Introduction
Erythropoietin (EPO) is a single chain glycoprotein
that promotes hematopoietic cell growth through binding to the EPO
receptor; recombinant human EPO (rhEPO) has previously been
successfully used in the treatment of severe anemia (1-3).
EPO is primarily produced in the kidneys but is also detectable in
other organs, such as the liver and the brain (4). In addition to hematopoietic
growth-promoting activity, EPO has been shown to exhibit
anti-apoptotic and neuroprotective effects in acute
hypoxic/ischemia cerebral damages (5). However, the effect of EPO treatment on
chronic cerebral ischemia (CCI) remains relatively unknown.
A major challenge for clinical application of EPO in
cerebral ischemia is to facilitate its delivery to the central
nervous system (CNS) across the blood-brain barrier (BBB) (6). Current approaches for EPO delivery to
the CNS in animal models include systemic [intraperitoneal (i.p.)
or subcutaneous], intracerebroventricular (i.c.v.) and intranasal
administrations. Because only 0.5-1% of systemically administered
EPO can cross the BBB (7), higher
doses of EPO are required to reach effective concentrations in the
brain, leading to severe side effects such as cerebral infarct and
overproduction of platelets (8-11).
Although direct i.c.v. injection of EPO has been shown to provide
significant protection against ischemic brain injury (12-14),
it may not be suitable for clinical use owing to high risks of
brain damage and infections (7).
Compared with systemic and i.c.v. administrations, the intranasal
delivery method has significant clinical potential owing to simple
and non-invasive drug administration, rapid CNS delivery and
minimal systemic exposure (15). A
previous study showed that the brain uptake of neurotherapeutics
after intranasal delivery is >5 times the uptake after i.p.
delivery (16). The present study
established a rat model of permanent bilateral common carotid
artery occlusion (2VO)-induced CCI that were treated with
intranasal rhEPO in order to explore the protective effects of
rhEPO on cognitive and visual impairments. Morris water maze (MWM)
and flash visual evoked potential (FVEP) measurement were used to
evaluate learning and memory abilities, and visual functions in
rats, respectively. Hematoxylin and eosin (H&E) staining was
performed to examine the histopathologic changes in the brain and
retina.
Materials and methods
Animals
Healthy male Sprague-Dawley rats (n=90; age, 6
months; weight, 300-340 g) were purchased from the Central Animal
House at Shanxi Medical University and maintained under standard
conditions according to the Animal Research Center guidelines of
Shanxi Medical University (Taiyuan, China). Rats were acclimatized
for 1 week before use. All rats were housed in rooms kept at 22˚C
with 60% humidity, and a 12-h light/dark cycle. Rats were provided
ad libitum access to food and water. All the experimental
procedures were approved by the Animal Use and Care Committee of
Shanxi Medical University. All animal experiments were performed in
accordance with the guidelines for Animal Use and Care of Shanxi
Medical University (Taiyuan, China).
2VO procedure
After a qualifying MWM test, rats were randomly
divided into sham-operated, 2VO + saline and 2VO + rhEPO groups
(n=30 rats/group). The 2VO surgery was performed to induce CCI as
previously described (17). Briefly,
rats were fasted for 12 h and deprived of water for 4 h followed by
an i.p. injection of 5% (mass/volume) chloral hydrate (325 mg/kg,
the dose for anesthesia before model establishment, Wuhan HeChang
Chemical Co., Ltd.). The rats were immobilized, shaved and
disinfected. The skin and mucosa at the front of the neck were cut
and the muscles were bluntly separated to expose the bilateral
common carotid arteries and the vagus nerve. The bilateral common
carotid arteries were tightly double ligated with silk braided
non-sutures (diameter, 26 mm; model number, 3-0; Johnson &
Johnson). The wound was then rinsed thoroughly with metronidazole
(Shijiazhuang No. 4 Pharmaceutical Co., Ltd.) and sutured layer by
layer. After recovery, rats were returned to their home cages with
free access to food and water. Rats in the sham-operated group were
subjected to the same procedure without ligation of the common
carotid arteries (17). The body
weight loss was <3% post-fasting for 12 h.
Intranasal drug delivery
rhEPO (Shenyang Sunshine Pharmaceutical Co., Ltd.;
3Sbio Group) was dissolved in sterile saline (Shijiazhuang No. 4
Pharmaceutical Co., Ltd.) at a concentration of 150 U rhEPO/120 µl.
At 3 days following the 2VO procedure, 2VO + rhEPO group was
intranasally administered with rhEPO (50 U/100 g/week; Shenyang
Sunshine Pharmaceuticals Co., Ltd.; 3Sbio Group) for 8 weeks.
