Introduction
For many years, particularly in view of the
increasingly ageing population in the Western world, haematologists
have had a profound interest in researching the the pathophysiology
and clinical relevance of anaemia in association with aging.
Despite the fact that numerous studies show a link between lower
haemoglobin levels and morbidity and/or mortality, this is also the
case for elevated or upper normal haemoglobin levels (1), which may be associated with secondary
polycythaemia; e.g., associated with underlying pulmonary or
cardiac disease, or resulting from increased blood viscosity as has
been reported with the use of erythropoiesis-stimulating agents,
which may increase the risk for thromboembolic events (2). Numerous studies have been carried out
on anaemia in distinct ethnic or geographic populations (3–8), in
children (9–12), elderly people (4,6,8,13)
and pregnant women (14).
Differences noted in such studies may not only be explained by
lifestyle and environmental factors, they may also and most
essentially be explained by different exclusion criteria that have
been used in these studies.
Presently, there are nearly 500 million (7%) adults
65 years or older in the world, but by 2030 this population will
double to 1 billion (12%) worldwide (15,16).
In Germany, the increasingly ageing population will be paralleled
by a continuously shrinking total population, which is currently
81.5 million (as reported for the year 2010) and which will
decrease to 77.4 million by the year 2030 and to 64.7 million by
2060. Thus, the number of people beyond the age of 65 currently
accounts for 20.6% of the total population (16.8 million) (2010),
while in 2030 this proportion will rise to 28.7% of the total
population, and in 2050 this percentage will climb to 33% of the
total German population (16).
This means that by the year 2050 the number of taxpayers in Germany
will roughly be equal to the number of people beyond the age of
65.
Since ageing is a process that results from the
accumulation of somatic damage, which increases the risk of
mortality (17), there is a
profound desire to assess the risk of mortality on the basis of
laboratory parameters. The evaluation of haemoglobin levels in the
elderly is a complex task, since it is difficulty to assess whether
a haemoglobin level beyond the normal range in a given individual
is the result of an underlying disease or whether it is a
phenomenon of the expression of age (4). Numerous factors have been described
as affecting blood counts in the elderly. Reduced numbers of
haematopoietic stem cells, the finite number of cell divisions
(18), a defect in progenitor cell
proliferation (19), the inability
to sufficiently mobilize such progenitors (6), and the lack of hormonal stimulation
or the reduced response to hormonal stimulation (20–23)
are a few examples of conditions that may concur with reduced
haemoglobin levels in the absence of an apparent illness.
Taking the current definition of the World Health
Organization, which defines anaemia as haemoglobin levels of ≤12.0
g/dl for women and ≤13.0 g/dl for men, we may run into a most
significant public health crisis in the near future. In view of the
fact that anaemia is a common and most frequently an underestimated
condition in the elderly, several key questions should be addressed
in order to better understand the following: i) to what extent
anaemia in the elderly is the result of pre-existing disorders, ii)
to what extent it predetermines potential subsequent morbidity, and
iii) to what extent public health improvements could make a
difference. In this context, it may be important to reflect on
whether the current definition of anaemia by the World Health
Organization is still adequate to define anaemia in the elderly, or
whether new definitions for different elderly subpopulations would
aid in more adequately describing the association of specific
haemoglobin levels in the context of actual patient morbidity.
Finally, but of equal importance, discussion should be initiated
regarding the appropriate management of anaemia in the elderly and
the economic implications to health care systems.
The objective of the study presented herein, was to
examine the influence of increasing age on peripheral blood
parameters obtained from hospitalized individuals with no known
haematological history and to identify criteria which could be
useful in the discussion of age-dependent reference values. Data
from 1,724 individuals in the age range between 18 and 101 years
were evaluated with particular consideration for red and white
blood cell parameters and platelet counts.
Materials and methods
Patients
The study population comprised 1,724 individuals
(908 women aged 18–101 years and 816 men aged 18–96 years) with no
known haematological history who were treated at the University of
Heidelberg Medical Center as inpatients or outpatients. All blood
samples were obtained using routine diagnostic procedures.
Haematological parameters and clinical chemistry were analyzed at
the University of Heidelberg Medical Center central laboratory.
Patients with a known malignant haematological or oncological
disease, with chronic infection or inflammation were excluded.
Patients with disorders affecting the kidneys, thyroid or stomach
as well as patients with a bleeding history, haemolysis or who had
been previously diagnosed to have anaemia were also excluded from
this study. All samples were anonymized, and all data were handled
confidentially. This study was carried out in accordance with the
local ethics committee in agreement with the Declaration of
Helsinki. The composition of the study population is outlined in
Table I.
 | Table I.Age-adjusted reference intervals for
women and men as calculated from age group-dependent mean values ±
2 SD (rows 3–9).a |
Table I.
