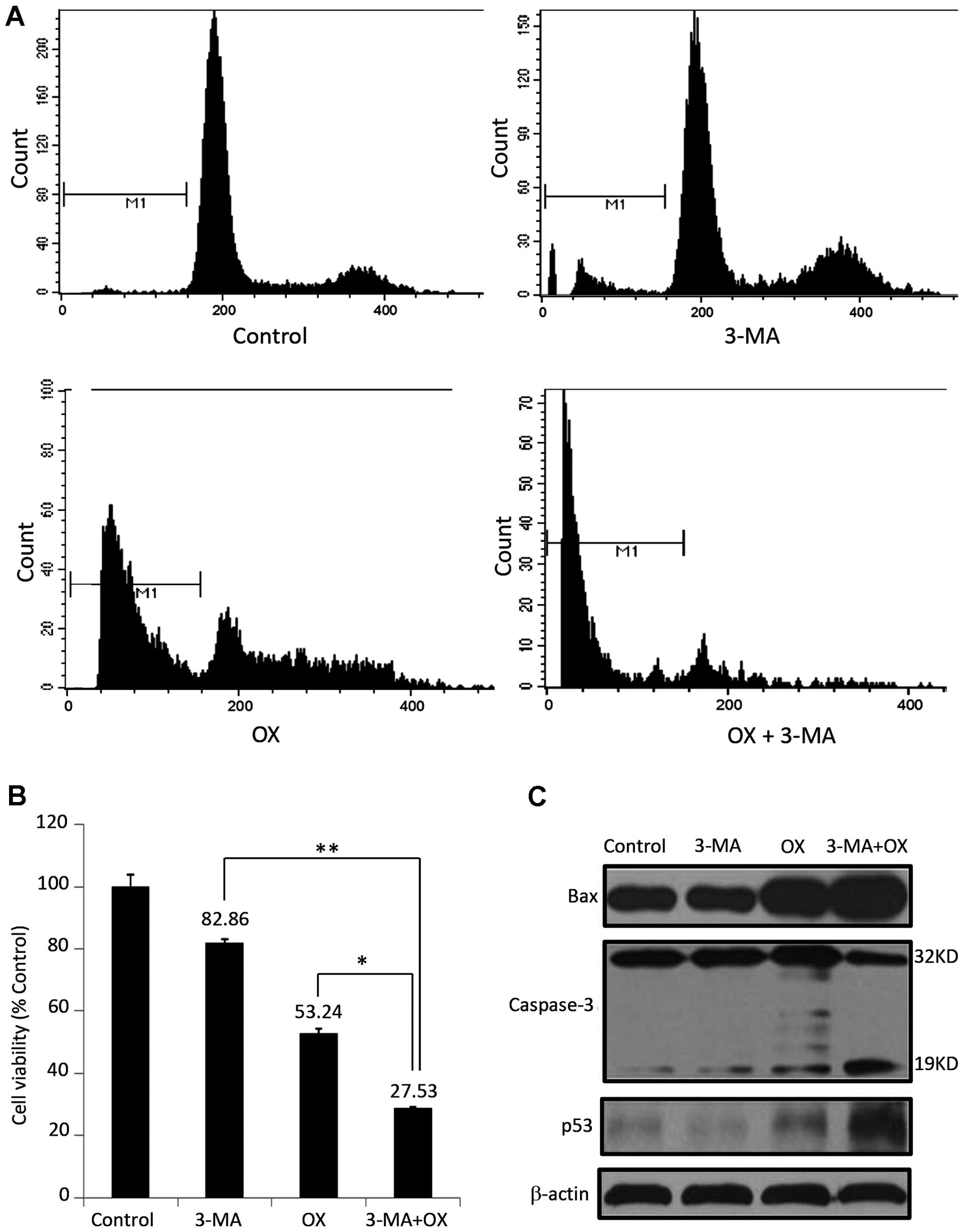
Investigation of the effects of different treatment
regimens on the apoptosis of CT26 cells demonstrated that, although
3-MA alone appears to exhibit minor effects on cell apoptosis
(10.27% of cells exhibited sub-G1 DNA content), 3-MA significantly
enhanced OX-induced apoptosis of CT26 cells when compared with OX
treatment alone (86.81 vs. 39.48% cells with sub-G1 DNA content;
P=0.0034; Fig. 3A). Consistently,
CT26 cells treated with 3-MA and OX showed the lowest cell
viability (27.5%), followed by cells treated with OX alone (53.2%)
and 3-MA alone (84.86%; Fig. 3B).
