Introduction
Mandibular invasion of oral squamous cell carcinoma
(OSCC) is a significant problem for oral surgeons. Such invasion
has a direct impact on surgical strategies and patient prognosis
(1). Although the final diagnosis
must be made through postoperative pathological examination,
mandibular invasion is most commonly suspected from pre-operative
radiography or computed tomography (2,3). In
clinical work, making a decision based on imaging alone is
sometimes difficult (4,5). Alternative methods for the
pre-operative detection of mandibular invasion are thus
required.
During bone invasion, osteoclasts still represent
the terminal cells for the absorption of bone. With malignant
lesions, osteoclasts are stimulated and activated through general
mechanisms. Certain cytokines, such as receptor activator of
nuclear factor-κB (RANK) ligand (RANKL), tumor necrosis factor
(TNF)-α, interleukin (IL)-1α and -6, parathyroid hormone-related
protein (PTHrP) and osteoprotegerin (OPG) are known to participate
in this process (6–8). Most research in this area has focused
on tissues adjacent to the bone. Biopsy samples have not commonly
been used due to their distance from bone. However, OSCC with the
ability to invade bone would presumably display telltale biological
characteristics even in superficial regions of the tumor from which
the biopsy is taken. Based on our previous research (9), this study examined the value of
osteoclast-related cytokines in biopsy specimens for predicting
mandibular invasion by OSCC using both immunohistochemical (IHC)
and tartrate-resistant acid phosphatase (TRAP) staining.
Materials and methods
Patients and specimens
In this retrospective study, biopsy specimens (when
available) were obtained from 30 patients with OSCC. Original tumor
locations were in the lower gingiva or oral floor. Background data
for patients are shown in Table I.
Diagnoses of OSCC and mandible invasion were based on serial slices
stained with H&E (10,11). Paraffin block biopsy specimens of
these 30 patients were retrieved and sliced into sections at a
thickness of 4 μm. All slices were inspected using digital images
captured using Axioplan2 and Axiophot2 microscopes (Carl Zeiss,
Jena, Germany).
 | Table I.General characteristics of the
patients. |
Table I.
General characteristics of the
patients.
| Gender | |
| Male | 21 |
| Female | 9 |
| Age (years) | |
| Range | 36-85 |
| Average | 64 |
| T stage | |
| 1 | 1 |
| 2 | 10 |
| 3 | 6 |
| 4 | 13 |
| N stage | |
| 0 | 9 |
| 1 | 11 |
| 2 | 10 |
| M (0) | 30 |
| Bone invasion | |
| Positive | 14 |
| Negative | 16 |
Immunohistochemical staining of
osteoclast-related cytokines
Seven antibodies against osteoclast-related
cytokines were used in this study: anti-IL-1α (Endogen, Woburn, MA,
USA), anti-IL-6 (Santa Cruz Biotechnology, Santa Cruz, CA, USA),
anti-OPG (R&D Systems, Minneapolis, MN, USA), anti-PTHrP (EMD
Chemicals, San Diego, CA, USA), anti-RANK (R&D Systems),
anti-RANKL (R&D Systems), and anti-TNF-α (goat anti-human
polyclonal antibody; R&D Systems).
Immunohistochemical analysis was performed using the
Streptomyces anti-biotin protein-peroxidase (SP) method with a
Histofine SAB-PO kit (Nichirei, Tokyo, Japan). Sections were
deparaffinized in xylene and rehydrated by serial incubation in a
graded ethanol series followed by washign in phosphate-buffered
saline (PBS). Antigen retrieval was performed by microwave heating
in 0.01 M citrate buffer at 95°C for 5 min. Endogenous peroxidase
activity was quenched by the addition of 3% hydrogen peroxide in
methanol for 15 min. After washing in PBS, sections were incubated
in normal rabbit serum for 30 min at room temperature to prevent
non-specific protein binding, then incubated with primary
antibodies diluted 1:100 in a humidified chamber at 37°C for 1 h.
Sequential incubations were then performed with biotin-labeled
secondary antibodies and peroxidase-labeled streptavidin at 37°C
for 30 min, in accordance with the instructions from the reagent
kit. The sections were washed thoroughly in PBS between two
incubations. A duration of 1–5 min was required to reveal brown
products with Histofine Simplestain DAB solution (Nichirei) under a
microscope. A section with PBS instead of the primary antibodies
was used as the negative control in every case. Slight
counterstaining with hematoxylin was performed as a final step.
Tartrate-resistant acid phosphatase
staining
The dewaxing and rehydrating procedures were the
same as those used in IHC staining. After washing with PBS, a TRAP
kit (Cell Garage, Tokyo, Japan) was used for TRAP staining.
Incubation lasted for 30–60 min at 37°C and was monitored under a
microscope. Hematoxylin was used to counterstain the cell
nucleus.
Double-staining with IHC and TRAP
staining
Double-stainings were performed to clarify the
relationships between TRAP-positive cells, osteoclasts and
pre-osteoclasts, and cytokine-positive cells upon IHC staining.
TRAP staining was performed just before antigen unmasking.
Subsequently, after washing with PBS, IHC staining was continued
following the above-mentioned protocol. Sections were dipped into
hematoxylin for the light conterstaining of nuclei.