Age-adjusted reference intervals for
women and men as calculated from age group-dependent mean values ±
2 SD (rows 3–9).a
| | Age (years)
|
|---|
| Reference values | 18–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80–89 | ≥90 |
|---|
| Women | | | | | | | | | | |
| Hb | 12–15 g/dl | 11.6 | 11.9 | 11.8 | 11.6 | 12.1 | 10.5 | 10.2 | 9.3 | 8.8 |
| | 15.0 | 15.3 | 14.9 | 15.0 | 15.3 | 15.3 | 14.8 | 14.9 | 14.3 |
| No. | | 36 | 105 | 115 | 114 | 121 | 100 | 120 | 112 | 50 |
| RBC | 4.0–5.2/pl | 3.8 | 3.9 | 3.8 | 3.7 | 3.8 | 3.4 | 3.3 | 3.0 | 2.8 |
| | 5.1 | 5.2 | 5.1 | 5.1 | 5.2 | 5.1 | 5.0 | 5.0 | 5.0 |
| No. | | 36 | 104 | 115 | 115 | 122 | 100 | 122 | 113 | 51 |
| Hct | 0.36–0.47 l/l | 0.33 | 0.34 | 0.34 | 0.33 | 0.35 | 0.31 | 0.29 | 0.26 | 0.25 |
| | 0.45 | 0.45 | 0.43 | 0.44 | 0.45 | 0.45 | 0.44 | 0.45 | 0.42 |
| No. | | 35 | 101 | 106 | 110 | 107 | 91 | 116 | 109 | 50 |
| MCV | 83–97 fl | 78.2 | 79.3 | 77.9 | 79.7 | 83.7 | 80.9 | 80.3 | 80.4 | 78.0 |
| | 94.7 | 94.0 | 97.2 | 98.3 | 97.7 | 97.3 | 97.8 | 97.6 | 102.1 |
| No. | | 33 | 103 | 111 | 112 | 113 | 101 | 122 | 109 | 49 |
| MCH | 27–33 pg | 26.9 | 27.3 | 26.4 | 27.3 | 28.1 | 27.6 | 26.9 | 27.0 | 26.1 |
| | 33.4 | 32.7 | 34.0 | 34.0 | 34.8 | 33.5 | 34.1 | 33.7 | 35.5 |
| No. | | 33 | 105 | 115 | 112 | 122 | 100 | 121 | 111 | 49 |
| Plt | 150–440/nl | 401.91 | 404.03 | 412.82 | 406.53 | 442.40 | 385.91 | 443.72 | 388.04 | 360.02 |
| | 157.18 | 160.03 | 175.79 | 156.15 | 179.04 | 146.15 | 122.37 | 125.33 | 117.79 |
| No. | | 35 | 103 | 114 | 114 | 117 | 99 | 119 | 113 | 50 |
| WBC | 4.0–10.0/nl | 2.2 | 3.9 | 3.6 | 3.7 | 4.6 | 3.2 | 4.5 | 4.2 | 4.0 |
| | 12.5 | 10.9 | 11.3 | 11.9 | 12.0 | 10.2 | 10.9 | 11.0 | 9.8 |
| No. | | 36 | 102 | 112 | 115 | 116 | 99 | 121 | 112 | 48 |
| Men | | | | | | | | | | |
| Hb | 13–17g/dl | 13.5 | 13.5 | 13.3 | 13.0 | 12.1 | 11.7 | 9.9 | 9.6 | 9.7 |
| | 17.5 | 16.9 | 17.0 | 16.7 | 16.6 | 16.3 | 16.0 | 14.9 | 14.8 |
| No. | | 19 | 98 | 109 | 115 | 102 | 101 | 104 | 113 | 20 |
| RBC | 4.3–6.1/pl | 4.3 | 4.4 | 4.3 | 4.3 | 3.9 | 3.7 | 3.3 | 3.0 | 2.9 |
| | 5.9 | 5.7 | 5.7 | 5.4 | 5.4 | 5.4 | 5.3 | 4.8 | 4.9 |
| No. | | 19 | 100 | 110 | 111 | 101 | 101 | 104 | 114 | 20 |
| Hct | 0.38–0.52 l/l | 0.40 | 0.39 | 0.38 | 0.37 | 0.35 | 0.34 | 0.29 | 0.27 | 0.28 |
| | 0.49 | 0.49 | 0.49 | 0.48 | 0.47 | 0.48 | 0.46 | 0.44 | 0.44 |
| No. | | 17 | 93 | 107 | 113 | 98 | 102 | 101 | 109 | 20 |
| MCV | 83–97 fl | 82.0 | 80.2 | 77.6 | 81.0 | 80.6 | 79.9 | 81.4 | 82.0 | 85.1 |
| | 90.8 | 94.6 | 96.2 | 95.3 | 98.8 | 100.1 | 97.2 | 100.7 | 98.4 |
| No. | | 18 | 100 | 113 | 115 | 99 | 104 | 100 | 109 | 20 |
| MCH | 27–33 pg | 28.3 | 27.7 | 27.3 | 28.2 | 27.9 | 27.7 | 27.5 | 26.9 | 28.8 |
| | 32.3 | 33.0 | 33.5 | 33.0 | 34.4 | 34.2 | 33.9 | 35.9 | 34.6 |
| No. | | 18 | 97 | 112 | 112 | 99 | 102 | 105 | 113 | 20 |
| Plt | 150–440/nl | 183.7 | 157.8 | 162.8 | 150.8 | 136.5 | 123.9 | 82.8 | 104.8 | 137.4 |
| | 342.0 | 336.7 | 366.9 | 366.9 | 377.6 | 374.7 | 385.2 | 307.2 | 292.7 |
| No. | | 18 | 99 | 111 | 113 | 101 | 99 | 102 | 110 | 20 |
| WBC | 4.0–10.0/nl | 3.7 | 4.0 | 4.4 | 4.2 | 4.3 | 3.9 | 4.1 | 4.2 | |
| | 11.5 | 11.8 | 11.2 | 10.9 | 11.4 | 11.8 | 11.1 | 10.5 | 4.99.8 |
| No. | | 18 | 100 | 110 | 112 | 99 | 100 | 104 | 108 | 20 |
Statistical procedures
Mean, median and standard deviation were calculated
for every haematological parameter in each study group. Outliers
were defined as arguments beyond the reference interval that
corresponded to the mean ± 2 standard deviations (SD), and were not
considered for the further calculation of mean values and SD.
