Introduction
Recent research has demonstrated that cancer stem
cells (CSCs) appear to be particularly resistant to conventional
chemo- and radiation therapies compared to the non-CSC compartment.
Conventional cytotoxic therapies initially shrink the bulk of a
tumor, but fail to eradicate it, resulting inevitably in tumor
recurrence. Treatment failure may in part be due to preferential
resistance of CSCs to chemotherapeutic agents (1,2). Bao
et al demonstrated that the population of cells enriched for
glioma CSCs was dramatically increased by irradiation, and that
radioresistant gliomas showed an increased percentage of
CD133-positive cells (3). Tsuchida
et al showed that anticancer drug treatment increases the
side-population fraction (considered as CSCs) in cancer cell lines
(4). Accordingly, we also
hypothesized that chemoradiotherapy (CRT) decreased non-CSCs which
are sensitive to CRT, while it increased the percentage of putative
CSCs characteristic of CRT resistance in the population of residual
cancer cells.
A cell surface protein, CD133, known as prominim-1,
is regarded as one of the most important markers of colon CSCs as
reported by two studies which demonstrated that CD133-expressing
cells sorted by a fluorescence-activated cell sorting system
exhibited tumor-forming abilities in xenografts (5,6). A
transmembrane glycoprotein molecule, CD44, is a widely expressed
cell surface hyaluronan receptor found in normal epithelial,
mesenchymal and hematopoietic cells. CD44 has also been reported as
an important cell surface marker for isolating colon CSCs (7–9).
Previous reports have demonstrated that both CD133 and CD44 are of
functional importance for colon CSCs. However, it remains to be
resolved whether CD133 or CD44 expression is clinically important
in CRT-surviving cells (residual cancer cells after CRT), or
whether CRT may increase the expression of these markers.
In this study, we investigated both CD133 and CD44
expression in residual cancer cells after CRT, and evaluated their
association with clinicopathological variables and clinical outcome
of rectal cancer patients. We also examined whether irradiation by
itself induces these markers in a human colon cancer cell line.
Materials and methods
Patients
A total of 52 patients with advanced rectal cancer
were included. All patients were treated with pre-operative CRT
followed by surgery at the Department of Gastrointestinal and
Pediatric Surgery, Mie University Graduate School of Medicine.
Formalin-fixed paraffin-embedded (FFPE) specimens were available
for this study. Thirty endoscopic tumor biopsy specimens before CRT
matched to the FFPE specimens were snap frozen in liquid nitrogen
and kept at −80°C until use. All patients signed informed consent
forms for their tissue to be used in this study. Selection criteria
were the availability of isolated RNA with quality suitable for
real-time PCR and complete clinical data.
Treatment
Pre-operative CRT regimen included 4 cycles of
5-fluorouracil (5FU) administered as 600 mg/m2 for 24 h
on a continuous intravenous route, and tegafur-uracil (UFT)
administered as 400 mg/m2 for 5 days orally, with
concurrent 20–45 Gy pelvic radiotherapy using a four-field box
technique. All patients underwent computed tomography simulation
for three-dimensional radiotherapy planning and were treated with a
10-MV photon using a linear accelerator. The radiation field
encompassed a volume that included the primary tumor, mesorectum,
presacral space, whole of the sacral hollow and regional lymph
nodes. The superior border was placed at L5/S1 and the inferior
border at ≥3 cm caudal to the primary tumor. The regimen of
chemotherapy was based on the combination of continuous infusion of
5FU and UFT (10). The time
interval between pre-operative CRT and rectal resection with total
mesorectal excision (TME) was 2–6 weeks. No delay of each treatment
due to severe toxicity was experienced. All patients underwent
standard surgery, including TME, and received 5FU-based adjuvant
chemotherapy after surgery for 6 months to 1 year.
Pathological evaluation and treatment
response
Pathological evaluation in the resection specimens
was performed according to TNM classification (11). Tumor regression of the primary
tumor was semi-quantitatively determined by the amount of viable
tumor vs. the amount of fibrosis. This ranged from no evidence of
any treatment effect to a complete response with no viable tumor
identified, as described by Dworak et al (12). Tumor regression grade (TRG) 0 was
defined as no regression; TRG1, minor regression (dominant tumor
with fibrosis in ≤25% of the tumor mass); TRG2, moderate regression
(dominant tumor with fibrosis in 26–50% of the tumor mass); TRG3,
good regression (>50% tumor regression); and TRG4, total
regression (no viable tumor cells, only fibrotic mass).
