Introduction
Anabolic steroids are synthetic derivatives of the
naturally occurring testosterone, which can be useful in the
treatment of some clinical conditions including hypogonadism.
Unfortunately, these agents are often illegally or used without
prescription by athletes and young physically active individuals
aiming to increase their muscle mass and physical performance
(1). At high doses, termed
supraphysiologic or toxic doses, the use of anabolic adrenergic
steroids (AASs) can predispose individuals to serious
complications, which may affect a number of organs, including: the
liver, kidney, sexual and reproductive organs, the brain, the
neurohormonal axis and the cardiovascular system (2-4).
The association between ischemic heart disease (IHD)
and the concurrent use of AASs is underestimated in medical
literature, possibly due to the tendency of the affected
individuals to conceal their use of AAS (5). However, several cardiovascular
complications have been reported with supraphysiologic doses of
anabolic steroids. Myocardial infarction, hypertension, stroke,
cardiomyopathy, pulmonary embolism and fatal and non-fatal
arrhythmias are examples of those complications (2,3).
Notably, only few case reports identified in the literature
describing young AASs users suffering from acute myocardial
infarction (AMI) (5). However, none
of the previous reports described such a case in a young physically
active physician.
The aim of the present report was to increase
awareness amongst physicians concerning the use of anabolic
steroids and their possible cardiovascular consequences,
particularly in young patients without any obvious or normal
cardiovascular risk factors. In addition, young medical personnel
cannot be excluded from the group of potential users of
non-prescription AASs. In fact, among these patients, admitting to
the use of AASs may be more embarrassing compared with others.
Case report
The publication of this report was approved by the
local Institutional Review Board of King Abdullah University
Hospital affiliated with the Jordan University of Science and
Technology (approval no. 781182018). The requirement for patient
consent was waived.
A 26-year-old physically active male who had no
prior medical history was admitted to the emergency department (ED)
in an associated public hospital. The primary complaint of the
patient was a severe chest pain lasting for 30 min. When obtaining
the medical history and initial examination, the patient appeared
healthy and had no other complaints, diseases or known risk factors
for coronary syndromes. The primary assessment of the attending
physicians and management plan were focused on a musculoskeletal
cause of the chest pain, taking into consideration the young age of
the patient, regular physical training, and the lack of
cardiovascular risk factors. The patient was discharged with oral
acetaminophen to be taken when needed.
At home, the patient's pain increased in severity
and was accompanied by excessive sweating and nausea. Consequently,
his family brought him back to the central university hospital. The
patient was admitted to the ED; he became dizzy, his blood pressure
was 80/40 mmHg, his pulse was regular (pulse rate 101/min), his
respiratory rate was 20/min and his blood O2 saturation
was 90%. The patient's electrocardiogram (ECG) revealed ST-segment
elevation up to 4 mm in leads V2 and V3.
At this stage, the diagnosis of a massive AMI
associated with cardiogenic shock was established. Immediately, the
patient was administered intravenous heparin (5,000 IU), oral
therapy with aspirin (300 mg crushed), clopidogrel (600 mg loading
dose), atorvastatin (40 mg), and provided with optimum oxygen
supply (simple mask, 3 liters/min).
Blood chemistry was obtained and demonstrated
increased levels of ischemic cardiac markers creatine kinase (CK)
(10,387 U/l) and CK-MB (958.1 U/l). The fasting lipid profile
revealed a very low concentration of high density lipoprotein (HDL)
(0.4 mmol/l), with normal levels of low density lipoprotein (LDL)
(1.48 mmol/l).
The patient was transferred to the cardiac care unit
(CCU) for monitoring and preparation for urgent catheterization. In
the CCU, a new right bundle branch block was identified in the
patient's ECG. The echocardiography demonstrated low ejection
fraction (35%), anterior apical wall akinesia with grade I mitral
regurgitation and the left ventricular end diastolic diameter was
5.7 cm.