Evaluation of positive-stained
tissues
Sections were reviewed independently with H&E
staining after IHC and TRAP staining. The characteristics and
locations of positive cells were recorded, and the rates were
calculated for positive H&E staining for each cytokine and for
TRAP staining, excluding the OPG cytokine. Positive rates of IHC
staining, TRAP staining and double-staining were compared to
histopathological diagnoses for uniformity. The diagnostic accuracy
of the staining for each cytokine and double-staining compared to
H&E staining was then determined according to a formula for
sensitivity and specificit. Positive and negative predictive values
of the dye applications were then calculated. A significant
correlation between the expression of these osteoclast-related
cytokines and mandibular invasion status was evaluated by the
Fisher's exact test. A value of P<0.05 indicated a significant
difference.
Results
Staining and statistical results in
gingival or oral floor OSCC
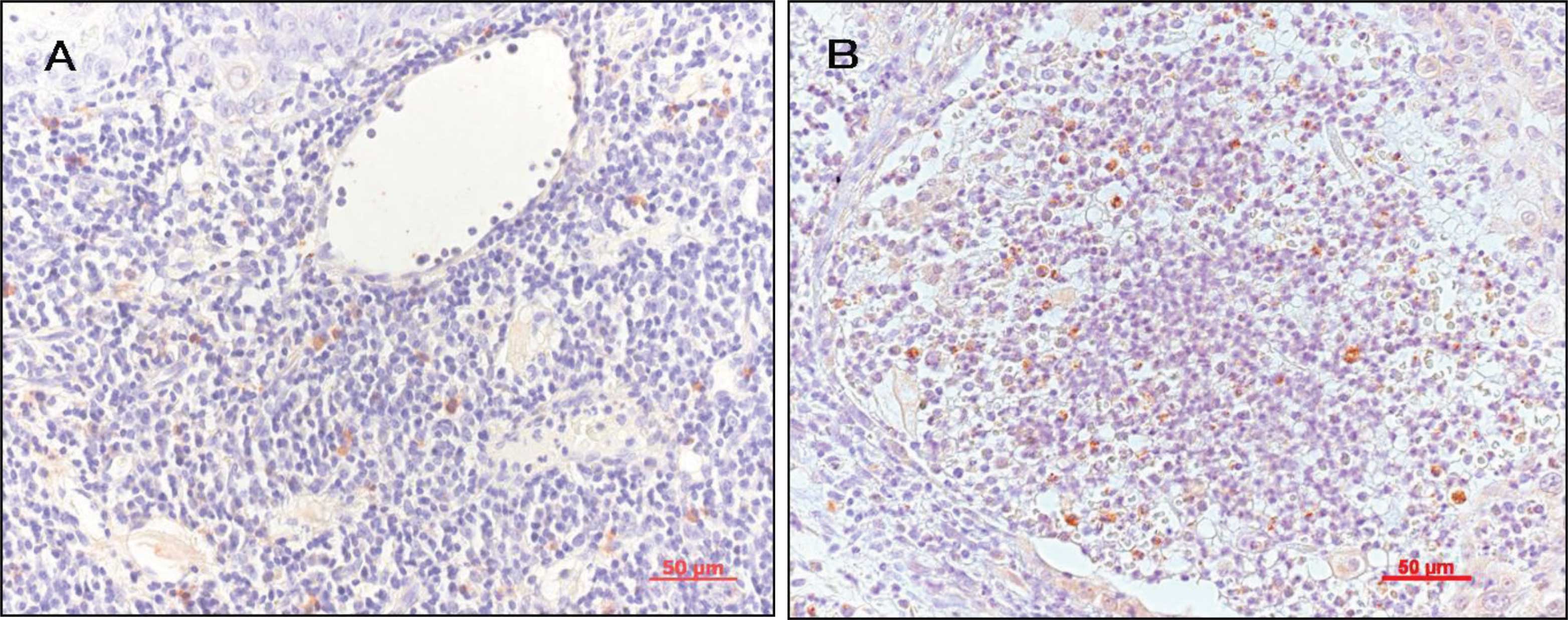
IHC staining revealed positive-stained cells in the
specimens as follows: IL-1α, lymphocytes; RANKL, stromal cell-like
cells and lymphocytes; PTHrP, tumor cells; OPG, stromal cell-like
cells; IL-6, lymphocytes; RANK, osteoclast-like cells; and TNF-α,
tumor cells and lymphocytes. Fig.
