Introduction
In 2008, an estimated 386,300 new cases and 150,200
deaths from bladder cancer were reported. The majority of bladder
cancer occurs in males and there is a 14-fold variation in
incidence internationally (1).
Non-muscle-invasive bladder cancer (NMIBC) accounts for
approximately 80% of total bladder cancer cases (2). Intravesical bacillus Calmette-Guérin
(BCG) therapy is the standard prophylaxis for recurrence of NMIBC
(3). However, after a single
6-week course of intravesical immunotherapy after transurethral
resection of bladder tumor (TUR-BT), the 5-year recurrence rates
range from 16 to 59% (4–6).
A randomized Southwest Oncology Group (SWOG) study
reported the results of intravesical maintenance immunotherapy.
This revealed that the median recurrence-free survival (RFS) time
was twice as long in the 3-week maintenance arm compared to the no
maintenance arm, and patients had significantly longer
worsening-free survival (4). At
least 1 week following biopsy of carcinoma in situ (CIS) and
resection of any stage Ta or T1 transitional cell carcinomas,
patients were started on a 6-week induction course of intravesical
and percutaneous Connaught BCG. Maintenance therapy of the SWOG
study consisted of intravesical and percutaneous BCG each week for
3 weeks, administered 3, 6, 12, 18, 24, 30 and 36 months from the
initiation of the induction therapy.
A number of randomized studies have focused on the
benefit of maintenance therapy following initial BCG induction
(7). Meta-analyses reported that
BCG maintenance significantly reduces recurrence or progression in
patients with NMIBC (8,9). Several studies, however, revealed no
benefit of maintenance therapy in controlling tumor recurrence or
progression (10–12). Differences in the results are
possibly due to the maintenance schedules. The maintenance
schedules varied considerably and it appears that a weekly,
monthly, quarterly or 6-monthly schedule for 1–2 years may be
immunologically suboptimal (4,10,11,13).
The aim of this study was to confirm the recurrence- and
progression-preventing efficacy and safety of 12 times monthly BCG
maintenance therapy for NMIBC.
Materials and methods
This case-control study included 126 patients
diagnosed with Ta, T1 and CIS bladder cancer between January 2000
and December 2009, who received intravesical immunotherapy. The
inclusion criteria were high-risk NMIBC and recurrent NMIBC, such
as, pathologically confirmed Ta, T1 and CIS of the bladder,
administration of intravesical initiation or maintenance
immunotherapy, performance status of 0–2, ability to undergo
cystoscopy and TUR-BT, and intact function of main organs (14). Exclusion criteria included reduced
dosage of BCG Tice strain, failure of consecutive treatment,
strongly positive tuberculin test, history of intravesical BCG
instillation, severe bladder irritation before the start of BCG
administration and active serious medical complications. Of 126
patients with NMIBC, 34 patients in the no maintenance group
received a single 6-week course of intravesical immunotherapy after
TUR-BT. Ninety-two patients in the maintenance group received 12
times monthly maintenance therapy course after a single 6-week
course of intravesical immunotherapy after TUR-BT.
Prior to intravesical immunotherapy, patients
provided a health history and underwent a physical examination,
urinalysis, urine cytology, complete blood count, blood urea
nitrogen, serum creatinine, liver function test and chest X-ray.
The single 6-week course of intravesical immunotherapy started
within 1 week after TUR-BT with 12.5 mg of BCG Tice strain
(OncoTICE; Oregano, West Orange, NJ, USA). BCG Tice strain was
first suspended in 3 ml diluents, followed by dilution with 40 ml
physiological saline. That suspension was then instilled into the
bladder via a urethral catheter. Patients were required to hold
their urine for ∼2 h after instillation (15). BCG treatment was repeated weekly
for 6 consecutive weeks. An additional 12 times monthly course
after the single 6-week course of intravesical immunotherapy was
initiated 1 month later after a single 6-week course with BCG Tice
strain. BCG treatment was repeated monthly for 12 consecutive
months.
