Introduction
The global geriatric population is expanding
rapidly, with individuals aged ≥65 years projected to more than
double in the coming decades, reaching ~2.2 billion by the late
2070s (1). Thailand transitioned to
an aged society as the proportion of its population aged ≥60 years
reached approximately 20%, reflecting significant demographic aging
in recent years (2). Aging is
associated with multisystem decline, particularly in the
musculoskeletal system, which increases vulnerability to low-energy
fragility injuries. Among these, hip fractures are common and
represent a major public health concern due to their association
with disability, reduced quality of life, elevated mortality and
substantial healthcare costs (3,4). In
the United States, hospitalization costs for hip fractures exceed
$30 billion annually, while in Japan they reach ~$2.99 billion
(5,6). Across Asia, fragility fractures are
projected to nearly double by 2050, with direct costs increasing
from $9.5 billion in 2018 to $15 billion (7). In Thailand, hip fractures with
hospitalization costs increased 2.5-fold between 2013 and
2022(8). Globally, hip fracture
incidence is estimated at 182 cases per 100,000 individuals (95%
uncertainty interval, 142-231) (9).
In Thailand, the incidence of hip fractures increased annually from
2013 to 2019 before stabilizing between 2019 and 2022, with the
age-standardized incidence rate rising from 116.3 cases per 100,000
individuals in 2013 to 145.1 cases in 2019, with a slight decline
to 140.7 cases in 2022(8).
Within the Thai context, fragility or osteoporotic
fractures are defined as hip fractures resulting from low-energy
traumatic mechanisms in individuals aged ≥50 years (10). Surgical intervention remains the
standard treatment, aiming to reduce mortality and prevent
long-term disability. However, postoperative functional and
ambulatory recovery is often suboptimal and varies considerably
across studies (11-13).
Previous reports have indicated that 40-60% of patients regain
pre-fracture mobility and instrumental activities of daily living
(ADLs) within 3 to 6 months post-surgery (13,14),
while more recent evidence has suggested that at 3 months, only 20%
achieve satisfactory ambulation and 21.5% regain pre-injury walking
ability (15). Nearly 30% fail to
recover ADLs within 1 year (16),
and registry data from Japan show that ~10% of previously
ambulatory patients remain unable to walk at 4 months (17). Furthermore, a systematic review
concluded that despite advances in anesthesia, perioperative care
and rehabilitation, the 1-year mortality rate remains substantial,
with a mean of 22% (range, 2.4-34.8%) and marked variation across
populations (18). Ambulatory
ability is an essential functional capacity in older adults,
enabling them to carry out basic ADLs and maintain social
participation through community ambulation (19). Therefore, early rehabilitation
training after hip fracture surgery, encompassing mobility,
transfer and ambulation training, is crucial for preventing
complications from prolonged bed rest and enabling patients to
regain mobility and independent ambulation (20-22).
Recovery of ambulatory capacity after hip fracture
surgery depends on multiple factors, including preoperative,
intraoperative and postoperative conditions (23). While several studies have examined
preoperative and perioperative predictors (24-26),
relatively few have focused on postoperative prognostic factors
(27,28). Postoperative complications play a
crucial role in determining functional outcomes after hip fracture
surgery. Prolonged Intensive Care Unit (ICU) stays, and the need
for ventilator support have been associated with increased
long-term morbidity and increased mortality rates (23,29).
Tangchitphisut et al (23)
reported that postoperative ICU admission or ventilator use was
significantly more common among patients who were unable to bear
self-weight at discharge (10/55 patients, 18.2%; P<0.001).
Similarly, Eschbach et al (29) found that geriatric hip-fracture
patients requiring prolonged ICU care (>3 days) had markedly
higher in-hospital, 6-month and 12-month mortality rates compared
with those with shorter ICU stays (P=0.001). Furthermore,
postoperative complications such as infections (particularly
pressure ulcers), delirium, arrhythmias and respiratory issues have
been linked to poorer functional and mobility outcomes (13,23,30).
Recent evidence has also identified postoperative medical
complications as the most significant risk factor for persistent
walking disability (23,24,27).
Although hip fractures profoundly affect both short and long-term
outcomes, evidence regarding prognostic factors for ambulation
during the early subacute period remains limited. Early
identification of patients at high risk for impaired ambulation is
essential to guide postoperative management, optimize
rehabilitation and support caregiver planning. The 6-week timeframe
represents a clinically relevant milestone, coinciding with routine
follow-up, facilitating timely rehabilitation and enabling
recognition of patients at risk of delayed recovery before
longer-term outcomes are established. To address this gap, the
present study aimed to identify postoperative prognostic factors
associated with the inability to ambulate 6 weeks after fragility
hip fracture surgery.
Materials and methods
Study design and setting
This retrospective cohort study was conducted at a
tertiary care referral center, Hatyai Hospital (Songkhla,
Thailand). Data were obtained from electronic medical records
(EMRs) of patients treated between October 1, 2018, and September
30, 2023. The inclusion criteria were as follows: i) Age ≥50 years;
ii) diagnosis of a single, closed hip fracture resulting from
low-energy trauma; iii) a fracture classified as a femoral neck,
intertrochanteric or subtrochanteric fracture, identified by
specific International Classification of Diseases (ICD)-10 codes
(31) (S72.000-S72.019,
S72.100-S72.101, S72.110-S72.111 and S72.200-S72.210); and iv)
surgical treatment for a hip fracture, identified using
ICD-9(32) procedure codes (79.15,
79.25, 79.35, 81.51, and 81.52). The exclusion criteria were as
follows: i) Hip fractures secondary to pathological conditions (for
example. malignancy); ii) multiple traumatic injuries sustained
during the same admission; iii) fractures caused by high-energy
trauma; iv) periprosthetic fractures or fractures involving
previous nail fixation; v) conservative (non-surgical) management;
vi) pre-fracture bedridden status or wheelchair dependence; vii)
in-hospital mortality before discharge; and viii) incomplete or
missing EMR data during the study period. The study was approved by
the Human Research Ethics Committee of Hatyai Hospital (approval
no. HYH EC 007-67-01).
Surgical intervention was performed using procedures
appropriate for the specific type of hip fracture. Following
surgery, all patients underwent a standardized postoperative
rehabilitation program based on the recommendations of the American
Academy of Orthopedic Surgeons (21) and the National Institute for Health
and Care Excellence (22). The
program was designed to promote functional recovery and ambulation,
with individual modifications made according to patient centered
care principles that considered physical status, comorbidities,
surgical procedure and overall tolerance. The rehabilitation
protocol for ambulatory training emphasized early mobilization and
included bed mobility exercises, transitions from supine to
sitting, sitting balance activities, sit to stand transfers, safe
pivot transfers from bed to chair or wheelchair and standing
balance training. Once the patient demonstrated adequate stability,
ambulation training with walking practice was introduced. Patients
were encouraged to ambulate with a walker and to practice partial
weight bearing on the surgical limb as tolerated. Each training
session was conducted once daily for ~20 to 30 min. Routine
follow-up evaluations were performed at 6 weeks postsurgery to
monitor recovery, assess ambulatory status, and address ongoing
complications and care needs.