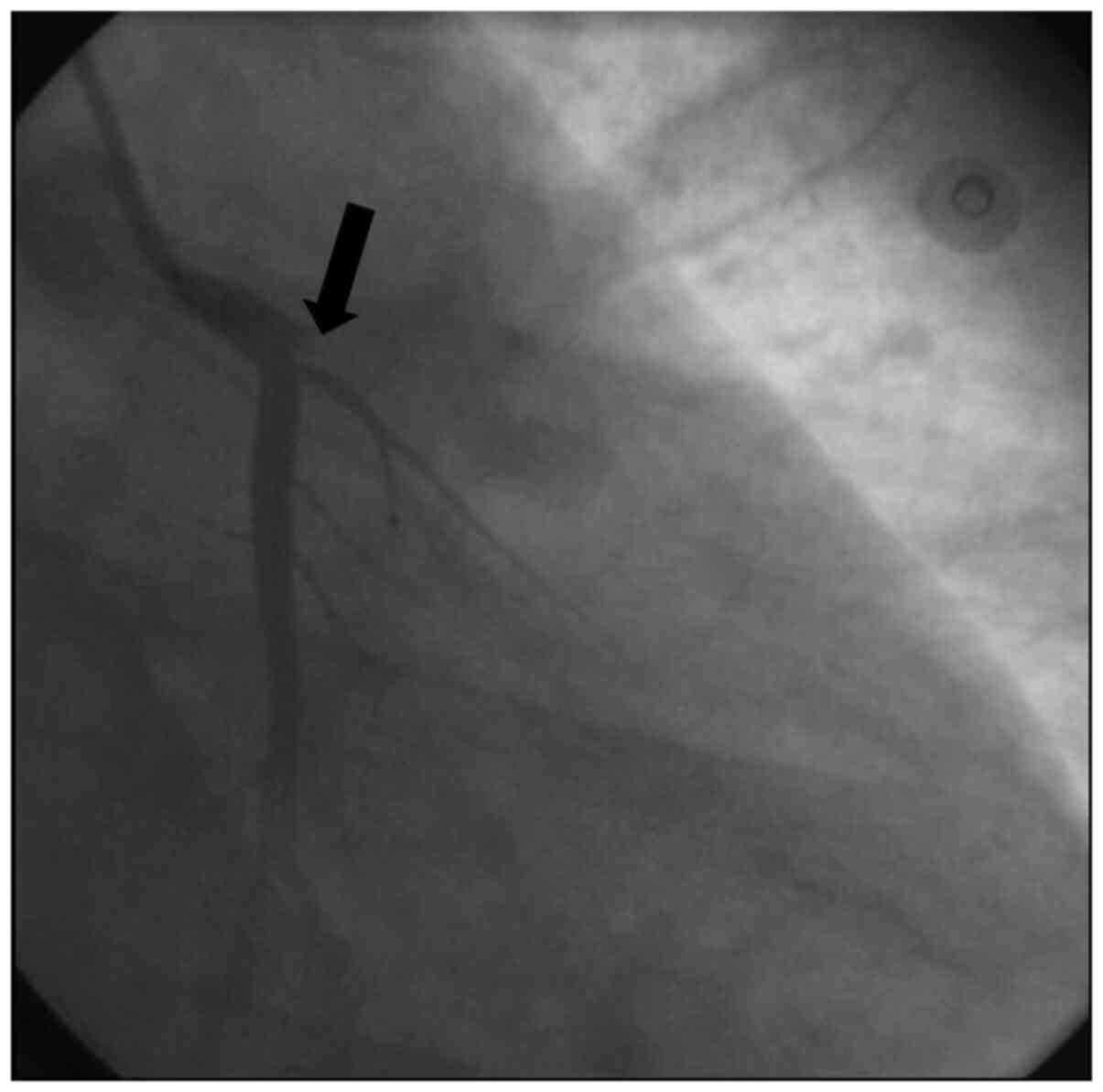
Urgent cardiac catheterization was performed 1 h
after admission to the CCU, and total occlusion of the ostium of
the left anterior descending artery by large thrombus was observed
(Fig. 1). Successful recanalization
was performed with a bare metal stent (BMS) (3.5x23 mm), and
thrombolysis in myocardial infarction 2 flow was established. The
patient was then administered tirofiban using percutaneous coronary
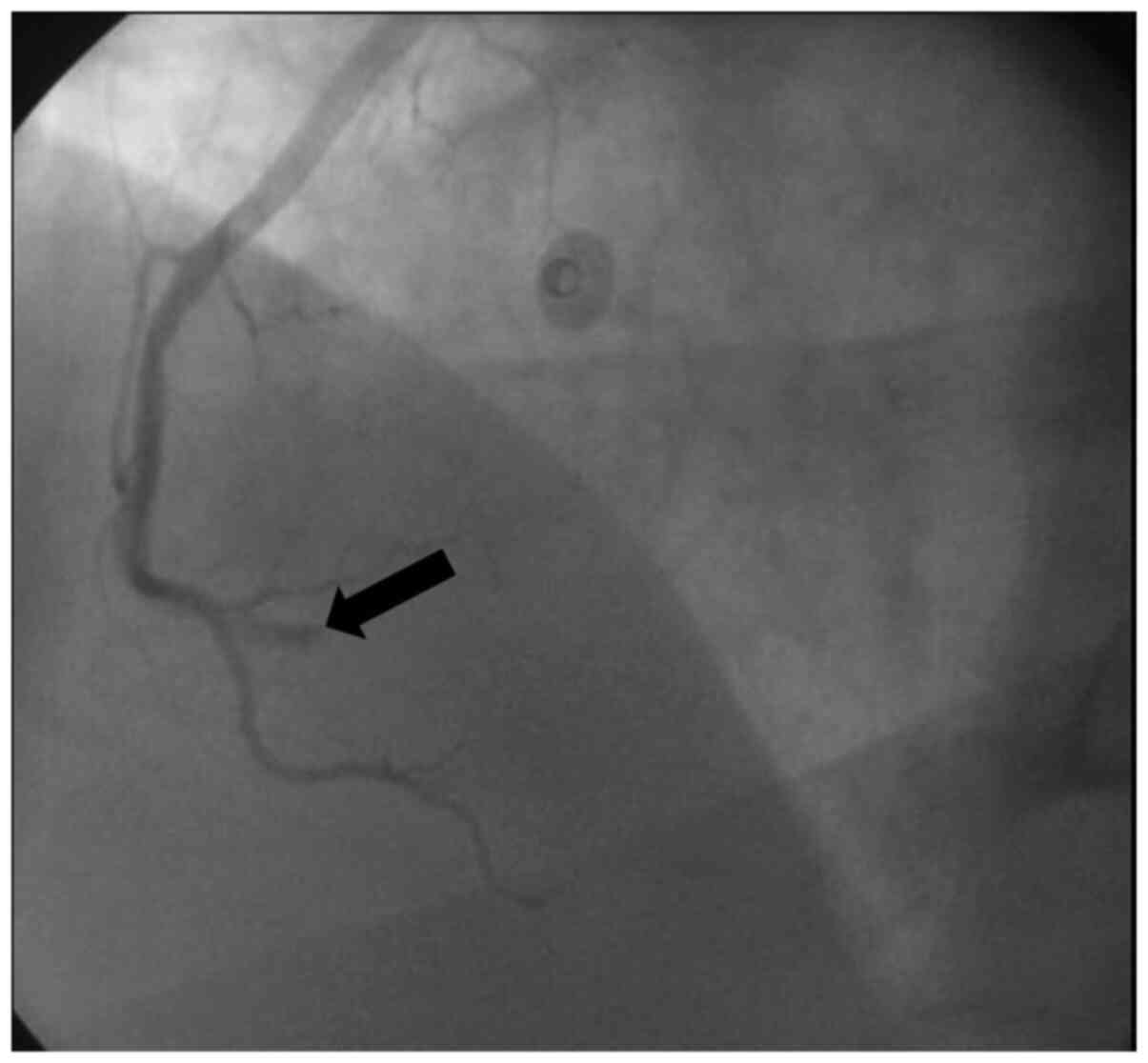
intervention (PCI). The left circumflex artery was normal; however,
notably, the right coronary artery (RCA) was affected: The
pre-bifurcation was totally occluded by an embolized thrombus
(Fig. 2). This may explain the
changes in ECG observed in the CCU. Successful recanalization was
performed with a BMS (3x18 mm). An intra-aortic balloon pump was
inserted, and the patient was administered a small dose (5
µg/kg/min) of the vasopressor dopamine for 2 days.
The patient had an uneventful hospital course. The
intra-aortic balloon pump was removed, and treatment with the
vasopressor was stopped after 2 days. After 7 days, the patient was
discharged with the following medications: Clopidogrel [75 mg per
os (PO) once daily]; aspirin (100 mg PO once daily); lansoprazole
(30 mg PO once daily); atorvastatin (40 mg PO once daily);
spirolactone (25 mg PO once daily); carvedilol (3.125 mg PO twice
daily); lasix (40 mg PO once daily); and enalapril (2.5 mg PO once
daily).