Microdissection in FFPE specimens
Tumor specimens were fixed in 10% formaldehyde
solution and embedded in paraffin. Sections of FFPE specimens
(10-μm) were stained with nuclear fast red and subsequently
manually microdissected to collect residual cancer and stromal
cells, with reference to H&E sections.
RNA extraction from FFPE specimens
Microdissected samples were digested with proteinase
K in lysis buffer containing Tris-HCl, EDTA and sodium dodecyl
sulfate, as previously reported, with minor modifications (13). RNA was purified by phenol and
chloroform extraction.
cDNA synthesis
cDNA was synthesized with random hexamer primers and
Superscript III reverse transcriptase (Invitrogen, Carlsbad, CA,
USA), according to the manufacturer's instructions.
Real-time quantitative RT-PCR
Real-time quantitative RT-PCR analysis was performed
with the SYBR Green PCR Master Mix using an Applied Biosystems 7500
Real-Time PCR System according to the manufacturer's instructions
(Applied Biosystems, Inc., Foster City, CA, USA). Primers and
probes for CD133, CD44 and β-actin were designed with Primer3
software (Biology Workbench version 3.2; San Diego Supercomputer
Center, University of California, San Diego, CA, USA). Sequences
were as follows: CD133 specific primers sense,
GCTTTGCAATCTCCCTGTTG; antisense, TTGATCCGGGTTCTTACCTG; CD44
specific primers sense, CGGACACCATGGACAAGTTT; antisense,
CACGTGGAATACACCTGCAA; and β-actin sense, ACAGAGCCTCGCCTTTGC;
antisense, GCGGCGATA TCATCATCC. PCR was performed in a final volume
of 25 μl with a SYBR Green PCR Master Mix using 1 μl cDNA, 400 nM
of each primer for the respective genes. Cycling conditions were
50°C for 2 min and 95°C for 10 min, followed by 40 cycles at 95°C
for 15 sec and 60°C for 1 min.
Relative mRNA levels of target genes
Relative mRNA levels were determined by the standard
curve method. The standard curves and line equations were generated
using 5-fold serially diluted solutions of cDNA from the LoVo colon
cancer cell line. All standard curves were linear in the analyzed
range with an acceptable correlation coefficient (R2).
The levels of target gene expression were calculated from the
standard curve. Quantitative normalization of cDNA in each sample
was performed using the expression of the β-actin gene as an
internal control. Finally, mRNA levels of the target gene were
expressed as ratios to β-actin mRNA levels. Real-time PCR assays
were carried out in duplicate for each sample and mean values were
used for the calculation of the mRNA levels.
Cell culture
The HT29 human colon cancer cell line was grown in
monolayer cultures in RPMI-1640 (Sigma-Aldrich, Inc., St. Louis,
MO, USA) supplemented with fetal bovine serum [FBS; 10% (v/v);
Gibco Brl., Tokyo, Japan), glutamine (2 mM), penicillin (100,000
U/l), streptomycin (100 mg/l) and gentamycin (40 mg/l) at 37°C in a
5% CO2 environment.
For routine passage, cultures were spilt 1:10 when
they reached 90% confluence, generally every 3 days. Cells at the
fifth to ninth passage were used for all experiments, which were
performed with exponentially growing cells.
Radiation exposure
HT-29 cells were plated at a density of
104 cells/well in three 100-mm culture dishes (BD
Falcon). Exponentially growing cells were plated on a 10-cm dish
and irradiated at doses of 1, 2.5 and 5 Gy (CAX-150-20; Chubu
Medical Co., Ltd.). Non-irradiated controls were handled
identically to the irradiated cells with the exception of the
radiation exposure. After irradiation, cultures were kept at 37°C
and 5% CO2 in an incubator.
Clonogenic survival assay after
radiation
Colony formation assays were performed in
triplicates. After 10–14 days of incubation, cells were fixed for
15 min with 2% formaldehyde and stained for 15 min with 0.5%
crystal violet. Colonies were counted when they contained >50
cells. The number of colonies was counted, then the surviving
fraction was normalized to the surviving fraction of the
corresponding control.