Efficacy of the treatment regimens was assessed on
the basis of cystoscopy and urinary cytology finding. The patients
were followed up every 3 months during the first 2 years, and every
6 months thereafter (14).
End-points were RFS and progression-free survival (PFS). When tumor
recurrence was suspected on the basis of the findings of cystoscopy
and urinary cytology, confirmation was carried out by performing
TUR-BT. Progression at the time of recurrence was defined as
pathological stage T2 disease or greater, or the use of cystectomy,
systemic chemotherapy or radiation therapy. Kaplan-Meier survival
curves were used to estimate disease-free survival. P-value
<0.05 was considered to denote statistical significance.
Results
The median follow-up period was 43 months
(interquartile range 18–64; range 3–123) in the maintenance group
and 16.5 months (interquartile range 6–35.75; range 3–75) in the no
maintenance group. The baseline clinicopathological characteristics
of the NMIBC patients are shown in Table I. One hundred and twenty-six
patients were eligible for enrollment in our study. In total, 92
patients with Ta (n=25) and T1 (n=67) were treated with
intravesical BCG maintenance therapy, and 34 patients with Ta
(n=15) and T1 (n=19) were treated with intravesical BCG initiation
therapy. There were no significant clinicopathological differences
between the maintenance and no maintenance groups.
 | Table I.Baseline characteristics of the
maintenance and no maintenance groups. |
Table I.
Baseline characteristics of the
maintenance and no maintenance groups.
|
Characteristics | Maintenance
(n=92) | No maintenance
(n=34) | P-value |
|---|
| Gender | | | 0.273 |
| Male | 75 | 31 | |
| Female | 17 | 3 | |
| Age (years) | 61.73±11.865 | 65.88±11.762 | 0.083 |
| T stage | | | 0.086 |
| Ta | 25 | 15 | |
| T1 | 67 | 19 | |
| Carcinoma in
situ | | | 0.526 |
| Yes | 9 | 5 | |
| No | 83 | 29 | |
| Grade | | | 0.520 |
| G1 | 14 | 6 | |
| G2 | 47 | 14 | |
| G3 | 28 | 14 | |
| Multiplicity | | | 0.677 |
| Single | 33 | 11 | |
| Multiple | 55 | 23 | |
| Recurrence
history | | | 0.793 |
| Primary | 75 | 27 | |
| Recurrent | 15 | 7 | |
| Smoking
history | | | 0.178 |
| Yes | 29 | 23 | |
| No | 25 | 10 | |
The complications and side effects of immunotherapy
are reported in Table II. The
incidence of overall side effects was 40.2% in the maintenance
group and 44.1% in the no maintenance group. Most of these
complications were irritative symptoms (frequency, urgency and
tenesmus). Two patients who had high-grade fever during maintenance
therapy were treated with antipyretic medication. However, these
patients had finished maintenance therapy. One patient who finished
maintenance therapy had pulmonary tuberculosis.
 | Table II.Toxicity and side effects of the
maintenance and no maintenance groups. |
Table II.
Toxicity and side effects of the
maintenance and no maintenance groups.
