Cardiovascular disease (CVD) and hypertension have
emerged as critical comorbid risk factors affecting the survival of
patients with COVID-19(1).
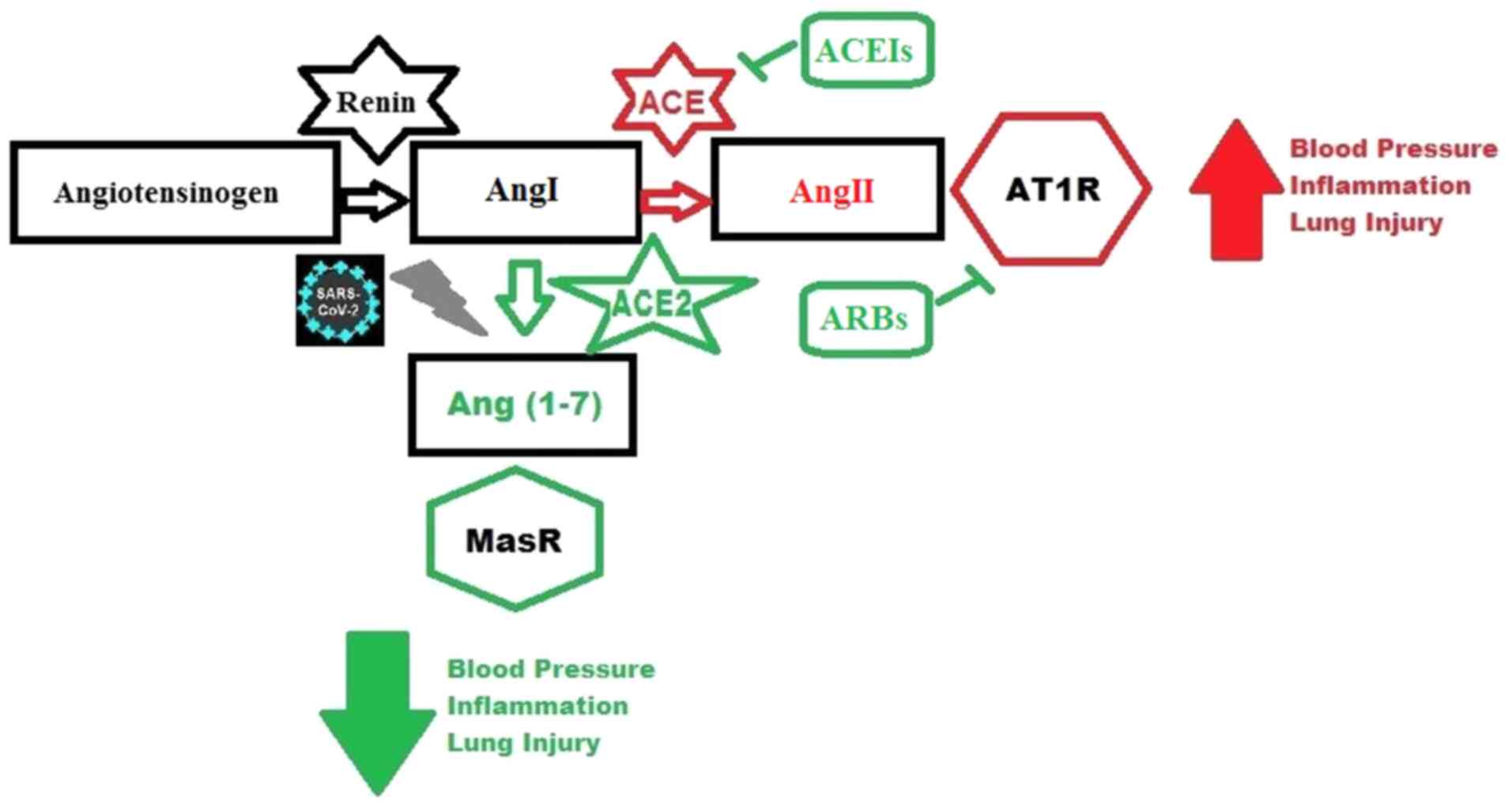
Inflammation is a major player in the progression of CVD, and the
renin-angiotensin-aldosterone system (RAAS) plays an important role
in producing and maintaining vascular inflammation (2). While RAAS serves a key role in
regulating blood pressure and hypertension, it also mediates
pro-inflammatory functions. Most importantly, blocking RAAS has
beneficial and protective outcomes in CVD treatment. Indeed, the
use of major RAAS inhibitors, such as angiotensin receptor blockers
(ARBs) and angiotensin-converting enzyme inhibitors (ACEIs)
improves CVD by effectively treating hypertension-induced injury
(3). Angiotensin-converting enzyme
2 (ACE2) is a major component of RAAS, and the receptor to which
SARS-CoV2 binds to enter the cells. Endothelial cell dysfunction
(ED) driven-ACE2 depletion is associated with an increase in
inflammation and blood coagulation; both are considered critical
factors in the progression of COVID-19. To date, this association
remains unclear and thus, there should be an increased effort to
better understand the relationship between ACE2, blood hemostasis
and inflammation in the pathogenesis of COVID-19 disease.
