Introduction
In numerous tumor types, distant metastases are the
major cause of cancer-related deaths. Metastasis is a complex
process involving several steps: local invasion, adhesion,
migration, survival in the blood or lymphatic system and
extravasation, colonization of distant organs and growth into
tumors. However, cancers exhibit distinct patterns of
organ-specific metastases. Multiple organs may be seeded, but
metastatic tumors may grow in only one or a few of these organs
(1). This non-random process is
dependent on multiple interactions of specific metastatic cells
with the organ-specific microenvironment (2). Scientific understanding of metastatic
spread is limited, and the molecular mechanisms causing particular
characteristics of metastases are largely unknown. In patients with
metastatic nasopharyngeal carcinoma (NPC), the prognosis is
generally poor. Despite modern intensity-modulated radiotherapy,
approximately 20% of patients with stage M0 disease still
experience distant metastases within 3 years after completing
treatment, and the total incidence of distant metastases is between
16 and 42% (3). Median survival of
patients with metastatic NPC is only 11–18 months after metastases
have been identified (4–7). NPC usually metastasizes to the lung,
bone and liver. Final prognosis is dependent on the involved organ.
Patients with liver metastasis (LM) have poorer survival (3–5
months) than patients with metastases in other organs (6–13 months)
(4,7,8).