Sham-operated and 2VO + saline groups were given an equivalent
volume of saline. Briefly, rats were anesthetized with 5%
(mass/volume) chloral hydrate (325 mg/kg) by i.p. injection
followed by stereotaxic frame (Chengdu Taimeng Technology &
Market Co. Ltd.,)-based immobilization in a supine position at a
-70˚ angle (18). A polyvinyl
chloride tube (inner diameter: 0.5 mm, outer diameter: 1.0 mm;
Jiangxi Hongda Medical Equipment Group Co., Ltd.) attached to a 1
ml syringe (Jiangxi Hongda Medical Equipment Group Co., Ltd.) was
inserted into each nostril to a depth of ~2 cm. A total of 125 µl
of rhEPO sterile solution containing 150 U rhEPO in 120 µl of
saline was delivered by gently pushing into the nasal cavities for
30 min. After delivery, the tube was removed, and the rats were
kept immobilized for 30 min to avoid the loss of rhEPO. Rats that
swallowed or expelled fluid were excluded from further analyses. A
total of eight rats in each group were included in the statistical
analysis. The other 12 rats were excluded as they did not meet the
test standards for various reasons.
MWM test
Rats were subjected to MWM test for spatial learning
and memory evaluation before 2VO surgery and after 8 weeks of
rhEPO/saline treatment, respectively. A black circular pool
(diameter, 150 cm; height, 50 cm) divided into four equal quadrants
and with four points designed as starting positions (I, II, III and
IV) was filled with water at 24˚C. A video camera was hanging over
the pool, and a black platform (diameter, 10 cm; height, 27 cm) was
submerged 2 cm below the surface of the water. The position of each
reference inside and outside the maze was kept unchanged during the
training sessions (19).
Before 2VO surgery, each rat received one training
session per day for 5 days consecutively (19,20).
Each session consisted of four trials with an interval of 1 h.
During each trial, the rat was gently placed in the water at one of
the four starting positions and faced toward the wall of the maze.
The time spent to find the hidden platform (escape latency) and the
swimming trajectories were recorded. If a rat failed to find the
platform within 2 min, the rat would be gently guided to the
platform and was allowed to stay on it for 5 sec before being
removed from the water. A maximum score of 2 min was assigned. On
day six, the platform was removed, and the rats were subjected to a
probe test for spatial memory assessment. Another probe test was
performed after 8 weeks of rhEPO or saline treatment. The number of
times a rat passed through the target platform within 2 min was
recorded.
FVEP measurement
FVEP, a cluster of electrical signals that occur in
the cerebral cortex in response to visual stimuli (21), was determined for visual function
evaluation. As two rats did not cooperate, in order to unify the
several indices in the experiments, a total of six rats
successfully administered drugs were selected from each group and
were anesthetized with chloral hydrate, such that comparisons could
be performed using paired statistics. Latency and amplitude of the
primary wave (P1) were recorded using a four channel signal
averager (Nicolet Biomedical Inc.).
H&E staining
After MWM test and FVEP measurement, rats were
anesthetized with 5% chloral hydrate and sacrificed by intracardial
perfusion with 0.9% saline (200-240 ml; Shijiazhuang No.4
pharmaceutical Co. Ltd.,) followed by 4% paraformaldehyde (250-400
ml; Tianjin Aoran Fine Chemical Research Institution) in 0.1 mol/l
PBS (pH 7.4; Tianjin Aoran Fine Chemical Research Institution).
When there is no sign of breath, the rats were deemed dead. The
brain and eyes of each rat were removed and fixed in 10%
formaldehyde for 48 h followed by dehydration in a graded series of
ethanol and paraffin embedding. Cerebral cortex, hippocampus CA1
and retina tissues were cut into sections (5 µm). The
paraffin-embedded sections were dewaxed in xylene, dehydrated using
a series of graded ethanol solutions (2 min each in 100, 90 and
70%), washed in distilled water, stained with H&E (Chengdu
Kelong Chemical Reagent Factory), dehydrated through graded ethanol
solutions (95% ethanol 15 sec, 100% ethanol 10 min), soaked for 10
min in turn in 100% xylene (I,II Tianjin Damao Chemical Reagent
Factory) and mounted using neutral balsam (Sinopharm Chemical
Reagent Co., Ltd.). Morphological changes were observed using an
optical microscopy (Chengdu Taimeng Technology & Market Co.,
Ltd.). The thicknesses of the cerebral cortex and the retina as
well as the number of hippocampus CA1 neurons and retinal ganglion
cells were measured using a light microscope (Olympus BX60F5;
Olympus Corporation) and a BI-2000 medical image analysis system
(Chengdu Taimeng Technology & Market Co., Ltd.).
Statistical analysis
Data were expressed as mean ± the standard error of
the mean. Statistical analysis was performed using R (22) version 3.5.1 and R-Studio version
1.0.44(23). Differences between
groups were compared using a one-way ANOVA with a post-hoc LSD
t-test, or a two-way ANOVA, followed by a LSD multiple comparisons
test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Clinical observation Model
establishment and behavioral observation after surgery
The rats were awake ~1 h after surgery. The main
clinical symptoms included drowsiness, poor spirit, apathy, a lack
of activity, limbs failing to fully stretch, vacillation to the
left and to the right when walking and a proneness to falling.