Western blot analysis
Plates were washed in ice-cold PBS, and cold lysis
buffer (Tris-buffered saline, pH 7.5, containing 1% Triton X-100)
was added directly to the plates. Cells were scraped from plates,
collected and homogenized using a Mixer Mill MM 300 homogenizer
(Qiagen Inc., Chatsworth, CA, USA). Supernatants were collected and
frozen at −20°C until use. The protein concentration was measured
by the BCA protein assay (Pierce, Rockford, IL, USA). Lysate
proteins (20 μg) were mixed with an equal volume of 2X Laemmli's
loading buffer containing 2ME and heated at 100°C for 5 min.
Samples were electrophoretically separated on 12.5% gradient
polyacrylamide gels containing 0.1% SDS, followed by semi-dry
transfer to an Immun-Blot PVDF membrane (Bio-Rad Laboratories,
Hercules, CA, USA). The membranes were blocked using 5% skimmed
milk in Tris-buffered saline, pH 7.5, supplemented with 0.1%
Tween-20 (TBS-T). The blots were then incubated with rabbit
monoclonal anti-CD133 antibody (Cell Signaling Technology, Inc.,
Boston, MA, USA) at a 1:1,000 dilution, mouse monoclonal anti-CD44
antibody (R&D Systems, Inc., Minneapolis, MN, USA) at a 1:1,000
dilution, and mouse monoclonal anti-actin (clone C4) antibody (MP
Biomedicals, LLC, Solon, OH, USA) at a 1:400 dilution in 5% skimmed
milk in TBS-T overnight at 4°C. After washing three times in TBS-T,
the blots were incubated with alkaline-phosphatase-conjugated goat
anti-rabbit or mouse IgG (Promega, Madison, WI, USA) at a 1:200
dilution in 5% skimmed milk in TBS-T. Following treatment with an
enhanced chemiluminescence detection solution, chemiluminescent
signals were visualized using CS Analyzer and AE-6962 Light Capture
(ATTO Corp., Tokyo, Japan).
Immunohistochemistry
Sections of FFPE specimens (2-μm) were constructed.
After deparaffinization and dehydration for antigen unmasking,
specimens were brought to a boil in 10 mM sodium citrate buffer.
Specimens were then blocked and incubated with primary antibody
overnight at 4°C. The antibody was detected by Envision reagents
(Envision kit/ HRP; Dako Cytomation, Denmark). All sections were
counterstained with hematoxylin. Primary CD133 rabbit monoclonal
antibody and CD44 mouse monoclonal antibody were used in dilutions
of 1:150 and 1:1,000 with labeled streptavidin biotin method (LASB2
kit/HRP; Dako Cytomation) added. Negative controls were run
simultaneously with pre-immune immunoglobulin.
Statistical analysis
All statistical analyses were carried out using JMP
version 5 (SAS Institute Inc., Cary, NC, USA). The value of each
target gene was expressed as a median value (inter-quartile range).
Associations between gene expression levels (continuous variables)
and clinicopathological variables (categorical variables) were
evaluated using Mann-Whitney U-test for two groups, or
Kruskal-Wallis test for multiple groups. Disease-free survival was
calculated from the date of surgery to the date of disease
recurrence. Overall survival was calculated from the date of
surgery to the date of death due to rectal cancer or last
follow-up. Survival was evaluated using the Kaplan-Meier method.
The log-rank test was used to compare the cumulative survival
durations in the patient groups. A non-parametric receiver
operating characteristic (ROC) analysis was performed to calculate
the best cutoff values predictive of distant recurrence using
Medcalc 7.2 for Windows (Mariakerke, Belgium). P-values of <0.05
were considered statistically significant.
Results
Patient and tumor characteristics
Fifty-two patients were included in this study. The
median age was 65 years (range 37–78). The male-to-female ratio was
42:10. The post-CRT pathological T stages were pT1–2 (35%) and
pT3–4 (65%), respectively. Seventeen patients (33%) had
pathological lymph node metastases. Lymphatic invasion was present
in 39 of 52 patients (75%), and vascular invasion was present in 30
patients (58%). Forty-five tumors (87%) showed well- or moderately
differentiated adenocarcinoma histology. None of the patients had
local recurrence. Patterns of distant recurrence included liver and
lung metastases in 3 patients, lung metastases alone in 4 patients,
and peritoneal metastasis in 1 patient.