Furthermore, 3-MA administration increased the expression of a
number of apoptosis-related proteins, including Bax, p53, and
active caspase-3, which were initially induced by OX treatment
(Fig. 3C). These results indicate
that blocking the autophagic effect of OX may enhance its apoptotic
effect on colon cancer cells.
In vivo synergistic anticancer effects
of OX combined with 3-MA
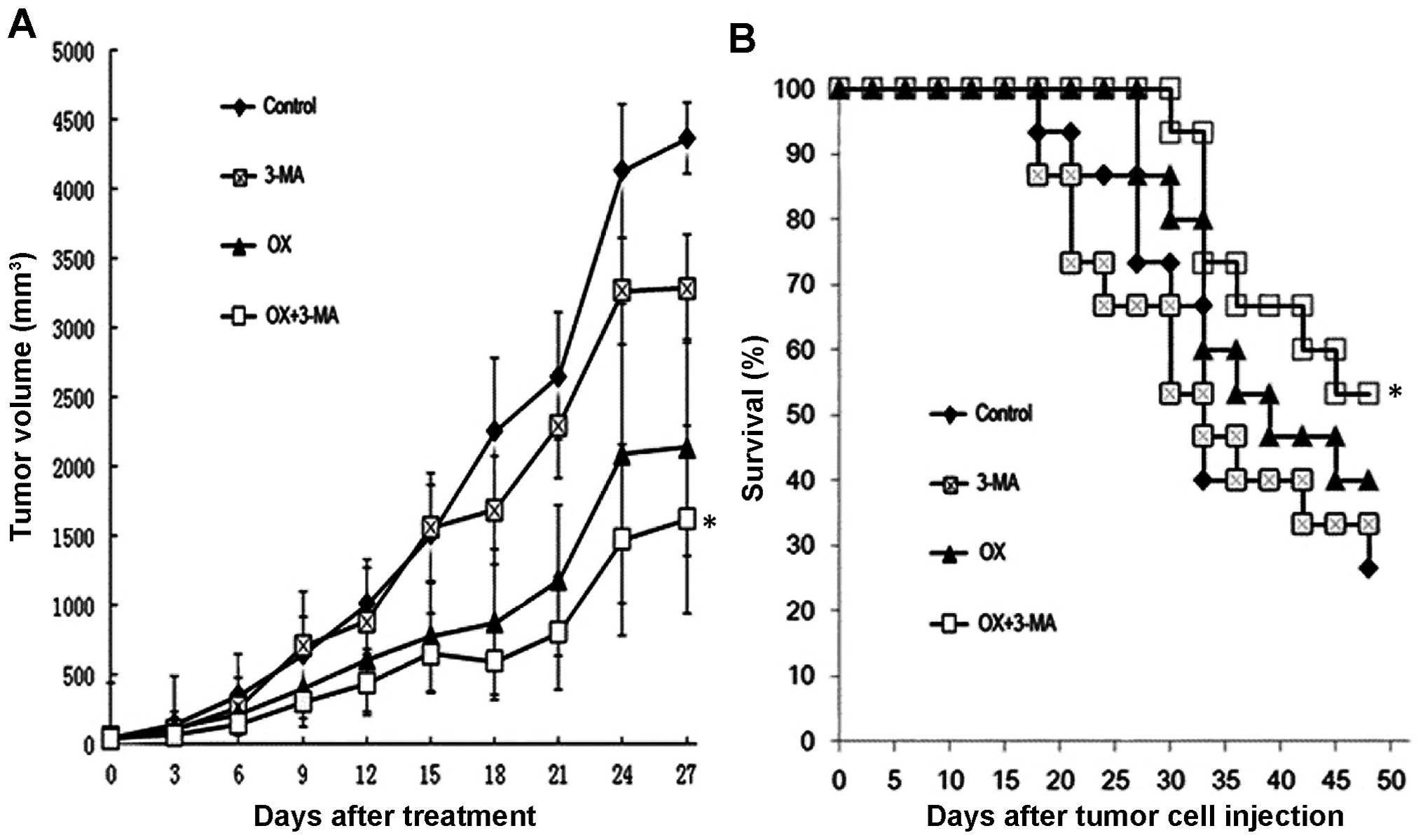
To investigate the synergistic cytotoxic effects of
OX combined with 3-MA in vivo, a mouse model in which colon
cancer-bearing mice received different treatment regimens was
established. Tumor growth was significantly slower in the mice that
received OX treatment alone compared with the mice that received
PBS or 3-MA alone (P<0.05). Furthermore, cotreatment of the
tumor-bearing mice with OX and 3-MA suppressed tumor growth to a
greater extent than OX treatment alone (Fig. 4A). Consistently, mice cotreated with
OX and 3-MA exhibited significantly longer survival times compared
with the mice treated with OX alone (P<0.01; Fig. 4B).