Data collection
A retrospective review was conducted using the EMRs
of 432 patients who underwent hip fracture surgery. Data collected
included admission dates, clinical characteristics and
postoperative variables considered potential prognostic factors for
the inability to walk 6 weeks after surgery. Candidate
postoperative predictors included: i) Postoperative ICU admission
or ventilator use (23,29), which was defined to include either
ICU admission regardless of ventilator support or endotracheal
intubation with mechanical ventilation, in the ICU or elsewhere;
ii) need for postoperative oxygen support (33,34),
referred to any supplemental oxygen via nasal cannula, face mask or
high-flow oxygen, administered to prevent hypoxemia and maintain a
peripheral oxygen saturation level generally ≥95% (unless
contraindicated); iii) urinary catheter use on the second
postoperative day (23,35); iv) the presence of postoperative
surgical complications (33,36),
such as postoperative weight-bearing restrictions due to poor bone
quality or revision surgery following fixation failure; v) anemia
from postoperative blood loss (37); vi) the presence of postoperative
medical complications (33,38) (such as pressure ulcers, urinary
tract infection and pneumonia); vii) time to initiation of
functional training (39-41)
(<48, 48-72 and >72 h post-operation); viii) the ability to
walk at hospital discharge; ix) the length of stay (LOS) (42); and x) the presence of overall
complications within 6 weeks after discharge (23,27,33),
classified as surgical, medical or mental-health related. The
primary endpoint was ambulatory status 6 weeks after surgery.
Patients were classified into two groups based on discharge
ambulation: i) a non-ambulatory group, consisting of patients who
were bedridden or wheelchair-dependent; and ii) an ambulatory
group, consisting of patients who could walk independently or with
the aid of a walking device.
Sample size calculation
The determination of an appropriate sample size for
logistic regression typically necessitates a minimum of 5 to 10
events per candidate predictor parameter to ensure model
reliability. Given that the present study included 14 exploratory
variables (10 postoperative factors and 4 demographic factors to
adjust the model), the corresponding requirement ranged from 90 to
140 events (43,44). Considering that the prevalence of
inability to walk in this study was 24.8%, a total sample size
between 364 and 565 participants was deemed optimal.
Statistical analysis
Statistical analysis was conducted using the Stata
Statistical Package (version 18.0; Stata Corp LLC). Categorical
variables are presented as frequencies and percentages, while
continuous variables are reported as means and standard deviations
for normally distributed data or medians and interquartile ranges
for skewed data. To compare proportions between the two groups
(i.e., inability or ability to walk 6 weeks after fragility hip
fracture surgery), the χ2 test was used. When the
expected cell count was less than five, Fisher's exact test was
applied. Continuous variables were compared using Student's t-test
for parametric data or a Mann-Whitney U test for non-parametric
data, depending on the distribution. Variables with clinical
relevance and those with P<0.25 (45-47)
in an initial screening were included in the univariable analysis,
with results presented as univariable risk ratios. To identify
factors associated with the inability to walk 6 weeks after
fragility hip fracture surgery, a multivariable Poisson regression
model was fitted with a log link and robust standard errors
(48). The model was adjusted for
age, sex, Charlson Comorbidity Index (CCI) (49) and fracture type. The binary outcome
was the ability/inability to walk at 6 weeks, and multivariable
risk ratios (mRRs) with 95% confidence intervals (CIs) were
estimated. Two-sided P<0.05 was considered statistically
significant. Multicollinearity among covariates was assessed using
variance inflation factors (VIF), with a VIF value of <5
considered acceptable (50). During
variable selection, it was found that ambulatory training and the
inability to walk at discharge were collinear, and a significant
association was observed between the two variables. As they are
also theoretically expected to be correlated, a pragmatic approach
was used to determine which variable contributed more effectively
to the multivariable model (51).
Inability to walk at discharge yielded a higher adjusted R-squared
value and was therefore retained in the final model. All other
postoperative predictors included in the analysis had VIF values
<5.
Results