Pathological response to
chemoradiotherapy
TRG was as follows: TRG0, 0 patients (0%); TRG1, 10
patients (20%); TRG2, 22 patients (42%); TRG3, 20 patients (38%)
and TRG4, 0 patients (0%). No TRG4 (complete regression of the
primary tumor) was noted in this study because of the
unavailability of residual cancer cells.
Associations of post-CRT CD133 and CD44
with clinico-pathological variables
The expression values (relative mRNA levels) of
CD133 and CD44 were expressed as ratios between the gene of
interest (CD133 and CD44) and the internal reference gene
(β-actin), providing a normalization factor for the amount of RNA.
Median value of post-CRT CD133 and CD44 mRNA levels was 0.104
(inter-quartile range 0.031-0.422) and 0.442 (inter-quartile range
0.242–0.875), respectively. Associations of post-CRT CD133 and CD44
with clinicopathological variables are summarized in Table I. CD133 was significantly higher in
patients with vascular invasion compared to those without (P=0.02).
CD44 was significantly higher in female patients compared to male
patients (P=0.02). Pathological T1–2 tumors had higher CD44
expression than pathological T3–4 tumors (P<0.05). As shown in
Table II, patients who developed
metachronous distant recurrence (n=8) had significantly higher
post-CRT CD133 levels compared to the patients without recurrence
(n=44; P=0.0209). No significant association between distant
recurrence and CD44 was observed.
 | Table I.Association of post-CRT CD133 and
CD44 with clinicopathological variables. |
Table I.
Association of post-CRT CD133 and
CD44 with clinicopathological variables.
| Variable | No. | CD133 | P-value | CD44 | P-value |
|---|
| Gender | | | | | |
| Male | 42 | 0.099 | | 0.411 | |
| Female | 10 | 0.132 | 0.83 | 1.063 | 0.02 |
| Age (years; median
65) | | | | | |
| ≤65 | 26 | 0.065 | | 0.457 | |
| >65 | 26 | 0.114 | 0.29 | 0.408 | 0.35 |
| Pathological T
category | | | | | |
| T1–2 | 18 | 0.087 | | 0.734 | |
| T3–4 | 34 | 0.125 | 0.30 | 0.356 | <0.05 |
| Pathological N
category | | | | | |
| Present | 17 | 0.097 | | 0.350 | |
| Absent | 35 | 0.107 | 0.56 | 0.524 | 0.08 |
| Histology | | | | | |
|
Well/moderate | 45 | 0.107 | | 0.452 | |
|
Poor-mucinous | 7 | 0.097 | 0.89 | 0.350 | 0.95 |
| Lymphatic
invasion | | | | | |
| Present | 39 | 0.148 | | 0.429 | |
| Absent | 13 | 0.032 | 0.06 | 0.773 | 0.41 |
| Vascular
invasion | | | | | |
| Present | 30 | 0.209 | | 0.429 | |
| Absent | 22 | 0.047 | 0.02 | 0.468 | 0.32 |
| Tumor Regression
Grading | | | | | |
| TRG1 | 10 | 0.123 | | 0.617 | |
| TRG2 | 22 | 0.099 | | 0.356 | |
| TRG3 | 30 | 0.079 | 0.78 | 0.582 | 0.21 |
 | Table II.Association of post-CRT CD133 and
CD44 with distant recurrence. |
Table II.
Association of post-CRT CD133 and
CD44 with distant recurrence.
| Target genes | Patients with
distant recurrence (n=8) | Patients without
distant recurrence (n=44) | P-value |
|---|
| CD133 | 0.248
(0.026–1.412) | 0.104
(0.032–0.291) | 0.0209 |
| CD44 | 0.543
(0.285–0.627) | 0.430
(0.228–1.118) | 0.4599 |
Predictive values of post-CRT CD133 and
CD44 for distant recurrence and overall survival
On the basis of these results, ROC analyses were
used to identify cutoff values of CD133 or CD44 predictive of
distant recurrence and overall survival. A non-parametric ROC
analysis showed that the best cutoff values of CD133 and CD44 for
distant recurrence were 1.225 and 0.64, respectively. The best
cutoff values of CD133 and CD44 for overall survival were 0.21 and
1.648, respectively. As shown in Fig.