1 illustrates the positive staining for the expression of RANKL
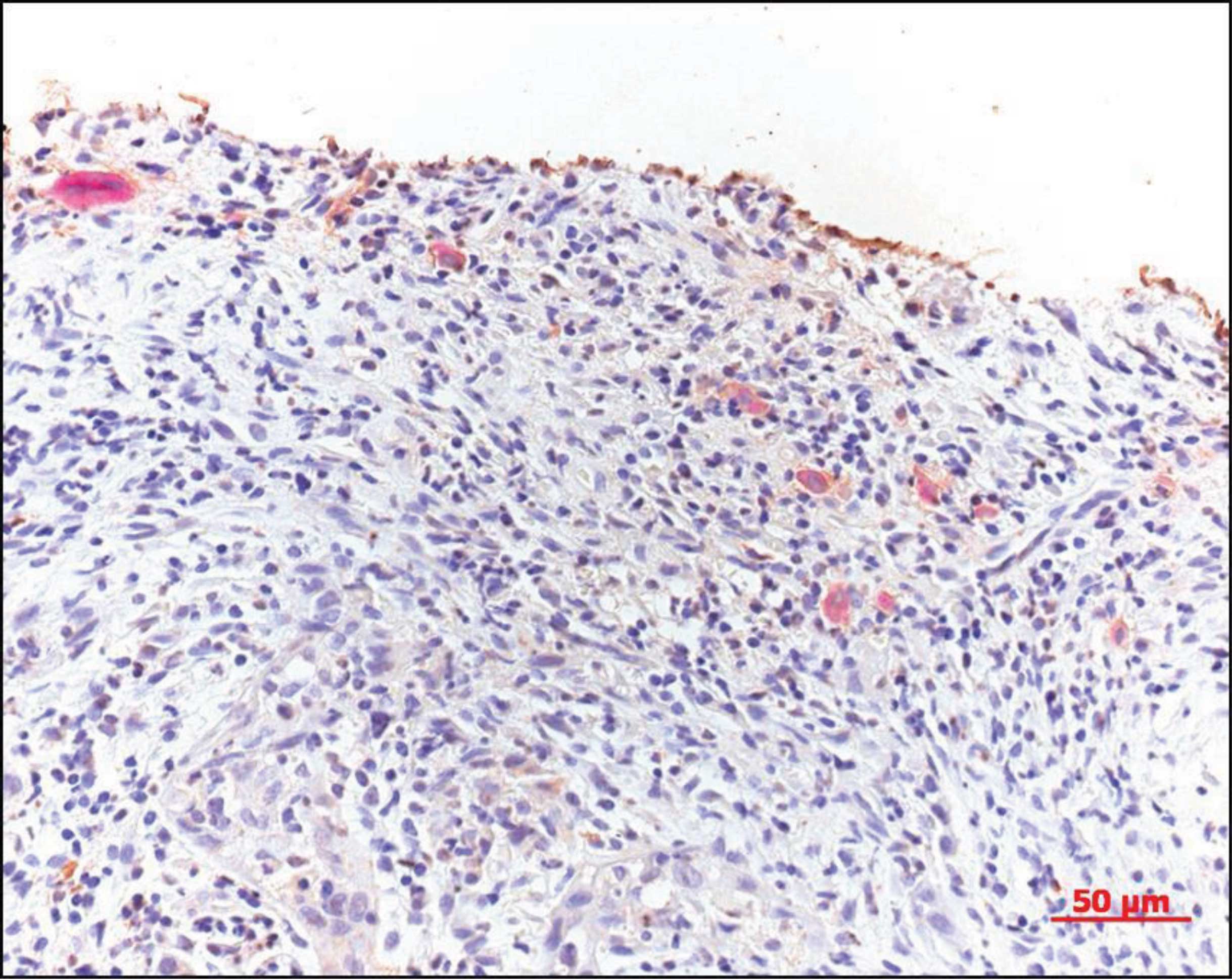
and IL-1α. Fig. 2 shows that the
positive results for TRAP staining included monocytes,
pre-osteoclast-like and osteoclast-like cells. Some TRAP-positive
cells were observed in the epithelium of capillaries in the tumor
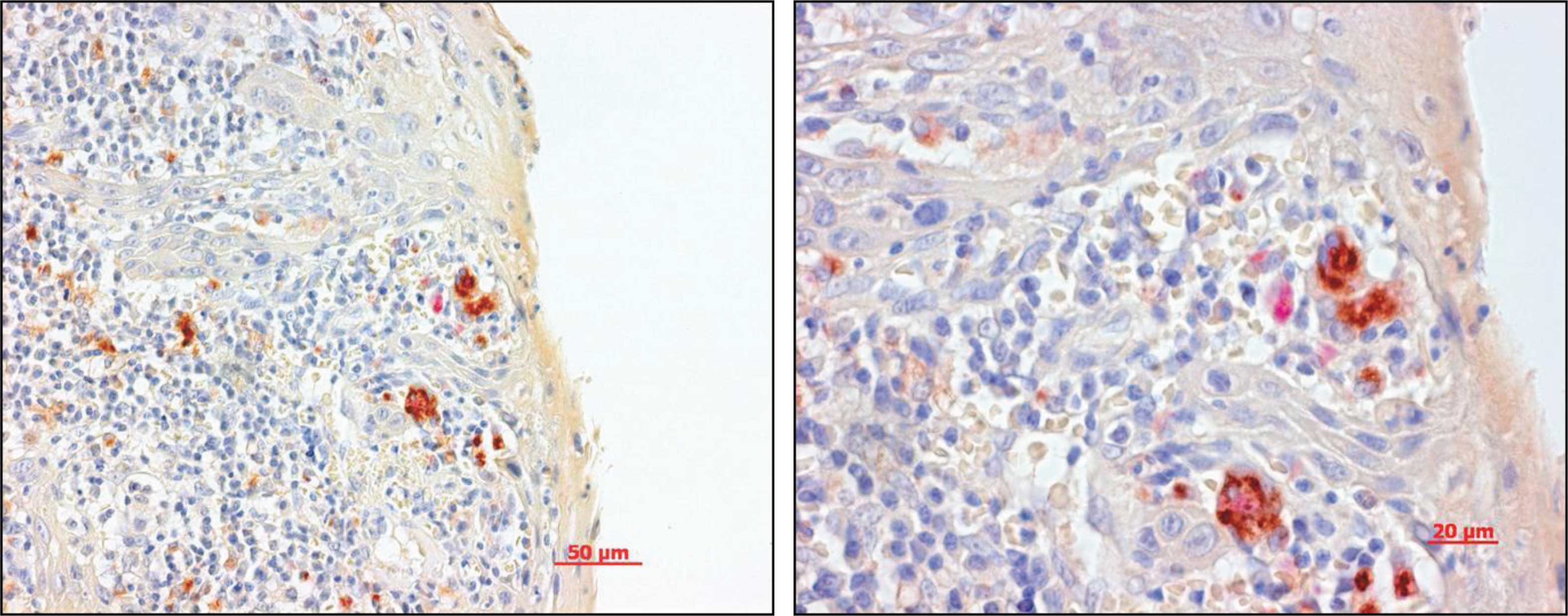
tissues. Fig. 3 shows the positive
results for IHC and TRAP staining. The antibody of the cytokine was
IL-1α. It was possible to distinguish between ICH-positive and
TRAP-positive cells.
Diagnostic accuracy of cytokine IHC
staining
Positive rates of IHC staining in bone invasive OSCC
were: IL-1α, 62.5%; IL-6, 37.5%; OPG, 90%; RANK, 80%; RANKL, 83.3%;
PTHrP, 88.9% and TNF-α, 55.6%. The positive predictive value of
IL-1α, IL-6, RANK, PTHrP was higher than that of the other
cytokines, and the negative predictive value of IL-1α, OPG, RANK,
RANKL, PTHrP was higher than that of the other cytokines. IL-1α,
RANK and PTHrP were shown to have better uniformity than the other
cytokines (Table II). There was
significant correlation between the expression of IL-1α, OPG,
RANKL, PTHrP and mandibular invasion status (P<0.05). While most
OSCC samples with positive staining of IL-1α, RANKL and PTHrP had
bone invasion, tumors without invasive lesions were negative for
these osteoclast-related cytokines. In contrast, most of the
OPG-negative-stained cases significantly exhibited bone
invasion.
 | Table II.The diagnostic accuracy of the
cytokines. |
Table II.
The diagnostic accuracy of the
