|
1
|
Damhuis SE, Ganzevoort W and Gordijn SJ:
Abnormal fetal growth: small for gestational age, fetal growth
restriction, large for gestational age: Definitions and
epidemiology. Obstet Gynecol Clin North Am. 48:267–279.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
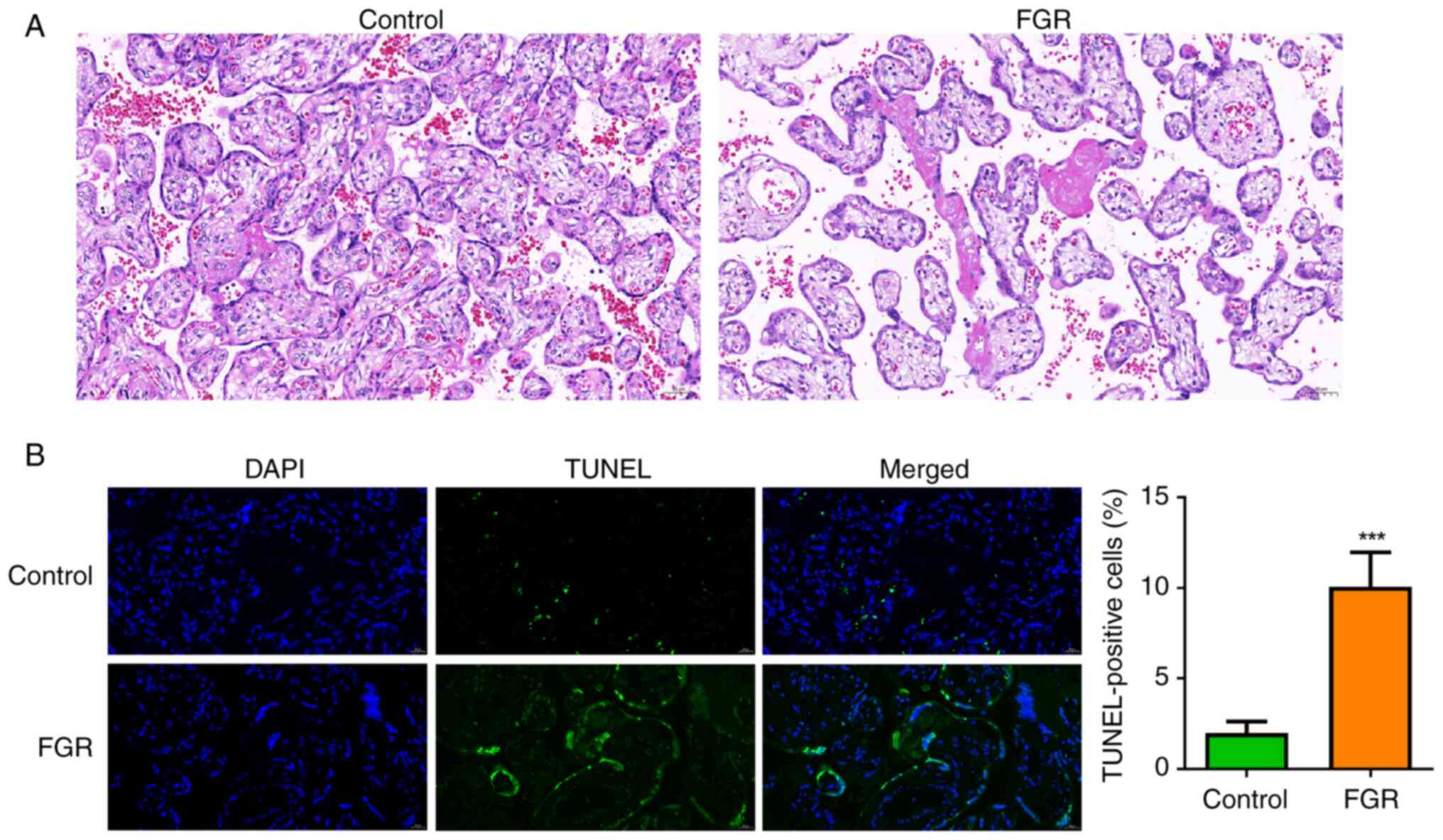
Gupta N and Khajuria A: Histomorphological
features of placenta in pregnancy complicated with intrauterine
growth retardation. JK Sci. 18:21–25. 2016.