1, patients with post-CRT CD133 above the cutoff value (High)
showed significantly worse disease-free survival (log-rank test;
P=0.0229).
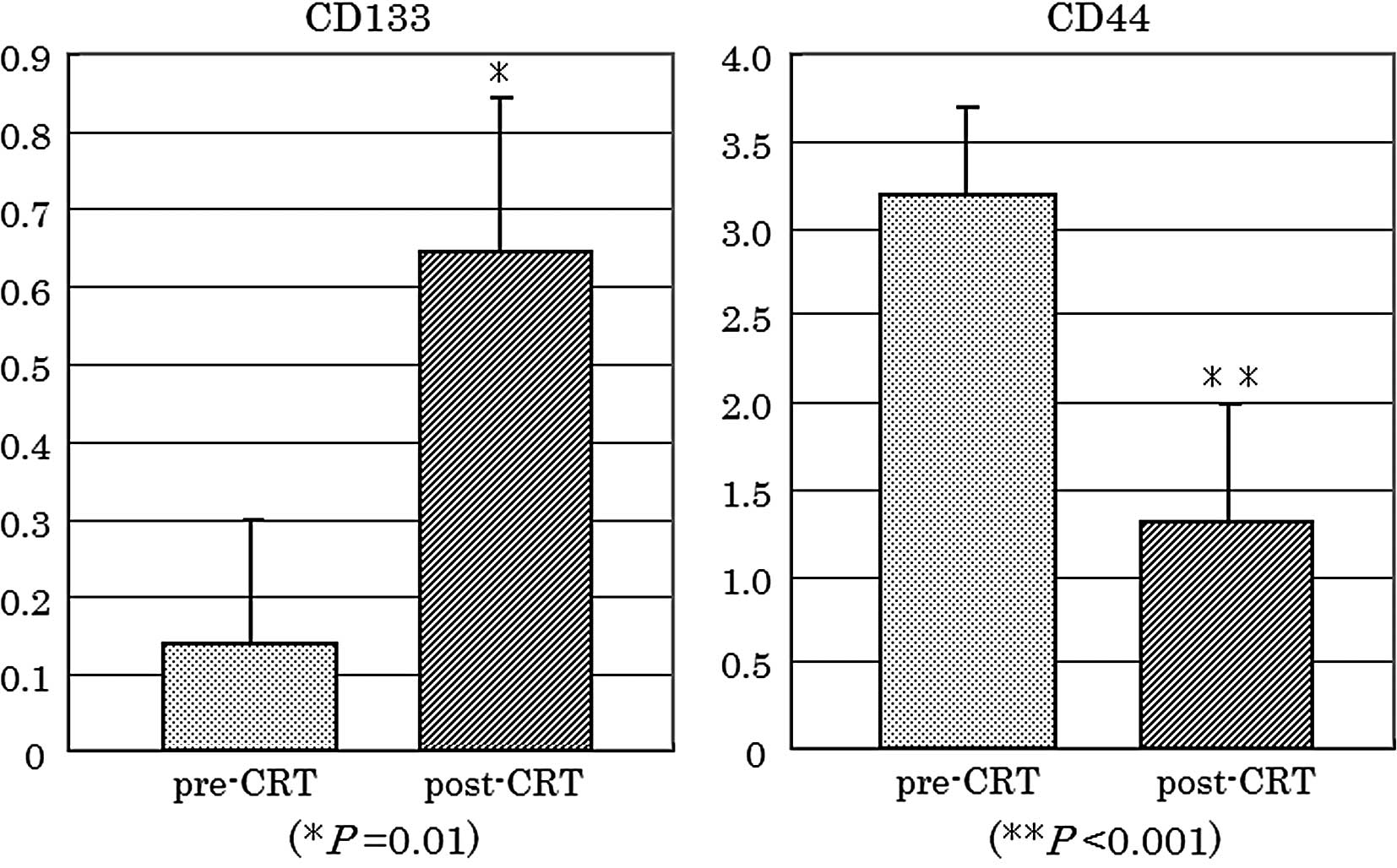
CD133 and CD44 expression in paired pre-
and post-CRT specimens
To confirm whether CD133 and CD44 expression was
altered during CRT, expression of each gene was compared between
matched pre-CRT and post-CRT specimens (n=30). As shown in Fig. 2, CD133 was significantly increased
in post-CRT specimens (P=0.01), compared to pre-CRT biopsy
specimens. By contrast, CD44 was significantly decreased in
residual cancer cells of the post-CRT specimens (P<0.001).