Study population and exclusions
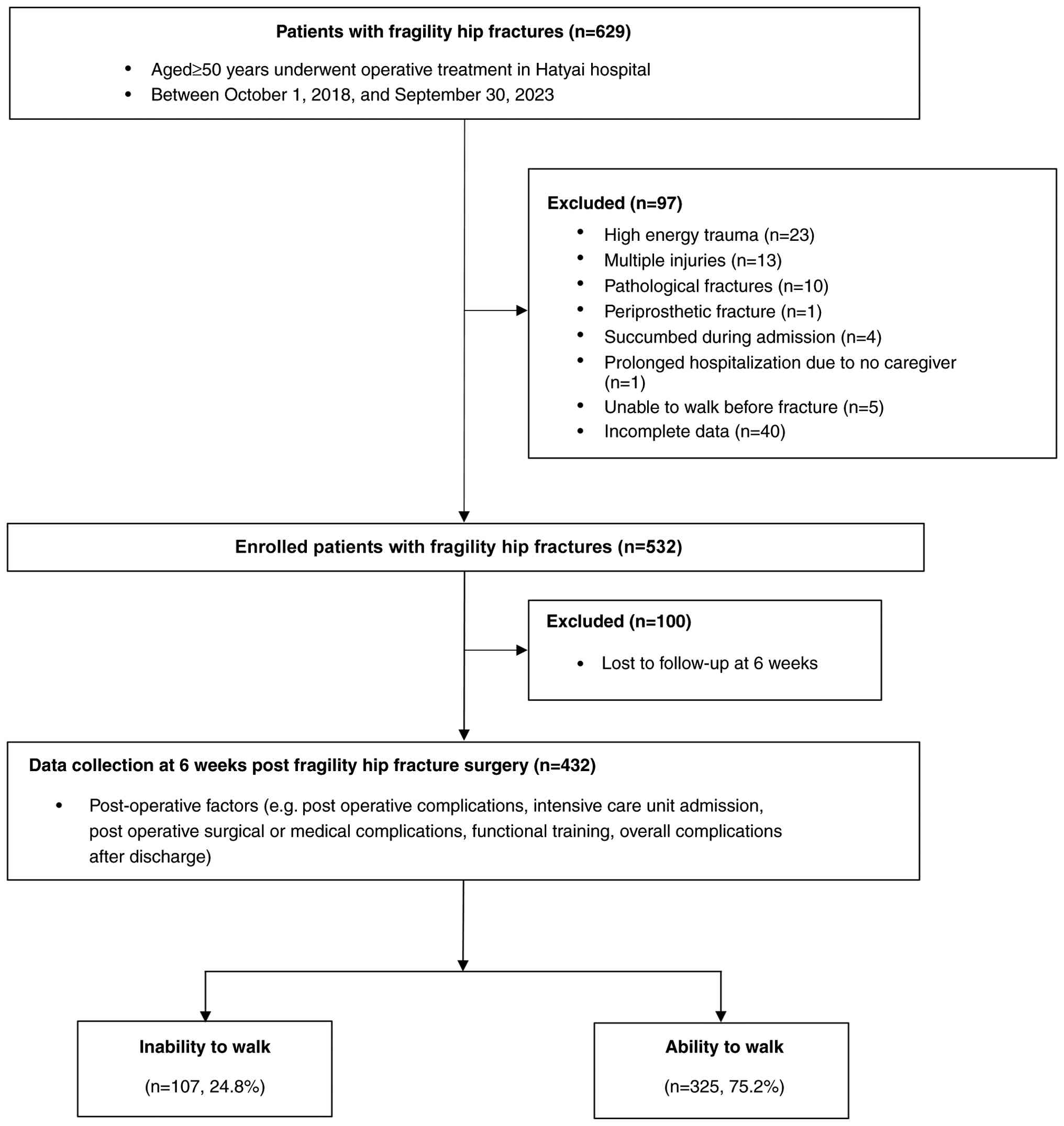
A total of 629 patients with fragility hip fractures
underwent surgery. Of these, 97 patients were excluded for the
following reasons: 23 experienced high-energy trauma, 13 sustained
multiple injuries, 10 had pathological fractures, 1 had a
periprosthetic fracture, 4 died during admission, 1 required
prolonged hospitalization due to the absence of a caregiver, 5 were
unable to walk prior to the fracture and 40 had incomplete data
collection. Consequently, 532 patients were left for the present
analysis. However, 100 patients were lost to follow-up at 6 weeks
postoperatively, resulting in a final study population of 432
patients. There were no statistically significant differences in
baseline characteristics [age, sex, CCI, preoperative hematocrit
(Hct) and fracture type] between patients who completed follow-up
and those who were lost to follow-up (Table SI). The majority of included
participants were female (313 patients, 72.5%) and overall age was
76.8±9.6 years (range, 52-100 years).
Comparative analysis of ambulatory and
non-ambulatory patient groups at 6 weeks postoperatively
At 6 weeks postsurgery, 325 patients (75.2%)
regained the ability to walk, while 107 patients (24.8%) remained
non-ambulatory (Fig. 1). No
statistically significant differences were observed between groups
regarding BMI, smoking status, and glomerular filtration rate.
However, Hct levels were significantly lower in the non-ambulatory
group (31.3 vs. 33.4%; P<0.001). When comparing the two groups,
the inability-to-walk group showed a significantly higher
proportion of female patients (81.3 vs. 69.5%; P=0.018), higher
mean age (79.3±9.6 vs. 76.0±9.4 years; P=0.001) and a lower
proportion of pre-fracture independent community ambulation (35.5
vs. 71.7%; P<0.001). Additionally, this group exhibited a
significantly higher prevalence of underlying diseases (92.5 vs.
82.8%; P=0.014), including diabetes mellitus, cerebrovascular
disease, Parkinson's disease, Alzheimer's disease or dementia,
heart disease and musculoskeletal disorders. Furthermore,
significant differences were found between the non-ambulatory and
ambulatory group in the proportion of patients who sustained indoor
falls (88.8 vs. 79.4%; P=0.049) and the distribution of fracture
types (P=0.002) (Table I).
 | Table IComparison of patients' demographic
and clinical characteristics between groups with the inability and
ability to walk at 6 weeks after fragility hip fracture surgery
(n=432). |
Table I
Comparison of patients' demographic
and clinical characteristics between groups with the inability and
ability to walk at 6 weeks after fragility hip fracture surgery
(n=432).
| Variables | Inability to walk
(n=107) | Ability to walk
(n=325) | P-value |
|---|
| Female, n (%) | 87 (81.3) | 226 (69.5) | 0.018 |
| Age,
yearsa | 79.3±9.6 | 76.0±9.4 | 0.002 |
| Body mass index,
kg/m2a | 22.3±4.5 | 22.5±4.1 | 0.577 |
| Smoking, n (%) | 7 (6.5) | 37 (11.4) | 0.711 |
| Pre fracture
community walking independent, n (%) | 38 (35.5) | 233 (71.7) | <0.001 |
| Underlying
diseases, n (%) | 99 (92.5) | 269 (82.8) | 0.014 |
|
Hypertension | 82 (76.6) | 217 (66.8) | 0.055 |
|
Diabetes
mellitus | 40 (37.4) | 88 (27.1) | 0.043 |
|
Dyslipidemia | 51 (47.7) | 125 (38.5) | 0.093 |
|
Cerebrovascular
disease | 33 (30.8) | 43 (13.2) | <0.001 |
|
Parkinson's
disease | 6 (5.6) | 5 (1.5) | 0.020 |
|
Alzheimer's/dementia | 12 (11.2) | 15 (4.6) | 0.014 |
|
Heart
disease (AF/VHD/IHD) | 16 (15.0) | 23 (7.1) | 0.014 |
|
Pulmonary
disease | 6 (5.6) | 40 (12.3) | 0.051 |
|
Anemia | 15 (14.0) | 36 (11.1) | 0.413 |
|
Musculoskeletal
problems | 19 (17.8) | 34 (10.5) | 0.046 |
| Charlson
Comorbidity Indexa | 5.0±1.7 | 4.1±1.5 | <0.001 |
| Falling indoors, n
(%) | 95 (88.8) | 258 (79.4) | 0.049 |
| Fracture types, n
(%) | | | 0.002 |
|
Subtrochanteric
fracture of the femur | 3 (2.8) | 5 (1.5) | |
|
Intertrochanteric
fracture of the femur | 69 (64.5) | 152 (46.8) | |
|
Femoral neck
fracture | 35 (32.7) | 168 (51.7) | |
| Preoperative
hematocrit, %a | 31.3±5.0 | 33.4±5.2 | <0.001 |
| Glomerular
filtration rate, ml/mina | 74.0±26.5 | 81.0±48.8 | 0.166 |
Postoperative factors associated with
ambulatory status
Regarding postoperative factors, patients in the
non-ambulatory group at 6 weeks after fragility hip fracture
surgery exhibited a significantly higher need for postoperative
oxygen support (59.8 vs. 40.6%; P=0.001), urinary catheter use on
the second postoperative day (62.6 vs. 50.5%; P=0.029), presence of
postoperative surgical complications (11.2 vs. 1.8%; P<0.001)
and presence of postoperative medical complications (39.2 vs.