Reduction of cell autophagy and
increase of cell apoptosis in tumor tissues by combinational
treatment with OX and 3-MA
To investigate the potential antitumor mechanism of
combined OX plus 3-MA treatment in vivo, three sacrificed
mice from each group were selected on day 27 after tumor cell
inoculation, and tumor tissue from each mouse was collected, cut
into ultrathin slices and used for detecting cell autophagy and
cell apoptosis. As indicated in Fig.
5A, autophagosomes with a double membrane structure accompanied
by typical swollen organelles were observed in the tumor tissues of
mice treated with OX and OX plus 3-MA. However, the frequency of
autophagosomes in the tumors of mice treated with OX alone were
significantly higher compared with the tumors of mice treated with
OX plus 3-MA (Fig. 5B; P<0.05),
indicating a reduction of autophagy in tumor tissues by the
cotreatment of mice with OX plus 3-MA. In contrast to tumor tissues
obtained from the OX and OX plus 3-MA group mice, transmission
electron microscopy of the tumor tissues obtained from the control
and 3-MA groups showed little ultrastructure change and few
autophagosomes (Fig. 5A and B).
Consistent with these ultrastructure changes, the protein
expression levels of LC3-II and ATG5 were increased in the tumor
tissues of the OX group, and reduced in the OX plus 3-MA
cotreatment group (Fig. 5C).
TUNEL staining of tumor tissues from mice that
underwent different treatment regimens revealed that 3-MA treatment
resulted in a low proportion of apoptotic cells while OX treatment
markedly increased the proportion of apoptotic cells, compared with
the control group. Furthermore, combined treatment with OX and 3-MA
significantly enhanced tumor cell apoptosis, compared with OX
treatment alone (Fig. 6A and B;
P<0.05). The increased level of tumor cell apoptosis observed in
mice treated with OX plus 3-MA supported the aforementioned
observations of the current study, including the significant
inhibition of tumor growth and the prolonged of survival time of
mice receiving combinational treatment.
Discussion
The present study demonstrated that OX treatment
induces cancer cell autophagy as well as cell apoptosis, and that
the induction of autophagy by OX compromised its apoptotic effects
on colon cancer cells. Furthermore, inhibition of autophagy by 3-MA
markedly augmented the OX-induced apoptosis of colon cancer cells
in vitro and consequently enhanced OX-suppressed tumor
growth in vivo.
Apoptosis and autophagy are two major cell death
pathways in healthy cells and in tumor cells. It has previously
been reported that the activation of autophagy in cancer cells
inhibits therapy-induced apoptosis (17,18). In
the current study, OX was observed to induce apoptosis as well as
autophagy in CT26 cells. The observed increase in apoptosis was
supported by the upregulated expression of apoptosis-related
proteins, such as Bax, active caspase-3 and p53. Furthermore, OX
administration was associated with the increased expression levels
of a number of autophagy marker proteins, such as LC3-II, Beclin1
and ATG5. Consistent with these results, activation of apoptosis by
OX was determined by conducting flow cytometric analysis and a
TUNEL assay, while activation of autophagy was corroborated by
immunofluorescence staining, AO staining, MDC staining and
electronic microscopy. Notably, inhibition of the autophagy
signaling pathway by 3-MA significantly enhanced OX-induced cell
apoptosis in vitro and tumor suppression in vivo,
indicating that the activation of autophagy by OX may reduce OX
cytotoxicity. The results of the current study are consistent with
previous findings (17,18) and a recent report (14), in which cisplatin-induced autophagy
reduced its apoptotic effect by downregulating the ER
stress-mediated apoptosis pathway and the mitochondrial apoptosis
pathway in HeLa cells. Considering the results of the present
study, it is plausible that OX-activated autophagy may be
responsible for the observed clinical inefficiency of OX in
specific patients with colon cancer. Although OX has proven
beneficial in the treatment of advanced colon cancer, previous
studies reported that ~50% of patients did not respond to a
combination of OX and 5-FU treatment (19), and OX failed to eradicate
micrometastatic disease in ~30% of patients who received
combination therapy of OX, 5-FU and leucovorin (20,21).