|
Characteristics | Maintenance
(n=92) | No maintenance
(n=34) |
|---|
| Overall side
effects | 37 (40.2) | 15 (44.1) |
| Local toxicity | | |
| Irritative
symptom | 30 (32.6) | 14 (41.1) |
| Low-grade
fever | 1 (1.1) | 0 (0.0) |
| Gross
hematuria | 5 (5.4) | 2 (5.8) |
| Tuberculosis
cystitis | 2 (2.2) | 0 (0.0) |
| Tuberculosis
prostatitis | 1 (1.1) | 0 (0.0) |
| General
toxicity | | |
| High-grade
fever | 2 (2.2) | 0 (0.0) |
| Pulmonary
tuberculosis | 1 (1.1) | 0 (0.0) |
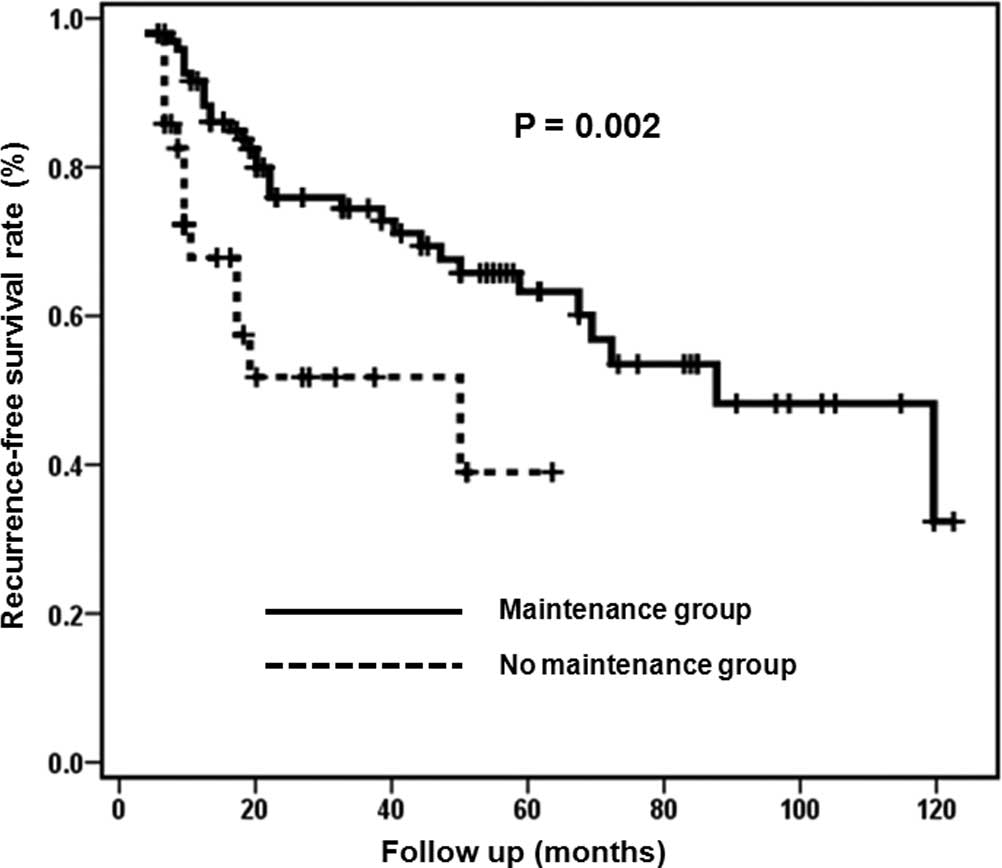
Fig. 1 shows RFS
curves of the maintenance and no maintenance groups. The estimated
median RFS was 87 months (95% CI 53.0–120.9) in the maintenance
group and 48 months (95% CI 0–96.8) in the no maintenance group
(log-rank test; P=0.002). The 2-year cumulative RFS rates were
77.3% in the maintenance group and 52.6% in the no maintenance
group. The 5-year cumulative RFS rates were 64.4% in the
maintenance group and 39.4% in the no maintenance group.
