Introduction
Postoperative exacerbation of interstitial pneumonia
in patients with lung cancer and interstitial lung disease has
emerged as a serious problem. Postoperative interstitial pneumonia
is a life-threatening complication with a high rate of mortality
following surgery (1–3). Since it is difficult for patients
with interstitial lung disease to undergo chemotherapy, radiation
therapy or both, for their lung cancers, due to a high rate of
exacerbation of interstitial pneumonia after treatment, surgical
resection is sometimes the sole method of treatment for these
patients. Moreover, performing surgical resection for patients with
interstitial lung disease cannot be avoided when they have
perquisite clinical stages and no other limitations. However,
special care must be taken in the surgical management of patients
with lung cancer and interstitial lung disease, as patients with
interstitial lung disease have a high risk of postoperative
exacerbation of interstitial pneumonia (4). Therefore, the risk factors for
postoperative exacerbation of interstitial pneumonia in patients
with interstitial lung disease must be identified. However, there
are relatively few reports regarding the postoperative exacerbation
of interstitial pneumonia. In this study, the predictive markers of
postoperative exacerbation of interstitial pneumonia were
investigated in patients with lung cancer and interstitial lung
disease.
Patients and methods
We analyzed 22 patients diagnosed with lung cancer
with interstitial lung disease who underwent surgical treatment at
the Kitasato University Hospital between 1990 and 2009.
Pre-operatively, interstitial lung diseases were detected by prior
patient history, pre-operative chest X-ray or pre-operative
computed tomography (CT) based on the ATS/ERS statement (5), and confirmed by pathological
diagnoses from the resected specimens. Acute exacerbation of
interstitial pneumonia was diagnosed when patients had intensified
dyspnea, a decrease in arterial oxygen tension or an increased fine
crackle on auscultation with an increased interstitial shadow on
chest CT. Patients with collagen diseases were excluded from this
study, as patients with these diseases may manifest different
clinical features.
The following patient parameters were investigated
from the medical records: gender, age, smoking history, clinical
staging, pre-operative symptoms, site of tumors, pre-operative
serum marker levels of Krebs von den Lungen-6 (KL-6), surgical
procedure, pathological findings, including tumor size, time of