Age-dependent reference ranges were proposed on the basis of the
95% confidence intervals (mean ± 2 SD) for a specific parameter in
a defined age group. The Kolmogorow-Smirnow test was carried out in
order to find out whether the included arguments follow a Gaussian
distribution. When a Gaussian distribution was confirmed, the
Student’s t-test was carried out in order to test for significant
differences. Alternatively, the Wilcoxon U-test was carried
out.
Results
The reference intervals for blood counts as used at
the University Medical Center Heidelberg and the new reference
intervals that were calculated by gender for specific age groups
are shown in Table I.
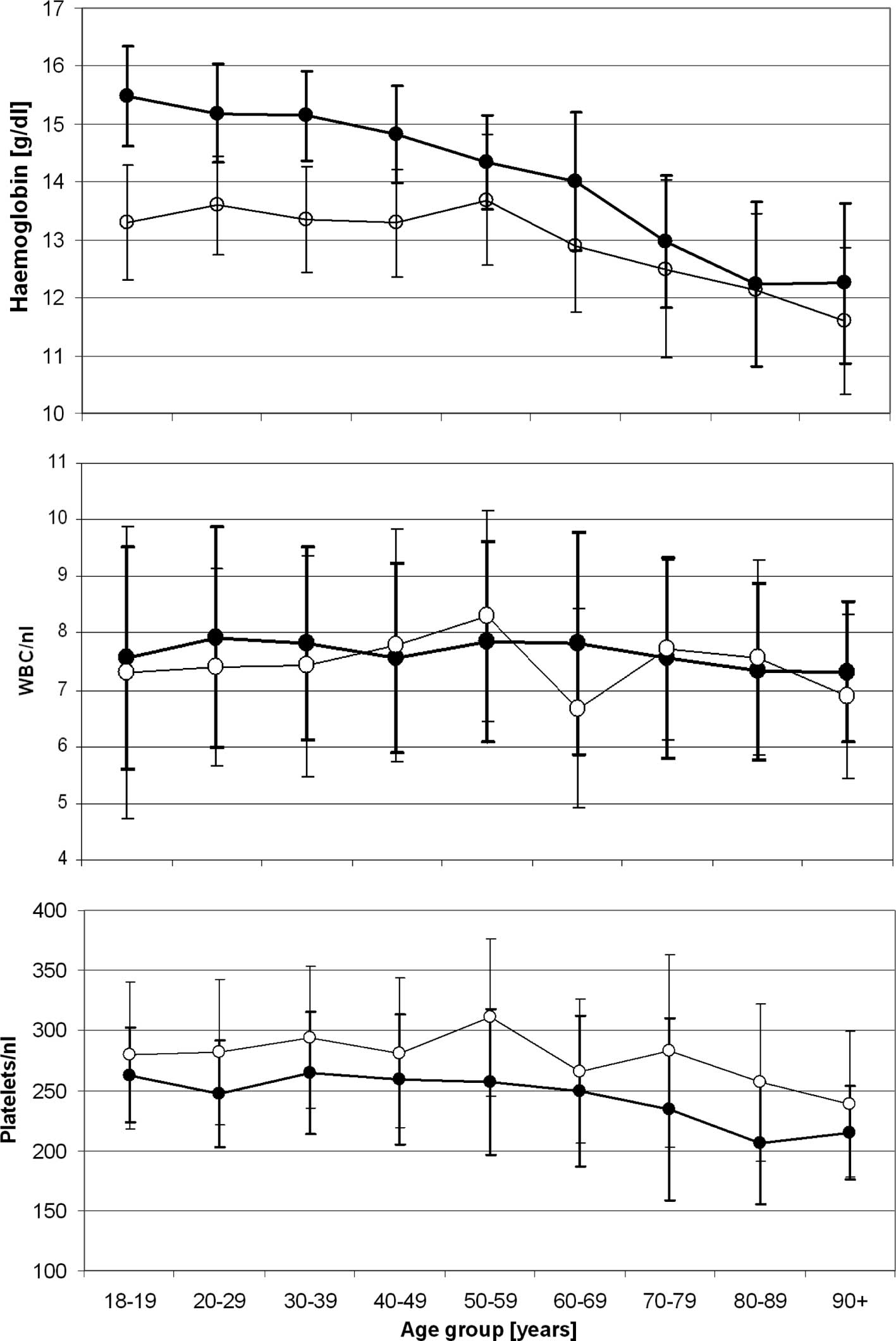
With the exception of platelet and neutrophil
counts, values were persistently higher in men than in women. These
gender differences were most prominent in the younger age groups,
and decreased continuously with increasing age. The most obvious
age-dependent changes were observed for erythropoiesis-related
parameters. A statistically significant (p<0.0001) age-dependent
decline in haemoglobin levels was observed for both genders
(Fig. 1). This decline was
paralleled by the decline in age-dependent haematocrit levels in
both genders (p<0.0001), and was more pronounced in men than in
women. We evaluated peripheral blood parameters from 1,724
hospitalised individuals between the ages of 18 and 101 years with
no known haematological history, who were admitted at the
University of Heidelberg Medical Center for a medical or surgical
condition. The average haemoglobin levels for men beyond the age of
70 and for women beyond the age of 80 were found to fulfil the WHO
criteria for the diagnosis of anaemia, which are set at haemoglobin
levels of ≤12.0 g/dl for women and ≤13.0 g/dl for men (Figs. 1 and 2). In contrast to haemoglobin,
erythrocyte counts and haematocrit, the values for mean corpuscular
volume (MCV) steadily increased in an age-dependent manner
(p<0.0001), while the age-dependent increase in mean corpuscular
haemoglobin levels was only statistically significant in males
(p>0.0001) and not in females (p=0.359) when individuals below
and beyond the age of 60 were compared.