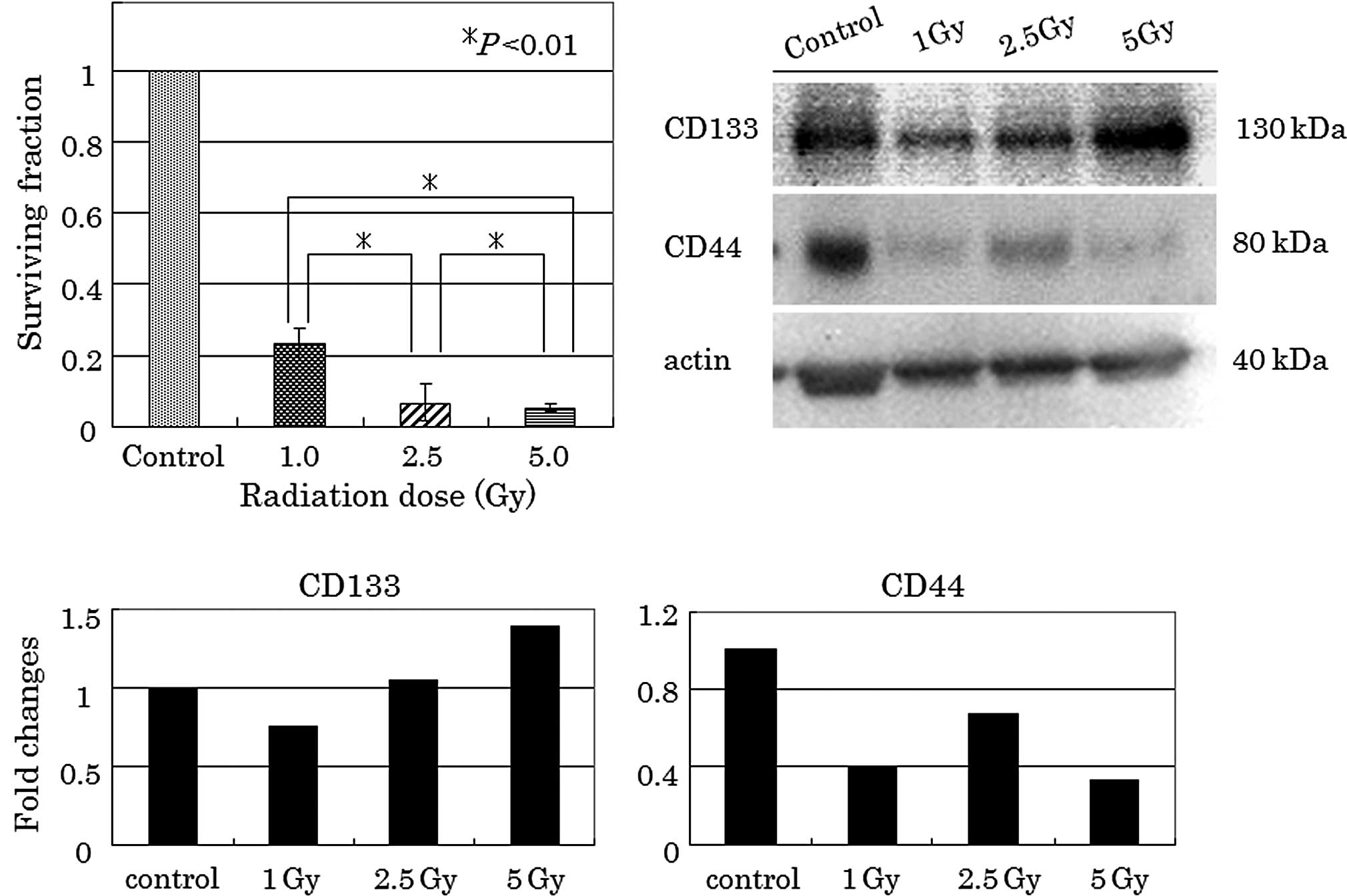
Clonogenic survival of HT-29 cells after
irradiation
Significant reduction in clonogenic survival was
observed in the radiation-treated HT-29 cells (Fig. 3A). Survival fractions of
approximately 23, 7 and 5% were noted when cells were irradiated
with 1, 2.5 and 5 Gy, respectively.