|
|
3
|
Nardozza LMM, Caetano ACR, Zamarian ACP,
Mazzola JB, Silva CP, Marçal VMG, Lobo TF, Peixoto AB and Araujo
Júnior E: Fetal growth restriction: Current knowledge. Arch Gynecol
Obstet. 295:1061–1077. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Turner S, Posthumus AG, Steegers EAP,
AlMakoshi A, Sallout B, Rifas-Shiman SL, Oken E, Kumwenda B,
Alostad F, Wright-Corker C, et al: Household income, fetal size and
birth weight: An analysis of eight populations. J Epidemiol
Community Health. 76:629–636. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
González-Fernández D, Muralidharan O,
Neves PA and Bhutta ZA: Associations of maternal nutritional status
and supplementation with fetal, newborn, and infant outcomes in
low-income and middle-income settings: An overview of reviews.
Nutrients. 16(3725)2024.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Dudink I, Hüppi PS, Sizonenko SV,
Castillo-Melendez M, Sutherland AE, Allison BJ and Miller SL:
Altered trajectory of neurodevelopment associated with fetal growth
restriction. Exp Neurol. 347(113885)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Della Gatta AN, Aceti A, Spinedi SF,
Martini S, Corvaglia L, Sansavini A, Zuccarini M, Lenzi J,
Seidenari A, Dionisi C, et al: Neurodevelopmental outcomes of very
preterm infants born following early foetal growth restriction with
absent end-diastolic umbilical flow. Eur J Pediatr. 182:4467–4476.
2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rock CR, White TA, Piscopo BR, Sutherland
AE, Miller SL, Camm EJ and Allison BJ: Cardiovascular and
cerebrovascular implications of growth restriction: Mechanisms and
potential treatments. Int J Mol Sci. 22(7555)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Bezemer RE, Schoots MH, Timmer A, Scherjon