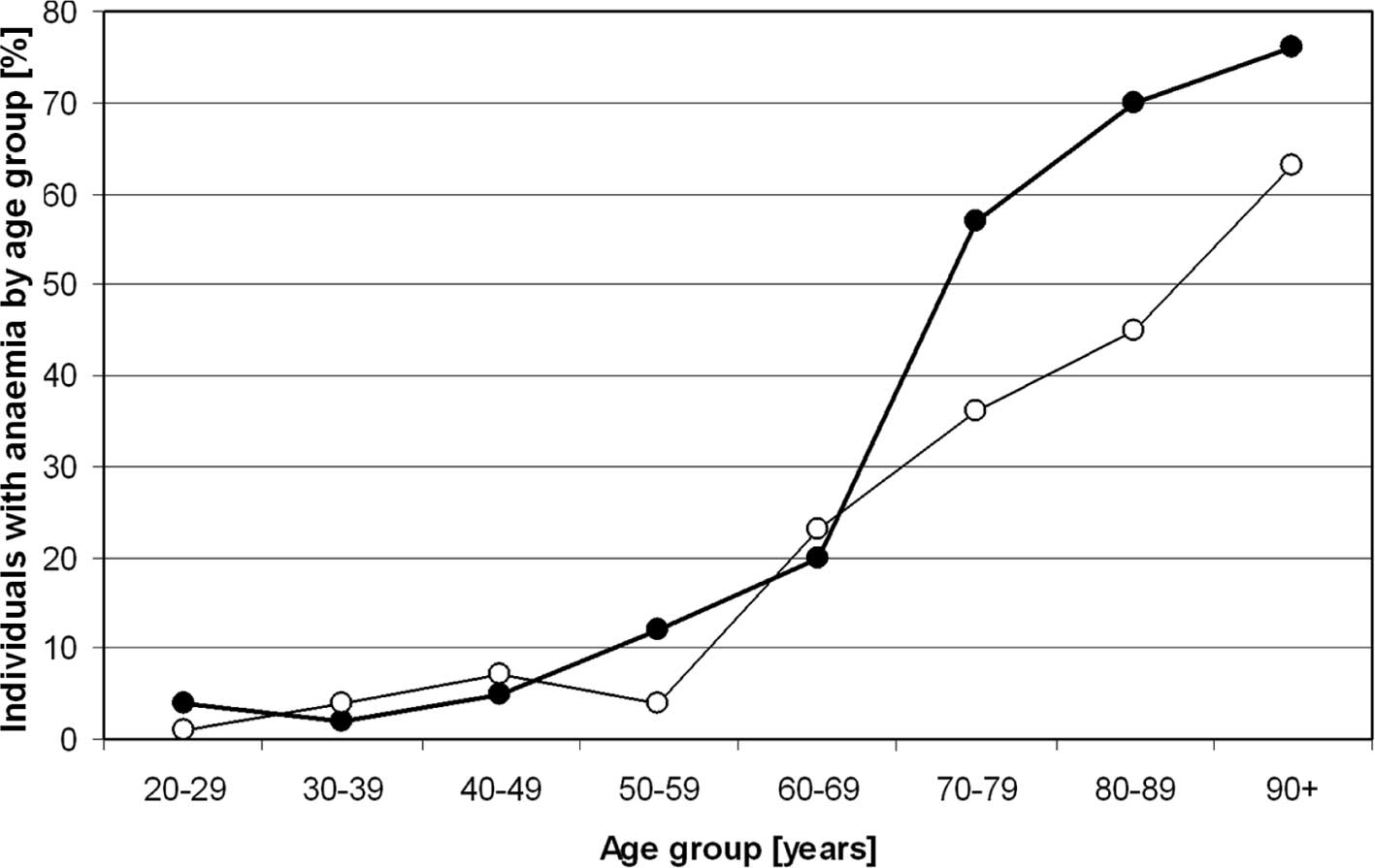
In our cohort, 23% of all women between 60 and 69
years of age were diagnosed as anaemic according to the WHO
criteria. This percentage increased to 36% in all female
individuals between 70 and 79 years of age and 45% in all female
individuals between 80 and 89 years of age. Sixty-three percent of
all female individuals beyond the age of 90 were anaemic by
definition. In the male population, these figures were even more
dramatic. In the age-range between 60 and 69 years, 20% fulfilled
the WHO criteria for anaemia, and 49% of all male individuals
between 70 and 79 years of age, 70% of all male individuals between
80 and 89 years of age and 76% of all male individuals beyond the
age of 90 were identified as anaemic according to the WHO criteria
for the diagnosis of anaemia (Fig.
2).
In contrast to almost all other haematopoiesis
parameters, which were higher in male individuals throughout all
age groups, platelet counts were higher in female individuals in
all evaluated age groups (Fig. 1),
and showed a significant age-related decline in both genders
(p<0.0001). However, the measured platelet levels remained
within the reference limits in use by the University of Heidelberg
Medical Center and in accordance with the German Accreditation
Council (DAR).