In CVD, chronic inflammation leads to ED and the
initiation and progression of atherosclerosis by enhancing the
migration of inflammatory cells into the vessel wall, foam cell
formation and the stimulation of smooth muscle cell hyperplasia,
which ultimately leads to tissue injury (4). Strong associations between Angiotensin
II (AngII), a major actor in RAAS, and inflammation have been
demonstrated, implicating AngII in enhancing pro-inflammatory
responses through the upregulation of pro-inflammatory cytokines
and chemokines, including IL-6, MCP-1, VCAM-1 and TNF-α (5-8).
In addition, AngII is a strong pro-oxidant and it mediates its
effects through the activation of NADH/NADPH signaling, production
of superoxide anions and reduction in nitric oxide (NO)
bioavailability, which is a key marker for a healthy endothelium
(9-12).
ACE2 is the target receptor to which SARS-CoV-2
binds with to gain entry into cells (1). Since ACE2 is an essential component of
RAAS, concerns arise regarding the plausible relationships between
hypertension, the use of ACEIs and ARBs, and the role of
cardiovascular disease in aggravating COVID-19 symptoms, restoring
the balance in the RAAS system may be a critical factor in
attenuating organ injuries. Indeed, this was addressed early during
the COVID-19 pandemic; drugs that block RAAS could affect the
severity of the disease (15).
Results from the initial outbreak in China showed that a majority
of patients with COVID-19 with severe symptoms had hypertension;
this led to speculations that ACEIs and ARBs may increase the risk
of viral infection since their administration enhances ACE2
expression (16,17). However, studies in humans and animal
models did not provide any convincing proof of this association,
and thus remains unclear and contested (18-20).
Adding to this controversy is the fact that the virus-binding
target, ACE2, converts AngII to Ang(1-7),
which decreases inflammation and lowers blood pressure. ACE2
therefore plays an important role in balancing the two RAAS arms,
the pro-inflammatory and hypertensive arm mediated by ACE, AngII
and Angiotensin Type 1 Receptor (AT1R), and the cardioprotective,
anti-inflammatory arm mediated by MAS1 oncogene (MasR) and AT2R.
Disruption of this balance is a crucial player in the
pathophysiology of CVD and COVID-19(21). Indeed, while the ACE/AngII pathway
is important in vasoconstriction, hypertension and oxidative
stress, which leads to inflammation, the ACE2/Ang(1-7)
pathway counteracts the above effects, and both pathways coexist in
various tissues including in the lungs, heart, blood vessels and
kidneys where they regulate blood pressure and contribute to CVD
pathophysiology (22,23).
The SARS-CoV-2 spike protein recognizes, with high
affinity, ACE2 present on the surface of host cells mediating the
entry of the virus. Endocytosis of the virus-ACE2 complex can
potentially lead to ACE2 downregulation and shedding from the
surface of the cell (24). This
loss of ACE2 function in infected cells could be a critical factor
in the progression and course of the disease (25). Even though there is no compelling
evidence that links ACEI and ARB treatment with an increase in
SARS-CoV-2 infection, it is becoming evident that these drugs may
attenuate AngII-driven lung injury (26). Since AngII promotes inflammation and
acute lung injury (27), any
increase in ACE2 activity could reduce AngII concentration in the
lungs and mitigate virus-driven lung injury. Indeed, a recent study
revealed correlations between biochemical and clinical markers of
lung injury, viral load and AngII concentrations in patients with
COVID-19(28). Similarly, results
link SARS-CoV-2 with a decrease in ACE2 expression and acute heart
injury (29). However, it was
reported that the use of ACEIs or ARBs in hospitalized patients
with COVID-19 had no effect on their survival rate; actually, there
was no significant difference in the mean number of days alive for
patients who were hospitalized with mild to moderate symptoms of
COVID-19 and who were assigned to continue vs. discontinue these
medications (30). Conversely,
another cohort study that assessed ACEIs and ARBs and included more
than 8 million individuals, has shown that these drugs are
associated with significantly reduced severe risks of the disease,
such as requiring intensive care. This study also hinted to the
role of ethnicity in modulating ACEIs/ARBs effects in relation to
the severity of the disease; it was shown that the risk of the
disease in association with the use of these drugs was higher in
Black African and Caribbean groups when compared with the Caucasian
group (31). Overall, the use of
ACEIs/ARBs is still a paradoxical issue that requires extended
investigation to resolve; it is also an area of research where the
benefit/risk analysis and potential efficacy of those drugs should
be addressed in connection with other comorbidities that are
related to COVID-19(22).