Post-irradiation CD133 and CD44
expression in clonogenic surviving cells
As shown in Fig. 3B and
C, a single dose of 1, 2.5 and 5 Gy radiation increased CD133
protein levels, compared to controls as determined by western blot
analysis. Densitometric analysis showed that CD133 was 1.4 times
increased at 5 Gy radiation with respect to the control. By
contrast, radiation decreased CD44 protein levels, regardless of
the radiation dose.
Immunohistochemistry for CD133 and CD44
in residual cancer cells
The minority of residual cancer cells had
immunoreactive CD133 and CD44 expression within the entire residual
cancer. CD133 was observed diffusely in the cytoplasm of residual
cancer cells, and was also located at an apical/endoluminal surface
(Fig. 4A and C). Immunoreactive
CD44 expression was found as membranous staining (Fig. 4B and D). There was no obvious
concordance between CD133 and CD44 positivity of the residual
cancer cells.
Discussion
The presence of CSCs in the primary tumor appears to
have prognostic significance in several types of malignancies
(14,15). In primary colorectal cancer, CD133
expression has been also reported to be a significant prognostic
marker (16,17). In this study, post-CRT CD133 in
residual cancer cells was significantly associated with
metachronous distant recurrence and poor disease-free survival of
rectal cancer patients, although pre-CRT CD133 in the primary tumor
did not correlate with clinical outcome (data not shown). There are
several potential explanations of these results. First, the small
sample size of pre-CRT biopsies (n=30) may have affected the
results. Second, CRT-resistant surviving cells, which are residual
cancer cells in post-CRT specimens, may have much more putative
CSCs than the pre-CRT primary tumor, so that post-CRT CD133
expression preferentially correlates with clinical outcome. Third,
CRT may alter CD133 expression, resulting in a difference in the
CD133 expression status between pre-CRT and post-CRT specimens.
To clarify whether irradiation may change CD133
expression, we compared CD133 expression in radiation-treated HT-29
cells to that in non-irradiated cells. CD133 protein levels were
increased in a radiation dose-dependent manner, despite the
decreased number of clonogenic radiation-surviving HT-29 cells.
These in vitro findings were consistent with the fact that
CD133 mRNA levels were increased after CRT in comparison to levels
before CRT. These results suggest that not only residual cancer
cells surviving CRT may enrich the population of putative CSCs
expressing CD133, but also CRT may induce CD133 expression. CD44
has been also considered as an important marker for isolating colon
CSCs (7–9). However, there was no significant
association between post-CRT CD44 and clinical outcome.
Furthermore, no significant correlation between CD133 and CD44 mRNA
levels was observed in pre-and post-CRT cancer cells (data not
shown).
Immunohistochemically, there was no clear
concordance between CD133 and CD44 positivity of residual cancer
cells. This may support the hypothesis that immunoreactive
CD133-positive and CD44-positive cells do not colocalize in
colorectal cancer specimens (8).
Introduction of pre-operative CRT and TME for rectal
cancer has improved the sphincter preservation rate, local pelvic
control and survival (18).
However, metachronous distant recurrence remains the major cause of
mortality in rectal cancer patients treated with CRT followed by
TME (19). Our data indicate that
CD133, but not CD44, in residual cancer cells may be significantly
relevant to the clinical outcome of rectal cancer patients who are
treated with pre-operative CRT followed by TME. However, data from
this study should be interpreted with caution. The main limitation
of this study was the relatively small number of patients (n=52),
including only 8 patients with distant recurrence. Large
prospective trials are required to confirm the validity of the
predictive value of post-CRT CD133 for distant recurrence and
survival.
In conclusion, CD133, but not CD44, was increased in
the radiation-resistant surviving colon cancer cells. Post-CRT
CD133 in residual cancer cells may predict metachronous distant
recurrence and poor survival of rectal cancer patients after
CRT.