Knowledge concerning the molecular mechanisms of liver-specific
metastasis in NPC could help guide a clincian towards efficient
treatment and assist in the prediction of final outcome. Among
several proteomic studies on NPC (9–11),
few involved markers of metastasis (12) and none specifically address the
characteristics of liver metastasis. We investigated whether the
behavior of liver metastases is related to changes in plasma
protein markers in patients with NPC.
Materials and methods
This retrospective comparative proteomic study was
approved by the Institutional Blood Sample Library of the Sun
Yat-sen University Cancer Center.
Patients
Valid records of the Sun Yat-Sen University Cancer
Center were searched for patients with a histological diagnosis of
NPC whose serum samples had been obtained at least 3 years prior.
The requirement for blood sample collection more than three years
prior was required, as most NPC patients of distant metastases,
including liver metastases, are identified within 3 years after
completion of radiotherapy (4,7).
Distant metastases were identified via histological evaluation or
imaging combined with a subsequent clinical follow-up examination.
Patient clinical data were collected and survival status was
verified on 31 August 2010 by direct telecommunication with the
patient or patient’s family and verification of clinic attendance
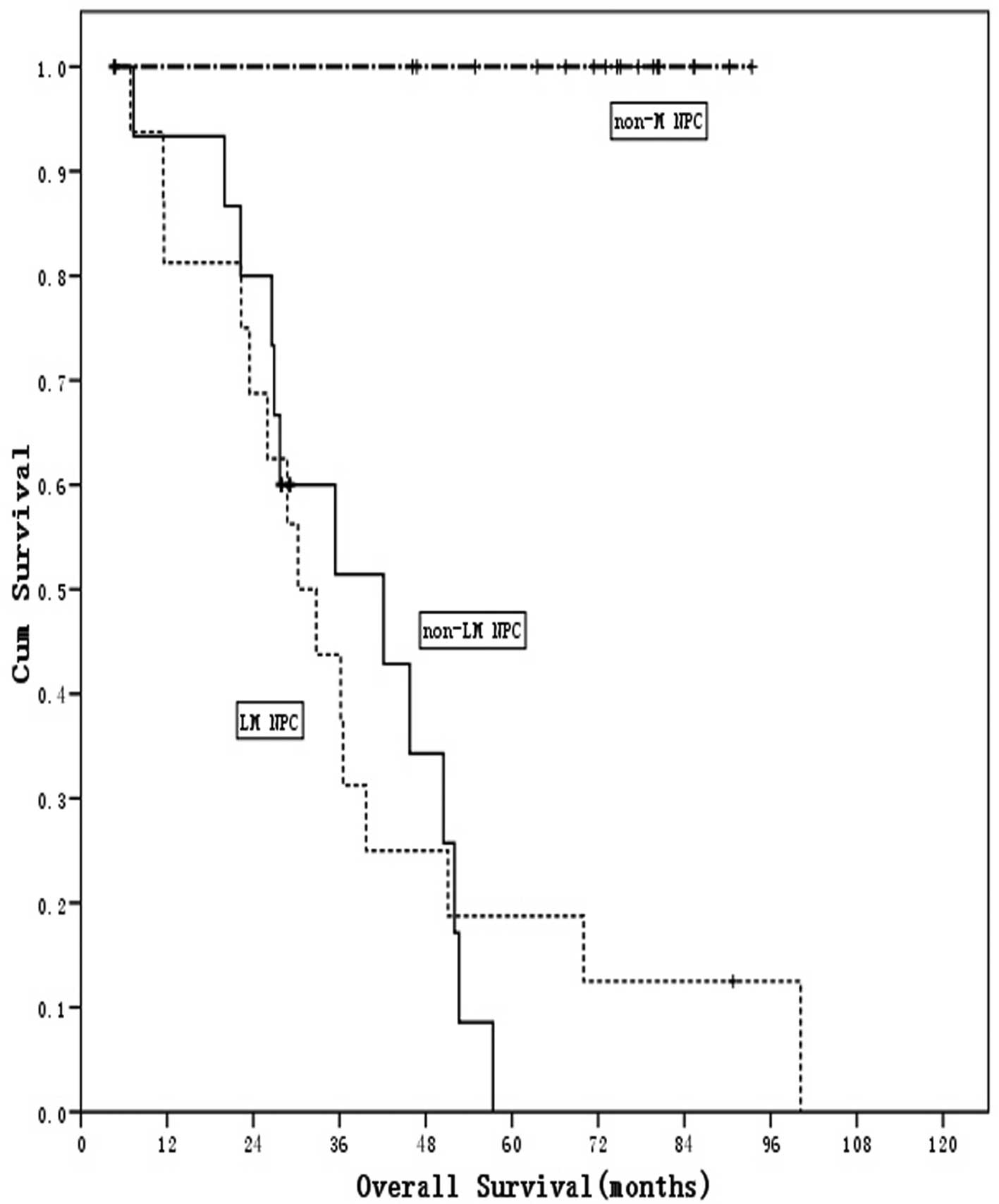
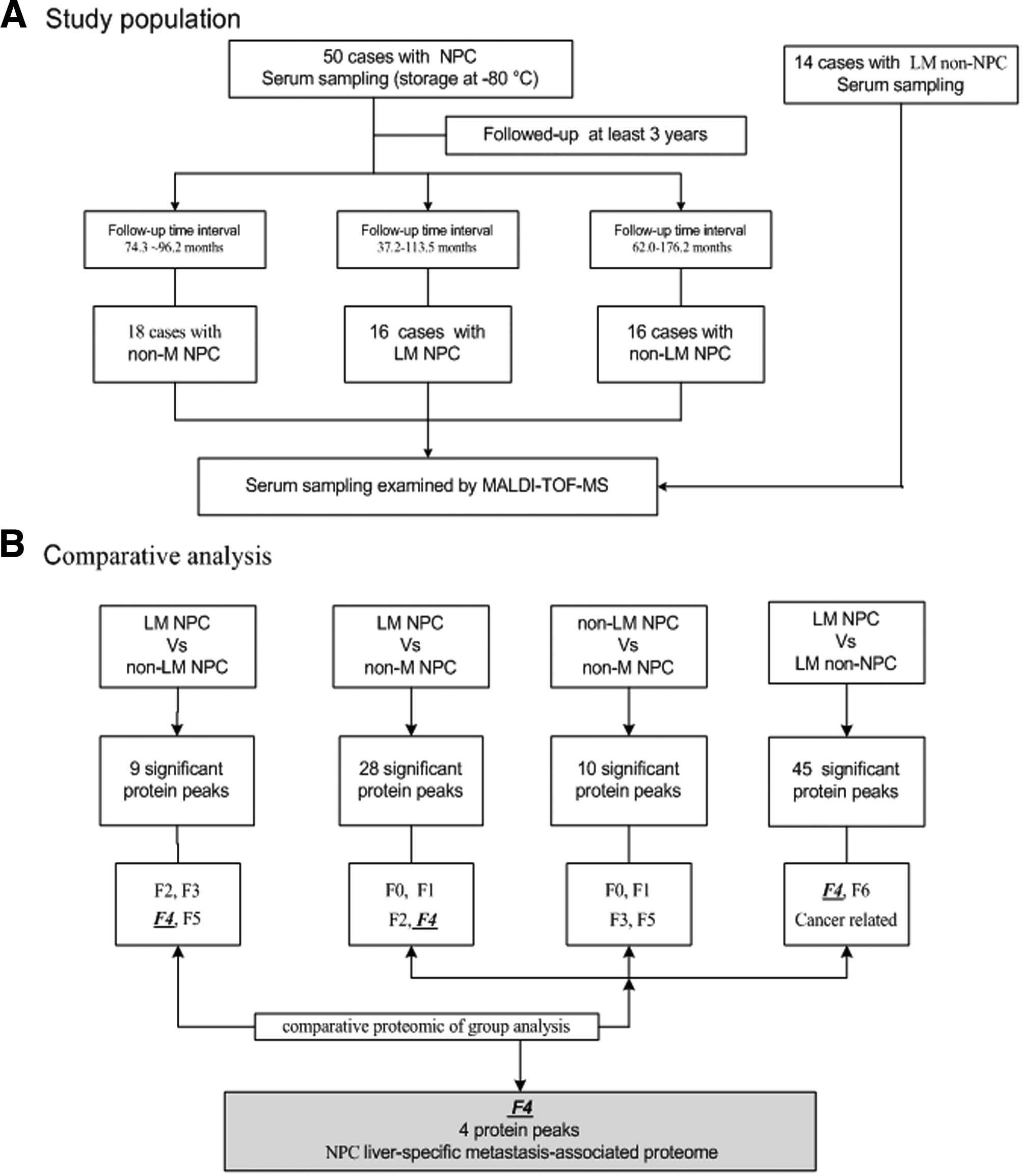
records. The present study included 50 NPC patients (Table I, Fig.