Rats after saline or rhEPO
treatment
After treatment, the control group (2VO + saline)
rats were less active, slow-moving, had memory deficits and
exhibited a lower sense of pain. One of the rats in the control
group repeatedly bit other rats. Rats in the experimental group
(2VO + rhEPO) and the sham-operated group were much more active and
more mentally quick and agile compared with the rats in the control
group.
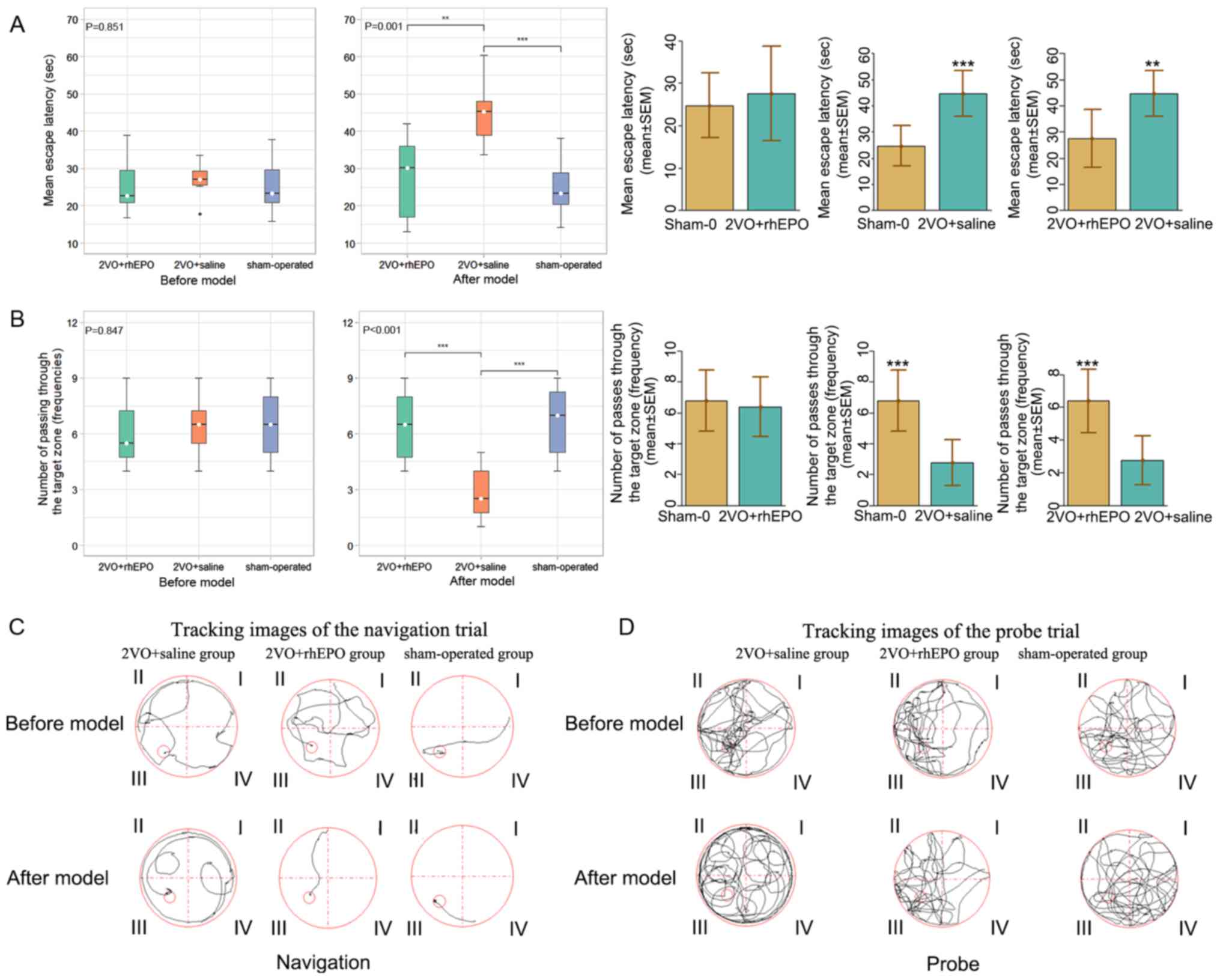
rhEPO protects CCI model rats from
learning and memory impairments
To investigate the effect of rhEPO on learning and
memory impairments in CCI, the present study established a
2VO-induced CCI rat model and treated the rats with rhEPO once a
week for 8 weeks. MWM training and tests were performed to evaluate
spatial learning and memory in rats before modeling and 8 weeks
after modeling/treatment. As shown in Fig. 1A (left), no significant difference
was observed in the escape latency among the three groups (P=0.851)
before modeling. After modeling, there was a significant difference
in the escape latency between the three groups (P=0.000). After 8
weeks of modeling and treatment, as shown in Fig. 1A (right) the escape latency in the
2VO + saline group was significantly increased compared with that
in the sham-operated group (P=0.000), which indicated that there
was an impaired spatial learning ability in the saline-treated CCI
rats. By contrast, the escape latency in the experimental group
(2VO + rhEPO) was significantly lower compared with that in the
control group (2VO + saline) (P=0.001) and remained comparable with
the sham-operated group (P=0.549).