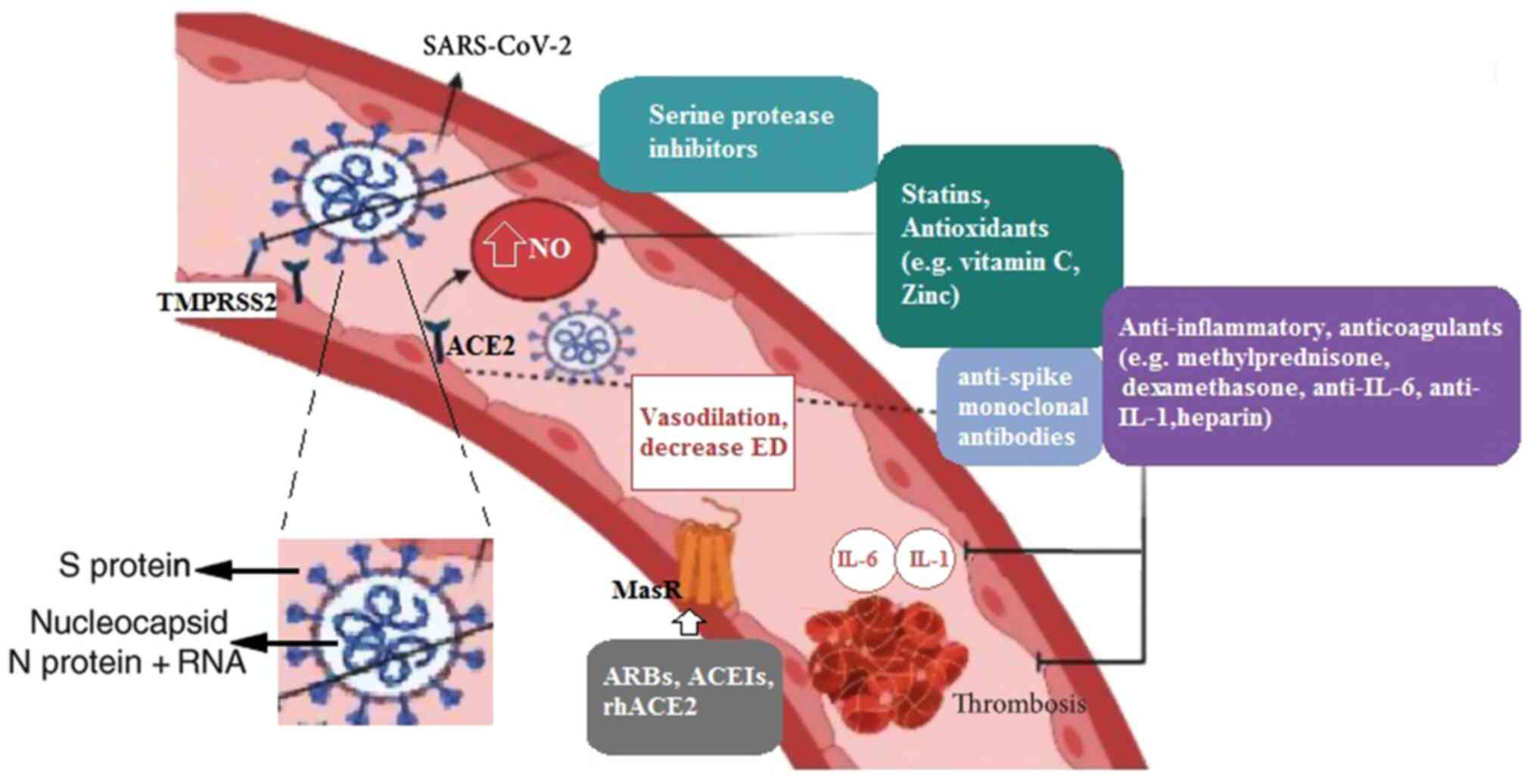
There is growing evidence for COVID-19 being a
disorder of blood clotting where the virus uses the respiratory
route to gain entry to blood circulation (32). It has been initially reported that
COVID-19 is strongly associated with ischemic strokes in patients
that required vacuum and clot retrieval devices as well as blood
thinning medications (33,34). It was shown that when the virus
enters the blood stream, it triggers a cascade of events resulting
in blood clotting and strokes. This all starts with the attachment
of the virus to the ACE2 receptor on endothelial cells, making use
of transmembrane protease, serine-2 (TMPRSS-2) which initiates the
process of ED (35). Thus,
SARS-CoV-2 mediated ACE2 downregulation on the surface of the cell
results in AngII accumulation and NADPH activation fueling the
generation of reactive oxygen species (ROS) and thus increasing
oxidative stress (36,37). ROS assists in the conversion of
β2-glycoprotein 1 into its oxidized form, which can no longer bind
competitively to the von Willebrand factor (vWF) that is secreted
by dysfunctional endothelial cells; subsequently, this will promote
the coagulation cascade, as vWF binds to the sub-endothelial layer,
crosslinking collagen and platelets together and accentuating
coagulation mechanisms that lead to strokes of the large vessels
(38,39).