cytokines.
| Bone invasion (by
H&E)
| P-valuea | Specificity | Sensitivity | Positive predictive
value | Negative predictive
value |
|---|
| + | − | Total |
|---|
| IL-1α | | | | | | | | |
| + | 5 | 0 | 5 | | | | | |
| − | 3 | 11 | 14 | 0.0048 | 1 | 0.63 | 1 | 0.79 |
| 8 | 11 | 19 | | | | | |
| IL-6 | | | | | | | | |
| + | 3 | 1 | 4 | | | | | |
| − | 5 | 9 | 14 | 0.2745 | 0.90 | 0.38 | 0.75 | 0.64 |
| 8 | 10 | 18 | | | | | |
| OPG | | | | | | | | |
| + | 9 | 5 | 14 | | | | | |
| − | 1 | 13 | 14 | 0.0044 | 0.72 | 0.90 | 0.64 | 0.93 |
| 10 | 18 | 28 | | | | | |
| RANK | | | | | | | | |
| + | 4 | 1 | 5 | | | | | |
| − | 1 | 6 | 7 | 0.0720 | 0.86 | 0.8 | 0.80 | 0.86 |
| 5 | 7 | 12 | | | | | |
| RANKL | | | | | | | | |
| + | 10 | 7 | 17 | | | | | |
| − | 2 | 11 | 13 | 0.0256 | 0.61 | 0.83 | 0.59 | 0.85 |
| 12 | 18 | 30 | | | | | |
| PTHrP | | | | | | | | |
| + | 8 | 1 | 9 | | | | | |
| − | 1 | 10 | 11 | 0.0009 | 0.91 | 0.89 | 0.89 | 0.91 |
| 9 | 11 | 20 | | | | | |
| TNF-α | | | | | | | | |
| + | 5 | 2 | 7 | | | | | |
| − | 4 | 9 | 13 | 0.1597 | 0.82 | 0.56 | 0.71 | 0.69 |
| 9 | 11 | 20 | | | | | |
Diagnostic accuracy of double-staining
using IHC and TRAP staining
All double-positive tissues for IHC and TRAP
staining were H&E invasion-positive, and all double-negative
tissues were H&E invasion-negative. The diagnostic accuracy was
a complete match for the positive tissues concerning the expression
of each of the cytokines and TRAP (Table III).
 | Table III.The diagnostic accuracy of the double
staining. |
Table III.