After obtaining a detailed history, and when the
patient realized the seriousness of his condition, he admitted that
he has been using anabolic steroids and amino acids
supplementations (sustanon 250 mg, once per week for 6 months and
whey protein isolate, 6 tabs every day for 1 year).
During follow up, the patient continued to suffer
heart failure with low ejection fraction. In addition, he developed
an apical thrombus 2 months after admission. The patient developed
tachycardia in spite of optimal medical treatment, and finally
received an implantable cardioverter defibrillator.
Discussion
Few case reports of AMI occurring in healthy
individuals who are regularly/chronically using AASs have been
documented in the literature (2,5-8).
The lack of predisposing risk factors for AMI, young age, male sex,
being physically active and the concurrent use of AASs were common
factors in the majority of these previous reports. All of the
reports concluded that the concomitant use of AAS may be
responsible for these events, as a well-known cardio-toxic factor.
However, none of these cases were able to prove a causal
association between AAS overuse and IHD. In agreement with this
observational association, evidence on other AAS-induced
cardiovascular complications exist. For example; chronic AAS abuse
has been associated with ischemic stroke and cerebral hemorrhage,
renal infarction and sudden cardiac death (7,9-11).
In the present case report, although the patient was
a physician, he did not realize the seriousness of his symptoms
until his condition had deteriorated significantly. The patient did
not disclose his chronic use of AASs, and the attending physician
trusted the patient's reported history. At first admission, both
the patient and the attending physician were considering a
musculoskeletal cause of the chest pain. The present report
emphasizes the fact that medical professionals can be AASs users
and they may ignore this usage and its association with IHD. This
may be associated with the effect of these substances on the users
mental status (12), the common
association between musculoskeletal chest pain and intense sports
activities, or the embarrassment of the medical professional users
to declare AAS usage, particularly because they are generally
perceived to understand the catastrophic effects of AASs.
The potential underlying pathological processes that
predispose individuals to AAS-induced AMI may include atherogenic,
thrombotic and vasospastic mechanisms, which were previously
reviewed (5). The risk of thrombosis
may be increased with AAS usage, which has been identified to
activate platelet aggregation (13,14).
Conversely, AAS usage, particularly in high doses, is known to
stimulate erythropoiesis, which in turn can increase blood
viscosity and may predispose for vascular thrombosis (2). In the present report, the blood
hematocrit values of the patient were normal. Although not
extensively investigated, these normal values may negate such an
assumption of erythropoiesis stimulation in this case. In addition,
AAS abuse can change patient lipid profiles unfavorably; with
increased levels of LDL-C and decreased levels of HDL and
lipoprotein-A (9). This was
confirmed in the present case report; however, in all previous case
reports that documented these changes, the patients were not
screened for a sufficient length of time. In these patients, the
lipid values were measured at the time when the patients were
admitted to hospital due to AMI symptoms.
Notably, in the present case, the patient may have
suffered from both atherogenic (Fig.
1) and thrombotic (Fig. 2)
coronary blockages. However, as it was not possible to examine the
patient prior to hospital admission, it is unknown if the use of
AASs caused the left atherosclerotic coronary lesion or,
alternatively, if this use exacerbated a pre-existing lesion.
Conversely, there was no clear evidence of an intra-ventricular
thrombus, which may have explained the embolic thrombus in the
right coronary artery. The documented evidence of the ability of
AASs to increase blood thrombosis (5) may explain this event. In addition,
although the vasospastic mechanism is less established as a factor
in AASs-based AMI (15,16), it may possibly intensify the
atherogenic or the thrombotic mechanisms of AMI in AASs users. In
concordance with these data, AAS abuse has been identified to
induce vascular and endothelial dysfunctions (17,18).
Therefore, vasospastic agents were added to the pharmacological
regimen of the patient in the present report. In addition, the
ability of chronic AASs use to cause arrhythmias (19,20) may
lead to spontaneous formation of small thrombotic embolisms, which
in turn, may be transported toward the coronary arteries and cause
significant blockages. Notably, the AMI itself in chronic AASs
users may also cause disruption to the autonomic nervous supply of
the heart, which may predispose these individuals to spontaneous
arrhythmias (5,21). In turn, this may cause a thrombotic
event within the ventricles, which may translocate to the coronary
arteries and cause an embolism.