While the WBC mean values showed an age-dependent
decreasing trend for both genders, no statistical significance was
noted when individuals below and beyond the age of 60 years were
compared to each other. However, when the cut-off age was set at 70
years, statistical significance was reached for male individuals
(p=0.008), but not for female subjects (p=0.23). Despite the
age-dependent decreasing trend for leukocyte values, these remained
within the reference interval in use by the University of
Heidelberg Medical Center (Fig.
1). A comparison of differential blood counts among the various
age groups and genders was quite inconsistent.
Discussion
The diagnosis and assessment of anaemia is an
essential part of everyday clinical practice and is gaining
importance, particularly in view of the increasingly ageing
population in the Western world. Anaemia is a common disorder in
the elderly and, while it is typically mild in this population, it
has been associated with substantial morbidity and mortality
(24). It is therefore important
to initially determine whether a patient is, in fact, anaemic, or
whether his/her low haemoglobin level is a phenomenon of the
expression of old age. This may be difficult to assess if a record
of previous blood counts is unavailable and a physician is forced
to make a judgement on the basis of a specific population’s
haemoglobin distribution.
In the 1960s the World Health Organization (WHO)
carried out a number of studies on nutritional anaemias of
pregnancy in India, Israel, Mexico, Poland and Venezuela. Based on
these data, in 1968, the WHO arbitrarily defined haemoglobin
limits, which became the standard in the diagnosis of anaemia and
which are still being used at present. Accordingly, the diagnosis
of anaemia is considered when haemoglobin levels are lower than
13.0 g/dl in males, 12.0 g/dl in non-pregnant females and 11 g/dl
in pregnant females for individuals residing at sea level (25). From the time of the establishment
of these first guidelines in 1968, there was difficulty in
precisely defining normality in the populations that were studied
and in deducing haemoglobin limits that were generally binding for
all populations worldwide. In addition, since 1968, numerous
parameters that may affect haemoglobin levels (environmental and
nutritional factors, lifestyle and others) have changed quite
considerably in the Western world. In addition and most
importantly, individuals beyond 65 years of age and racial and
ethnic differences were not considered in these studies. Also,
numerous factors have been described that affect blood counts in
the elderly. Reduced numbers of haematopoietic stem cells, the
finite number of cell divisions (18), a defect in progenitor cell
proliferation (19), the inability
to sufficiently mobilize such progenitors (6), and the lack of hormonal stimulation
or the reduced response to hormonal stimulation (20–23)
are a few examples of conditions that may be associated with
reduced haemoglobin levels in the absence of an apparent illness. A
considerable decline in oxygen need due to the diminishing body
mass and/or physical activity which is reflected in the
relationship between haemoglobin and body mass index are also
factors that contribute to low haemoglobin levels, and should
therefore be considered (6,19,26).
The current definition of anaemia suggested by a WHO expert
committee in 1968 is therefore not applicable to the elderly, and
urgently needs to be updated (25,27–31).
Despite the fact that numerous studies have been
carried out in the last 40 years showing aberrant haemoglobin
distributions within distinct populations, most authors have
dismissed the need for a modification of the lower haemoglobin
reference values solely on the basis of an individual’s age
(3–12,32).
This is essentially due to the fear of incorrectly underdiagnosing
anaemia once age-related haemoglobin changes are considered, and
consequently accepting an overdiagnosis of anaemia when an
individual’s age is not being taken into account (33). Several studies have aimed to
determine the most relevant causes of anaemia in the elderly. In