SA, Erwich JJHM, van Goor H, Gordijn SJ and Prins JR: Altered
levels of decidual immune cell subsets in fetal growth restriction,
stillbirth, and placental pathology. Front Immunol.
11(1898)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Muskavitch MA: Delta-notch signaling and
Drosophila cell fate choice. Dev Biol. 166:415–430. 1994.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Siebel C and Lendahl U: Notch signaling in
development, tissue homeostasis, and disease. Physiol Rev.
97:1235–1294. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kopan R and Ilagan MX: The canonical Notch
signaling pathway: Unfolding the activation mechanism. Cell.
137:216–233. 2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
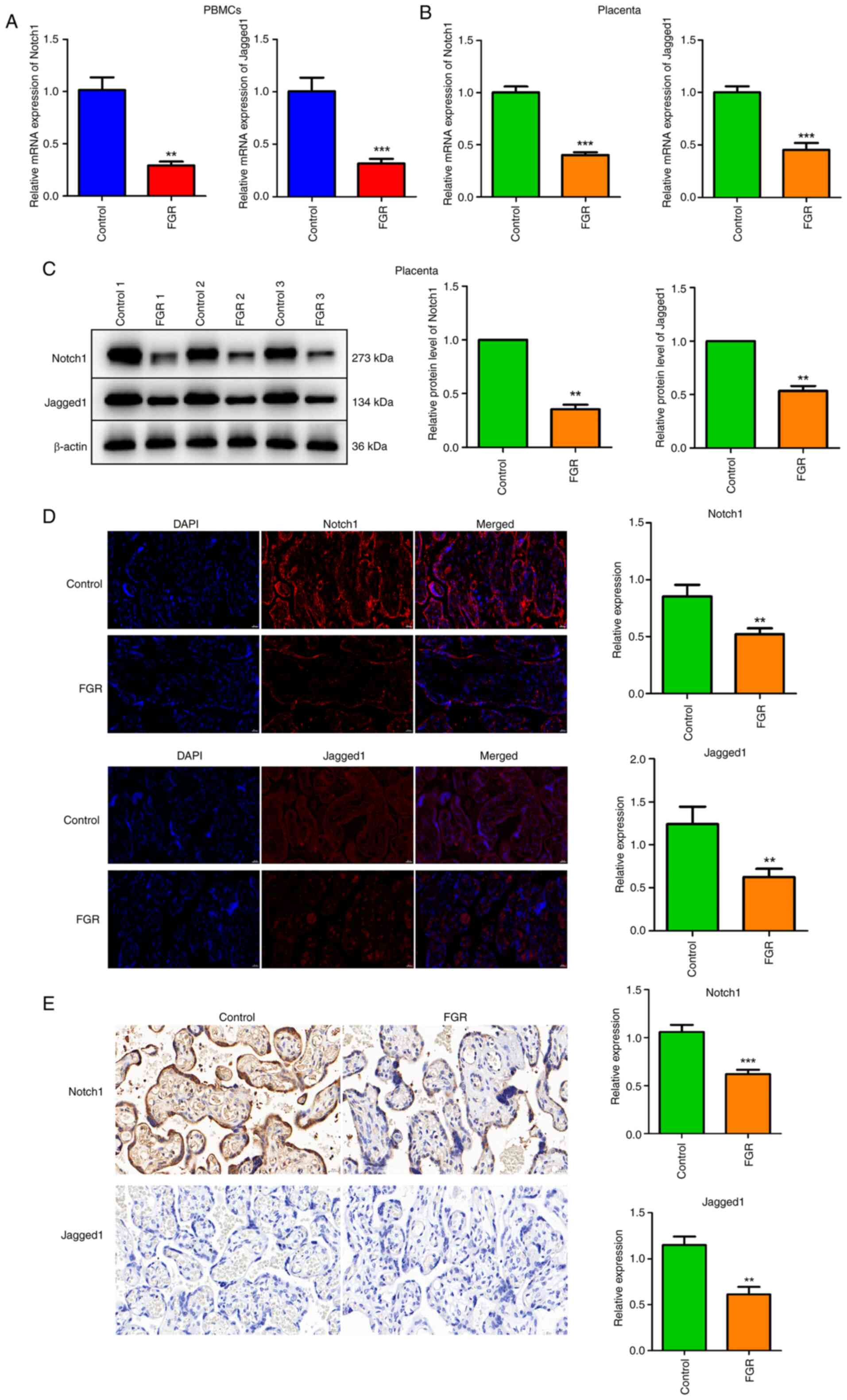
Afshar Y, Miele L and Fazleabas AT: Notch1
is regulated by chorionic gonadotropin and progesterone in
endometrial stromal cells and modulates decidualization in
primates. Endocrinology. 153:2884–2896. 2012.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hunkapiller NM, Gasperowicz M, Kapidzic M,
Plaks V, Maltepe E, Kitajewski J, Cross JC and Fisher SJ: A role
for Notch signaling in trophoblast endovascular invasion and in the
pathogenesis of pre-eclampsia. Development. 138:2987–2998.
2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sahin Z, Acar N, Ozbey O, Ustunel I and
Demir R: Distribution of Notch family proteins in intrauterine
growth restriction and hypertension complicated human term
placentas. Acta Histochem. 113:270–276. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Chen YH, Liu ZB, Ma L, Zhang ZC, Fu L, Yu
Z, Chen W, Song YP, Wang P, Wang H and Xu X: Gestational vitamin D
deficiency causes placental insufficiency and fetal intrauterine
growth restriction partially through inducing placental
inflammation. J Steroid Biochem Mol Biol.