Conversely, it has been suggested that chronic AASs
use may affect ventricular diastolic function (22). It may also cause significant
hypertrophy and consequent arrhythmias (23). Coronary artery filling and normal
coronary blood flow depends on the diastolic period of the cardiac
cycle. Therefore, this may cause blood stasis, blood flow
turbulence, and can affect the endothelial-vascular functions.
Consequently, it may predispose patients to thrombotic or
atherosclerotic events. The hypertrophic nature of the heart in AAS
users can also contribute to this mechanism. In addition, certain
studies have investigated the role of chronic AASs abuse in
increasing both systolic and diastolic blood pressure values
(24), which in turn may increase
the heart load and predispose for AMI. However, the patient in the
present report arrived at the ER in cardiogenic shock. Therefore,
the chronic effect on blood pressure or cardiac hypertrophy were
not measured, and remain unknown.
Finally, it was difficult to evaluate if the chronic
complications in the patient were due to the AASs use or his acute
ischemic condition. However, a number of previous studies in the
literature describe the ability of AASs to affect the functions of
the heart even after long periods of discontinued use (3-5).
In conclusion, a case of a massive anterior MI in a
young physically active person who had no past medical history of
any cardiovascular risk factors was described. In this case, AMI
incidence was complicated with a cardiogenic shock and a mid-RCA
embolic obstruction. The chronic use of AASs was considered as the
most likely cause for the condition of the patient.
Physicians should always be aware of the possibility
of AASs use in young patients suffering from chest pain,
particularly in patients without obvious risk factors for ischemic
diseases. IHD should always be suspected and investigated with
typical chest pain in healthy young patients, even if regular risk
factors are not present. Increased efforts toward increasing public
awareness of the potential complications of AASs abuse are required
from medical and educational institutes. Medical professionals
should not be excluded as potential AASs users/abusers.
Acknowledgements
Not applicable.
Funding
Funding
No funding was received.
Availability of data and materials
The ECGs and the records of the coronary angiogram
are available from the authors upon reasonable request.
Authors' contributions
All authors contributed to the conception of the
study. NA prepared the first draft and was a major contributor in
writing the manuscript. MIJ and KHA revised the manuscript
critically for important intellectual content. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The publication of this report was approved by the
local Institutional Review Board of King Abdullah University
Hospital affiliated with the Jordan University of Science and
Technology (approval no. 781182018). The requirement for patient
consent was waived.
Patient consent for publication
The requirement for patient consent for publication
was waived.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Santos RP, Pereira A, Guedes H, Lourenço
C, Azevedo J and Pinto P: Anabolic drugs and myocardial
infarction-a clinical case report. Arq Bras Cardiol. 105:316–319.
2015.PubMed/NCBI View Article : Google Scholar : (In English,
Portuguese).
|
|
2
|
Stergiopoulos K, Brennan JJ, Mathews R,
Setaro JF and Kort S: Anabolic steroids, acute myocardial
infarction and polycythemia: A case report and review of the
literature. Vasc Health Risk Manag. 4:1475–1480. 2008.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Luijkx T, Velthuis BK, Backx FJ, Buckens
CF, Prakken NH, Rienks R, Mali WP and Cramer MJ: Anabolic
androgenic steroid use is associated with ventricular dysfunction
on cardiac MRI in strength trained athletes. Int J Cardiol.
167:664–668. 2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kersey RD, Elliot DL, Goldberg L, Kanayama
G, Leone JE, Pavlovich M and Pope HG Jr: National Athletic
Trainers' Association. National athletic trainers' association
position statement: Anabolic-androgenic steroids. J Athl Train.
47:567–588. 2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Christou GA, Christou KA, Nikas DN and
Goudevenos JA: Acute myocardial infarction in a young bodybuilder
taking anabolic androgenic steroids: A case report and critical
review of the literature. Eur J Prev Cardiol. 23:1785–1796.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Peoples K, Kobe D, Campana C and Simon E:
Hyperhomocysteinemia-induced myocardial infarction in a young male
using anabolic steroids. Am J Emerg Med. 32:948.e1–2.