During viral infection, the dysfunctional
endothelium plays a detrimental role by worsening inflammation
which is associated with a poor prognosis in patients with COVID-19
(Fig. 2) (35). As the coagulation mechanism is a
highly organized process that involves endothelial cells,
endotheliitis plays a critical role in the pathogenesis of
SARS-CoV-2 by increasing the risk of excessive and disseminated
intravascular coagulation and the rates of fatality (40). During infection, pro-inflammatory
cytokines, such as IL-1β, IL-6 and TNF-α are amplified and lead to
a simultaneous increase in the vWF and tissue factor release from
endothelial cells, which will promote blood clotting through the
increase in platelet aggregation and the initiation of the clotting
cascade (41). Similarly, those
cytokines enhance blood clotting by downregulating pro-fibrinolytic
and anticoagulant factors, including endothelial protein C receptor
and thrombomodulin and by upregulating anti-fibrinolytic factors,
namely plasminogen activator inhibitor-1 (PAI-1) (42,43).
There is cumulative proof that ACE2 downregulation may contribute
to an increase in the thrombotic risk in patients with
COVID-19(44). It has been
speculated that the decrease in ACE2 activity seen in patients with
COVID-19 may lead to a series of mechanisms that are promoted by
the dysfunctional endothelium and that affect blood hemostasis.
This comprises an increase in vascular permeability, as well as an
upregulation of tissue factor and PAI-1 culminating in the
activation of the extrinsic coagulation pathway and the reduction
in fibrinolysis (45). On this same
note, it has been reported that, in animal models of thrombosis,
there is a clear association between coagulation and ACE2 pathways.
In rats with an induced thrombosis, ACE2 inhibition is
significantly correlated with the increase in blood clot weight;
conversely, ACE2 administration induced a decrease in thrombus size
as well as a reduction in platelet adhesion to the endothelium
(46). Similarly, it has been shown
that a decrease in ACE2 activity is associated with an increase in
blood coagulation in spontaneous hypertensive rats, and that the
activation of ACE2 attenuates thrombosis by reducing the attachment
of platelets to the vessel wall (47).
Interestingly, it was reported that SARS-CoV-2 can
directly bind to platelets through its spike protein, which will
enhance platelet activation. It was shown that platelets are
hyperactive in patients with COVID-19 and that they express ACE2
and TMPRSS2. ACE2-mediated viral binding to platelets stimulated
them to release inflammatory and coagulation factors, which lead to
an enhancement in leukocyte-platelet aggregation (48).
At present, the treatment of COVID-19 is limited to
alleviating the symptoms of the disease, with no specific antiviral
drugs that are effective in targeting the virus (49). Accordingly, there exist numerous
ongoing clinical trials and treatments that aim to target
COVID-19-associated ED in order to mitigate disease progression and
the high mortality rate associated with it. Such treatments include
the use of RAAS inhibitors, serine protease inhibitors, recombinant
human ACE2, monoclonal anti-spike antibodies, heparin,
corticosteroids as well as other agents directed towards specific
cytokines and inflammatory signaling pathways (Fig. 3) (50-54).
Serine protease inhibitors may affect SARS-CoV-2 entry to the cell
by inhibiting TMPRSS-2, which plays an instrumental role in
mediating S protein fusion to the endothelial cell membrane
(49). One study showed that
targeting TMPRSS2 using a clinically proven protease inhibitor can
effectively prevent SARS-CoV-2 infection in vitro (25). Additionally, numerous studies and
ongoing clinical trials point to the vital role that the RAAS
inhibitors may contribute to improving ED and the pathogenesis of
COVID-19 (55-59).
On this same note, statins were also reported to improve
endothelial cell function in a manner distinct from their major
lipid-lowering activities. These drugs can increase the expression
of NO synthase, whilst inhibiting NADPH oxidase, which leads to the
suppression of pro-inflammatory pathways in endothelial cells
(60). Meanwhile, there is a
growing evidence showing that statins can improve the prognosis of
COVID-19 through the decrease in the production of inflammatory
biomarkers (61). In addition,
heparin is known to have anti-inflammatory and protective effects
in endothelial cells, and recent studies confirmed its role in
improving the prognosis of severely infected patients and reducing
mortality rates through its well-known anticoagulation properties
(62). Furthermore, given the
importance of inflammation in the pathophysiology of COVID-19,
clinical evaluation of the anti-inflammatory effects of
corticosteroids has gained high priority recently. One study has
shown the efficacy of methylprednisone in treating severely ill
patients with acute respiratory distress syndrome (63). Another study also confirmed the
significant role of dexamethasone in decreasing mortality rates in
patients who are severely affected with COVID-19(64). Lastly, other promising therapeutic
approaches include targeting cytokines, such as interferon-γ, IL-1
and IL-6 and, as well as the VEGFA/VEGFR2 signaling pathways in
order to alleviate virus-driven injury and inflammation (54).