The diagnostic accuracy of the double
staining.
| Bone
invasiona
| P-valueb |
|---|
| + | − | Total |
|---|
| IL-1α + TRAP | | | | |
| + | 5 | 0 | 5 | |
| − | 0 | 9 | 9 | 0.0005 |
| 5 | 9 | 14 | |
| IL-6 + TRAP | | | | |
| + | 3 | 0 | 3 | |
| − | 0 | 7 | 7 | 0.0083 |
| 8 | 10 | 18 | |
| OPG + TRAP | | | | |
| + | 10 | 0 | 10 | |
| − | 0 | 12 | 12 | <0.0001 |
| 10 | 12 | 22 | |
| RANK + TRAP | | | | |
| + | 3 | 0 | 3 | |
| − | 0 | 1 | 1 | 0.0250 |
| 3 | 1 | 4 | |
| RANKL + TRAP | | | | |
| + | 10 | 0 | 10 | |
| − | 0 | 10 | 10 | <0.0001 |
| 10 | 10 | 20 | |
| PTHrP + TRAP | | | | |
| + | 8 | 0 | 8 | |
| − | 0 | 8 | 8 | 0.0002 |
| 8 | 8 | 16 | |
| TNF-α + TRAP | | | | |
| + | 5 | 0 | 5 | |
| − | 0 | 7 | 7 | 0.0013 |
| 5 | 7 | 12 | |
Discussion
The more information obtained pre-operatively
regarding the patient and disease, the better the outlook is for
treatment and prognosis. In cases of OSCC, determining whether
mandibular invasion has occurred is critical for the oral surgeon.
Clinical features and medical imaging modalities, such as
radiography, computed tomography and magnetic resonance imaging,
are commonly used in this situation. However, the sensitivity and
specificity of these systems remain problematic (2,4).
Ideally, determination of mandibular invasion should be performed
using a highly sensitive and specific test that is both inexpensive
and non-invasive.
Pre-operative biopsy indicates certain
characteristics of the tumor. However, in cases of OSCC with
potential mandibular invasion, estimating invasion based solely on
an H&E-stained biopsy specimen is difficult, since the
interface between the carcinoma and bone is not directly
distinguishable (10). Research to
determine whether osteoclast-related cytokines show relationships
between carcinoma and bone has revealed that some cytokines play
important roles in the mandibular invasion of OSCC (6). We therefore aimed to ascertain
whether these cytokines in biopsy specimens can predict bone
invasion.
Many cytokines participate in osteoclast
differentiation and activation. RANKL, RANK and OPG are regarded as
the basic cytokines influencing the entire process. Other
cytokines, such as TNF-α, IL-1α and PTHrP, have also been found to
exert certain effects on osteoclasts (12,13).
The present study found that all of the investigated 7 cytokines in
the biopsy samples of gingival OSCC indicated mandibular
invasion.
In the TRAP staining, the positive cells consisted
of monocytes, pre-osteoclasts and osteoclasts. These cells are
believed to be in the early stages of osteoclast maturation
(14). In carcinomas with the
potential for bone invasion, tumor cells express factors that allow
further maturation of pre-osteoclasts. When this does not occur,
the pre-osteoclasts remain in an early stage. This may be why the
TRAP-positive cells were observed in both the invasion-positive and
invasion-negative specimens. However, only tumor tissues with the