2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ilhan E, Demirci D, Güvenç TS and Calık
AN: Acute myocardial infarction and renal infarction in a
bodybuilder using anabolic steroids. Turk Kardiyol Dern Ars.
38:275–278. 2010.PubMed/NCBI
|
|
8
|
Wysoczanski M, Rachko M and Bergmann SR:
Acute myocardial infarction in a young man using anabolic steroids.
Angiology. 59:376–378. 2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Hartgens F, Rietjens G, Keizer HA, Kuipers
H and Wolffenbuttel BH: Effects of androgenic-anabolic steroids on
apolipoproteins and lipoprotein (a). Br J Sports Med. 38:253–259.
2004.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Fineschi V, Riezzo I, Centini F,
Silingardi E, Licata M, Beduschi G and Karch SB: Sudden cardiac
death during anabolic steroid abuse: Morphologic and toxicologic
findings in two fatal cases of bodybuilders. Int J Legal Med.
121:48–53. 2007.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kennedy MC, Corrigan AB and Pilbeam ST:
Myocardial infarction and cerebral haemorrhage in a young body
builder taking anabolic steroids. Aust N Z J Med.
23(713)1993.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lyngberg KK: Myocardial infarction and
death of a body builder after using anabolic steroids. Ugeskr
Laeger. 153:587–588. 1991.PubMed/NCBI(In Danish).
|
|
13
|
Pilo R, Aharony D and Raz A: Testosterone
potentiation of ionophore and ADP induced platelet aggregation:
Relationship to arachidonic acid metabolism. Thromb Haemost.
46:538–542. 1981.PubMed/NCBI
|
|
14
|
Kokkonen L, Anttonen O, Penttilä O and
Voutilainen S: Protein C deficiency and use of anabolic steroids
behind the myocardial infarction in a young man. Duodecim.
117:2279–2281. 2001.PubMed/NCBI(In Finnish).
|
|
15
|
Buttner A, Sachs H, Mall G, Tutsch-Bauer E
and Weis S: Progressive idiopathic bilateral
striato-pallido-dentate calcinosis (Fahr's disease) in a person
with anabolic steroid abuse. Leg Med (Tokyo). 3:114–118.
2001.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sonmez E, Turkdogan KA, Yilmaz C,
Kucukbuzcu S, Ozkan A and Sogutt O: Chronic anabolic androgenic
steroid usage associated with acute coronary syndrome in
bodybuilder. Turk J Emerg Med. 16:35–37. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Skogastierna C, Hotzen M, Rane A and
Ekström L: A supraphysiological dose of testosterone induces nitric
oxide production and oxidative stress. Eur J Prev Cardiol.
21:1049–1054. 2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tischer KH, Heyny-von Haussen R, Mall G
and Doenecke P: Coronary thrombosis and ectasia of coronary
arteries after long-term use of anabolic steroids. Z Kardiol.
92:326–331. 2003.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
19
|
Phillis BD, Abeywardena MY, Adams MJ,
Kennedy JA and Irvine RJ: Nandrolone potentiates arrhythmogenic
effects of cardiac ischemia in the rat. Toxicol Sci. 99:605–611.
2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Sculthorpe N, Grace F, Jones P and Davies
B: Evidence of altered cardiac electrophysiology following
prolonged androgenic anabolic steroid use. Cardiovasc Toxicol.
10:239–243. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Maior AS, Carvalho AR, Marques-Neto SR,
Menezes P, Soares PP and Nascimento JH: Cardiac autonomic
dysfunction in anabolic steroid users. Scand J Med Sci Sports.
23:548–555. 2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kasikcioglu E, Oflaz H, Umman B and Bugra
Z: Androgenic anabolic steroids also impair right ventricular
function. Int J Cardiol. 134:123–125. 2009.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Frati P, Busardò FP, Cipolloni L,
Dominicis ED and Fineschi V: Anabolic androgenic steroid (AAS)
related deaths: Autoptic, histopathological and toxicological
findings. Curr Neuropharmacol. 13:146–159. 2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Gheshlaghi F, Piri-Ardakani MR, Masoumi
GR, Behjati M and Paydar P: Cardiovascular manifestations of
anabolic steroids in association with demographic variables in body
building athletes. J Res Med Sci. 20:165–168. 2015.PubMed/NCBI
|