Overall, ACE2 is a key player in SARS-CoV-2
infection and in abrogating the detrimental effects of the
ACE/AngII/AT1R arm of RAAS; namely, the ACE2/Ang(1-7)
pathway instigates a shift away from ACE/AngII/AT1R, which affects
the progression of COVID-19 symptoms. Moreover, there is a clear
association linking ACE2 and blood coagulation pathways, which
could play an important role in COVID-19. This relationship
suggests that ACE2 may be a novel target for the treatment of
thrombogenic diseases, including COVID-19. Future investigations
into the role of ACEIs and ARBs in this disease shall expose their
potential value for managing COVID-19 symptoms. In addition, there
is an urgent need to better understand the effect of recombinant
human ACE2 as a potential treatment for SARS-CoV-2 driven injury.
Equally important is the need to define the promising role of
anti-Spike monoclonal antibodies in alleviating COVID-19 symptoms
by reversing SARS-CoV-2 spike protein-induced platelet activation,
excessive coagulation and the rates of strokes and fatalities.
Future research shall hopefully address these issues as there
remain significant gaps in our knowledge pertaining to these
related subjects. Accordingly, it is extremely essential that
future clinical practice deals with the precise therapeutic
processes pertaining to the action of anti-spike monoclonal
antibodies and recombinant human ACE2 as fully integrated subjects
of high priority. This should help scientists in confirming and
verifying the efficacy of those recommended therapeutic strategies
in well-designed clinical trials since, as to date, the
pathogenesis of COVID-19 is still a vaguely understood subject.
Shedding more light onto ED in clinical practice may be more
significant than we expect; in this context, a collaborative effort
of biomedical and clinical science is urgently required, as this
will assist in completing our understanding of the paradigm of the
pathogenesis of COVID-19, and in translating our current
understanding of the disease to successful treatment
strategies.
The author would sincerely like to thank the
University of Balamand for their unbounded support.
No funding was received.
Not applicable.
JD wrote and revised the manuscript, and has read
and approved the final manuscript. Data authentication is not
applicable.
Not applicable.
Not applicable.
The author declares that he has no competing
interests.
|
1
|
South AM, Brady TM and Flynn JT: ACE2
(angiotensin-converting enzyme 2), COVID-19, and ACE inhibitor and
Ang II (angiotensin II) receptor blocker use during the pandemic:
The pediatric perspective. Hypertension. 76:16–22. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Pacurari M, Kafoury R, Tchounwou PB and
Ndebele K: The Renin-Angiotensin-aldosterone system in vascular
inflammation and remodeling. Int J Inflamm.
2014(689360)2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ferrario CM and Strawn WB: Role of the
renin-angiotensin-aldosterone system and proinflammatory mediators
in cardiovascular disease. Am J Cardiol. 98:121–128.
2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Daher J: Other forms of oxidized LDL:
Emerging functions. World Acad Sci J. 2:1. 2020.
|
|
5
|
Álvarez A, Cerdá-Nicolás M, Naim Abu Nabah
Y, Mata M, Issekutz AC, Panés J, Lobb RR and Sanz MJ: Direct
evidence of leukocyte adhesion in arterioles by angiotensin II.
Blood. 104:402–408. 2004.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kranzhöfer R, Schmidt J, Pfeiffer CA, Hagl
S, Libby P and Kübler W: Angiotensin induces inflammatory
activation of human vascular smooth muscle cells. Arterioscler
Thromb Vasc Biol. 19:1623–1629. 1999.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Hahn AW, Jonas U, Bühler FR and Resink TJ:
Activation of human peripheral monocytes by angiotensin II. FEBS
Lett. 347:178–180. 1994.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tummala PE, Chen X-L, Sundell CL, Laursen
JB, Hammes CP, Alexander RW, Harrison DG and Medford RM:
Angiotensin II induces vascular cell adhesion molecule-1 expression
in rat vasculature: A potential link between the renin-angiotensin
system and atherosclerosis. Circulation. 100:1223–1229.
1999.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Rajagopalan S, Kurz S, Münzel T, Tarpey M,
Freeman BA, Griendling KK and Harrison DG: Angiotensin II-mediated
hypertension in the rat increases vascular superoxide production
via membrane NADH/NADPH oxidase activation. Contribution to
alterations of vasomotor tone. J Clin Invest. 97:1916–1923.