ability to express sufficient osteoclast-related cytokines promote
preosteoclasts and osteoclasts to differentiate and activate.
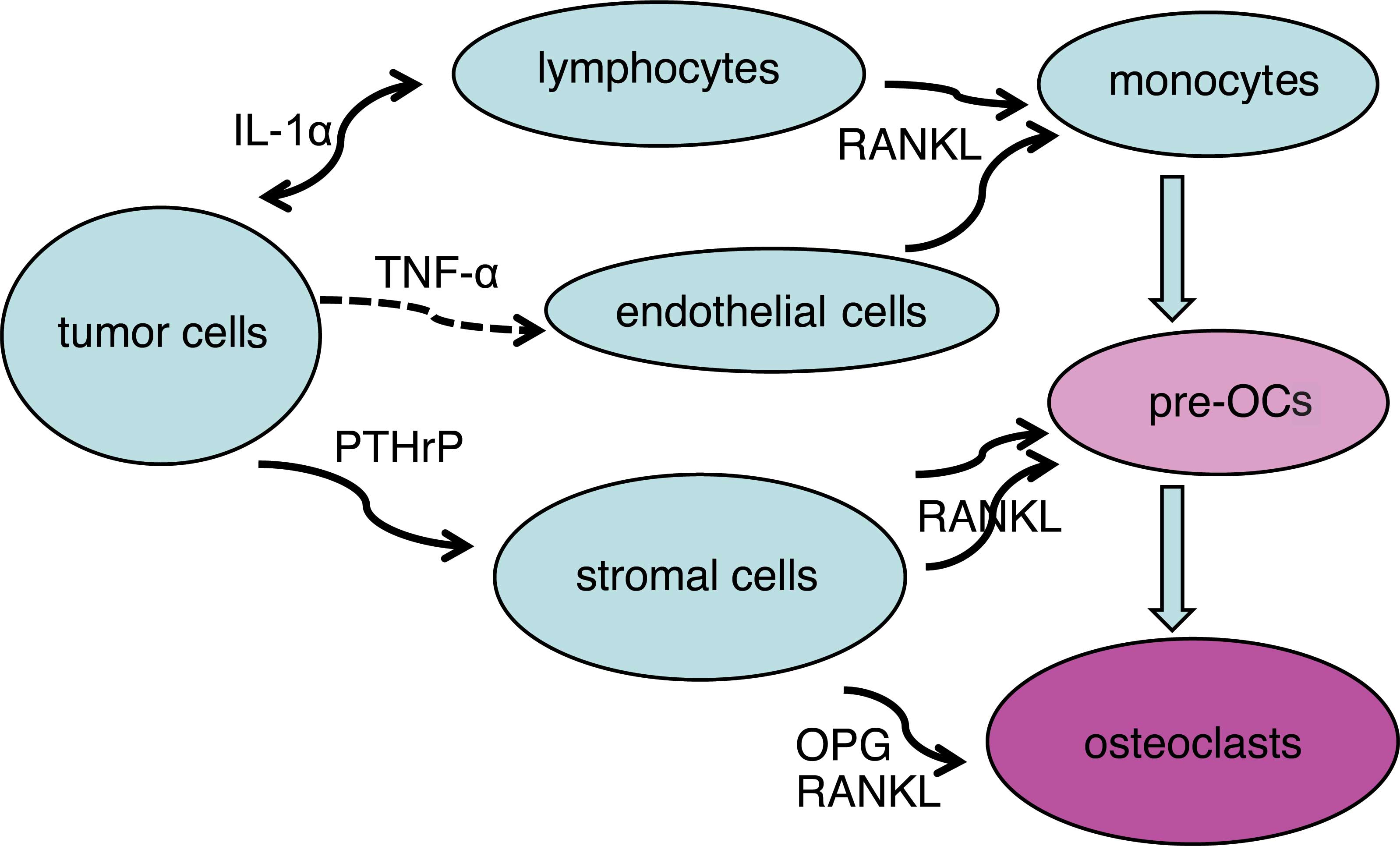
Based on the percentage of positive cells for each
cytokine, we hypothesized a network of tumor cells, osteoclasts and
other cells connected with cytokines (Fig. 4). Bone-invasive tumor cells
expressed TNF-α, IL-1α and PTHrP. These cytokines have been found
to influence lymphocytes and endothelial cells to induce monocyte
migration from blood vessels and differentiation into
pre-osteoclasts via RANKL, which is expressed by capillary
endothelial cells in the tumor (15). Stromal cells and osteoblasts, which
are also influenced by tumor-expressed cytokines, regulate the
differentiation and activation of pre-osteoclasts and osteoclasts
via RANKL and OPG.
Statistical analysis of the diagnostic uniformity of
the bone invasion according to H&E-stained sections revealed
significant correlations with invasiveness for RANKL, IL-1α, PTHrP
and OPG. Ranked in descending order according to diagnostic
accuracy, these four cytokines were PTHrP, IL-1α, OPG and RANKL.
Based on these results, negative staining for OPG was used due to
the negative correlation with bone invasion. However, to exclude
the presence of the antibody based solely on negative results from
IHC staining was not possible, therefore a negative finding for OPG
was considered unsuitable for diagnosis. The remaining three
cytokines, PTHrP, IL-1α and RANKL, were closly associated with bone
invasion and demonstrated diagnostic potential.
In both physical and pathological situations, bone
resorption is performed by osteoclasts. The number, the
differentiation and the activation of osteoclasts are directly
related to the outcome of bone resorption. Cytokines regulating
osteoclast activity thus participate in this process. IHC and TRAP
staining was carried out together in one section. The location and
relationship of the cytokine-expressing and osteoclast-like cells
were revealed more clearly and directly in this investigation.
Cytokine-negative cells were so close to TRAP-positive cells that
some cells exhbited staining in two colors, and cytokines, such as
RANKL, IL-1α and PTHrP, were confirmed to be strong regulators of
mandibular invasion by OSCC. In cases of OSCC showing bone
invasion, TRAP-positive osteoclasts were previously identified at
the interface between tumor and bone (9). In the present study, TRAP-positive
cells, pre-osteoclasts and osteoclast-like cells were noted in the
biopsy tissues only in specimens with bone invasion, and not in
invasion-negative specimens. Some TRAP-positive cells were found in
the walls of tumor capillaries, indicating that certain
pre-osteoclasts may have originated from the circulation. Such
cells would be induced by various factors in cancer tissue to pass
through the capillary endothelium, where they then activate and
differentiate into functional osteoclasts.