203(105733)2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
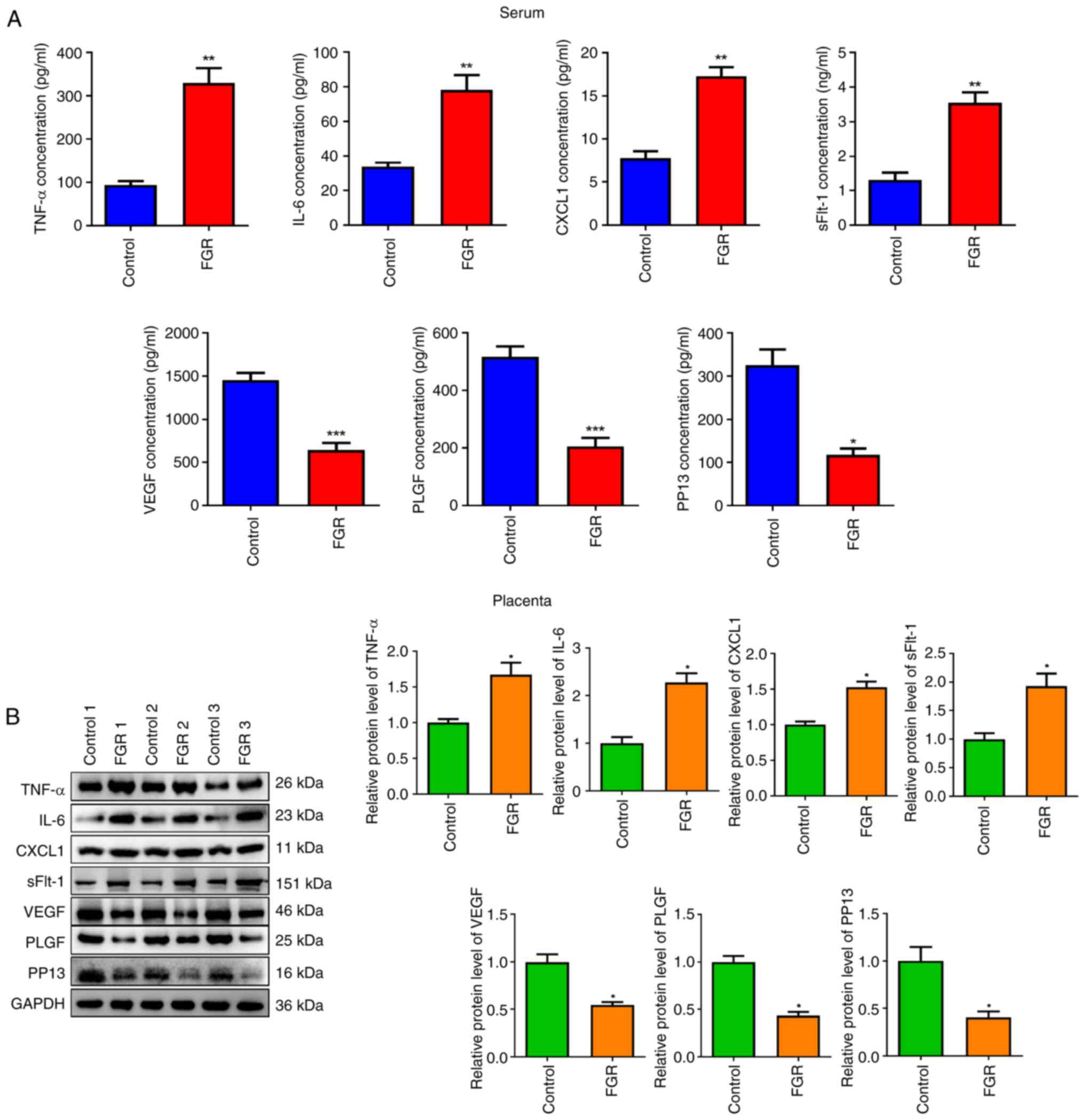
Hong J and Kumar S: Circulating biomarkers
associated with placental dysfunction and their utility for
predicting fetal growth restriction. Clin Sci (Lond). 137:579–595.
2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Dietrich B, Haider S, Meinhardt G,
Pollheimer J and Knöfler M: WNT and NOTCH signaling in human
trophoblast development and differentiation. Cell Mol Life Sci.
79(292)2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Scifres CM and Nelson DM: Intrauterine
growth restriction, human placental development and trophoblast
cell death. J Physiol. 587:3453–3458. 2009.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gale NW, Dominguez MG, Noguera I, Pan L,
Hughes V, Valenzuela DM, Murphy AJ, Adams NC, Lin HC, Holash J, et
al: Haploinsufficiency of delta-like 4 ligand results in embryonic
lethality due to major defects in arterial and vascular
development. Proc Natl Acad Sci USA. 101:15949–15954.
2004.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Thurston G and Gale NW: Vascular
endothelial growth factor and other signaling pathways in
developmental and pathologic angiogenesis. Int J Hematol. 80:7–20.