22.5%; P=0.001). Additionally, LOS (≥14 days) was more prevalent
among patients who remained unable to walk (35.5 vs. 15.4%;
P<0.001), as was the occurrence of postoperative complications
within 6 weeks after discharge (16.8 vs. 3.1%; P<0.001).
Conversely, the attainment of ambulation training was significantly
higher in the group that regained walking ability compared with
that in the non-ambulatory group (86.1 vs. 28.4%; P<0.001)
(Table II).
 | Table IIComparison of patients'
post-operative factors between groups with the inability and
ability to walk at 6 weeks after fragility hip fracture
surgery. |
Table II
Comparison of patients'
post-operative factors between groups with the inability and
ability to walk at 6 weeks after fragility hip fracture
surgery.
| Variables | Inability to walk
(n=107) | Ability to walk
(n=325) | P-value |
|---|
| Postoperative ICU
admission or ventilator use, n (%) | 7 (6.5) | 9 (2.8) | 0.082 |
| Postoperative need
for oxygen support, n (%) | 64 (59.8) | 132 (40.6) | 0.001 |
| Urinary catheter
used in the second day post operative, n (%) | 67 (62.6) | 164 (50.5) | 0.029 |
| Presence of post
operative surgical complications, n (%) | 12 (11.2) | 6 (1.8) | <0.001 |
| Anemia due to post
operative blood loss, n (%) | 45 (42.1) | 107 (32.9) | 0.086 |
| Presence of the
post operative medical complications, n (%) | 42 (39.3) | 73 (22.5) | 0.001 |
| Time to start
functional training, n (%) | | | 0.056 |
|
<24 h
post-operation | 43 (40.2) | 168 (51.7) | |
|
24-48 h
post-operation | 32 (29.9) | 92 (28.3) | |
|
>72 h
post-operation | 30 (29.9) | 65 (20.0) | |
| Type of functional
training, n (%) | | | |
|
Mobility
training | 106 (99.1) | 327 (100.0) | 0.081 |
|
Transfer
training | 107 (100.0) | 323 (99.4) | 0.416 |
|
Ambulation
training | 30 (28.0) | 280 (86.2) | <0.001 |
| Inability to walk
at discharge, n (%) | 102 (95.3) | 72 (22.2) | <0.001 |
| Length of stay ≥14
days, n (%) | 38 (35.5) | 50 (15.4) | <0.001 |
| Presence of the
overall complications within 6 weeks after discharge, n (%) | 18 (16.8) | 10 (3.1) | <0.001 |
Regression analysis results
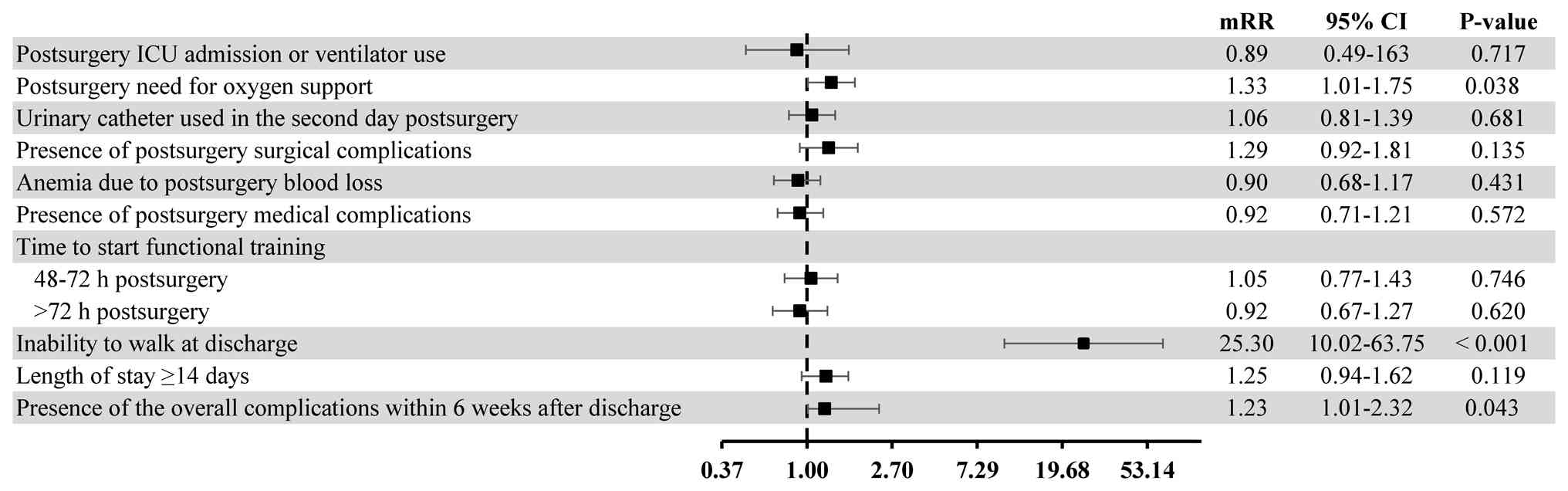
The results of univariable and multivariable
regression analyses are presented in Table III. In the univariate analysis,
several factors emerged as significant predictors, including
postoperative ICU admission or ventilator use, the need for
postoperative oxygen support, urinary catheter use on the second
postoperative day, the presence of postoperative surgical
complications, the presence of postoperative medical complications,
time to start functional training (>72 h post-operation),
inability to walk at hospital discharge, LOS (≥14 days), and the
occurrence of overall complications within 6 weeks post-discharge.
However, the multivariable regression analysis identified only the
following key prognostic factors: Inability to walk at discharge
(mRR, 25.3; 95% CI, 10.0-63.8; P<0.001), postsurgery need for
oxygen support (mRR, 1.33; 95% CI, 1.01-1.75; P=0.038) and the
presence of overall postsurgery complications within 6 weeks after
discharge (mRR, 1.23; 95% CI, 1.01-2.32; P=0.043) (Fig. 2).
 | Table IIIuRR and mRR of post-operative
prognostic factors of patients with the inability to walk at 6
weeks after fragility hip fracture surgery. |
Table III
uRR and mRR of post-operative
prognostic factors of patients with the inability to walk at 6
weeks after fragility hip fracture surgery.