1996.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wassmann S and Nickenig G:
Pathophysiological regulation of the AT1-receptor and implications
for vascular disease. J Hypertens Suppl. 24 (Suppl 1):S15–S21.
2006.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Judkins CP, Diep H, Broughton BRS, Mast
AE, Hooker EU, Miller AA, Selemidis S, Dusting GJ, Sobey CG and
Drummond GR: Direct evidence of a role for Nox2 in superoxide
production, reduced nitric oxide bioavailability, and early
atherosclerotic plaque formation in ApoE-/- mice. Am J
Physiol Heart Circ Physiol. 298:H24–H32. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Förstermann U and Münzel T: Endothelial
nitric oxide synthase in vascular disease: From marvel to menace.
Circulation. 113:1708–1714. 2006.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ferrari R: RAAS inhibition and mortality
in hypertension. Glob Cardiol Sci Pract. 2013:269–278.
2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mansur SJ, Hage FG and Oparil S: Have the
renin-angiotensin-aldosterone system perturbations in
cardiovascular disease been exhausted? Curr Cardiol Rep.
12:450–463. 2010.PubMed/NCBI View Article : Google Scholar
|
|
15
|
South AM, Tomlinson L, Edmonston D,
Hiremath S and Sparks MA: Controversies of renin-angiotensin system
inhibition during the COVID-19 pandemic. Nat Rev Nephrol.
16:305–307. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Fang L, Karakiulakis G and Roth M: Are
patients with hypertension and diabetes mellitus at increased risk
for COVID-19 infection? Lancet Respir Med. 8(e21)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ferrario CM, Jessup J, Chappell MC,
Averill DB, Brosnihan KB, Tallant EA, Diz DI and Gallagher PE:
Effect of angiotensin-converting enzyme inhibition and angiotensin
II receptor blockers on cardiac angiotensin-converting enzyme 2.
Circulation. 111:2605–2610. 2005.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Bean D, Kraljevic Z, Searle T, Bendayan R,
Pickles A, Folarin A, Roguski L, Noor K, Shek A, O'Gallagher K, et
al: Treatment with ACE-inhibitors is associated with less severe
disease with SARS-Covid-19 infection in a multi-site UK acute
Hospital Trust. medRxiv: Apr 11, 2020 (Epub ahead of print). doi:
https://doi.org/10.1101/2020.04.07.20056788.
|
|
19
|
Vaduganathan M, Vardeny O, Michel T,
McMurray JJ, Pfeffer MA and Solomon SD:
Renin-angiotensin-aldosterone system inhibitors in patients with
Covid-19. N Engl J Med. 382:1653–1659. 2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kuster GM, Pfister O, Burkard T, Zhou Q,
Twerenbold R, Haaf P, Widmer AF and Osswald S: SARS-CoV2: Should
inhibitors of the renin-angiotensin system be withdrawn in patients
with COVID-19? Eur Heart J. 41:1801–1803. 2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Simões E, Silva AC and Flynn JT: The
renin-angiotensin-aldosterone system in 2011: Role in hypertension
and chronic kidney disease. Pediatr Nephrol. 27:1835–1845.
2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
South AM, Shaltout HA, Washburn LK,
Hendricks AS, Diz DI and Chappell MC: Fetal programming and the
angiotensin-(1-7) axis: A review of the experimental and clinical
data. Clin Sci (Lond). 133:55–74. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Masi S, Uliana M and Virdis A: Angiotensin
II and vascular damage in hypertension: Role of oxidative stress
and sympathetic activation. Vascul Pharmacol. 115:13–17.
2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Wan Y, Shang J, Graham R, Baric RS and Li
F: Receptor recognition by novel coronavirus from Wuhan: An
analysis based on decade-long structural studies of SARS. J Virol.
94:e00127–e20. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Hoffmann M, Kleine-Weber H, Schroeder S,
Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH,
Nitsche A, et al: SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2
and is blocked by a clinically proven protease inhibitor. Cell.
181:271–280.e8. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Gu H, Xie Z, Li T, Zhang S, Lai C, Zhu P,
Wang K, Han L, Duan Y, Zhao Z, et al: Angiotensin-converting enzyme
2 inhibits lung injury induced by respiratory syncytial virus. Sci
Rep. 6(19840)2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Li X, Molina-Molina M, Abdul-Hafez A, Uhal
V, Xaubet A and Uhal BD: Angiotensin converting enzyme-2 is
protective but downregulated in human and experimental lung
fibrosis. Am J Physiol Lung Cell Mol Physiol. 295:L178–L185.