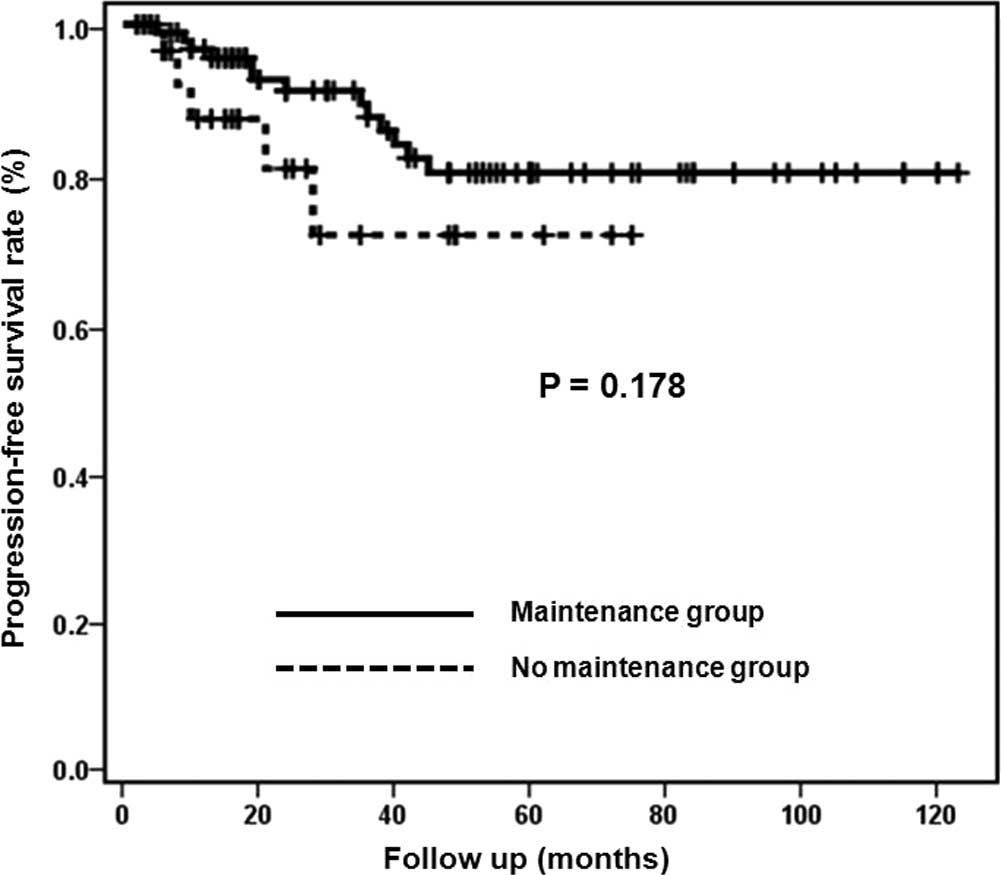
Fig. 2 shows PFS
curves of the maintenance and no maintenance groups. Median PFS
rates were not estimable in both groups (log-rank test; P=0.178).
The 2-year cumulative PFS rates were 91.1% in the maintenance group
and 80.5% in the no maintenance group. The 5-year cumulative PFS
rates were 80.0% in the maintenance group and 71.6% in the no
maintenance group.
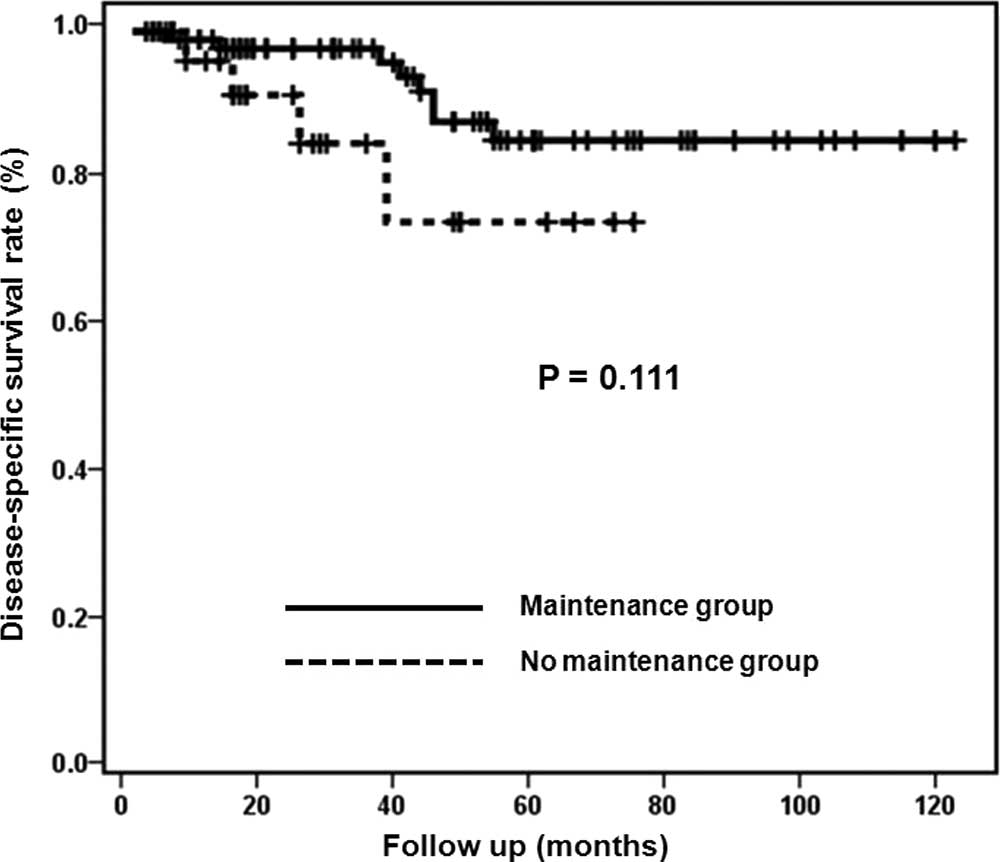
Fig. 3 shows
disease-specific survival (DSS) curves of the maintenance and no
maintenance groups. Median DSS rates were not estimable in both
groups (log-rank test; P=0.111). The 2-year cumulative DSS rates
were 97.7% in the maintenance group and 91.4% in the no maintenance
group. The 5-year cumulative DSS rates were 85.3% in the
maintenance group and 74.3% in the no maintenance group.
Discussion
Morales et al reported that adjuvant
intravesical BCG therapy reduced tumor recurrence (3). Large randomized clinical trials
performed by the SWOG demonstrated that BCG immunotherapy provides
significantly longer time to first recurrence compared to
chemotherapy. A randomized SWOG study reported that estimated
median RFS was 76.8 months (95% CI 64.3–93.2) in the maintenance
arm and 35.7 months (95% CI 25.1–56.8) in the no maintenance. They
concluded that the overall 5-year survival was 83% in the
maintenance arm compared to 78% in the no maintenance arm (4). Our study, using a monthly schedule,
produced similar results: the estimated median RFS was 87 months
(95% CI 53.0–120.9) in the maintenance group and 48 months (95% CI
0–96.8) in the no maintenance group. The 5-year survival rates were
85.3% in the maintenance group and 74.3% in the no maintenance
group.
Two meta-analyses showed that intravesical BCG
maintenance therapy reduced the risk of tumor progression (8,9).
Sylvester et al reported that intravesical BCG significantly