addition to well-described causes such as chronic disease,
infection, iron or vitamin B12 deficiency, renal or liver failure,
in up to 36% of individuals the origin of anaemia was unknown
(34,35). In accordance with our study, the
vast majority of authors identified a higher prevalence of anaemic
subjects in the elderly population as compared to younger
individuals. Therefore, the question arises as to whether this
phenomenon is part of the physiological ageing process, or whether
it is the consequence or cause of an underlying disease process as
yet undiagnosed (4). Studies
involving only elderly patients over a long period of time are
difficult to interpret, as ageing itself is a process that
increases the mortality risk as a function of time. Therefore,
whether an elderly person carries an increased risk of mortality
because of low haemoglobin levels or because of advanced age is
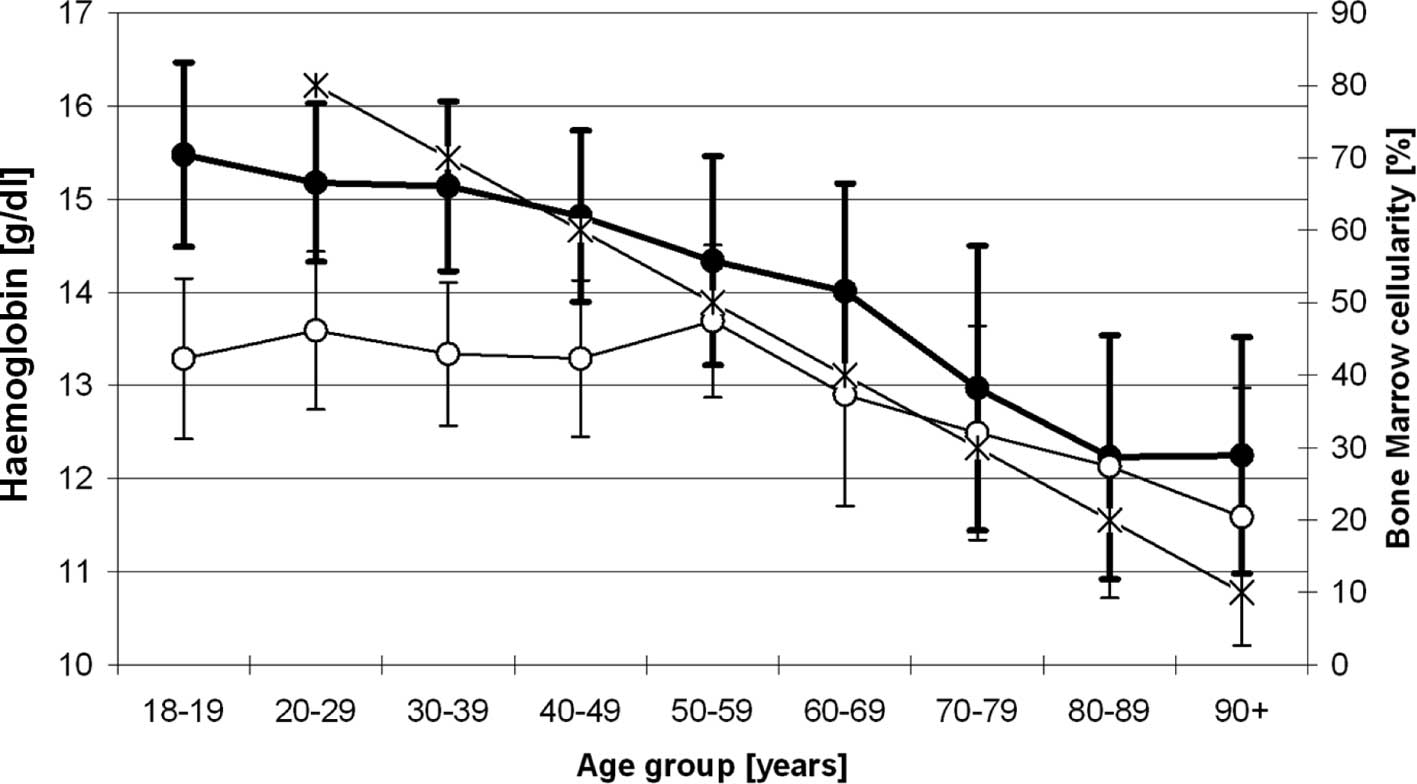
still unclear. One possible explanation for low haemoglobin levels
in the aged is the reduced haematopoietic activity, as determined
by a decrease in bone marrow cellularity of up to 50% in
individuals beyond the age of 60 years, which occurs along with a
significant reduction in peripheral blood counts (19,36).
In one study, reduced numbers of both bone marrow erythroid and
myeloid progenitors were observed to be more pronounced in elderly
men than in elderly women, which may at least in part explain
gender differences in the decline of haemoglobin levels in the
elderly (6). Also, stem cells are
subject to replicative senescence and can only perform a finite
number of cell divisions, which provides an additional explanation
for the age-dependent reduction in haematopoiesis (Fig. 4) (18,37–39).
As demonstrated by several research groups, an age-dependent
decline in bone marrow cellularity is observed after the 3rd decade
of life. By contrast, in young individuals below the age of 30,
over 70% of haematopoietic cellular matter comprises the bone
marrow volume and 30% consist of degenerated marrow fat. In
accordance with the following simplified formula: 100 - age (years)
= bone marrow cellularity (%) (40,41),
an estimate of bone marrow cellularity within single age groups can
be determined, and – particularly in the elderly – a dramatic
age-associated loss of bone marrow cellularity has been described
by several authors (42–44). In addition, it must be taken into
consideration that the bone marrow response and thus the
haematopoietic response to incoming stimuli and the cellular
crosstalk are reduced in aged indiciduals (Figs. 3 and 4) (19,45–47).
Even though average haemoglobin values vary from
laboratory to laboratory, a working definition of anaemia in a
specific population may be described by haemoglobin levels less
than the mean values in a population minus 2 SD. Based on the
results of our study data collected at the University of Heidelberg
Medical Center, the proposed age-adjusted lower haemoglobin levels
that would allow the diagnosis of anaemia in healthy elderly
individuals are lower than the reference values that are currently
being used worldwide based on the WHO studies of the 1960s
(Table II).
 | Table II.Geriatric assessment based on
performance status (ECOG or Karnofski-Index) and the presence of
comorbidities (upper panel) (50,51)
and proposal of a novel age-adjusted definition of anaemia for
elderly Caucasians. |
Table II.
Geriatric assessment based on
performance status (ECOG or Karnofski-Index) and the presence of
comorbidities (upper panel) (50,51)
and proposal of a novel age-adjusted definition of anaemia for
elderly Caucasians.
Fit
patient
ECOG 0 or Karnofski index 90–100%
No comorbidities | Frail
patient
ECOG ≥ 1 or Karnofski index ≤80%
Comorbidities |
|---|
|
|---|
Men
| Women
|
|---|
| ≤59 years | ≤79 years | ≥80 years | ≤59 years | ≤79 years | ≥80 years |
|
| 13.0 g/dl | 11.5 g/dl | 11.0 g/dl | 12.0 g/dl | 10.5 g/dl | 10.0 g/dl |
Haemoglobin levels in healthy elders are generally
lower than those in younger adults, and the differences between
males and females that are noted in younger adults are continuously
narrowed with increasing age (Fig.