2004.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Herr F, Schreiner I, Baal N, Pfarrer C and
Zygmunt M: Expression patterns of Notch receptors and their ligands
Jagged and Delta in human placenta. Placenta. 32:554–563.
2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kirici P, Çağıran FT, Kali Z, Tanriverdi
ES, Mavral N and Ecin SM: Determination of maternal serum
pro-inflammatory cytokine changes in intrauterine growth
restriction. Eur Rev Med Pharmacol Sci. 27:1996–2001.
2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Al-Azemi M, Raghupathy R and Azizieh F:
Pro-inflammatory and anti-inflammatory cytokine profiles in fetal
growth restriction. Clin Exp Obstet Gynecol. 44:98–103.
2017.PubMed/NCBI
|
|
26
|
Kluivers ACM, Biesbroek A, Visser W, Saleh
L, Russcher H, Danser AHJ and Neuman RI: Angiogenic imbalance in
pre-eclampsia and fetal growth restriction: enhanced soluble
fms-like tyrosine kinase-1 binding or diminished production of
placental growth factor? Ultrasound Obstet Gynecol. 61:466–473.
2023.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Gadde R, Cd D and Sheela SR: Placental
protein 13: An important biological protein in preeclampsia. J Circ
Biomark. 7(1849454418786159)2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Yu N, Cui H, Chen X and Chang Y: First
trimester maternal serum analytes and second trimester uterine
artery Doppler in the prediction of preeclampsia and fetal growth
restriction. Taiwan J Obstet Gynecol. 56:358–361. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Rana S, Burke SD and Karumanchi SA:
Imbalances in circulating angiogenic factors in the pathophysiology
of preeclampsia and related disorders. Am J Obstet Gynecol. 226
(2S):S1019–S1034. 2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Garcia-Manau P, Mendoza M, Bonacina E,
Garrido-Gimenez C, Fernandez-Oliva A, Zanini J, Catalan M, Tur H,
Serrano B and Carreras E: Soluble fms-like tyrosine kinase to
placental growth factor ratio in different stages of early-onset
fetal growth restriction and small for gestational age. Acta Obstet
Gynecol Scand. 100:119–128. 2021.PubMed/NCBI View Article : Google Scholar
|
|
31