In addition, the frequencies of passing through the
target zone were comparable among the three groups before modeling
(P=0.847; Fig. 1B, left), whereas
after modeling, there was a significant difference in the number of
passes through the target zone between the three groups (P=0.000).
After 8 weeks of modeling and treatment, as shown in Fig. 1B (right), the rats in the 2VO +
saline treatment group crossed the target zone significantly less
often than those in the sham-operated group after the
model/treatment was established (P=0.000), which suggested that
there may be a memory deficit in rats with 2VO-induced CCI. By
contrast, the frequency of passing through the target zone in
rhEPO-treated CCI rats was significantly higher compared with that
in saline-treated ones (P=0.001) and remained comparable with the
sham-operated group (P=0.591), which suggested that there was a
protective role of rhEPO against memory impairment in CCI rats.
Similar results were observed in the swimming trajectory length
(Fig. 1C and D). Taken together, these data suggested
that rhEPO may provide effective protection against learning and
memory deficits in rats with CCI.
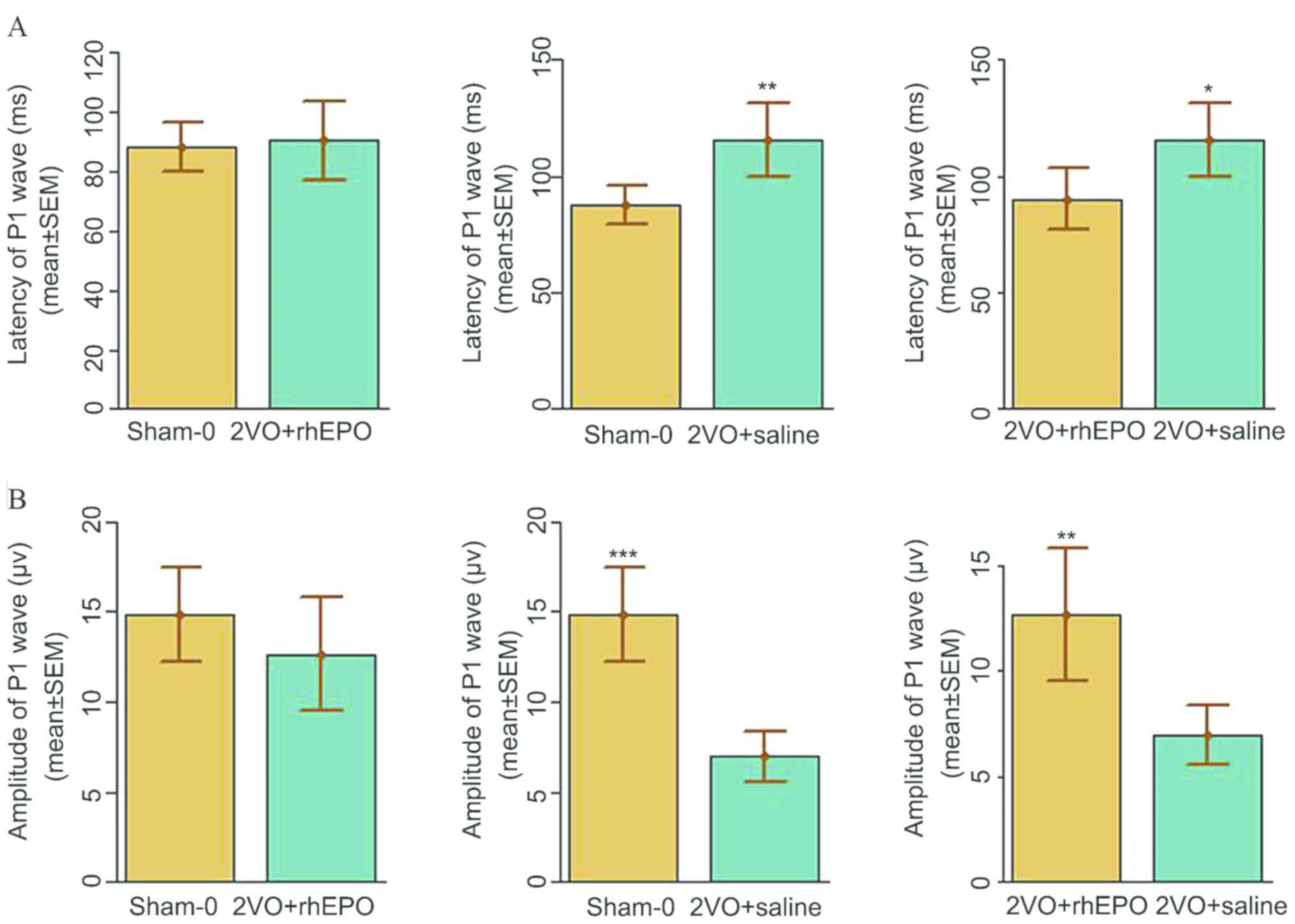
rhEPO improves visual dysfunction in
rats with CCI
As cerebral ischemia has previously been shown to
cause retinal damage, which can lead to visual function impairment
and subsequent deteriorated spatial learning ability (24,25), the
present study next sought to investigate the effect of rhEPO on
visual functions in CCI model rats. As shown in Fig. 2, the results of FVEP measurements
indicated that the latency and amplitude of the P1 wave were
significantly increased and decreased, respectively, in the 2VO +
saline group compared with those in the sham-operated group, which
suggested that CCI induced visual dysfunction in rats with 2VO.