1): 18 cases without distant metastasis (non-M NPC group), 16
patients with liver metastasis (LM NPC group) and 16 patients with
non-liver distant metastasis (non-LM NPC group) prior to the
cut-off follow-up day. To create a control group, serum samples
were collected, as described below, from 14 patients with LM from
other pathologically confirmed forms of cancer (LM non-NPC group).
Of these 14 patients, 11 had colorectal cancer, 1 had pancreatic
cancer, 1 had breast cancer and 1 had ovarian cancer.
 | Table I.Clinical characteristics and long-term
follow-up data for 50 patients with pathologically confirmed
nasopharyngeal carcinoma (NPC), with and without distant
metastases. |
Table I.
Clinical characteristics and long-term
follow-up data for 50 patients with pathologically confirmed
nasopharyngeal carcinoma (NPC), with and without distant
metastases.
| Characteristics | Non-M NPC (n=18) | LM NPC (n=16) | Non-LM NPC
(n=16) |
|---|
| Age, median (range)
in years | 44.7 (32–61) | 45.1 (18–71) | 45.4 (21–65) |
| Gender,
male/female | 13/5 | 10/6 | 12/4 |
| T stage (1998) | | | |
| T1 | 1 | 0 | 1 |
| T2 | 5 | 4 | 3 |
| T3 | 7 | 7 | 11 |
| T4 | 5 | 5 | 1 |
| N stage (1998) | | | |
| N0 | 3 | 2 | 0 |
| N1 | 5 | 4 | 5 |
| N2 | 7 | 6 | 8 |
| N3 | 3 | 4 | 3 |
| Histological
classification (WHO) | | | |
| I | 0 | 1 | 0 |
| II | 8 | 7 | 10 |
| III | 10 | 8 | 6 |
| Presentation of
metastases | | | |
|
Synchronous/metachronous | - | 0/16 | 1/15 |
| Mean follow-up time
(months) | 87 | 82 | 93 |
| Survival status
(alive/deceased) | 18/0 | 1/15 | 3/13 |
| Median overall
survival (months) | - | 33.0 | 36.72 |
| Median metastatic
survival (months) | - | 14.3 | 21.17 |
Blood sample preparation
In the present study, all serum samples from NPC
patients with metastasis were obtained between January 2000 and
July 2007. Samples from 18 cases of non-M NPC were obtained prior
to verifiable distant metastasis during the same period.
Blood samples were collected and processed according
to a standardized protocol: samples were collected in 8.5-ml BD
Vacutainer SST tiger-top tubes and 1 h later were centrifuged at
1400–2000 x g at room temperature for 10 min. Serum (supernatant)
was transferred to 4-ml cryovials, with 1 ml in each and stored at
−80°C until analysis.
Plasma protein fractionation
All plasma samples were thawed and purified using a
reagent set with chemically coated magnetic beads (weak
cation-coated, Bruker Daltonics Co., Billerica, MA). As previously
described (13), serum (2 μl) was
incubated with 5 μl of magnetic beads for 10 min on a ClinProt
robotic platform (Bruker Daltonics Co.) according to the
manufacturer’s specifications. Unbound proteins were discarded and
each sample was washed twice in binding buffer. Briefly, samples
were purified through binding, washing and elution, according to
the manufacturer’s suggested protocol. A total of 5 μl of each
sample was eluted and the purified plasma was further diluted
8-fold with the elution solution in preparation for mass
spectrometry analysis.
Mass spectrometry profiling of the plasma
proteome
For matrix-assisted, laser desorption-ionization,
time-of-flight mass spectrometry (MALDI-TOF-MS) analysis, 1 µl of
the above-mentioned diluted plasma was mixed with 0.5 µl of matrix
solution containing 2 g/l α-cyano-4-hydroxycinnamic acid and 1%
formic acid in 50% acetonitrile and the droplet was allowed to dry
on the MALDI sample plate (AnchorChip, Bruker Daltonics Co.). Mass
spectra were obtained with an Ultraflex MALDI-TOF-MS (Bruker
Daltonics Co.) operated in either positive ion linear or reflectron
mode, depending on the analysis being performed. Profiling data
were acquired in linear mode geometry and mass maps were acquired
in reflectron mode (13,14). All spectra were obtained randomly
over the surface of the matrix spot. The profiling spectra were
calibrated externally using a mixture of protein and peptide
standards (Bruker Daltonics Co.). A ±2 Da mass accuracy for each
spectrum was observed and was likely due to differences in sample
geometry on the plate surface. Briefly, all spectra were processed
by automatic baseline subtraction, peak detection, recalibration
and peak area calculation according to predefined settings. Each
spectrum was the result of 400 laser pulses per m/z segment per
sample delivered in four sets of 100 pulses (at 50 Hz) to each of
four different locations on the surface of the spot.