2008.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Liu Y, Yang Y, Zhang C, Huang F, Wang F,
Yuan J, Wang Z, Li J, Li J, Feng C, et al: Clinical and biochemical
indexes from 2019-nCoV infected patients linked to viral loads and
lung injury. Sci China Life Sci. 63:364–374. 2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Oudit GY, Kassiri Z, Jiang C, Liu PP,
Poutanen SM, Penninger JM and Butany J: SARS-coronavirus modulation
of myocardial ACE2 expression and inflammation in patients with
SARS. Eur J Clin Invest. 39:618–625. 2009.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Lopes RD, Macedo AVS, de Barros E Silva
PG, Moll-Bernardes RJ, Dos Santos TM, Mazza L, Feldman A, D'Andréa
Saba Arruda G, de Albuquerque DC, Camiletti AS, et al: BRACE CORONA
investigators: Effect of discontinuing vs. continuing
angiotensin-converting enzyme inhibitors and angiotensin ii
receptor blockers on days alive and out of the hospital in patients
admitted with COVID-19: A Randomized Clinical Trial. JAMA.
325:254–264. 2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Hippisley-Cox J, Young D, Coupland C,
Channon KM, Tan PS, Harrison DA, Rowan K, Aveyard P, Pavord ID and
Watkinson PJ: Risk of severe COVID-19 disease with ACE inhibitors
and angiotensin receptor blockers: Cohort study including 8.3
million people. Heart. 106:1503–1511. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Simko F and Baka T: Angiotensin-converting
enzyme inhibitors and angiotensin II receptor blockers: Potential
allies in the COVID-19 pandemic instead of a threat? Clin Sci
(Lond). 135:1009–1014. 2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Janardhan V, Janardhan V and Kalousek V:
COVID-19 as a blood clotting disorder masquerading as a respiratory
illness: a cerebrovascular perspective and therapeutic implications
for stroke thrombectomy. J Neuroimaging. 30:555–561.
2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Zhang Y, Xiao M, Zhang S, Xia P, Cao W,
Jiang W, Chen H, Ding X, Zhao H, Zhang H, et al: Coagulopathy and
antiphospholipid antibodies in patients with COVID-19. N Engl J
Med. 382(e38)2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Oxley TJ, Mocco J, Majidi S, Kellner CP,
Shoirah H, Singh IP, De Leacy RA, Shigematsu T, Ladner TR, Yaeger
KA, et al: Large-vessel stroke as a presenting feature of COVID-19
in the young. N Engl J Med. 382(e60)2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Varga Z, Flammer AJ, Steiger P, Haberecker
M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka
F and Moch H: Endothelial cell infection and endotheliitis in
COVID-19. Lancet. 395:1417–1418. 2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Hess DC, Eldahshan W and Rutkowski E:
COVID-19-related stroke. Transl Stroke Res. 11:322–325.
2020.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Garrido AM and Griendling KK: NADPH
oxidases and angiotensin II receptor signaling. Mol Cell
Endocrinol. 302:148–158. 2009.PubMed/NCBI View Article : Google Scholar
|
|
39
|
El-Assaad F, Krilis SA and Giannakopoulos
B: Posttranslational forms of beta 2-glycoprotein I in the
pathogenesis of the antiphospholipid syndrome. Thromb J. 14 (Suppl
1)(20)2016.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Ho YC, Ahuja KDK, Körner H and Adams MJ:
β2GP1, anti-β2GP1 antibodies and platelets: Key players in the
antiphospholipid syndrome. Antibodies (Basel).
5(E12)2016.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Han H, Yang L, Liu R, Liu F, Wu KL, Li J,
Liu XH and Zhu CL: Prominent changes in blood coagulation of
patients with SARS-CoV-2 infection. Clin Chem Lab Med.
58:1116–1120. 2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Wang J, Saguner AM, An J, Ning Y, Yan Y
and Li G: Dysfunctional coagulation in COVID-19: From cell to
bedside. Adv Ther. 37:3033–3039. 2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Gong J, Dong H, Xia SQ, Huang ZY, Wang DK,
Zhao Y, Liu WH, Tu SH, Zhang MM, Wang Q, et al: Correlation
analysis between disease severity and inflammation-related
parameters in patients with COVID-19: a retrospective study. BMC
Infect Dis. 20(963)2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Lipinski S, Bremer L, Lammers T, Thieme F,
Schreiber S and Rosenstiel P: Coagulation and inflammation.
Molecular insights and diagnostic implications. Hamostaseologie.