Importantly, rhEPO treatment markedly reduced the latency and
elevated the amplitude of the P1 wave compared with the 2VO +
saline treatment group, which suggested that rhEPO may restore some
visual function in CCI rats, which in turn improves the spatial
learning ability in these rats.
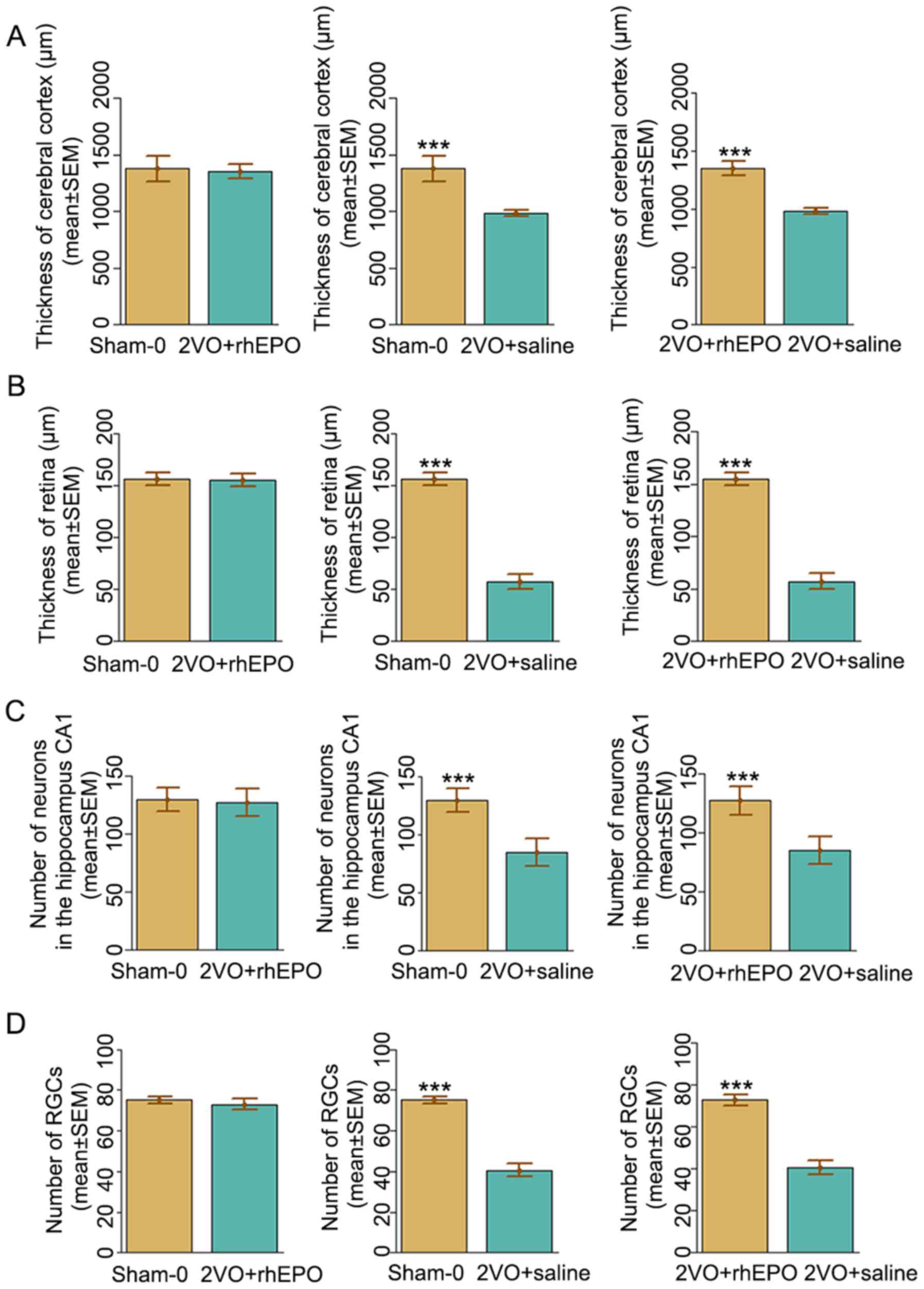
rhEPO reverses neuropathological and
retinal alterations in rats with CCI
To further study the histopathological basis of the
improved learning and memory impairments in rhEPO-treated rats,
H&E staining was performed to observe the morphological changes
in the hippocampal CA1 region, which is known to be highly involved
in learning and memory (26), as
well as morphological changes in the retina in response to rhEPO
administration. Neurons with abnormal nuclear shape and massive
vacuolation of cytoplasm were loosely and irregularly arranged in
the control (2VO + saline) group. By contrast, in the experimental
(2VO + rhEPO) group, neuronal cells with normal size and morphology
were tightly packed and ordered. In addition, the thickness of
cerebral cortex was significantly decreased in the 2VO + saline
group compared with that in the sham-operated group (982±28 µm vs.