Therefore, incorporating autophagy inhibitors into the current
regimens for advanced colon cancer may increase their therapeutic
efficiency and improve the clinical outcomes of patients with
advanced colon cancer.
The findings of the present study are in line with a
recent report in which OX was demonstrated to activate autophagy in
colon cancer cells via the ER stress and ROS pathways, and
inhibition of this autophagy increased cell death upon OX treatment
in vitro (13). However, the
current study performed an additional step to demonstrate the
potential therapeutic efficiency and feasibility in vivo,
using a combinational treatment strategy of an autophagy inhibitor
and OX in a mouse model. In addition, a potential mechanism for the
suppression of OX-induced cytotoxicity in colon cancer cells was
proposed; i.e., that OX-induced autophagy inhibits its own
apoptotic effect in colon cancer cells. Similar to OX, a previous
study identified that cisplatin induces autophagy, in turn
antagonizing cisplatin-induced cytotoxicity in HeLa cells (14).
It appears to be a common phenomenon in colon cancer
that systemic therapies, such as chemotherapy and radiotherapy,
activate autophagy when they are intended to induce apoptosis. For
example, 5-FU, an alternative standard chemotherapeutic reagent in
colon cancer, has been demonstrated in vitro to induce
autophagy, which compromised the cytotoxic effects of 5-FU.
Furthermore, the administration of an autophagy inhibitor appeared
to increase the sensitivity of the colon cancer cells to 5-FU
(11,12). Similarly, radiotherapy was able to
induce autophagy while inhibition of autophagy enhanced
radiation-induced apoptosis in colon cancer cells in vitro
(22). These studies support the
clinical importance of inhibiting autophagy in colon cancer
therapy. Notably, high expression levels of autophagy-related
proteins, such as Beclin1 and LC3, have been detected in human
tumor samples. This upregulated expression appears to significantly
correlate with aggressive features and poor prognosis in colon
cancer (23–25), indicating that autophagy is highly
active in advanced colon cancer. Thus, the therapeutic effects of
OX and 5-FU are compromised in patients exhibiting cancer with high
expression levels of autophagy marker proteins, due to active
autophagy in these tumors. This may be an alternative explanation
for the failure of adjuvant therapeutic strategies containing OX
and 5-FU in specific patients with advanced colon cancer.
Therefore, in agreement with previous reports, the present study
highlights the need to combine autophagy inhibitors and OX for the
effective treatment of advanced colon cancer.
In conclusion, the present study identified that OX
treatment induces autophagy as well as apoptosis in colon cancer
cells, and that the autophagy induced by OX compromises its
apoptotic effects. However, blockage of the autophagy signaling
pathway using a combination of autophagy inhibitors and OX appears
to significantly increase the cytotoxicity of OX and, therefore,
enhance OX-induced tumor growth suppression in vivo. The
current study indicates that the addition of an autophagy inhibitor
to current regimens with OX may enhance the therapeutic effects
and, thus, benefit patients with advanced colon cancer.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. Feb 4–2015.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dahan L, Sadok A, Formento JL, Seitz JF
and Kovacic H: Modulation of cellular redox state underlies
antagonism between oxaliplatin and cetuximab in human colorectal
cancer cell lines. Br J Pharmacol. 158:610–620. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bleiberg H: Oxaliplatin (L-OHP): a new
reality in colorectal cancer. Brit J Cancer. (Suppl 4). 1–3. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Alcindor T and Beauger N: Oxaliplatin: a
review in the era of molecularly targeted therapy. Curr Oncol.
18:18–25. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Howells LM, Sale S, Sriramareddy SN, et
al: Curcumin ameliorates oxaliplatin-induced chemoresistance in
HCT116 colorectal cancer cells in vitro and in vivo. Int J Cancer.