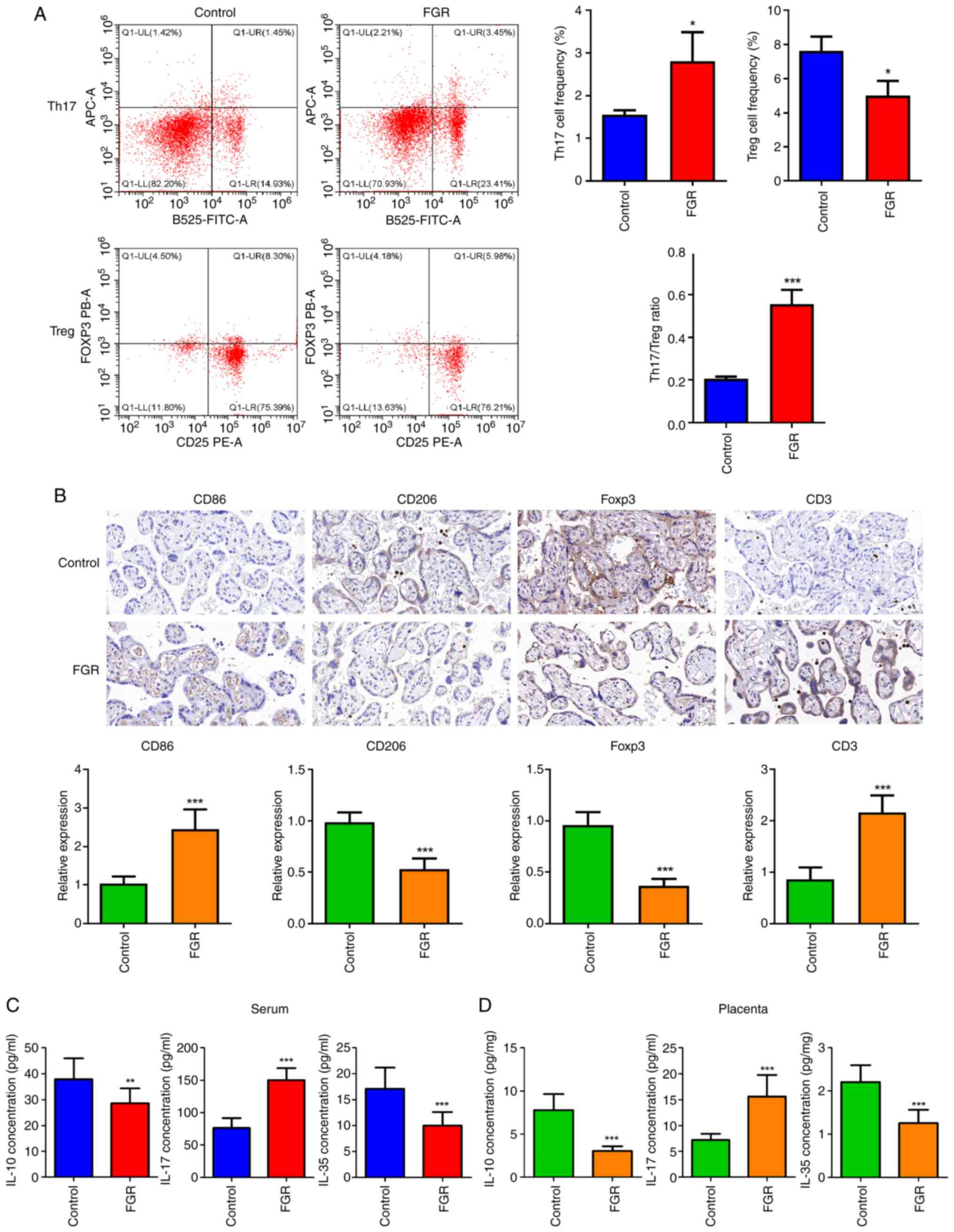
|
Zhang Z, Liu H, Shi Y, Xu N, Wang Y, Li A
and Song W: Increased circulating Th22 cells correlated with Th17
cells in patients with severe preeclampsia. Hypertens Pregnancy.
36:100–107. 2017.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Liu ZZ, Sun GQ, Hu XH, Kwak-Kim J and Liao
AH: The transdifferentiation of regulatory T and Th17 cells in
autoimmune/inflammatory diseases and its potential implications in
pregnancy complications. Am J Reprod Immunol. 78:2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Niedźwiecki M, Budziło O, Zieliński M,
Adamkiewicz-Drożyńska E, Maciejka-Kembłowska L, Szczepański T and
Trzonkowski P:
CD4+CD25highCD127low/-FoxP3+
regulatory T cell subpopulations in the bone marrow and peripheral
blood of children with ALL: Brief report. J Immunol Res.
2018(1292404)2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Matsuda M, Terada T, Kitatani K, Kawata R
and Nabe T: Analyses of Foxp3+ Treg cells and Tr1 cells
in subcutaneous immunotherapy-treated allergic individuals in
humans and mice. Nihon Yakurigaku Zasshi. 154:17–22.
2019.PubMed/NCBI View Article : Google Scholar : (In Japanese).
|
|
35
|
Laresgoiti-Servitje E: A leading role for
the immune system in the pathophysiology of preeclampsia. J Leukoc
Biol. 94:247–257. 2013.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Wang LL, Li ZH, Wang H, Kwak-Kim J and
Liao AH: Cutting edge: The regulatory mechanisms of macrophage
polarization and function during pregnancy. J Reprod Immunol.
151(103627)2022.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Yao Y, Xu XH and Jin L: Macrophage
polarization in physiological and pathological pregnancy. Front
Immunol. 10(792)2019.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Bezemer RE, Faas MM, van Goor H, Gordijn
SJ and Prins JR: Decidual macrophages and Hofbauer cells in fetal
growth restriction. Front Immunol. 15(1379537)2024.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Berezhna VA, Mamontova TV and Gromova AM:
Cd68+ M1 macrophages is associated with placental insufficiency
under fetal growth restriction. Wiad Lek. 74:213–219.
2021.PubMed/NCBI
|