The criteria for protein mass peak detection (m/z)
were as follows: signal-to-noise ratio (S/N) >5, a 2-Da peak
width filter, and a maximum peak number of 200. The intensities of
the peaks of interest were normalized with the peak intensity of an
ACTH internal standard. More than 10% of the molecular weight was
sieved in simultaneous samples, with the discrepancy of identical
spinnacle in different samples <0.3% after removal of the
initial data noise.
Identifying potential liver-specific,
metastasis-associated protein masses
According to the seed and soil theory of metastasis
and a recent report on the molecular basis of metastasis (2,15),
potential proteomic printing was sorted into seven groups of plasma
markers related to: Factor 0, the absence of distant metastasis
from any cancer; Factor 1, the initiation and progression of
metastasis; Factor 2, liver-specific metastases; Factor 3,
non-liver distant metastases; Factor 4, liver-specific metastases
from NPC; Factor 5, non-liver distant metastases from NPC; Factor
6, liver-specific metastases from non-NPC.
To verify the claim that the peaks identified are
clearly associated with liver-specific metastasis, an attempt to
identify peaks with this comparative analysis of serum proteomic of
the groups was conducted (Fig. 2).
Subsequently, the differential expression of the protein mass peaks
was analyzed by an alternative statistical approach, discriminant
analysis.
Statistical methods
Each spectrum obtained from MALDITOF-MS was analyzed
by ClinProt software version 2.0 (Bruker Daltonics Co.). When
differential expression of the protein mass peaks was identified
between any two groups, these data were imported into the ClinProt
software. Expression of the protein mass peaks was considered to be
significant at a P-value of <0.05. Each serum sample was
processed at least twice to confirm the results and to reduce bias.
In the last step, a commonly used shared nearest neighbors approach