| | Univariable
analysis | Multivariable
analysis |
|---|
| Variables | uRR | 95% CI | P-value | mRR | 95% CI | P-value |
|---|
| Postoperative ICU
admission or ventilator use | 1.82 | 1.02-3.25 | 0.043 | 0.89 | 0.49-1.63 | 0.717 |
| Postoperative need
for oxygen support | 1.79 | 1.28-2.51 | 0.001 | 1.33 | 1.01-1.75 | 0.038 |
| Urinary catheter
used in the second day post operative | 1.46 | 1.03-2.05 | 0.031 | 1.06 | 0.81-1.39 | 0.681 |
| Presence of post
operative surgical complications | 2.9 | 2.00-4.21 | <0.001 | 1.29 | 0.92-1.81 | 0.135 |
| Anemia due to post
operative blood loss | 1.34 | 0.96-1.85 | 0.084 | 0.90 | 0.68-1.17 | 0.431 |
| Presence of the
post operative medical complications | 1.78 | 1.29-2.46 | <0.001 | 0.92 | 0.71-1.21 | 0.572 |
| Time to start
functional training | | | | | | |
|
<48 h
post-operation | | Reference | | | Reference | |
|
48-72 h
post-operation | 1.27 | 0.84-1.89 | 0.248 | 1.05 | 0.77-1.43 | 0.746 |
|
>72 h
post-operation | 1.62 | 1.10-2.39 | 0.015 | 0.92 | 0.67-1.27 | 0.620 |
| Inability to walk
at discharge | 30.2 | 12.58-72.7 | <0.001 | 25.3 | 10.02-63.75 | <0.001 |
| Length of stay ≥14
days | 2.15 | 1.56-2.96 | <0.001 | 1.25 | 0.94-1.65 | 0.119 |
| Presence of the
overall complications within 6 weeks after discharge | 2.82 | 2.02-3.92 | <0.001 | 1.23 | 1.01-2.32 | 0.043 |
Discussion
Hip fractures rank among the most serious fractures
in elderly individuals, often leading to impaired function, and
increased morbidity and mortality rates (13,52).
Elderly patients undergoing hip fracture surgery frequently exhibit
physical instability in the acute postoperative phase, which may
delay the initiation of rehabilitation (53,54).
Previous research has demonstrated that by 6 weeks postsurgery,
patients typically exhibit improved physical stability, enabling
participation in rehabilitation programs; however, vigilant
monitoring for potential complications remains imperative (27,55).
The present study aimed to identify prognostic factors associated
with the inability to walk at 6 weeks following fragility hip
fracture surgery. The findings emphasize the inability to walk at
discharge, the postoperative need for oxygen support and the
presence of postoperative complications within 6 weeks as
significant predictors of ambulatory outcomes.
The presence of overall complications after
discharge within 6 weeks increased the risk of the inability to
walk at 6 weeks post-fragility hip fracture surgery by 1.23 times
(95% CI, 1.01-2.32; P=0.043). Similarly, Chanthanapodi et al
(27) reported that postoperative
medical complications within the first 6 weeks were the strongest
prognostic factor for the inability to walk 6 weeks after surgery,
with a risk ratio (RR) of 2.04 (95% CI, 1.37-3.02; P<0.001).
However, the findings of the present study contrast with those in
the study by Monkuntod et al (56), which was a prospective observational
cohort study on older adults diagnosed with hip fractures,
scheduled for surgery and followed up for 2 weeks postoperatively
at three tertiary care hospitals. The study found that adverse
health outcomes during and after hospitalization did not predict
poor functional ability at discharge. This discrepancy may be
attributed to the shorter duration of complication recording (2
weeks) compared with both the present study and the research
conducted by Chanthanapodi et al (27). Empirical evidence suggests that
early identification of postoperative complications during the
acute to subacute rehabilitation phase is crucial in facilitating
functional recovery (33,55,57).
Ambulatory ability is a key concern for both
patients and caregivers (58).
Since walking ability is a crucial indicator of functional
recovery, it remains a primary focus for patients undergoing
surgery for fragility hip fractures during the postoperative period
(59). Previous research has
demonstrated that patients with hip fractures who regain early
walking ability have significantly higher survival rates at both 1-
and 10-years post-surgery (60).
Adulkasem et al (61)
reported that both pre-injury ambulatory status [odds ratio (OR),
52.72; 95% CI, 5.19-535.77] and ambulatory status at discharge (OR,
8.5; 95% CI, 3.33-21.70) were strong prognostic factors for
postoperative functional recovery, underscoring the importance of
baseline mobility. Similarly, the present study demonstrated a high
effect estimate for the inability to walk at discharge (mRR, 25.3;
95% CI, 10.02-63.75), although the wide confidence interval
observed may reflect the modest sample size and a potential risk of
model overfitting. The higher effect estimates in the present study
compared with those reported by Adulkasem et al (15,61)
are likely attributable to differences in study populations and
model specifications. While Adulkasem et al (15,61)
included patients across all baseline walking abilities, including
those who were non-ambulatory prior to hip fracture, the present
cohort was restricted to individuals who were ambulatory before the
fracture. Furthermore, the previous study analyses incorporated
both pre-fracture and discharge ambulatory status as predictors,
whereas the present model included only ambulatory ability at
discharge. Limiting the sample to pre-fracture ambulatory patients
and including a single post-fracture mobility variable may have
contributed to the more pronounced effect size observed.
The postoperative need for oxygen therapy was a
significant predictor of inability to walk at 6 weeks in the
present study. While chest physiotherapy and bed-mobility exercises
can be initiated with supplemental oxygen, achieving adequate
oxygenation on room air is an essential milestone before commencing
ambulation training in Hatyai Hospital. Dependence on oxygen
supplementation may therefore be associated with delayed
ambulation, a condition linked to an increased risk of medical
complications, higher mortality rate and prolonged hospital stay
(62,63). In line with this, the Clinical
Insights on Thailand Postoperative Hip Fracture Care (20) recommend early mobilization programs
for patients undergoing surgery for fragility hip fractures.
Although postoperative ICU admission or ventilatory
support were significant in the univariate analysis, they were not
significant in the multivariate model. This finding aligns with a
previous study that reported no significant increase in the risk of
an inability to self-bear weight at discharge among patients
admitted to the ICU postoperatively or requiring ventilatory
support. ICU admission and ventilatory support primarily address
acute postoperative complications that are often transient and
treatable with current medical interventions; therefore, they may
not serve as indicators of long-term functional recovery.
Additionally, these factors were associated with other stronger
predictors included in the model, such as overall postoperative
complications and ability to ambulate at discharge. After
adjustment for these variables, ICU/ventilator use and early
complications were no longer significant, suggesting that their
effects were largely accounted for by these stronger
predictors.
The presence of postoperative surgical
complications, the presence of postoperative medical complications,
urinary catheter usage on the second postoperative day and a LOS of
≥14 days were significant predictors in the univariate analysis but
not in the multivariate model in the present study. Previous
studies have reported conflicting findings regarding postoperative
complications. While several studies have reported an association
between postoperative surgical and medical complications and poorer
mobility outcomes (27,64,65),
the study by Tangchitphisut et al (23) found no such association. One study
identified urinary catheter use as a significant predictor
(35), whereas another reported no
association (23). Similarly,
although earlier studies reported LOS as a significant predictor
(25,66), subsequent research did not confirm
this association (67).