death, latest follow-up day, postoperative interstitial pneumonia,
administration of steroid and outcome.
Statistical analysis
Fisher’s exact test was used to compare binomial
proportions. The χ2 test was used to assess differences
in treatment. A P-value of <0.05 was considered statistically
significant.
Results
The characteristics of the patients are listed in
Table I. All 22 patients had a
history of smoking. Five patients (22.7%) had postoperative
exacerbation of interstitial pneumonia. There were no significant
differences in gender, sites of lung cancers, pre-operative lung
function, smoking history or the levels of lymph node dissection
between the group with postoperative exacerbation of interstitial
pneumonia and the group without. Among the patients with
postoperative exacerbation, 4 patients were aged ≥75 years; there
was a significantly higher rate of patients ≥75 years of age than
among those without postoperative exacerbation. Patients with
postoperative exacerbation presented with significantly advanced
clinical stages compared to patients without postoperative
exacerbation, and most patients with postoperative exacerbation
underwent lobectomy. All patients with postoperative exacerbation
had elevated serum KL-6 levels (Table
II). Moreover, only 2 patients with postoperative exacerbation
had prophylactic administration of steroid postoperatively, which
was a significantly lower rate compared to patients without
postoperative exacerbation. In 5 patients with postoperative
exacerbation, 2 had a history of inflammation just prior to the
exacerbation: 1 had a common cold and the other had pyothorax. The
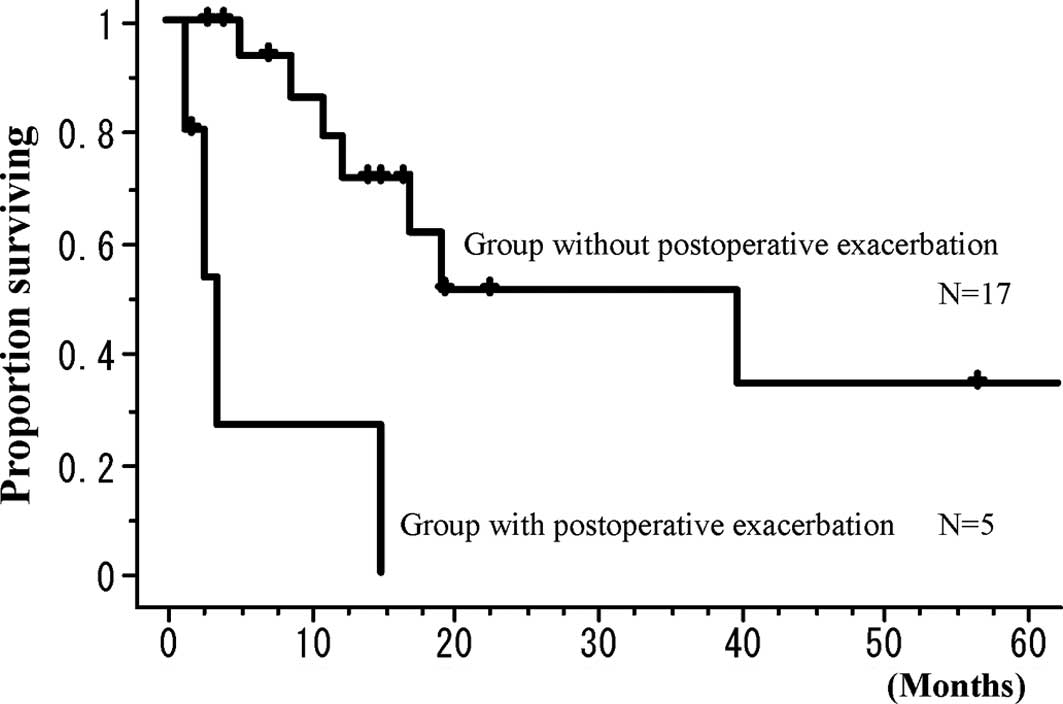
prognosis of patients with postoperative exacerbation was
significantly poorer than that of patients without postoperative
exacerbation (P=0.0252, Fig.
1).
 | Table IPatient characteristics (n=22). |
Table I
Patient characteristics (n=22).
| Factor | No. (%) |
|---|
| Age | |
| Mean ± SD | 69.9±6.9 |
| Gender | |
| Male | 19 (86.4) |
| Female | 3 (13.6) |
| Site | |
| Right | 14 (63.6) |
| Left | 8 (36.4) |
| Clinical stage | |
| IA | 7 (31.8) |
| IB | 12 (54.5) |
| IIB | 2 (9.0) |
| IIIA | 1 (4.5) |
| Smoking | |
| Smoker | 16 (72.7) |
| Ex-smoker | 6 (27.3) |
| Surgery | |
| Lobectomy | 17 (77.3) |
| Wedge
resection | 5 (22.7) |
| Postoperative
exacerbation | |
| + | 5 (22.7) |
| − | 17 (77.3) |
 | Table IIComparison between patients with and
without postoperative exacerbation. |
Table II
Comparison between patients with and
without postoperative exacerbation.