was applied in order to obtain alternative estimates of the
diagnostic potential of combining all peaks. After each diagnostic
model was generated, a 20% leave out cross-validation process was
performed.
Results
As shown in Fig. 2,
28 protein mass peaks from 2000 to 20000 m/z between the LM NPC and
non-M NPC groups were identified, as well as 9 significant protein
mass peaks of protein between LM NPC and non-LM NPC groups, and so
on. By comparing the LM NPC and LM non-NPC groups, one can identify
not only cancer-specific serum peptides (NPC and non-NPC related
markers) but also proteins associated with cancer-specific and
organ-specific metastases (Factor 4, Factor 6). Also by comparing
the LM NPC and non-LM NPC groups, cancer-specific serum peptides,
that is NPC-related markers, and common markers related to
metastasis initiation and progression (Factor 1) could be deleted,
but NPC- and organ-specific, metastasis-associated peptides
(Factors 2–5) could be identified. It is valid that Factor 4 cannot
be obtained by comparing the non-LM NPC and the non-M NPC groups
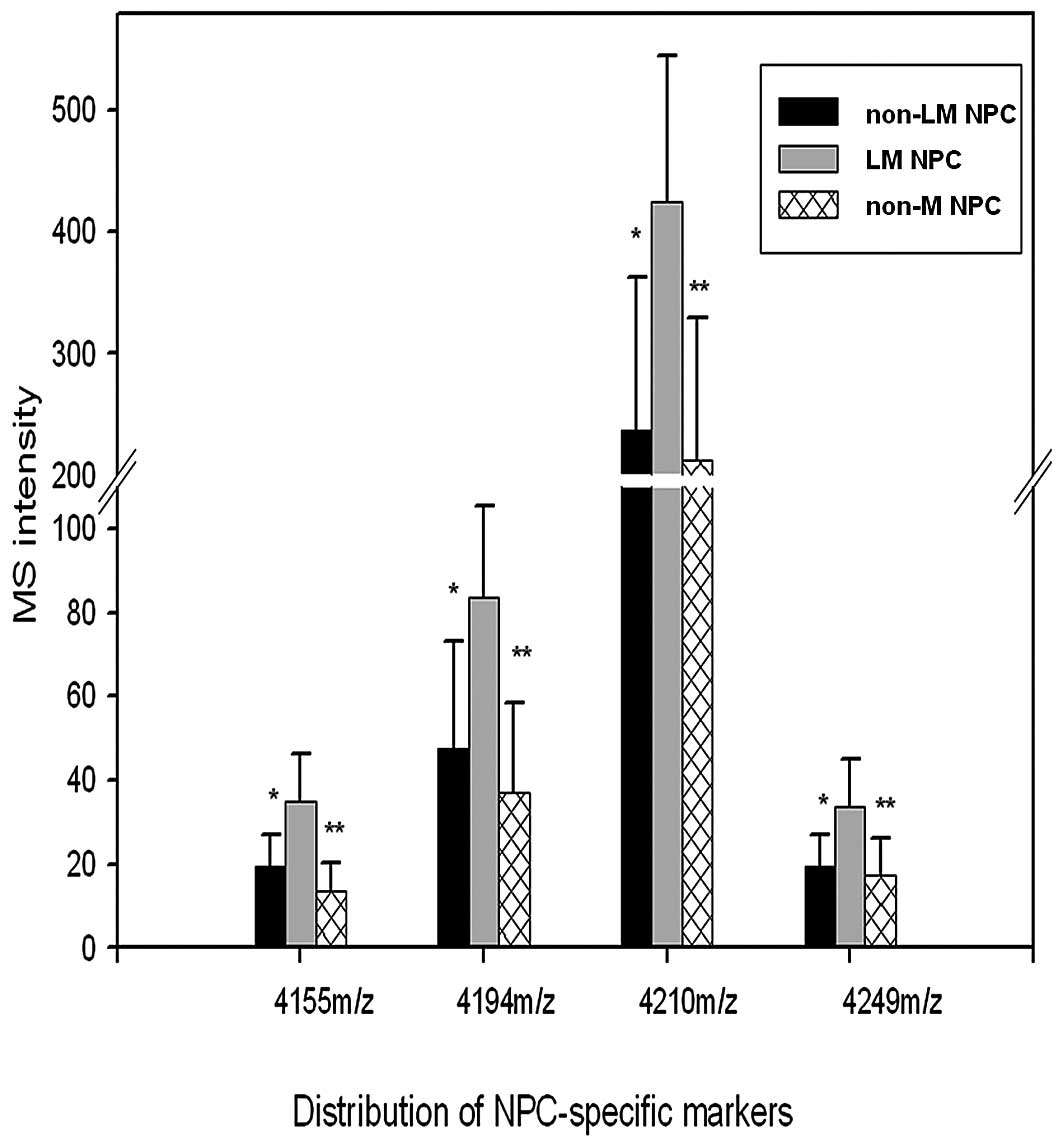
(Fig. 2). After discriminant and
comparison analysis, Factors 4 including 4 protein mass peaks
(4155.34, 4194.87, 4210.78 and 4249.56 m/z) were identified as NPC
liver-specific, metastasis-associated protein peaks (Fig. 1). The value in the LM NPC group was
significantly higher than that of the non-LM NPC and the non-M NPC
groups (Table II, Fig. 3). These four protein mass peaks
were not detected in comparisons between the non-LM NPC and non-M
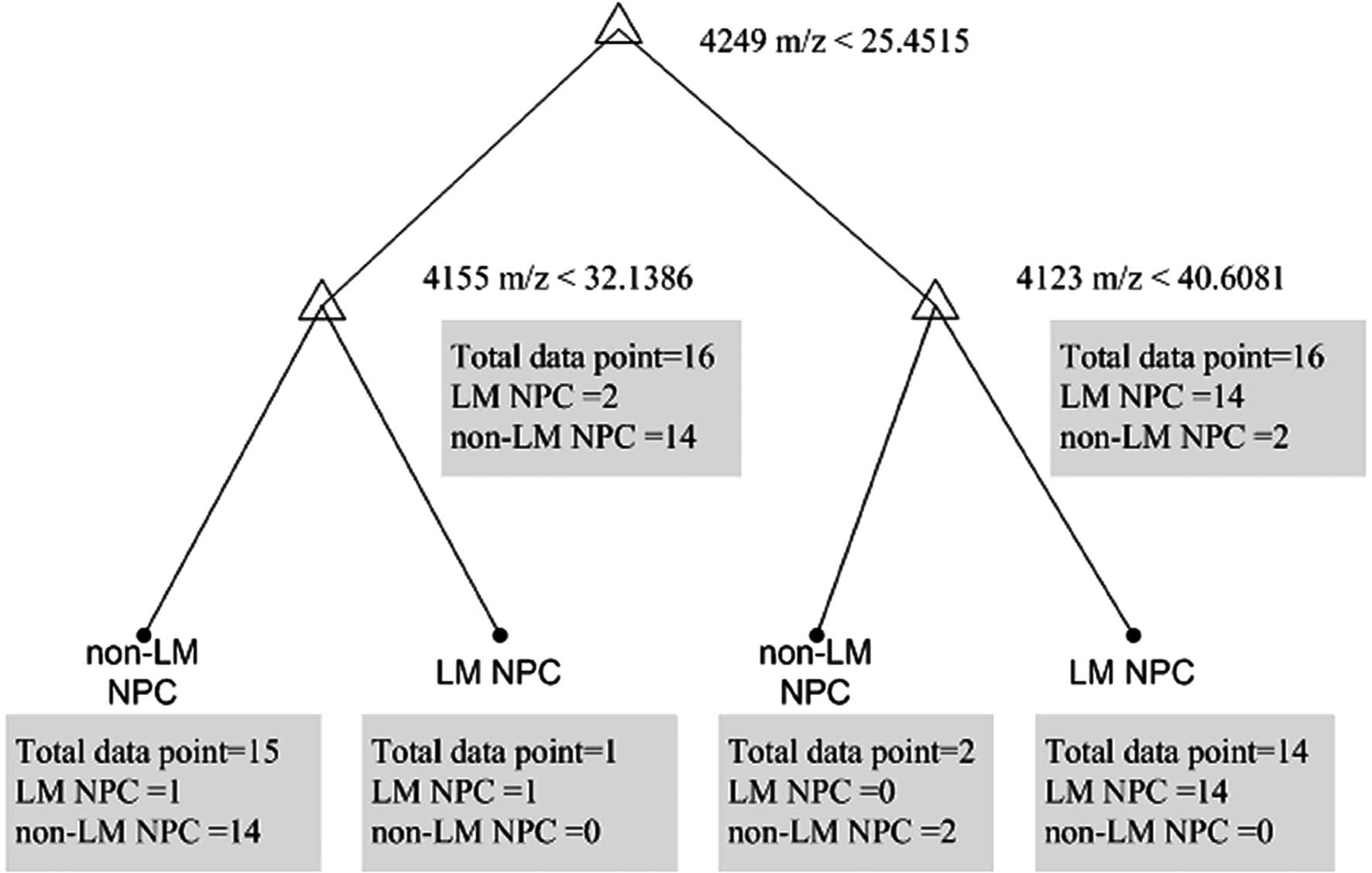
NPC groups. The decision tree differentiated between the LM NPC and
non-LM NPC groups and was built up, and 3 final crunodes consisting
of 4155, 4249 and 4123 m/z were identified (Fig. 4). Two (4155 and 4249 m/z) of these
above four protein mass peaks fulfilled two different statistical
criteria in both ClinProt software analyses and discriminant
analyses.