Importantly, while acute postoperative complications were not
independent predictors in the present multivariate analysis, late
complications occurring after discharge were significantly
associated with poorer walking ability. This observation supports
the hypothesis that early postoperative complications may reflect
transient conditions amenable to contemporary medical management,
whereas late complications may exert a more profound and lasting
impact on functional recovery.
Despite providing valuable insights, the present
study has several limitations that warrant consideration. The
single-center design may limit generalizability. Also, the final
analysis included 432 patients, of whom 107 were unable to walk.
With 14 variables, the events-per-variable (EPV) ratio was 7.6
(107/14), falling within the commonly accepted 5-10 range for
exploratory analyses (43,44). Nevertheless, a modestly low EPV may
increase the risk of model overfitting, potentially leading to
wider confidence intervals and inflated effect estimates for some
variables. Resource constraints such as bed shortages also
necessitated early discharges and patient transfers based on
healthcare coverage policies, potentially introducing referral bias
that influenced outcomes. In addition, the retrospective design
required excluding patients with incomplete data, which may have
reduced statistical power and could potentially lead to under- or
overestimation of prognostic factors. The outcome ‘inability to
walk’ provides a simple measure of functional recovery but may not
fully capture other aspects of postoperative function, such as
independence in ADLs or mobility scores. The present study was
designed to explore postoperative predictive factors rather than to
develop or validate a formal predictive model. Development of a
robust, clinically applicable model would require a larger sample
and further research. The factors identified here should therefore
be interpreted as potential predictors that may help clinicians
remain vigilant when caring for patients who present with these
characteristics. Finally, although multidisciplinary rehabilitation
teams play a critical role in postoperative care, early
identification of prognostic indicators for functional recovery
remains insufficiently understood. This highlights the need for
prospective, multicenter studies incorporating comprehensive
geriatric assessments and rehabilitation-specific variables and
outcomes to better identify patients who may benefit from
additional rehabilitation support.
In conclusion, the present study identified three
key prognostic factors for early functional recovery at 6 weeks
after fragility hip fracture surgery: The ability to ambulate at
hospital discharge, the postoperative need for oxygen support and
the presence of overall postoperative complications within 6 weeks.
Early rehabilitation and proactive management of medical
complications are critical strategies to enhance postoperative
mobility and improve long-term outcomes in this vulnerable patient
population.
Supplementary Material
Comparison of demographic and clinical
characteristics between patients who completed follow-up and those
who were lost to follow-up.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
TJ performed data collection and analysis, wrote the
original draft of the manuscript, and prepared all materials. PL
contributed to the data collection. JS performed data analysis and
coordination, as well as supervised and revised the manuscript. TJ,
PL and JS contributed to the conceptual and methodological design
of the study. All authors have read and approved the final version
of the manuscript. TJ and JS confirm the authenticity of all the
raw data.
Ethics approval and consent to
participate
The protocol of this study was approved by the Human
Research Ethics Committee of Hatyai Hospital (Songkhla, Thailand;
approval no. HYH EC 007-67-01). All procedures involved in this
study followed the ethical standards of and complied with the
Declaration of Helsinki.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
United Nations Department of Economic and
Social Affairs, Population Division. World Population Prospects
2024: Summary of Results (UN DESA/POP/2024/TR/NO. 9), 2024.
https://population.un.org/wpp/assets/Files/WPP2024_Summary-of-Results.pdf.
|
|
2
|
Aung TNN, Moolphate S, Koyanagi Y,
Angkurawaranon C, Supakankunti S, Yuasa M and Aung MN: Determinants
of health-related quality of life among community-dwelling Thai
older adults in Chiang Mai, Northern Thailand. Risk Manag Healthc
Policy. 15:1761–1774. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mattisson L, Bojan A and Enocson A:
Epidemiology, treatment and mortality of trochanteric and
subtrochanteric hip fractures: Data from the Swedish fracture
register. BMC Musculoskelet Disord. 19(369)2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Amarilla-Donoso FJ, Lopez-Espuela F,
Roncero-Martin R, Leal-Hernandez O, Puerto-Parejo LM, Aliaga-Vera
I, Toribio-Felipe R and Lavado-García JM: Quality of life in
elderly people after a hip fracture: A prospective study. Health
Qual Life Outcomes. 18(71)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sarode AL, Su E, Drost J, Evan M, Haselton
L and Blecker N: The economic burden of hip fractures in the
geriatric population by mental health illness and substance use
status: National estimates 2016 to 2020. Injury.
56(112615)2025.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mori T, Komiyama J, Fujii T, Sanuki M,
Kume K, Kato G, Mori Y, Ueshima H, Matsui H, Tamiya N and Sugiyama
T: Medical expenditures for fragility hip fracture in Japan: A
study using the nationwide health insurance claims database. Arch
Osteoporos. 17(61)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Cheung CL, Ang SB, Chadha M, Chow ES,
Chung YS, Hew FL, Jaisamrarn U, Ng H, Takeuchi Y, Wu CH, et al: An
updated hip fracture projection in Asia: The Asian federation of
osteoporosis societies study. Osteoporos Sarcopenia. 4:16–21.
2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Charatcharoenwitthaya N, Nimitphong H,
Wattanachanya L, Songpatanasilp T, Ongphiphadhanakul B,
Deerochanawong C and Karaketklang K: Epidemiology of hip fractures
in Thailand. Osteoporos Int. 35:1661–1668. 2024.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Dong Y, Zhang Y, Song K, Kang H, Ye D and
Li F: What was the epidemiology and global Burden of disease of hip
fractures from 1990 to 2019? results from and additional analysis
of the global Burden of disease study 2019. Clin Orthop Relat Res.
481:1209–1220. 2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Amphansap T and Sujarekul P: Quality of
life and factors that affect osteoporotic hip fracture patients in
Thailand. Osteoporos Sarcopenia. 4:140–144. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sing CW, Lin TC, Bartholomew S, Bell JS,
Bennett C, Beyene K, Bosco-Lévy P, Chan AHY, Chandran M, Cheung CL,
et al: Global epidemiology of hip fractures: A study protocol using
a common analytical platform among multiple countries. BMJ Open.
