Introduction
Hypertension is caused by multiple factors. The
kidney is an organ that plays an important role in the regulation
of blood pressure. The hyperactive sympathetic nervous system in
the kidney has been found to be an important cause of hypertension.
Since the early 1900s, researchers have attempted to explore the
non-drug treatment of hypertension via blocking the sympathetic
nervous system in the kidney. In a multicenter, randomized control
study in 2010 (1), researchers
applied radiofrequency ablation of sympathetic nerves aiming to
treat refractory hypertension. The results demonstrated the safety
and effectiveness of interventional therapy of hypertension.
However, to date, the blood pressure-lowering effect of renal
denervation has not been confirmed and whether another mechanism
apart from suppression of the sympathetic nervous system is
involved is yet unclear. In the present study, the blood pressure,
plasma renalase content and expression of renalase and tyrosine
hydroxylase (TH) in the kidney were detected before and after renal
denervation aiming to explore the mechanism of renal denervation in
lowering blood pressure.
Materials and methods
Animals and main reagents
Spontaneously hypertensive rats (n=48) and
age-matched WKY rats (n=12) weighing 240–280 g were purchased from
Beijing Vitalriver Experimental Animal Co., Ltd. Animals were
housed until they were aged 12 weeks and then used for experiments.
The ELISA kit for renalase detection (Wier Biotech Co., Ltd),
renalase antibody (Abcam), TH antibody (Minipo, USA) and goat
anti-rabbit IgG (Proteintech, USA) were used in the present
study.
Grouping
i) The baseline control group, 12 WKY rats aged 12
weeks, were sacrificed before which the blood pressure was
measured. Then, the blood and kidney were collected for
examination. ii) The baseline group, male SH rats aged 12 weeks
(n=12), were sacrificed before which the blood pressure was
measured. Then, the blood and kidney were collected for
examination. iii) The surgery (renal denervation) group, male SH
rats aged 12 weeks (n=12), received renal denervation. iv) The sham
group, male SH rats aged 12 weeks (n=12), underwent laparotomy but
not renal denervation. v) The control group, male SH rats aged 12
weeks (n=12), were not treated.
In the surgery, sham and control groups the blood
pressure was measured. One and six weeks following surgery, 6
animals in each group were sacrificed at each timepoint and the
blood and kidney were collected for examination.
Surgical procedure
Rats were anesthetized intraperitoneally at room
temperature with chloral hydrate at 25 mg/kg. After sterilization,
a midline incision was made in the abdomen followed by exposure of
the subcutaneous tissues and the kidneys. The ureters and the
arteries, veins and nerves in the sheath were observed. After
stripping the arterial/venous sheath, the renal nerve was exposed
followed by denervation under a microscope (magnification, ×25).
Then, 10% phenol in 95% ethanol was used to treat the tissues
around the veins. In the sham group, laparotomy was performed and
the sympathetic nerve was exposed and treated with normal saline.
The wound was subsequently closed, and rats were allowed to wake
spontaneously. Within 3 days following surgery, intraperitoneal
injection of 16 U of penicillin was administered once daily for
prevention of infection.
Measurement of blood pressure
A non-invasive blood pressure measuring instrument
was used to measure the blood pressure at the tail artery. At room
temperature, the rested rats were fixed on a table, and the balloon
of the measuring instrument was inserted into the proximal end of
the tail artery and the pulse transducer in the abdomen of the
rats. The temperature was then increased to 39°C to completely
dilate the tail artery. The other end of the instrument was
connected to a computer. When the collected signals became stable,
the balloon was inflated until the pulse signal became a straight
line followed by deflation. When the pulse signals formed regular
waves, the blood pressure was calculated with the software. Blood
pressure was measured every 3 min which was performed three times
and the mean was calculated.
Detection of plasma renalase content in
the kidney by ELISA
Washing solution was added to each well followed by
vortexing for 30 sec, and then the washing solution was removed.