1378±113 µm), which was significantly improved in the 2VO + rhEPO
group (1,350±63 µm vs. 982±28 µm, F=49.645, P<0.001) (Fig. 3A). Similar results were observed in
the thickness of retina (Fig. 3B),
the number of neurons in hippocampus CA1 area (Fig. 3C) and the number of retinal ganglion
cells (Fig. 3D). These data
collectively suggested a protective role of rhEPO against neuronal
and retinal damage in rats with CCI.
Discussion
Intranasal delivery of neurotherapeutics is widely
used in animal experiments owing to its simple and non-invasive
administration, repeatability, and rapid and effective CNS delivery
(15). EPO is a heat-resistant
acidic glycoprotein containing sialic acid and is typically used to
treat different types of anemia (1,3). In
addition, EPO has been shown to exert neuroprotective effects on
acute ischemia in the CNS through various mechanism (27), such as inhibiting glutamate
overproduction (28), inflammation
(29,30) and oxidative stress (31). It has been reported that intranasal
administration of EPO is a non-invasive, simple approach to bypass
the BBB (32) and is safer, 10-times
more rapid and more efficient than intravenous delivery in acute
brain injury animal models (33).
However, the effect of intranasally delivered EPO on CCI-induced
brain and retina damage remains unclear. The present study explored
the effects of intranasally delivered rhEPO on behavior, spatial
orientation, learning and memory and vision function in rats with
2VO-induced CCI.
CCI is considered both a neurological and
cerebrovascular disease and is characterized by progressive
cognitive and behavioral deterioration caused by long-term cerebral
blood perfusion insufficiency (34).
Permanent 2VO in rats can induce cognitive impairment and has been
widely used to establish CCI models (17). CCI is closely associated with several
cerebrovascular diseases, including cerebral arteriosclerosis,
cerebral infarction, vascular dementia and Alzheimer's disease.
With an increasingly aging population, CCI is becoming a major
cause of disability and constitutes a large burden to healthcare
systems (34).
The MWM test performed in the present study showed a
significant increase in escape latency, swimming trajectory length
and a decreased frequency of passing through the target quadrant in
the saline-treated animals 8 weeks after the 2VO procedure compared
with the sham-operated group, which suggested that a CCI model was
successfully established in the present study. Furthermore, these
cognitive impairments were significantly improved in response to
rhEPO administration compared with the 2VO + saline treatment
group, which suggested a protective role of rhEPO against neuronal
damage in CCI. The hippocampus is an important region of the brain
that governs spatial learning and memory (26). Hippocampal neuronal damage and
thinning of the cerebral cortex in response to hypoxia are possible
mechanisms underlying cognitive and abnormal dysfunction in CCI. In
the present study, it was found that the neurons in the cortex and
hippocampus CA1 region exhibited morphological changes and the
overall number of neurons was significantly reduced in the 2VO +
saline group compared with those observed in the sham group, which
is consistent with previous studies (17). Importantly, these pathological
alterations were noticeably reversed in the rhEPO-treated rats
compared with the saline-treated ones, further confirming that
rhEPO may alleviate neuronal damage in CCI.
Ocular ischemic syndrome commonly occurs in the
elderly, and is typically a local manifestation of internal
diseases, such as high blood pressure, arteriosclerosis and
diabetes (35). The ophthalmic
artery is the first branch of the internal carotid artery (36). Thus, internal carotid artery
occlusion may lead to retina ischemia. It has previously been
reported that ocular ischemic syndrome is an early sign of cerebral
ischemia and the occurrence between retinal and brain ischemia is
significantly positively correlated (35). Retinal damage induces visual function
impairment, which contributes to deteriorated spatial learning
ability (24,25). Indeed, the present results showed
that the latency and amplitude of the P1 wave were significantly
increased and decreased, respectively, in the saline-treated CCI
rats compared with those in the sham-operated group, which suggests
that CCI may induce visual dysfunction in rats. Intriguingly, rhEPO
treatment restored some visual function in CCI rats as evidenced by
significantly reduced latency and elevated amplitude of P1 wave
compared with 2VO + saline, which at least partially contributed to
improvement of spatial learning ability in these rats. Consistent
results were observed in the changes in the thickness of retina and
the number of retinal ganglion cells. These data collectively
suggested a potential protective role of rhEPO against retinal
damage in rats with CCI.