11(e047258)2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wongtriratanachai P, Luevitoonvechkij S,
Songpatanasilp T, Sribunditkul S, Leerapun T, Phadungkiat S and
Rojanasthien S: Increasing incidence of hip fracture in Chiang Mai,
Thailand. J Clin Densitom. 16:347–352. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Dyer SM, Crotty M, Fairhall N, Magaziner
J, Beaupre LA, Cameron ID and Sherrington C: Fragility Fracture
Network (FFN) Rehabilitation Research Special Interest Group. A
critical review of the long-term disability outcomes following hip
fracture. BMC Geriatr. 16(158)2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Vochteloo AJ, Moerman S, Tuinebreijer WE,
Maier AB, de Vries MR, Bloem RM, Nelissen RG and Pilot P: More than
half of hip fracture patients do not regain mobility in the first
postoperative year. Geriatr Gerontol Int. 13:334–341.
2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Adulkasem N, Chotiyarnwong P,
Vanitcharoenkul E and Unnanuntana A: Ambulation recovery prediction
after hip fracture surgery using the Hip fracture short-term
ambulation prediction tool. J Rehabil Med.
56(jrm40780)2024.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kitcharanant N, Atthakomol P, Khorana J,
Phinyo P and Unnanuntana A: Prognostic factors for functional
recovery at 1-year following fragility hip fractures. Clin Orthop
Surg. 16:7–15. 2024.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Hosoi T, Yakabe M, Matsumoto S, Fujimori
K, Tamaki J, Nakatoh S, Ishii S, Okimoto N, Kamiya K, Akishita M,
et al: Relationship between antidementia medication and fracture
prevention in patients with Alzheimer's dementia using a nationwide
health insurance claims database. Sci Rep. 13(6893)2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Downey C, Kelly M and Quinlan JF: Changing
trends in the mortality rate at 1-year post hip fracture-a
systematic review. World J Orthop. 10:166–175. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Salpakoski A, Tormakangas T, Edgren J,
Sihvonen S, Pekkonen M, Heinonen A, Pesola M, Kallinen M, Rantanen
T and Sipilä S: Walking recovery after a hip fracture: A
prospective follow-up study among community-dwelling over 60-year
old men and women. Biomed Res Int. 2014(289549)2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Unnanuntana A, Kuptniratsaikul V,
Srinonprasert V, Charatcharoenwitthaya N, Kulachote N,
Papinwitchakul L, Wattanachanya L and Chotanaphuti T: A
multidisciplinary approach to post-operative fragility hip fracture
care in Thailand-a narrative review. Injury.
54(111039)2023.PubMed/NCBI View Article : Google Scholar
|
|
21
|
American Academy of Orthopaedic Surgeons.
Postoperative rehabilitation of low energy hip fractures in older
adults: Appropriate use criteria. Re-issued by the American Academy
of Orthopaedic Surgeons Board of Directors 2023 September 9, 2025.
Available from: https://www.aaos.org/globalassets/quality-and-practice-resources/hip-fractures-in-the-elderly/hip-fx-rehab-auc_reapproval.pdf.
|
|
22
|
National Institute for Health and Care
Excellence (NICE). Hip fracture: management (update): Economic
model report for total hip replacement versus hemiarthroplasty.
NICE guideline CG124.2023 September 9, 2025]. Available from:
https://www.nice.org.uk/guidance/cg124/evidence/economic-model-report-pdf-11317540285.
|
|
23
|
Tangchitphisut P, Khorana J, Phinyo P,
Patumanond J, Rojanasthien S and Apivatthakakul T: Prognostic
factors of the inability to bear self-weight at discharge in
patients with fragility femoral neck fracture: A 5-year
retrospective cohort study in Thailand. Int J Environ Res Public
Health. 19(3992)2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kitcharanant N, Atthakomol P, Khorana J,
Phinyo P and Unnanuntana A: Predictive model of recovery to
prefracture activities-of-daily-living status one year after
fragility hip fracture. Medicina (Kaunas). 60(615)2024.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ko Y: Pre- and perioperative risk factors
of post hip fracture surgery walking failure in the elderly.
Geriatr Orthop Surg Rehabil. 10(2151459319853463)2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Pajulammi HM, Pihlajamaki HK, Luukkaala TH
and Nuotio MS: Pre- and perioperative predictors of changes in
mobility and living arrangements after hip fracture-a
population-based study. Arch Gerontol Geriatr. 61:182–189.
2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Chanthanapodi P, Tammata N, Laoruengthana
A and Jarusriwanna A: Independent walking disability after
fragility hip fractures: A prognostic factors analysis. Geriatr
Orthop Surg Rehabil. 15(21514593241278963)2024.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Sheehan KJ, Guerrero EM, Tainter D, Dial
B, Milton-Cole R, Blair JA, Alexander J, Swamy P, Kuramoto L, Guy
P, et al: Prognostic factors of in-hospital complications after hip
fracture surgery: A scoping review. Osteoporos Int. 30:1339–1351.
2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Eschbach D, Bliemel C, Oberkircher L,
Aigner R, Hack J, Bockmann B, Ruchholtz S and Buecking B: One-year
outcome of geriatric hip-fracture patients following prolonged ICU
treatment. Biomed Res Int. 2016(8431213)2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Cohn MR, Cong GT, Nwachukwu BU, Patt ML,
Desai P, Zambrana L and Lane JM: Factors associated with early
functional outcome after hip fracture surgery. Geriatr Orthop Surg
Rehabil. 7:3–8. 2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
World Health Organization. International
Statistical Classification of Diseases and Related Health Problems.
10 edition. World Health Organization, Geneva, 2016.
|
|
32
|
World Health Organization. International
Classification of Diseases, Ninth Revision, Clinical Modification
(ICD-9-CM). National Center for Health Statistics, Hyattsville, MD,
2011.
|
|
33
|
Carpintero P, Caeiro JR, Carpintero R,
Morales A, Silva S and Mesa M: Complications of hip fractures: A
review. World J Orthop. 5:402–411. 2014.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Jo YY, Park CG, Lee JY, Kwon SK and Kwak
HJ: Prediction of early postoperative desaturation in extreme older
patients after spinal anesthesia for femur fracture surgery: A
retrospective analysis. Korean J Anesthesiol. 72:599–605.
2019.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Cecchi F, Pancani S, Antonioli D, Avila L,
Barilli M, Gambini M, Landucci Pellegrini L, Romano E, Sarti C,
Zingoni M, et al: Predictors of recovering ambulation after hip
fracture inpatient rehabilitation. BMC Geriatr.
18(201)2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Gonzalez de Villaumbrosia C, Barba R,
Ojeda-Thies C, Grifol-Clar E, Alvarez-Diaz N, Alvarez-Espejo T,
Cancio-Trujillo JM, Mora-Fernández J, Pareja-Sierra T,
Barrera-Crispín R, et al: Predictive factors of gait recovery after
hip fracture: A scoping review. Age Ageing.