reduced the risk of tumor progression after transurethral resection
in patients with superficial bladder cancer who received
maintenance treatment. They identified 24 trials with progression
information on 4,863 patients, and 260 of 2,658 patients in the BCG
maintenance group (9.8%) had progression compared to 304 of 2,205
patients in the no maintenance group (13.8%) (8). Bohle et al revealed similar
results for BCG prevention of tumor progression. They reported that
BCG maintenance showed a statistically significant superiority over
mitomycin C (OR=0.66; 95% CI 0.47–0.94) (9).
Several studies, however, have not been able to show
that intravesical chemotherapy and immunotherapy have an influence
on the time to progression to muscle invasive disease (4,16,17).
Lamm et al found that maintenance chemotherapy failed to
improve significant benefit of early post-operative intravesical
chemotherapy. These data showed no decreased tumor progression, and
overall among 2,011 randomized patients progression occurred in
7.5% of those receiving intravesical chemotherapy and 6.9% of those
treated by surgery alone (17).
Pawinski et al reported that no clear advantage of adjuvant
treatment was shown with respect to progression to invasion, time
to appearance of distant metastases or duration of survival and
PFS. They concluded that, despite prolongation of the disease-free
interval, adjuvant treatment has no apparent long-term impact on
the evolution of stage Ta and T1 bladder cancer (16). The SWOG study reported that the
estimated median time for worsening-free survival, defined as no
evidence of progression, including pathological stage T2 disease or
greater, or the use of cystectomy, systemic chemotherapy or
radiation therapy, was 111.5 months in the no maintenance and not
estimable in the maintenance arm (4).