Abbreviations:
|
RT-PCR
|
reverse transcription-polymerase chain
reaction
|
References
|
1.
|
CE EylerJN RichSurvival of the fittest:
cancer stem cells in therapeutic resistance and angiogenesisJ Clin
Oncol2628392845200810.1200/JCO.2007.15.182918539962
|
|
2.
|
M BaumannM KrauseR HillExploring the role
of cancer stem cells in radioresistanceNat Rev
Cancer8545554200810.1038/nrc241918511937
|
|
3.
|
S BaoQ WuRE McLendonGlioma stem cells
promote radioresistance by preferential activation of the DNA
damage responseNature444756760200610.1038/nature0523617051156
|
|
4.
|
R TsuchidaB DasH YegerCisplatin treatment
increases survival and expansion of a highly tumorigenic
side-population fraction by upregulating VEGF/Flt1 autocrine
signalingOncogene2739233934200610.1038/onc.2008.3818332870
|
|
5.
|
L Ricci-VitianiDG LombardiE PilozziM
BiffoniM TodaroC PeschleR de MariaIdentification and expansion of
human colon-cancer-initiating
cellsNature445111115200710.1038/nature0538417122771
|
|
6.
|
CA O'BrienA PollettS GallingerJE DickA
human colon cancer cell capable of initiating tumour growth in
immunodeficient miceNature445106110200717122772
|
|
7.
|
N HaraguchiM OhkumaH
SakashitaCD133+CD44+ population efficiently enriches
colon cancer initiating cellsAnn Surg Oncol15292729332008
|
|
8.
|
L DuH WangL HeCD44 is of functional
importance for colorectal cancer stem cellsClin Cancer
Res1467516760200810.1158/1078-0432.CCR-08-103418980968
|
|
9.
|
P ChuDJ ClantonTS SnipasCharacterization
of a subpopulation of colon cancer cells with stem cell-like
propertiesInt J Cancer12413121321200910.1002/ijc.2406119072981
|
|
10.
|
R YoshikawaM KusunokiH YanagiDual
antitumor effects of 5-fluorouracil on the cell cycle in colorectal
carcinoma cells: a novel target mechanism concept for
pharmacokinetic modulating chemotherapyCancer Res61102910372001
|
|
11.
|
LH SobinID FlemingTNM Classification of
Malignant Tumors, fifth edition (1997). Union Internationale Contre
le Cancer and the American Joint Committee on
CancerCancer8018031804199710.1002/(SICI)1097-0142(19971101)80:9%3C1803::AID-CNCR16%3E3.0.CO;2-99351551
|
|
12.
|
O DworakL KeilholzA HoffmannPathological
features of rectal cancer after preoperative radiochemotherapyInt J
Colorectal Dis121923199710.1007/s0038400500729112145
|
|
13.
|
KE BijwaardNS AguileraY MonczakM TrudelJK
TaubenbergerJH LichyQuantitative real-time reverse
transcription-PCR assay for cyclin D1 expression: utility in the
diagnosis of mantle cell lymphomaClin Chem47195201200111159766
|
|
14.
|
R LiuX WangGY ChenThe prognostic role of a
gene signature from tumorigenic breast-cancer cellsN Engl J
Med356217226200710.1056/NEJMoa06399417229949
|
|
15.
|
F ZeppernickR AhmadiB CamposStem cell
marker CD133 affects clinical outcome in glioma patientsClin Cancer
Res14123129200810.1158/1078-0432.CCR-07-093218172261
|
|
16.
|
D HorstL KrieglJ EngelT KirchnerA
JungCD133 expression is an independent prognostic marker for low
survival in colorectal cancerBr J
Cancer9912851289200810.1038/sj.bjc.660466418781171
|
|
17.
|
M KojimaG IshiiN AtsumiS FujiiN SaitoA
OchiaiImmunohistochemical detection of CD133 expression in
colorectal cancer: a clinicopathological studyCancer
Sci9915781583200810.1111/j.1349-7006.2008.00849.x18754869
|
|
18.
|
JF BossetL ColletteG CalaisEORTC
Radiotherapy Group Trial 22921Chemotherapy with preoperative
radiotherapy in rectal cancerN Engl J
Med35511141123200710.1056/NEJMoa06082916971718
|
|
19.
|
K BujkoW MichalskiL KepkaPolish Colorectal
Study GroupAssociation between pathologic response in metastatic
lymph nodes after preoperative chemoradiotherapy and risk of
distant metastases in rectal cancer: an analysis of outcomes in a
randomized trialInt J Radiat Oncol Biol
Phys67369377200710.1016/j.ijrobp.2006.08.065
|