 | Table II.Mass-to-charge ratios for protein mass
peaks that differentiate between patients who have nasopharyngeal
carcinoma with and without distant metastases. |
Table II.
Mass-to-charge ratios for protein mass
peaks that differentiate between patients who have nasopharyngeal
carcinoma with and without distant metastases.
| Protein mass
peaks | Patients without
distant metastases (n=18) | Patients with liver
metastases (n=16) | Patients without
liver metastases (n=16) |
|---|
| 4155, mean (SD)
m/z | 33.72 (13.52) | 19.28 (11.50) | 7.71 (6.56) |
| P-value | - | 0.00214 | 2.4E-5 |
| 4194, mean (SD)
m/z | 83.63 (37.05) | 47.61 (21.94) | 25.53 (21.43) |
| P-value | - | 0.00199 | 6.84E-6 |
| 4210, mean (SD)
m/z | 425.30 (212.65) | 236.37 (120.77) | 126.44 (116.6) |
| P-value | - | 0.00158 | 9.18E-5 |
| 4249, mean (SD)
m/z | 33.72 (17.14) | 19.28 (17.14) | 7.71 (8.94) |
| P-value | - | 0.00158 | 2.4E-5 |
The above four protein mass peaks were randomly
chosen to ClinProt software by optimization in order to establish
the combined diagnostic model for differentiating between the LM
NPC group from the non-LM NPC group (Table III). The recognition capability of
the diagnostic model for differentiation of the LM NPC group from
the non-LM NPC group was found to be 100% for both groups. The
diagnostic accuracy of cross-verification was 80.5% for the LM NPC
group and 79% for the non-LM NPC group. After deletion of the
4210.78 or the 4194.87 m/z protein mass peaks in the above 4 peaks,
the remaining 3 protein mass peaks were again chosen to establish
the combined diagnostic model for differentiation between the LM
NPC from the non-LM NPC groups. The accuracy for differentiating
the LM NPC group from the non-LM NPC group of the diagnostic models
was once again found to be 100% for both groups. The accuracy of
cross-verification was between 74.2 and approximately 80.5% for the
LM NPC and between 73.3 and approximately 77.8% for the non-LM NPC
groups.
 | Table III.Diagnostic models for differentiating
among patients with and without nasopharyngeal carcinoma and with
and without distant metatases. |
Table III.
Diagnostic models for differentiating
among patients with and without nasopharyngeal carcinoma and with
and without distant metatases.
| Model 1a
| Model 2a
| Model 3a
|
|---|
| Groups | LM NPC | Non-LM NPC | LM NPC | Non-LM NPC | LM NPC | Non-LM NPC | LM NPC | Non-M NPC | LM NPC | LM non-NPC |
|---|
| Protein mass
peaks | 4155, 4194, 4210,
4249 | 4155, 4194,
4249 | 4155, 4210,
4249 | 4055, 4123, 4155,
4210 | 1546, 3192, 3263,
9297 |
| Recognition
capability (%) | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Cross-validation
(%) | 80.5 | 79.0 | 81.2 | 77.8 | 74.2 | 73.3 | 92.9 | 80 | 100 | 100 |
The combined diagnostic model for differentiation
between the LM NPC and non-M NPC, as well as the diagnostic model
for differentiation between the LM NPC from LM non-NPC groups, were
set up as shown in Table III. The
recognition capability and accuracy of cross-verification was
between 80 and approximately 100%.
Discussion
Progression to distant metastasis is a critical
point in the disease course of patients with solid epithelial
malignancies, such as NPC. The standard clinical process for
discovery of distant metastasis is mostly based on imaging. The
early seeding of metastatic cells into the bloodstream is usually
not identified by radiography or scans such as CT and MRI. Also, an
ideal serum tumor marker has yet to be identified for monitoring
the early metastasis of NPC. Such molecular markers need to be
identified, not only for detecting early metastases, but also for
classifying disease and developing appropriate treatments.