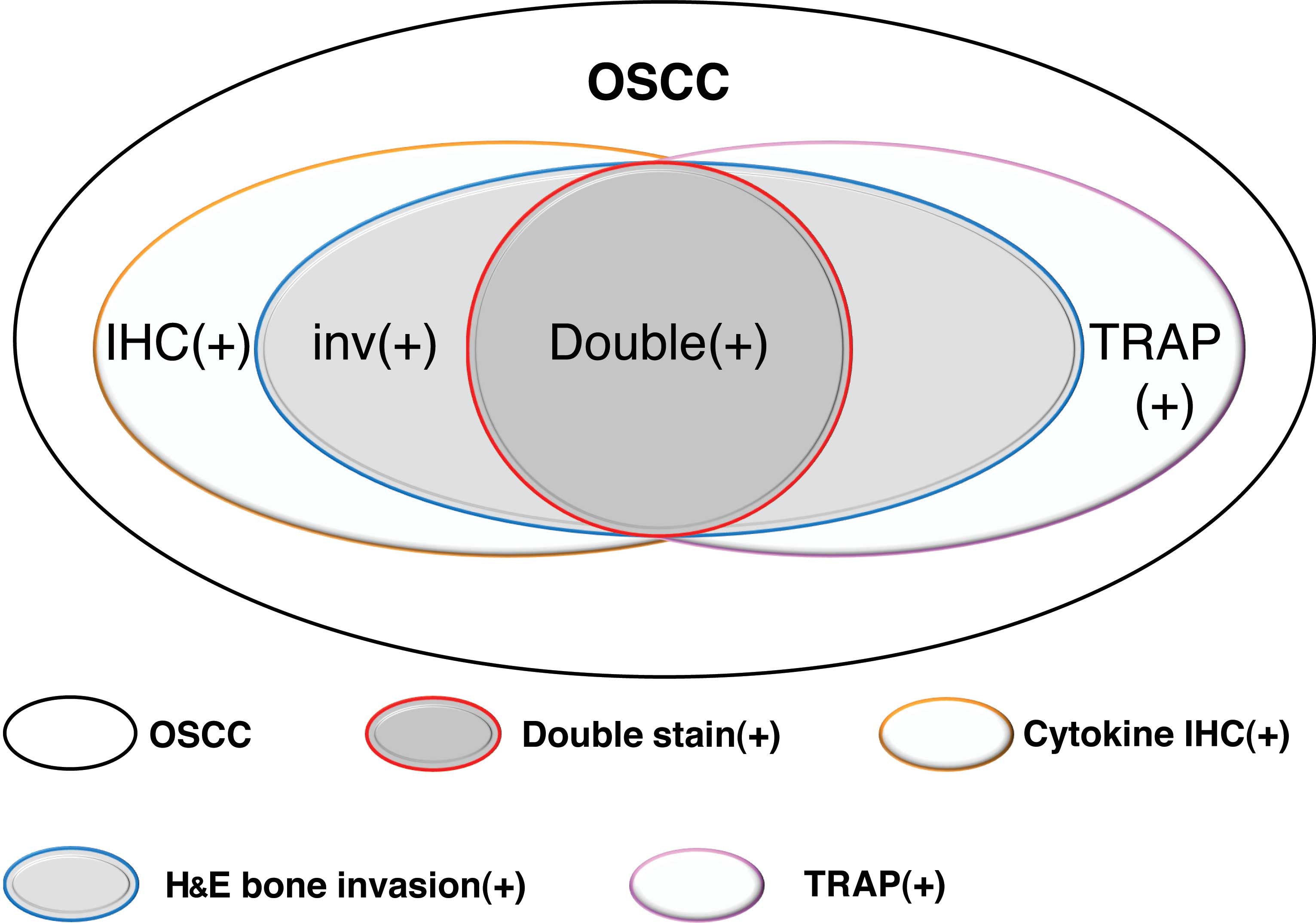
In cytokine IHC and TRAP double-staining, when the
result was double-positive or double-negative, the sensitivity and
specificity were 100%. This means that double-staining offers high
diagnostic value for mandibular invasion by OSCC. However, samples
showing single-positive results sometimes indicated bone invasion
and sometimes not. Thus, the use of double-staining as a diagnostic
criterion resulted in some false-negatives, but no false-positives
(Fig. 5).
As previously mentioned, IHC and TRAP staining of
biopsy specimens offered a certain diagnostic value for the
prediction of mandibular invasion by OSCC. This may be divided into
three levels of certainty: i) double-positive or double-negative,
definite diagnosis of invasion or non-invasion; ii) positive IHC
staining for PTHrP, IL-1α or RANKL, most of the specimens represent
bone invasion; iii) positive IHC staining for other cytokines or
TRAP staining only, combining clinical features and medical imaging
would offer a better indication of possible bone invasion.
Originally, gingiva is placed in an inflammatory
milieu. It is a non-specific environment which is common in all
adults, in particular the elderly. However, the gingival
environment in the case of gingival cancer with bone invasion may
be considered a specific environment or a ‘further exacerbation of
inflammation’. In other words, it is assumed to present the
‘further increased expression of osteoclastic cytokines’. In this
study, we evaluated the exacerbation of the inflammatory reaction
in gingival cancer with bone invasion by scoring IHC staining,
using gingival cancer without bone invasion as the control. A
stronger expression of inflammatory cytokines (osteoclastic
cell-induced cytokines) and osteoclastic cells was noted in the
bone invasion group. The stronger inflammatory reaction was not
caused simply by the gingival cancer, but by the presence of bone
invasion. This was considered to be a specific inflammatory
reaction, which was not observed in specimens of ordinary
gingiva.
The establishment of novel screening techniques for
the detection of mandibular invasion before treatment is needed.