| Factor | Postoperative
exacerbation (+) (n=5) | Postoperative
exacerbation (−) (n=17) | P-value |
|---|
| Age (years) | | | 0.0207 |
| ≥75 | 4 | 3 | |
| <75 | 1 | 14 | |
| Gender | | | >0.9999 |
| Male | 4 | 15 | |
| Female | 1 | 2 | |
| Site | | | >0.9999 |
| Right | 3 | 11 | |
| Left | 2 | 6 | |
| Clinical stage | | | 0.0344 |
| IA | 2 | 5 | |
| IB | 1 | 11 | |
| IIB | 2 | 0 | |
| IIIA | 0 | 1 | |
| Lung function | | | |
| VC (ml) | 2,753 | 3,081 | 0.3522 |
| FEV1.0 (ml) | 2,158 | 2,306 | 0.5360 |
| PaO2
(torr) | 77.1 | 81.6 | 0.4828 |
| Smoking | | | >0.9999 |
| Smoker | 4 | 12 | |
| Ex-smoker | 1 | 5 | |
| Surgery | | | >0.9999 |
| Lobectomy | 4 | 13 | |
| Wedge
resection | 1 | 4 | |
| Lymph node
dissection | | | 0.6980 |
| ND0 | 2 | 7 | |
| ND1 | 3 | 8 | |
| ND2 | 0 | 2 | |
| KL-6 | | | 0.5165 |
| High | 4 | 8 | |
| Low | 0 | 4 | |
| Postoperative
steroid | | | 0.0239 |
| Yes | 2 | 16 | |
| No | 3 | 1 | |
Discussion
At present, patients with various complications must
undergo resection for lung cancer. Nakajima et al (6) reported that patients with lung cancer
and collagen disease were not contraindicated to undergo surgical
resection for lung carcinoma, although they frequently had
interstitial pneumonia as pointed out in the resected specimens.
Kutlu et al (1)
investigated the frequency and mortality of acute lung injury and
acute respiratory distress syndrome in patients after pulmonary
resection, and reported that 45 (3.9%) of 1,139 resected cases had
postoperative acute lung injury or acute respiratory distress
syndrome, while 29 (64.4%) of these 45 patients died. Ruffini et
al (2) reported that 27 (2.2%)
of 1,221 cases had postoperative acute lung injury or acute
respiratory distress syndrome, and that 14 (51.9%) of those 27
patients died. Muraoka et al (7) reported that 9 (56.3%) of 16 patients
died due to respiratory failure.
Therefore, postoperative exacerbation of
interstitial pneumonia is a serious problem after pulmonary
resection. However, little is known regarding postoperative
exacerbation of interstitial pneumonia; in particular, the cause
and the risk factors for interstitial pneumonia remain unknown
(7). In various surgical
approaches for lung cancers, Koizumi et al (8) compared the use of video-assisted
thoracoscopic surgery to posterolateral thoracotomy or
muscle-sparing thoracotomy and reported that the use of
video-assisted thoracoscopic surgery did not prevent acute
exacerbation of postoperative interstitial pneumonia. Therefore,
postoperative acute interstitial pneumonia may be related to
factors other than the surgical approach.
Takeda et al (3) reported that the measurement of serum
KL-6 levels is useful to assess the activity of interstitial
pneumonia. Moreover, Muraoka et al (7) reported that factors including a tumor
located on the right side, pre-operative radiation or chemotherapy,
pneumonectomy, blood transfusion and intraoperative complications
were independent risk factors for the incidence of acute
interstitial pneumonia. Koizumi et al (8) reported that exertion dyspnea
(Hugh-Jones classification), serum C-reactive protein, serum
lactate dehydrogenase and total lung capacity were considered to be
pre-operative risk factors of acute exacerbation. Chida et
al (9) reported that 11 of 15
patients with postoperative interstitial pneumonia were found to
have interstitial pneumonia in pre-operative CT scans, and patients
with findings of interstitial pneumonia in pre-operative CT scans
had a significantly higher rate of postoperative acute respiratory
distress syndrome (ARDS) than did patients with no such findings.
They also reported that induction chemotherapy or chemoradiotherapy
was a risk factor of postoperative ARDS (9).
In the present study, we selected patients with
interstitial pneumonia pre-operatively and examined risk factors of
postoperative exacerbation. The limitations of this study were that
it was retrospective and that the number of patients was limited.