Results from the present study suggested that
intranasally delivered rhEPO may attenuate cognitive and visual
impairments in 2VO-induced CCI in rats possibly through protecting
the cerebral cortex and retina from thinning, and preventing losses
of neurons and retinal ganglion cells. These data indicated that
intranasal administration of rhEPO may be a potential therapeutic
approach in CCI treatment. Further studies are required to reveal
the molecular mechanism of rhEPO in CCI therapy.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
YZ and BS conceived and supervised the study, YZ
designed and performed the experiments. JG made substantial
contributions to the conception of the study and provided new tools
and reagents. GZ developed new software and performed the
simulations. YZ analyzed data and wrote the manuscript. YZ, BS and
JG revised the manuscript. All authors reviewed the results and
approved the final manuscript.
Ethics approval and consent to
participate
All the experimental procedures were approved by the
Animal Use and Care Committee in Shanxi Medical University
(Taiyuan, China). All animal experiments were performed in
accordance with the guidelines for Animal Use and Care of Shanxi
Medical University (Taiyuan, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Miller JL, Church TJ, Leonoudakis D,
Lariosa-Willingham K, Frigon NL, Tettenborn CS, Spencer JR and
Punnonen J: Discovery and characterization of nonpeptidyl agonists
of the tissue-protective erythropoietin receptor. Mol Pharmacol.
88:357–367. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Rainville N, Jachimowicz E and Wojchowski
DM: Targeting EPO and EPO receptor pathways in anemia and
dysregulated erythropoiesis. Expert Opin Ther Targets. 20:287–301.
2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Miller JL, Rai M, Frigon NL, Pandolfo M,
Punnonen J and Spencer JR: Erythropoietin and small molecule
agonists of the tissue-protective erythropoietin receptor increase
FXN expression in neuronal cells in vitro and in Fxn-deficient KIKO
mice in vivo. Neuropharmacology. 123:34–45. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wang L, Wang X, Su H, Han Z, Yu H, Wang D,
Jiang R, Liu Z and Zhang J: Recombinant human erythropoietin
improves the neurofunctional recovery of rats following traumatic
brain injury via an increase in circulating endothelial progenitor
cells. Transl Stroke Res. 6:50–59. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ren Q, Zhang XF and Yang JY:
Erythropoietin reduces white matter damage in two-day-old rats
exposed to hypoxic/ischemia injury. Neurol Res. 38:1020–1026.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zhang F, Xing J, Liou AK, Wang S, Gan Y,
Luo Y, Ji X, Stetler RA, Chen J and Cao G: Enhanced delivery of
erythropoietin across the blood-brain barrier for neuroprotection
against ischemic neuronal injury. Transl Stroke Res. 1:113–121.
2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Brines M and Cerami A: Emerging biological
roles for erythropoietin in the nervous system. Nat Rev Neurosci.
6:484–494. 2005.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
Wolf RF, Peng J, Friese P, Gilmore LS,
Burstein SA and Dale GL: Erythropoietin administration increases
production and reactivity of platelets in dogs. Thromb Haemost.
78:1505–1509. 1997.PubMed/NCBI
|
|
9
|
Wiessner C, Allegrini PR, Ekatodramis D,
Jewell UR, Stallmach T and Gassmann M: Increased cerebral infarct
volumes in polyglobulic mice overexpressing erythropoietin. J Cereb
Blood Flow Metab. 21:857–864. 2001.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Leyland-Jones B, Investigators B and Study
G: Breast cancer trial with erythropoietin terminated unexpectedly.
Lancet Oncol. 4:459–460. 2003.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wun T, Law L, Harvey D, Sieracki B,
Scudder SA and Ryu JK: Increased incidence of symptomatic venous
thrombosis in patients with cervical carcinoma treated with
concurrent chemotherapy, radiation, and erythropoietin. Cancer.
98:1514–1520. 2003.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sadamoto Y, Igase K, Sakanaka M, Sato K,
Otsuka H, Sakaki S, Masuda S and Sasaki R: Erythropoietin prevents
place navigation disability and cortical infarction in rats with
permanent occlusion of the middle cerebral artery. Biochem Biophys
Res Commun. 253:26–32. 1998.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sakanaka M, Wen TC, Matsuda S, Masuda S,
Morishita E, Nagao M and Sasaki R: In vivo evidence that
erythropoietin protects neurons from ischemic damage. Proc Natl
Acad Sci USA. 95:4635–4640. 1998.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bernaudin M, Marti HH, Roussel S, Divoux
D, Nouvelot A, MacKenzie ET and Petit E: A potential role for
erythropoietin in focal permanent cerebral ischemia in mice. J
Cereb Blood Flow Metab. 19:643–651. 1999.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Alcalá-Barraza SR, Lee MS, Hanson LR,
McDonald AA, Frey WH II and McLoon LK: Intranasal delivery of
neurotrophic factors BDNF, CNTF, EPO, and NT-4 to the CNS. J Drug
Target. 18:179–190. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chauhan MB and Chauhan NB: Brain Uptake of
neurotherapeutics after intranasal versus intraperitoneal delivery
in Mice. J Neurol Neurosurg. 2(009)2015.PubMed/NCBI
|
|
17
|
Zhang T, Gu J, Wu L, Li N, Sun Y, Yu P,
Wang Y, Zhang G and Zhang Z: Neuroprotective and axonal
outgrowth-promoting effects of tetramethylpyrazine nitrone in
chronic cerebral hypoperfusion rats and primary hippocampal neurons
exposed to hypoxia. Neuropharmacology. 118:137–147. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Merelli A, Caltana L, Girimonti P, Ramos
AJ, Lazarowski A and Brusco A: Recovery of motor spontaneous
activity after intranasal delivery of human recombinant
erythropoietin in a focal brain hypoxia model induced by CoCl2 in
rats. Neurotox Res. 20:182–192. 2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Patil SS, Sunyer B, Höger H and Lubec G:
Evaluation of spatial memory of C57BL/6J and CD1 mice in the Barnes
maze, the Multiple T-maze and in the Morris water maze. Behav Brain
Res. 198:58–68. 2009.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Miskowiak KW, Vinberg M, Macoveanu J,
Ehrenreich H, Køster N, Inkster B, Paulson OB, Kessing LV,
Skimminge A and Siebner HR: Effects of erythropoietin on
hippocampal volume and memory in mood disorders. Biol Psychiatry.