129:476–486. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Klionsky DJ and Emr SD: Autophagy as a
regulated pathway of cellular degradation. Science. 290:1717–1721.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
White E: Deconvoluting the
context-dependent role for autophagy in cancer. Nat Rev Cancer.
12:401–410. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Holohan C, Van Schaeybroeck S, Longley DB
and Johnston PG: Cancer drug resistance: an evolving paradigm. Nat
Rev Cancer. 13:714–726. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen S, Rehman SK, Zhang W, Wen A, Yao L
and Zhang J: Autophagy is a therapeutic target in anticancer drug
resistance. Biochim Biophys Acta. 1806:220–229. 2010.PubMed/NCBI
|
|
11
|
Bijnsdorp IV, Peters GJ, Temmink OH,
Fukushima M and Kruyt FA: Differential activation of cell death and
autophagy results in an increased cytotoxic potential for
trifluorothymidine compared to 5-fluorouracil in colon cancer
cells. Int J Cancer. 126:2457–2468. 2010.PubMed/NCBI
|
|
12
|
Li J, Hou N, Faried A, Tsutsumi S,
Takeuchi T and Kuwano H: Inhibition of autophagy by 3-MA enhances
the effect of 5-FU-induced apoptosis in colon cancer cells. Ann
Surg Oncol. 16:761–771. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shi Y, Tang B, Yu PW, et al: Autophagy
protects against oxaliplatin-induced cell death via ER stress and
ROS in Caco-2 cells. PloS One. 7:e510762012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xu Y, Yu H, Qin H, et al: Inhibition of
autophagy enhances cisplatin cytotoxicity through endoplasmic
reticulum stress in human cervical cancer cells. Cancer Lett.
314:232–243. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sasaki K, Tsuno NH, Sunami E, et al:
Chloroquine potentiates the anti-cancer effect of 5-fluorouracil on
colon cancer cells. BMC Cancer. 10:3702010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shi W, Tang Q, Chen X, et al: Antitumor
and antimetastatic activities of vesicular stomatitis virus matrix
protein in a murine model of breast cancer. J Mol Med (Berl).
87:493–506. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Amaravadi RK, Yu D, Lum JJ, et al:
Autophagy inhibition enhances therapy-induced apoptosis in a
Myc-induced model of lymphoma. J Clin Invest. 117:326–336. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Romano S, D'Angelillo A, Pacelli R, et al:
Role of FK506-binding protein 51 in the control of apoptosis of
irradiated melanoma cells. Cell Death Differ. 17:145–157. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
de Gramont A, Figer A, Seymour M, et al:
Leucovorin and fluorouracil with or without oxaliplatin as
first-line treatment in advanced colorectal cancer. J Clin Oncol.
18:2938–2947. 2000.PubMed/NCBI
|
|
20
|
André T, Boni C, Navarro M, et al:
Improved overall survival with oxaliplatin, fluorouracil and
leucovorin as adjuvant treatment in stage II or III colon cancer in
the MOSAIC trial. J Clin Oncol. 27:3109–3116. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kuebler JP, Wieand HS, O'Connell MJ, et
al: Oxaliplatin combined with weekly bolus fluorouracil and
leucovorin as surgical adjuvant chemotherapy for stage II and III
colon cancer: results from NSABP C-07. J Clin Oncol. 25:2198–2204.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
He G, Wang Y, Pang X and Zhang B:
Inhibition of autophagy induced by TSA sensitizes colon cancer cell
to radiation. Tumour Biol. 35:1003–1011. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Giatromanolaki A, Koukourakis MI, Harris
AL, Polychronidis A, Gatter KC and Sivridis E: Prognostic relevance
of light chain 3 (LC3A) autophagy patterns in colorectal
adenocarcinomas. J Clin Pathol. 63:867–872. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Giatromanolaki A, Koukourakis MI,
Koutsopoulos AV, Harris AL, Gatter KC and Sivridis E: Autophagy and
hypoxia in colonic adenomas related to aggressive features.
Colorectal Dis. 15:e223–e230. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Koukourakis MI, Giatromanolaki A, Sivridis
E, Pitiakoudis M, Gatter KC and Harris AL: Beclin 1 over- and
underexpression in colorectal cancer: distinct patterns relate to
prognosis and tumour hypoxia. Brit J Cancer. 103:1209–1214. 2010.
View Article : Google Scholar : PubMed/NCBI
|