Advancements in genomics, proteomics and
bioinformatics have improved our understanding of the cause,
carcinogenesis and progression of the disease (16). Proteomic profiling is based upon
the fact that proteins represent the dynamic state of the cells,
reflecting earlier pathophysiological changes in the disease more
accurately than genomic sequencing (17). Proteomic patterns should assist in
the detection of tumor biomarkers, as well as in evaluating the
efficacy of anticancer drugs. Unfortunately, the proteome
associated with NPC distant metastasis is currently poorly
understood. In this study, an extensive proteomic analysis of
organ-specific metastasis in the serum of patients with NPC was
performed. A standardized serum preparation method for MALDI-TOF-MS
was utilized based on weak cation magnetic beads and was able to
identify many valuable, low-abundance protein masses of interest.
MALDI-TOF-MS is capable of detecting proteins that can aid in the
diagnosis of many common types of cancer. Serum proteomics
profiling may also help predict the response to treatment, in
addition to improving our understanding of metastasis (18). Such analyses have identified
several clues concerning the markers of metastasis. Zheng et
al identified two serum protein biomarkers (9184.4 and 9340.9
m/z) useful for monitoring micro-metastases in colorectal cancer
(19). Another recent study also
associated a collection of membrane and membrane-associated
proteins with colorectal cancer (20). Additionally, protein markers
associated with lymph node metastases in colorectal and prostate
cancer have been profiled (21,22).
In a previous NPC study, assays of MALDI-TOF were
used to detect 13 differentially expressed protein spots. Three
potential NPC metastasis-specific serum biomarkers were further
validated including sICAM-1, HSP70 and SAA, by comparing lymph node
metastasis and non-lymph node metastasis groups (12). Two separate statistical approaches
were used to search for serum biomarkers that were significantly
associated with liver-specific metastasis and two proteins were
identified (4155 and 4249 m/z) that met statistical criteria in
both analyses. With this in mind, several other questions remain
such as which protein and what functions of these identified
protein masses were differentially expressed in our study. Also,
what is the basis for organ-specific metastases associated with
these proteins? As we know, three major theories have been proposed
to explain these organ-specific metastases. According to the first
theory, tumor cells exit the blood and lymphatic systems equally
throughout all organs, but multiply only in those organs which have
the appropriate growth factors. The second theory proposes that the
endothelial cells that line blood vessels in target organs express
adhesion molecules that cause circulating tumor cells to become
attracted in those organs. Finally, the third theory of
‘chemoattraction’ holds that organ-specific attractant molecules
enter the circulation, stimulating the migrating tumor cells to
invade the walls of blood vessels and enter the organs. Therefore,
the further identification of these liver-specific,
metastasis-associated protein peaks may provide us with a better
understanding of the events involved in liver colonization, NPC
metastasis and provide a new mechanistic insight into
organ-specific metastasis and the therapeutic potential for
liver-specific metastasis in NPC. Jun et al identified
(using MALDI-TOF-MS) 6 proteins which are differentially expressed
in a lymph node metastatic prostate cancer group relative to a
localized prostate cancer group which had been previously
identified. These proteins, e-FABP5, MCCC2, PPA2, Ezrin, SLP2 and
SM22, were further identified and validated as functionally
relevant to cancer metastasis in tissue samples using real-time
PCR, western blot analysis and immunohistochemistry staining.
Since the hematogeneous spread of tumor cells is
considered to be a crucial event in metastasis, detecting serum
biomarkers of this event could be of great clinical importance
(17). In the present study, it
was found that 4 serum protein mass peaks (4155.34, 4194.87,
4210.78 and 4249.56 m/z) differentiated LM NPC from non-LM NPC,
which may be an NPC, liver-specific, metastasis-associated
proteomic printing. Simultaneously, the three combined diagnostic
models were also based on serum protein mass peaks that differed
significantly between the LM NPC, non-LM NPC and LM non-NPC groups.
The diagnostic models for differentiating LM NPC and non-M NPC had
similar recognition accuracies when cross-verified (70 to
approximately 80%) by deletion of the 4194.87 or 4210.78 m/z
protein mass peaks in the 4 significant protein mass peaks. As a
result of these findings, there is evidence that the 4 serum
protein mass peaks are useful diagnostic markers for the existence
of LM NPC. In view of the meta-static heterogeneous nature of NPC
and lack of valid methods for detecting early metastases in NPC, we
believe our current proteomic approach has provided valuable
information in the early differentiation between patients with NPC
who have and who do not have liver metastases.
The difference in molecular weight between 4194.87
and 4210.78 m/z is 16 m/z - the molecular weight of oxygen - so one
could postulate that these two protein mass peaks might be the same
protein, with or without oxidation. This postulate needs
verification through further experimentation.
In conclusion, through ClinProt software analysis
and comparative proteomics of group analysis, we identified 4 serum
mass spectrometry protein profiles among 50 patients with
pathologically confirmed NPC who had at least 3 years of clinical
follow-up data. These 4 protein peaks are potentially related to
liver metastasis associated with NPC and are useful diagnostic
markers for the existence of LM NPC.