1) (13,48,49).
We therefore propose a re-definition of the
diagnosis criteria for anaemia in the elderly in conjunction with
geriatric assessment, which distinguishes ‘fit’ from ‘frail’
patients. A patient should be considered ‘frail’ when fulfilling at
least 1 out of the 5 criteria that are listed for frail patients
(Table II), and the WHO diagnostic
criteria for anaemia should be applied in accordance with the
previous WHO recommendations with lower haemoglobin limits of ≤12.0
g/dl for women and ≤13.0 g/dl for men. However, when a patient
fulfills the criteria for a ‘fit’ patient, i.e., all indicated
criteria are met (Table II), the
age-adjusted haemoglobin levels should be used as proposed in
Table II.
Acknowledgements
This work was supported by the
Deutsche José Carreras Leukämie-Stiftung (DJCLS R09/20) to U.M.
References
|
1.
|
Zakai NA, Katz R, Hirsch C, et al: A
prospective study of anemia status, hemoglobin concentration, and
mortality in an elderly cohort: the Cardiovascular Health Study.
Arch Intern Med. 165:2214–2220. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Bohlius J, Wilson J, Seidenfeld J, et al:
Recombinant human erythropoietins and cancer patients: updated
meta-analysis of 57 studies including 9353 patients. J Natl Cancer
Inst. 98:708–714. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Castro OL, Haddy TB and Rana SR: Age- and
sex-related blood cell values in healthy black Americans. Public
Health Rep. 102:232–237. 1987.PubMed/NCBI
|
|
4.
|
Izaks GJ and Westendorp RG: Ill or just
old? Towards a conceptual framework of the relation between ageing
and disease. BMC Geriatr. 3:72003. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Lugada ES, Mermin J, Kaharuza F, et al:
Population-based hematologic and immunologic reference values for a
healthy Ugandan population. Clin Diagn Lab Immunol. 11:29–34.
2004.PubMed/NCBI
|
|
6.
|
Nilsson-Ehle H, Jagenburg R, Landahl S and
Svanborg A: Blood haemoglobin declines in the elderly: implications
for reference intervals from age 70 to 88. Eur J Haematol.
65:297–305. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Nordin G, Martensson A, Swolin B, et al: A
multicentre study of reference intervals for haemoglobin, basic
blood cell counts and erythrocyte indices in the adult population
of the Nordic countries. Scand J Clin Lab Invest. 64:385–398. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Tsang CW, Lazarus R, Smith W, Mitchell P,
Koutts J and Burnett L: Hematological indices in an older
population sample: derivation of healthy reference values. Clin
Chem. 44:96–101. 1998.PubMed/NCBI
|
|
9.
|
Akdag R, Energin VM, Kalayci AG and
Karakelleoglu C: Reference limits for routine haematological
measurements in 7–14-year-old children living at an intermediate
altitude (1869 m, Erzurum, Turkey). Scand J Clin Lab Invest.
56:103–109. 1996.PubMed/NCBI
|
|
10.
|
Bao W, Dalferes ER Jr, Srinivasan SR,
Webber LS and Berenson GS: Normative distribution of complete blood
count from early childhood through adolescence: the Bogalusa Heart
Study. Prev Med. 22:825–837. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Serjeant GR, Grandison Y, Mason K,
Serjeant B, Sewell A and Vaidya S: Haematological indices in normal
Negro children: a Jamaican cohort from birth to five years. Clin
Lab Haematol. 2:169–178. 1980.PubMed/NCBI
|
|
12.
|
Shiga S, Koyanagi I, Ohsaga J, Ichiyama S
and Kannagi R: [Clinical reference values for laboratory hematology
tests calculated using the iterative truncation method with
correction: Part 2, reference values for white blood cell (WBC)
count, WBC differential including segmented neutrophil, band
neutrophil, lymphocyte, monocyte, eosinophil, basophil, platelet
count and mean platelet volume]. Rinsho Byori. 47:281–288.
1999.
|
|
13.
|
Nilsson-Ehle H, Jagenburg R, Landahl S,
Svanborg A and Westin J: Haematological abnormalities and reference
intervals in the elderly. A cross-sectional comparative study of
three urban Swedish population samples aged 70, 75 and 81 years.
Acta Med Scand. 224:595–604. 1988.
|
|
14.
|
Marchant T, Schellenberg JA, Nathan R, et
al: Anaemia in pregnancy and infant mortality in Tanzania. Trop Med
Int Health. 9:262–266. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
United_Nations: Population Division: World
Population Prospects. The 2006 Revision. United Nations; New York,
NY: 2007
|
|
16.
|
Bundesamt S: German Population until 2060.
Wiesbaden. 2009.
|
|
17.
|
Kirkwood TB and Austad SN: Why do we age?
Nature. 408:233–238. 2000. View
Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Hayflick L: The limited in vitro lifetime
of human diploid cell strains. Exp Cell Res. 37:614–636. 1965.
View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Lipschitz DA, Udupa KB, Milton KY and
Thompson CO: Effect of age on hematopoiesis in man. Blood.