31:94–102, 104. 2011.PubMed/NCBI View
Article : Google Scholar
|
|
45
|
Lupi L, Adamo M, Inciardi RM and Metra M:
ACE2 down-regulation may contribute to the increased thrombotic
risk in COVID-19. Eur Heart J. 41(3200)2020.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Mehrabadi ME, Hemmati R, Tashakor A,
Homaei A, Yousefzadeh M, Hemati K and Hosseinkhani S: Induced
dysregulation of ACE2 by SARS-CoV-2 plays a key role in COVID-19
severity. Biomed Pharmacother. 137(111363)2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Fraga-Silva RA, Sorg BS, Wankhede M,
Dedeugd C, Jun JY, Baker MB, Li Y, Castellano RK, Katovich MJ,
Raizada MK, et al: ACE2 activation promotes antithrombotic
activity. Mol Med. 16:210–215. 2010.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Zhang S, Liu Y, Wang X, Yang L, Li H, Wang
Y, Liu M, Zhao X, Xie Y, Yang Y, et al: SARS-CoV-2 binds platelet
ACE2 to enhance thrombosis in COVID-19. J Hematol Oncol.
13(120)2020.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Deng H, Tang TX, Chen D, Tang LS, Yang XP
and Tang ZH: Endothelial dysfunction and SARS-CoV-2 infection:
Association and therapeutic strategies. Pathogens.
10(582)2021.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Libby P and Lüscher T: COVID-19 is, in the
end, an endothelial disease. Eur Heart J. 41:3038–3044.
2020.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Batlle D, Wysocki J and Satchell K:
Soluble angiotensin-converting enzyme 2: A potential approach for
coronavirus infection therapy? Clin Sci (Lond). 134:543–545.
2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Jahanshahlu L and Rezaei N: Monoclonal
antibody as a potential anti-COVID-19. Biomed Pharmacother.
129(110337)2020.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Fodor A, Tiperciuc B, Login C, Orasan OH,
Lazar AL, Buchman C, Hanghicel P, Sitar-Taut A, Suharoschi R,
Vulturar R, et al: Endothelial dysfunction, inflammation, and
oxidative stress in COVID-19-mechanisms and therapeutic targets.
Oxid Med Cell Longev. 2021(8671713)2021.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Jin Y, Ji W, Yang H, Chen S, Zhang W and
Duan G: Endothelial activation and dysfunction in COVID-19: From
basic mechanisms to potential therapeutic approaches. Signal
Transduct Target Ther. 5(293)2020.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Shahin Y, Khan JA, Samuel N and Chetter I:
Angiotensin converting enzyme inhibitors effect on endothelial
dysfunction: A meta-analysis of randomised controlled trials.
Atherosclerosis. 216:7–16. 2011.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Reynolds HR, Adhikari S, Pulgarin C,
Troxel AB, Iturrate E, Johnson SB, Hausvater A, Newman JD, Berger
JS, Bangalore S, et al: Renin-angiotensin-Aldosterone system
inhibitors and risk of covid-19. N Engl J Med. 382:2441–2448.
2020.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Fosbøl EL, Butt JH, Østergaard L,
Andersson C, Selmer C, Kragholm K, Schou M, Phelps M, Gislason GH,
Gerds TA, et al: Association of angiotensin-converting enzyme
inhibitor or angiotensin receptor blocker use with COVID-19
diagnosis and mortality. JAMA. 324:168–177. 2020.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Flacco ME, Acuti Martellucci C, Bravi F,
Parruti G, Cappadona R, Mascitelli A, Manfredini R, Mantovani LG
and Manzoli L: Treatment with ACE inhibitors or ARBs and risk of
severe/lethal COVID-19: A meta-analysis. Heart. 106:1519–1524.
2020.PubMed/NCBI View Article : Google Scholar
|
|
59
|
De Spiegeleer A, Bronselaer A, Teo JT,
Byttebier G, De Tré G, Belmans L, Dobson R, Wynendaele E, Van De
Wiele C, Vandaele F, et al: The effects of ARBs, ACEis, and statins
on clinical outcomes of COVID-19 infection among nursing home
residents. J Am Med Dir Assoc. 21:909–914.e2. 2020.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Reriani MK, Dunlay SM, Gupta B, West CP,
Rihal CS, Lerman LO and Lerman A: Effects of statins on coronary
and peripheral endothelial function in humans: A systematic review
and meta-analysis of randomized controlled trials. Eur J Cardiovasc
Prev Rehabil. 18:704–716. 2011.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Nägele MP, Haubner B, Tanner FC,
Ruschitzka F and Flammer AJ: Endothelial dysfunction in COVID-19:
Current findings and therapeutic implications. Atherosclerosis.
314:58–62. 2020.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Ayerbe L, Risco C and Ayis S: The
association between treatment with heparin and survival in patients
with Covid-19. J Thromb Thrombolysis. 50:298–301. 2020.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S,
Huang H, Zhang L, Zhou X, Du C, et al: Risk factors associated with
acute respiratory distress syndrome and death in patients with
coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern
Med. 180:934–943. 2020.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Horby P, Lim WS, Emberson JR, Mafham M,
Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi
E, et al: RECOVERY Collaborative Group: Dexamethasone in
hospitalized patients with Covid-19. N Engl J Med. 384:693–704.
2021.PubMed/NCBI View Article : Google Scholar
|