Two monthly maintenance therapies for NMIBC have
been reported (10,18). In a study by Badalament et
al, 46 patients received BCG weekly for 6 weeks and were
compared to 47 patients receiving the 6-weekly doses of BCG plus
monthly BCG for 2 years. They concluded that patients receiving
maintenance and no maintenance therapy had similar tumor recurrence
and progression rates. These results indicate that monthly
maintenance BCG does not prevent, delay or reduce tumor recurrence
or progression observed with the 6-week regimen (10). In a study by Akaza et al, 39
patients receiving prophylactic maintenance therapy consisting of
BCG of 40 mg monthly for 12 times were compared to 55 patients not
receiving maintenance therapy. After a 3-year follow-up period, the
final cumulative RFS rates were 77.6% in the maintenance group and
74.2% in the no maintenance group. They concluded that
transurethral resection of tumors of the bladder alone is unlikely
to eliminate the bladder tumor, and intravesical BCG is potentially
the treatment of choice.
Our previous study examined changes in bladder
mucosal immune cells in patients with superficial bladder carcinoma
treated with BCG and doxorubicin. The post-treatment bladder
mucosal B cells and T cells were significantly increased compared
to pre-treatment in patients treated with BCG instillation. There
was, however, no change in B or T cells in patients treated with
doxorubicin. There was no tumor recurrence in cases with
significantly increased numbers of B cells after BCG instillation.
The results of our study suggest that intravesical BCG
immunotherapy induces a significant increase in T cells as well as
B cells, and B cells have a preventive effect on tumor recurrence.
We conclude that stimulation at regular intervals may be effective
to activate T and B cells, such as booster injection for
immunization (19).
Regarding tumor progression, our results showed that
the 2-year cumulative PFS rates were 91.1% in the maintenance group
and 80.5% in the no maintenance group. However, the difference was
not statistically significant. Maintenance therapy of the SWOG
study consisted of intravesical and percutaneous BCG each week for
3 weeks, administered 3, 6, 12, 18, 24, 30 and 36 months from the
initiation of induction therapy (4). The total number of maintenance
therapy sessions was 21 in the SWOG study and 12 in our study. This
difference may have affected the PFS rates. In addition, the
difference in the number of patients between the maintenance and no
maintenance groups and the small sample size reduced the
statistical significance of the results. These were limitations of
our case-control study.
Acknowledgements
This study was supported by the Korea
Science and Engineering Grant Foundation of the Korean Government
(no. 20100028333).
References
|
1.
|
A JemalF BrayMM CenterJ FerlayE WardD
FormanGlobal cancer statisticsCA Cancer J
Clin616990201110.3322/caac.20107
|
|
2.
|
S AldousariW KassoufUpdate on the
management of non-muscle invasive bladder cancerCan Urol Assoc
J45664201020165581
|
|
3.
|
A MoralesD EidingerAW BruceIntracavitary
bacillus Calmette-Guerin in the treatment of superficial bladder
tumorsJ Urol1161801831976820877
|
|
4.
|
DL LammBA BlumensteinJD
CrissmanMaintenance bacillus Calmette-Guerin immunotherapy for
recurrent TA, T1 and carcinoma in situ transitional cell carcinoma
of the bladder: a randomized Southwest Oncology Group StudyJ
Urol16311241129200010.1016/S0022-5347(05)67707-510737480
|
|
5.
|
HW HerrDD WartingerWR FairHF
OettgenBacillus Calmette-Guerin therapy for superficial bladder
cancer: a 10-year follow-upJ Urol1471020102319921552578
|
|
6.