54(afaf057)2025.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Foss NB, Kristensen MT and Kehlet H:
Anaemia impedes functional mobility after hip fracture surgery. Age
Ageing. 37:173–178. 2008.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Kim JL, Jung JS and Kim SJ: Prediction of
ambulatory status after hip fracture surgery in patients over 60
years old. Ann Rehabil Med. 40:666–674. 2016.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Malik AT, Quatman-Yates C, Phieffer LS, Ly
TV, Khan SN and Quatman CE: Factors associated with inability to
bear weight following hip fracture surgery: An analysis of the
ACS-NSQIP Hip fracture procedure targeted database. Geriatr Orthop
Surg Rehabil. 10(2151459319837481)2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Xiang Z, Chen Z, Wang P, Zhang K, Liu F,
Zhang C, Wong TM, Li W and Leung F: The effect of early
mobilization on functional outcomes after hip surgery in the
Chinese population-A multicenter prospective cohort study. J Orthop
Surg (Hong Kong). 29(23094990211058902)2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Goubar A, Martin FC, Potter C, Jones GD,
Sackley C, Ayis S and Sheehan KJ: The 30-day survival and recovery
after hip fracture by timing of mobilization and dementia: A UK
database study. Bone Joint J. 103-B:1317–1324. 2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Manosroi W, Koetsuk L, Phinyo P,
Danpanichkul P and Atthakomol P: Predictive model for prolonged
length of hospital stay in patients with osteoporotic femoral neck
fracture: A 5-year retrospective study. Front Med (Lausanne).
9(1106312)2022.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Vittinghoff E and McCulloch CE: Relaxing
the rule of ten events per variable in logistic and Cox regression.
Am J Epidemiol. 165:710–718. 2007.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Peduzzi P, Concato J, Kemper E, Holford TR
and Feinstein AR: A simulation study of the number of events per
variable in logistic regression analysis. J Clin Epidemiol.
49:1373–1379. 1996.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Sperandei S: Understanding logistic
regression analysis. Biochem Med (Zagreb). 24:12–18.
2014.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Bursac Z, Gauss CH, Williams DK and Hosmer
DW: Purposeful selection of variables in logistic regression.
Source Code Biol Med. 3(17)2008.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Chowdhury MZI and Turin TC: Variable
selection strategies and its importance in clinical prediction
modelling. Fam Med Community Health. 8(e000262)2020.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Munoz-Pichardo JM, Pino-Mejias R,
Garcia-Heras J, Ruiz-Munoz F and Luz Gonzalez-Regalado M: A
multivariate Poisson regression model for count data. J Appl Stat.
48:2525–2541. 2021.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Charlson ME, Carrozzino D, Guidi J and
Patierno C: Charlson comorbidity index: A critical review of
clinimetric properties. Psychother Psychosom. 91:8–35.
2022.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Kim JH: Multicollinearity and misleading
statistical results. Korean J Anesthesiol. 72:558–569.
2019.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Tomaschek F, Hendrix P and Baayen RH:
Strategies for addressing collinearity in multivariate linguistic
data. J Phon. 71:249–267. 2018.
|
|
52
|
Andaloro S, Cacciatore S, Risoli A, Comodo
RM, Brancaccio V, Calvani R, Giusti S, Schlögl M, D'Angelo E,
Tosato M, et al: Hip fracture as a systemic disease in older
adults: A narrative review on multisystem implications and
management. Med Sci (Basel). 13(89)2025.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Hulsbæk S, Larsen RF and Troelsen A:
Predictors of not regaining basic mobility after hip fracture
surgery. Disabil Rehabil. 37:1739–1744. 2015.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Gray R, Lacey K, Whitehouse C, Dance R and
Smith T: What factors affect early mobilisation following hip
fracture surgery: A scoping review. BMJ Open Qual. 12 (Suppl
2)(e002281)2024.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Magaziner J, Chiles N and Orwig D:
Recovery after Hip fracture: Interventions and their timing to
address deficits and desired outcomes-evidence from the baltimore
hip studies. Nestle Nutr Inst Workshop Ser. 83:71–81.
2015.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Monkuntod K, Aree-Ue S and Roopsawang I:
Associated factors of functional ability in older persons
undergoing hip surgery immediately post-hospital discharge: A
prospective study. J Clin Med. 12(6258)2023.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Istianah U, Nurjannah I and Magetsari R:
Post-discharge complications in postoperative patients with hip
fracture. J Clin Orthop Trauma. 14:8–13. 2020.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Elli S, Contro D, Castaldi S, Fornili M,
Ardoino I, Caserta AV and Panella L: Caregivers' misperception of
the severity of hip fractures. Patient Prefer Adherence.
12:1889–1895. 2018.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Yoo JI, Lee YK, Koo KH, Park YJ and Ha YC:
Concerns for older adult patients with acute hip fracture. Yonsei
Med J. 59:1240–1244. 2018.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Iosifidis M, Iliopoulos E, Panagiotou A,
Apostolidis K, Traios S and Giantsis G: Walking ability before and
after a hip fracture in elderly predict greater long-term
survivorship. J Orthop Sci. 21:48–52. 2016.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Adulkasem N, Phinyo P, Khorana J,
Pruksakorn D and Apivatthakakul T: Prognostic factors of 1-year
postoperative functional outcomes of older patients with
intertrochanteric fractures in Thailand: A retrospective cohort
study. Int J Environ Res Public Health. 18(6896)2021.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Kristensen MT: Factors affecting
functional prognosis of patients with hip fracture. Eur J Phys
Rehabil Med. 47:257–264. 2011.PubMed/NCBI
|
|
63
|
Handoll HH, Cameron ID, Mak JC, Panagoda
CE and Finnegan TP: Multidisciplinary rehabilitation for older
people with hip fractures. Cochrane Database Syst Rev.
11(CD007125)2021.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Ravi B, Pincus D, Choi S, Jenkinson R,
Wasserstein DN and Redelmeier DA: Association of duration of
surgery with postoperative delirium among patients receiving hip
fracture repair. JAMA Netw Open. 2(e190111)2019.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Tarrant SM, Attia J and Balogh ZJ: The
influence of weight-bearing status on post-operative mobility and
outcomes in geriatric hip fracture. Eur J Trauma Emerg Surg.
48:4093–4103. 2022.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Xu BY, Yan S, Low LL, Vasanwala FF and Low
SG: Predictors of poor functional outcomes and mortality in
patients with hip fracture: A systematic review. BMC Musculoskelet
Disord. 20(568)2019.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Wong RMY, Qin J, Chau WW, Tang N, Tso CY,
Wong HW, Chow SK, Leung KS and Cheung WH: Prognostic factors
related to ambulation deterioration after 1-year of geriatric hip
fracture in a Chinese population. Sci Rep. 11(14650)2021.PubMed/NCBI View Article : Google Scholar
|