78:270–277. 2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Holmes MD and Sires BS: Flash visual
evoked potentials predict visual outcome in traumatic optic
neuropathy. Ophthalmic Plast Reconstr Surg. 20:342–346.
2004.PubMed/NCBI View Article : Google Scholar
|
|
22
|
R Core Team. R: A language and environment
for statistical computing. R Foundation for Statistical Computing,
Vienna, Austria, 2012. ISBN 3-900051-07-0, URL http://www.R-project.org/.
|
|
23
|
R-Studio Team. R-Studio: Integrated
Development for R. RStudio, Inc., Boston MA, 2015. URL http://www.rstudio.com/.
|
|
24
|
Brown RE and Wong AA: The influence of
visual ability on learning and memory performance in 13 strains of
mice. Learn Mem. 14:134–144. 2007.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kaur C, Foulds WS and Ling EA:
Hypoxia-ischemia and retinal ganglion cell damage. Clin Ophthalmol.
2:879–889. 2008.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Bartsch T, Döhring J, Rohr A, Jansen O and
Deuschl G: CA1 neurons in the human hippocampus are critical for
autobiographical memory, mental time travel, and autonoetic
consciousness. Proc Natl Acad Sci USA. 108:17562–17567.
2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Hu MC, Shi M, Cho HJ, Zhang J, Pavlenco A,
Liu S, Sidhu S, Huang LJ and Moe OW: The erythropoietin receptor is
a downstream effector of Klotho-induced cytoprotection. Kidney Int.
84:468–481. 2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Lourhmati A, Buniatian GH, Paul C,
Verleysdonk S, Buecheler R, Buadze M, Proksch B, Schwab M, Gleiter
CH and Danielyan L: Age-dependent astroglial vulnerability to
hypoxia and glutamate: The role for erythropoietin. PLoS One.
8(e77182)2013.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Alnaeeli M, Raaka BM, Gavrilova O, Teng R,
Chanturiya T and Noguchi CT: Erythropoietin signaling: A novel
regulator of white adipose tissue inflammation during diet-induced
obesity. Diabetes. 63:2415–2431. 2014.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Vinberg M, Weikop P, Olsen NV, Kessing LV
and Miskowiak K: Effect of recombinant erythropoietin on
inflammatory markers in patients with affective disorders: A
randomised controlled study. Brain Behav Immun. 57:53–57.
2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Ardalan MR, Estakhri R, Hajipour B,
Ansarin K, Asl NA, Nasirizade MR, Azar AN, Ghorbanihaghjou A,
Vatankhah AM and Esmaili HA: Erythropoietin ameliorates oxidative
stress and tissue injury following renal ischemia/reperfusion in
rat kidney and lung. Med Princ Pract. 22:70–74. 2013.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Yu YP, Xu QQ, Zhang Q, Zhang WP, Zhang LH
and Wei EQ: Intranasal recombinant human erythropoietin protects
rats against focal cerebral ischemia. Neurosci Lett. 387:5–10.
2005.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Fletcher L, Kohli S, Sprague SM, Scranton
RA, Lipton SA, Parra A, Jimenez DF and Digicaylioglu M: Intranasal
delivery of erythropoietin plus insulin-like growth factor-I for
acute neuroprotection in stroke. Laboratory investigation. J
Neurosurg. 111:164–170. 2009.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Zhu S, Min D, Zeng J, Ju Y, Liu Y and Chen
X: Transplantation of Stem Cells from human exfoliated deciduous
teeth decreases cognitive impairment from chronic cerebral ischemia
by reducing neuronal apoptosis in rats. J Stem Cells Int.
2020(6393075)2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Masuda T, Shimazawa M, Ishizuka F,
Nakamura S, Tsuruma K and Hara H: Tissue kallikrein
(kallidinogenase) protects against retinal ischemic damage in mice.
Eur J Pharmacol. 738:74–82. 2014.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Bird B and Stawicki SP: Anatomy, head and
neck, ophthalmic arteries. In: StatPearls. Treasure Island (FL),
2019.
|