|
V PansadoroP EmiliozziL DefidioBacillus
Calmette-Guerin in the treatment of stage T1 grade 3 transitional
cell carcinoma of the bladder: long-term resultsJ
Urol15420542058199510.1016/S0022-5347(01)66692-87500457
|
|
7.
|
MD ShelleyMD MasonH KynastonIntravesical
therapy for superficial bladder cancer: a systematic review of
randomised trials and meta-analysesCancer Treat
Rev36195205201010.1016/j.ctrv.2009.12.00520079574
|
|
8.
|
RJ SylvesterMA van derDL LammIntravesical
bacillus Calmette-Guerin reduces the risk of progression in
patients with superficial bladder cancer: a meta-analysis of the
published results of randomized clinical trialsJ
Urol16819641970200210.1016/S0022-5347(05)64273-5
|
|
9.
|
A BohlePR BockIntravesical bacille
Calmette-Guerin versus mitomycin C in superficial bladder cancer:
formal meta-analysis of comparative studies on tumor
progressionUrology63682687200410.1016/j.urology.2003.11.049
|
|
10.
|
RA BadalamentHW HerrGY WongA prospective
randomized trial of maintenance versus nonmaintenance intravesical
bacillus Calmette-Guerin therapy of superficial bladder cancerJ
Clin Oncol54414491987
|
|
11.
|
MA HudsonTL RatliffDP GillenEO HaaffSM
DresnerWJ CatalonaSingle course versus maintenance bacillus
Calmette-Guerin therapy for superficial bladder tumors: a
prospective, randomized trialJ Urol1382952981987
|
|
12.
|
H AkazaS KameyamaT KakizoeAblative and
prophylactic effects of BCG Tokyo 172 strain for intravesical
treatment in patients with superficial bladder cancer and carcinoma
in situ of the bladder. Bladder cancer BCG Study GroupNippon
Hinyokika Gakkai Zasshi831831891992(In Japanese).
|
|
13.
|
J PalouP LagunaF Millan-RodriguezRR HallJ
Salvador-BayarriJ Vicente-RodriguezControl group and maintenance
treatment with bacillus Calmette-Guerin for carcinoma in situ
and/or high grade bladder tumorsJ
Urol16514881491200110.1016/S0022-5347(05)66333-111342902
|
|
14.
|
H KogaS OzonoT TsushimaMaintenance
intravesical bacillus Calmette-Guerin instillation for Ta, T1
cancer and carcinoma in situ of the bladder: randomized controlled
trial by the BCG Tokyo Strain Study GroupInt J
Urol17759766201010.1111/j.1442-2042.2010.02584.x
|
|
15.
|
S JungSI JungJI ChungBacillus
Calmette-Guerin intravesical therapy in superficial bladder cancer:
the early experience of comparison of 6 week course and modified 6
3 maintenance therapyKorean J
Urol49703708200810.4111/kju.2008.49.8.703
|
|
16.
|
A PawinskiR SylvesterKH KurthA combined
analysis of European Organization for Research and Treatment of
Cancer, and Medical Research Council randomized clinical trials for
the prophylactic treatment of stage TaT1 bladder cancer. European
Organization for Research and Treatment of Cancer Genitourinary
Tract Cancer Cooperative Group and the Medical Research Council
Working Party on Superficial Bladder CancerJ
Urol156193419411996
|
|
17.
|
DL LammDR RiggsCL TraynelisUO
NseyoApparent failure of current intravesical chemotherapy
prophylaxis to influence the long-term course of superficial
transitional cell carcinoma of the bladderJ
Urol15314441450199510.1016/S0022-5347(01)67427-57714962
|
|
18.
|
H AkazaS HinotsuY AsoT KakizoeK
KoisoBacillus Calmette-Guerin treatment of existing papillary
bladder cancer and carcinoma in situ of the bladder. Four-year
results The Bladder Cancer BCG Study
GroupCancer7555255919957812924
|
|
19.
|
SG ChangSJ LeeJS HuhJH LeeChanges in
mucosal immune cells of bladder tumor patient after BCG
intravesical immunotherapyOncol Rep8257261200111182036
|