However, the rate of postoperative exacerbation was high and,
therefore, patients with pre-operative interstitial lung disease
have a severe risk for postoperative exacerbation of interstitial
pneumonia. In the present study, patients with postoperative
exacerbation included patients with advanced age, those with a high
rate of elevated serum KL-6, those who underwent lobectomy, and
patients who did not receive steroid administration. Thus, special
attention should be paid to postoperative exacerbation of
interstitial pneumonia for patients with the above factors. Despite
the limitation of the relatively small patient population, the
occurrence of inflammation just prior to the postoperative
exacerbation in the 2 patients with postoperative exacerbation was
evaluated. Consequently the existence of inflammation may likely be
one of the risk factors for postoperative exacerbation.
Acknowledgments
This study was supported in part by a Grant-in-aid
for Scientific research (C) 21591822 of the Japanese Ministry of
Education, Culture, Sports, Science, and Technology. The authors
thank Mr. Robert E. Brandt, CEO, MedEd Japan, for the editorial
assistance in the preparation of the manuscript.
References
|
1
|
Kutlu CA, Williams EA, Evans TW, Pastorino
U and Goldstraw P: Acute lung injury and acute respiratory distress
syndrome after pulmonary resection. Ann Thorac Surg. 69:376–380.
2000. View Article : Google Scholar
|
|
2
|
Ruffini E, Parola A, Papalia E, Filosso
PL, Mancuso M, Oliaro A, Actis-Dato G and Maggi G: Frequency and
mortality of acute lung injury and acute respiratory distress
syndrome after pulmonary resection for bronchogenic carcinoma. Eur
J Cardiothorac Surg. 20:30–36. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Takeda S, Maeda H, Sawabata N, Kitada S,
Mori M, Takashima S and Matsubara Y: Clinical impact of
interstitial pneumonia following surgery for lung cancer. Thorac
Cardiovasc Surg. 54:268–272. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chiyo M, Sekine Y, Iwata T, Tatsumi K,
Yasufuku K, Iyoda A, Otsuji M, Yoshida S, Shibuya K, Iizasa T,
Saitoh Y and Fujisawa T: Impact of interstitial lung disease on
surgical morbidity and mortality for lung cancer: analyses of
short-term and long-term outcomes. J Thorac Cardiovasc Surg.
126:1141–1146. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
American Thoracic Society; European
Respiratory Society: American Thoracic Society/European Respiratory
Society International Multidisciplinary Consensus Classification of
the Idiopathic Interstitial Pneumonias. This joint statement of the
American Thoracic Society (ATS), and the European Respiratory
Society (ERS) was adopted by the ATS board of directors, June 2001
and by the ERS Executive Committee, June 2001. Am J Respir Crit
Care Med. 165:277–304. 2002.
|
|
6
|
Nakajima J, Takamoto S, Murakawa T, Fukami
T and Sano A: Is interstitial pneumonia in patients with collagen
diseases a contraindication to lung cancer surgery? Surg Today.
37:14–18. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Muraoka M, Tagawa T, Akamine S, Oka T,
Tsuchiya T, Araki M, Hayashi T and Nagayasu T: Acute interstitial
pneumonia following surgery for primary lung cancer. Eur J
Cardiothorac Surg. 30:657–662. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Koizumi K, Hirata T, Hirai K, Mikami I,
Okada D, Yamagishi S, Kawashima T, Nakajima Y and Shimizu K:
Surgical treatment of lung cancer combined with interstitial
pneumonia: the effect of surgical approach on postoperative acute
exacerbation. Ann Thorac Cardiovasc Surg. 10:340–346.
2004.PubMed/NCBI
|
|
9
|
Chida M, Ono S, Hoshikawa Y and Kondo T:
Subclinical idiopathic pulmonary fibrosis is also a risk factor of
postoperative acute respiratory distress syndrome following
thoracic surgery. Eur J Cardiothorac Surg. 34:878–881. 2008.
View Article : Google Scholar
|