OSCC, which has the potential for mandibular invasion, demonstrates
more invasive biological characteristics. Whether such invasive
potential is associated with metastatic potential represents a
question for future study (16).
In conclusion, the expression of both osteoclasts and
osteoclast-related cytokines is an important factor for the
prediction of mandibular invasion.
Acknowledgements
This study was supported by a research
grant from the Ministry of Education, Science and Culture,
Japan.
References
|
1.
|
Genden EM, Rinaldo A, Jacobson A, Shaha
AR, Suarez C, Lowry J, Urguhart AC, Werner JA, Gullane PJ and
Ferlito A: Management of mandibular invasion: when is a marginal
mandibulectomy appropriate? Oral Oncol. 41:776–782. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Nakayama E, Yoshiura K, Ozeki S, Nakayama
H, Yamaguchi T, Yoshikawa H, Kanda S, Ohishi M and Shirasuna K: The
correlation of histological features with a panoramic radiography
pattern and a computed tomography pattern of bone destruction in
carcinoma of the mandibular gingival. Oral Surg Oral Med Oral
Radiol Endod. 96:774–782. 2003. View Article : Google Scholar
|
|
3.
|
Brockenbrough JM, Petruzzelli GJ and
Lomasney L: Dentascan as an accurate method of predicting
mandibular invasion in patients with squamous cell carcinoma of
oral cavity. Arch Otolaryngol Head Neck Surg. 129:113–117. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Imaizumi A, Yoshino N, Yamada I, Nagumo K,
Amagasa T, Omura K, Okada N and Kurabayashi T: A potential pitfall
of MR imaging for assessing madibular invasion of squamous cell
carcinoma in oral cavity. Am J Neuroradiol. 27:114–122.
2006.PubMed/NCBI
|
|
5.
|
Ash CS, Nason RW, Abdoh AA and Cohen M:
Prognostic implication of mandibular invasion in oral cancer. Head
Neck. 22:794–798. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Shibahara T, Nomura T, Cui NH and Noma H:
A study of osteoclast-related cytokines in mandibular invasion by
squamous cell carcinoma. Int J Oral Maxillofac Surg. 34:789–793.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Tada T, Jimi E, Okamoto M, Ozeki S and
Okabe K: Oral squamous cell carcinoma cells induce osteoclast
differentiation by suppression of osteoprotegerin expression in
osteoblasts. Int J Cancer. 116:253–262. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Dunne FP, Bowden SJ, Brown JS, Ratcliffe
WA and Browne RM: Parathyroid hormone related protein in oral
squamous cell carcinomas invading the mandible. J Clin Pathol.
48:300–303. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Cui N, Nomura T, Noma H, Yokoo K, Takagi
R, Hashimoto S, Okamoto M, Sato M, Yu G, Guo C and Shibahara T:
Effect of YM529 on a model of mandibular invasion by oral squamous
cell carcinoma in mice. Clin Cancer Res. 11:2713–2719. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Lukinmaa PL, Hietanen J, Söderholm AL and
Lindgvis C: The histologic pattern of bone invasion by squamous
cell carcinoma of the mandibular region. Br J Oral Maxillofac Surg.
30:2–7. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Brown JS, Lowe D, Kalavrezos N, D'Souza J,
Magennis P and Woolgar J: Patterns of invasion and routes of tumor
entry into the mandible by oral squamous cell carcinoma. Head Neck.
24:370–383. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Azuma Y, Kaji K, Katogi R, Takeshita S and
Kudo A: Tumor necrosis factor-alpha induces differentiation of and
bone resorption by osteoclasts. J Biol Chem. 275:4858–4864. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Kobayashi K, Takahashi N, Jimi E, Udagawa
N, Takami M, Kotake S, Nakagawa N, Kinosaki M, Yamaguchi K, Shima
N, Yasuda H, Morinaga T, Higashio K, Martin TJ and Suda T: Tumor
necrosis factor alpha stimulates osteoclast differentiation by a
mechanism independent of the ODF/RANKL-RANK interaction. J Exp Med.
191:275–286. 2000. View Article : Google Scholar
|
|
14.
|
Van de Wijingaert FP and Burger EH:
Demonstration of tartrate-resistant acid phosphatase in
un-decalcified, glycolmethacrylate-embedded mouse bone: a possible
marker for (pre) osteoclast identification. J Histochem Cytochem.
34:1317–1323. 1986.
|
|
15.
|
Cui NH, Zhang W, Wang EB, Wei MJ, Guo CB
and Yu GY: Osteoclastic bone destruction and its regulating factors
in oral squamous cell carcinoma. Beijing Da Xue Xue Bao. 39:30–32.
2007.PubMed/NCBI
|
|
16.
|
Jones DH, Nakashima T, Sanchez OH,
Kozieradzki I, Komarova SV, Sarosi I, Morony S, Rubin E, Sarao R,
Hojilla CV, Komnenovic V, Kong YY, Schreiber M, Dixon SJ, Sims SM,
Khokha R, Wada T and Penninger JM: Regulation of cancer cell
migration and bone metastasis by RANKL. Nature. 440:692–696. 2006.
View Article : Google Scholar : PubMed/NCBI
|