Acknowledgements
We would like to thank Sun Yat-Sen
University Cancer Center Blood Sample Library and Bioyong
Technologies Inc. This study was supported by the grants from the
Ministry of Science and Technology of China (No. 2006AA02Z4B4).
References
|
1.
|
Husemann Y, Geigl JB, Schubert F, et al:
Systemic spread is an early step in breast cancer. Cancer Cell.
13:58–68. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Chiang AC and Massague J: Molecular basis
of metastasis. N Engl J Med. 359:2814–2823. 2008. View Article : Google Scholar
|
|
3.
|
Kam MK, Teo PM, Chau RM, et al: Treatment
of nasopharyngeal carcinoma with intensity-modulated radiotherapy:
the Hong Kong experience. Int J Radiat Oncol Biol Phys.
60:1440–1450. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Hui EP, Leung SF, Au JSK, et al: Lung
metastasis alone in nasopharyngeal carcinoma: a relatively
favorable prognostic group - a study by the Hong Kong
nasopharyngeal carcinoma study group. Cancer. 101:300–306. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Teo PM, Kwan WH, Lee WY, et al:
Prognosticators determining survival subsequent to distant
metastasis from nasopharyngeal carcinoma. Cancer. 77:2423–2431.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Wang CT, Cao KJ, Li Y, et al: Prognosis
analysis of nasopharyngeal carcinoma patients with distant
metastasis. Ai Zheng. 26:212–215. 2007.PubMed/NCBI
|
|
7.
|
Pan C, He N, Zhao M, et al: Subdividing
the M1 stage of liver metastasis for nasopharyngeal carcinoma to
better predict meta-static survival. Med Oncol. 28:1349–1355. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Huang CJ, Leung SW, Lian SL, et al:
Patterns of distant metastases in nasopharyngeal carcinoma.
Kaohsiung J Med Sci. 12:229–234. 1996.PubMed/NCBI
|
|
9.
|
Huang YJ, Xuan C, Zhang BB, et al:
SELDI-TOF MS profiling of serum for detection of nasopharyngeal
carcinoma. J Exp Clin Cancer Res. 28:852009. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Chang KP, Wu CC, Chen HC, et al:
Identification of candidate nasopharyngeal carcinoma serum
biomarkers by cancer cell secretome and tissue transcriptome
analysis: potential usage of cystatin A for predicting nodal stage
and poor prognosis. Proteomics. 10:2644–2660. 2010. View Article : Google Scholar
|
|
11.
|
Wu CC, Chien KY, Tsang NM, et al: Cancer
cell-secreted proteomes as a basis for searching potential tumor
markers: nasopharyngeal carcinoma as a model. Proteomics.
5:3173–3182. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Liao Q, Zhao L, Chen X, et al: Serum
proteome analysis for profiling protein markers associated with
carcinogenesis and lymph node metastasis in nasopharyngeal
carcinoma. Clin Exp Metastasis. 25:465–476. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Cheng AJ, Chen LC, Chien KY, et al: Oral
cancer plasma tumor marker identified with bead-based
affinity-fractionated proteomic technology. Clin Chem.
51:2236–2244. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Chang JT, Chen LC, Wei SY, et al: Increase
diagnostic efficacy by combined use of fingerprint markers in mass
spectrometry -plasma peptidomes from nasopharyngeal cancer patients
for example. Clin Biochem. 39:1144–1151. 2006. View Article : Google Scholar
|
|
15.
|
Fokas E, Engenhart-Cabillic R, Daniilidis
K, et al: Metastasis: the seed and soil theory gains identity.
Cancer Metastasis Rev. 26:705–715. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Cho WC: Nasopharyngeal carcinoma:
molecular biomarker discovery and progress. Mol Cancer. 6:12007.
View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Hudler P, Gorsic M and Komel R: Proteomic
strategies and challenges in tumor metastasis research. Clin Exp
Metastasis. 27:441–451. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Liao CC, Mehta A, Ward NJ, et al: Analysis
of post-operative changes in serum protein expression profiles from
colorectal cancer patients by MALDI-TOF mass spectrometry: a pilot
methodological study. World J Surg Oncol. 8:332010. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Zheng GX, Wang CX, Qu X, et al:
Establishment of serum protein pattern for screening colorectal
cancer using SELDITOF-MS. Exp Oncol. 28:282–287. 2006.PubMed/NCBI
|
|
20.
|
Luque-Garcia JL, Martinez-Torrecuadrada
JL, Epifano C, et al: Differential protein expression on the cell
surface of colorectal cancer cells associated to tumor metastasis.
Proteomics. 10:940–952. 2010.PubMed/NCBI
|
|
21.
|
Pang J, Liu WP, Liu XP, et al: Profiling
protein markers associated with lymph node metastasis in prostate
cancer by DIGE-based proteomics analysis. J Proteome Res.
9:216–226. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Pei H, Zhu H, Zeng S, et al: Proteome
analysis and tissue micro-array for profiling protein markers
associated with lymph node metastasis in colorectal cancer. J
Proteome Res. 6:2495–2501. 2007. View Article : Google Scholar : PubMed/NCBI
|