63:502–509. 1984.PubMed/NCBI
|
|
20.
|
Young DS: Pre-analytical variability in
the elderly. Geriatr Clin Chem. 19–39. 1994.
|
|
21.
|
Carpenter MA, Kendall RG, O’Brien AE, et
al: Reduced erythropoietin response to anaemia in elderly patients
with normocytic anaemia. Eur J Haematol. 49:119–121. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Kario K, Matsuo T, Kodama K, Nakao K and
Asada R: Reduced erythropoietin secretion in senile anemia. Am J
Hematol. 41:252–257. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Nafziger J, Pailla K, Luciani L, Andreux
JP, Saint-Jean O and Casadevall N: Decreased erythropoietin
responsiveness to iron deficiency anemia in the elderly. Am J
Hematol. 43:172–176. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Price EA and Schrier SL: Anemia in the
elderly: introduction. Semin Hematol. 45:207–209. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Blanc B, Finch CA, Hallberg L, et al:
Nutritional anaemias. Report of a WHO Scientific Group. WHO Tech
Rep Ser. 405:1–40. 1968.
|
|
26.
|
Lapin A and Bohmer F: [Laboratory findings
in elderly patients: a forgotten aspect of laboratory medicine?]. Z
Gerontol Geriatr. 32:41–46. 1999.
|
|
27.
|
Kilpatrick GS and Hardisty RM: The
prevalence of anaemia in the community. A survey of a random sample
of the population. Br Med J. 1:778–782. 1961. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
De Leeuw NK, Lowenstein L and Hsieh YS:
Iron deficiency and hydremia in normal pregnancy. Medicine.
45:291–315. 1966.PubMed/NCBI
|
|
29.
|
Sturgeon P: Studies of iron requirements
in infants. III. Influence of supplemental iron during normal
pregnancy on mother and infant. B. The infant. Br J Haematol.
5:45–55. 1959. View Article : Google Scholar
|
|
30.
|
Natvig K: Studies on hemoglobin values in
Norway. V. Hemoglobin concentration and hematocrit in men aged
15–21 years. Acta Med Scand. 180:613–620. 1966.PubMed/NCBI
|
|
31.
|
Beutler E and Waalen J: The definition of
anemia: what is the lower limit of normal of the blood hemoglobin
concentration? Blood. 107:1747–1750. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Izaks GJ, Remarque EJ, Becker SV and
Westendorp RG: Lymphocyte count and mortality risk in older
persons. The Leiden 85-Plus Study. J Am Geriatr Soc. 51:1461–1465.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
Melillo KD: Interpretation of laboratory
values in older adults. Nurse Pract. 18:59–67. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
34.
|
Balducci L: Epidemiology of anemia in the
elderly: information on diagnostic evaluation. J Am Geriatr Soc.
51:S2–S9. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
35.
|
Gabrilove J: Anemia and the elderly:
clinical considerations. Best Pract Res Clin Haematol. 18:417–422.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
36.
|
Vogel JM: Hematologic problems of the
aged. Mt Sinai J Med. 47:150–165. 1980.PubMed/NCBI
|
|
37.
|
Wagner W, Bork S, Horn P, et al: Aging and
replicative senescence have related effects on human stem and
progenitor cells. PLoS One. 4:e58462009. View Article : Google Scholar : PubMed/NCBI
|
|
38.
|
Waterstrat A and Van Zant G: Effects of
aging on hematopoietic stem and progenitor cells. Curr Opin
Immunol. 21:408–413. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
39.
|
Rossi DJ, Jamieson CH and Weissman IL:
Stems cells and the pathways to aging and cancer. Cell.
132:681–696. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
40.
|
Longo DL: Closing in on a killer: anemia
in elderly people. J Gerontol A Biol Sci Med Sci. 60:727–728. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
41.
|
Burkhardt R, Kettner G, Bohm W, et al:
Changes in trabecular bone, hematopoiesis and bone marrow vessels
in aplastic anemia, primary osteoporosis, and old age: a
comparative histomorphometric study. Bone. 8:157–164. 1987.
View Article : Google Scholar
|
|
42.
|
Aapro MS, Cella D and Zagari M: Age,
anemia, and fatigue. Semin Oncol. 29:55–59. 2002. View Article : Google Scholar
|
|
43.
|
Goldstein S: The biology of aging. N Engl
J Med. 285:1120–1129. 1971. View Article : Google Scholar
|
|
44.
|
Hartsock RJ, Smith EB and Petty CS: Normal
variations with aging of the amount of hematopoietic tissue in bone
marrow from the anterior iliac crest. A study made from 177 cases
of sudden death examined by necropsy. Am J Clin Pathol. 43:326–331.
1965.
|
|
45.
|
Baldwin JG Jr: True anemia: incidence and
significance in the elderly. Geriatrics. 44:33–36. 1989.PubMed/NCBI
|
|
46.
|
Baldwin JG Jr: Hematopoietic function in
the elderly. Arch Intern Med. 148:2544–2546. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
47.
|
Eisenstaedt R, Penninx BW and Woodman RC:
Anemia in the elderly: current understanding and emerging concepts.
Blood Rev. 20:213–226. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
48.
|
Nilsson-Ehle H, Jagenburg R, Landahl S,
Svanborg A and Westin J: Decline of blood haemoglobin in the aged:
a longitudinal study of an urban Swedish population from age 70 to
81. Br J Haematol. 71:437–442. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
49.
|
Patel KV: Epidemiology of anemia in older
adults. Semin Hematol. 45:210–217. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
50.
|
Karnofsky DA and Burchenal JH: The
Clinical Evaluation of Chemotherapeutic Agents in Cancer. Columbia
University Press; New York: 1949
|
|
51.
|
Oken MM, Creech RH, Tormey DC, et al:
Toxicity and response criteria of the Eastern Cooperative Oncology
Group. Am J Clin Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|