These procedures were performed 5 times. Chromogenic reagent A (50
μl) and B (50 μl) were consecutively added to each well followed by
vortexing and incubation in the dark at 37°C for 15 min. Then, stop
solution (50 μl) was added to each well followed by incubation for
15 min (blue to yellow). The optical density (OD) was measured at
450 nm, and the standard curve was delineated. The renalase content
was calculated according to the standard curve.
Detection of renalase and TH expression
by western blot analysis
The kidney was collected from SH rats in the
baseline group and the WKY rats in the baseline control group and
SH rats in the sham, surgery and control groups 1 and 6 weeks after
surgery. The kidney was homogenated in RIPA followed by extraction
of total protein. The protein concentration was detected with the
Bradford method, and proteins were stored at −80°C. The proteins
underwent denaturation for 5 min and were then subjected to
SDS-PAGE for 3 h. Then, the proteins were transferred onto a PVDF
membrane (90 min for TH; 60 min for renalase) which was blocked in
5% non-fat milk in TBST at room temperature for 1 h. The membrane
was incubated with an anti-TH (1:500) or anti-renalase antibody
(1:800) at 4°C overnight and then with a secondary antibody
(1:3,000) at room temperature for 1 (TH) or 2 h (renalase).
Following visualization, Quatity One software was employed to
determine the optical density of the bands.
Statistical analysis
SPSS version 17.0 was employed for statistical
analysis. Quantitative data were expressed as means ± standard
deviation (SD). Normal distribution was tested before comparisons.
Comparisons of means between two groups were carried out with
Student's t-test and those among different groups with one-way
analysis of variance. A P-value <0.05 was considered to indicate
a statistically significant result.
Results
General data
There were no significant differences in the heart
rate and body weight among the surgery, sham and control groups
before and after surgery (P>0.0).
Blood pressure and plasma renalase of the
SH rats in the baseline group and WKY rats
In the SH rats, the systolic blood pressure (SBP),
diastolic blood pressure (DBP) and mean arterial pressure (MAP)
were markedly higher than those in the WKY rats (SBP, 198±29 vs.
140±11 mmHg; DBP, 144±24 vs. 80±9 mmHg; MAP, 163±23 vs. 100±9 mmHg,
P<0.05 for all). SH rats had a markedly reduced plasma renalase
content when compared with the WKY rats (113.8±10.4 vs. 133.0±6.7
μg/ml, P<0.05) (Table I).
 | Table IBlood pressure and plasma renalase of
SH rats in the baseline group and WKY rats (mean ± SD). |
Table I
Blood pressure and plasma renalase of
SH rats in the baseline group and WKY rats (mean ± SD).
| Group (n=12) | SBP (mmHg) | DBP (mmHg) | MAP (mmHg) | Renalase (μg/ml) |
|---|
| SHR | 198±29a | 144±24a | 163±23a | 113.8±10.4a |
| WKY | 140±11 | 80±9 | 100±9 | 133.0±6.7 |
Effect of renal denervation on MAP and
plasma renalase content
Prior to surgery, there were no pronounced
differences in the MAP and plasma renalase content among the
surgery, sham and control groups (P>0.05). One week after the
surgery, the MAP in the surgery group was markedly reduced (131±12,
164±9 and 163±7 mmHg, respectively; P<0.05) while the plasma
renalase content was dramatically increased (127±5.1, 111.7±3.4 and
112.5±5.8 ng/l, respectively; P<0.05) when compared with the
sham and control groups. Six weeks after surgery, no pronounced
differences were found in the MAP and plasma renalase content among
the three groups (P>0.05). In addition, the MAP and plasma
renalase content in the sham group were comparable to those in the
control group before and after surgery (P>0.05) (Table II).
 | Table IIMAP and plasma renalase content before
and after renal denervation (mean ± SD). |
Table II
MAP and plasma renalase content before
and after renal denervation (mean ± SD).
| MAP (mmHg)
| Renalase (μg/ml)
|
|---|
| Group | Before | 1 week | 6 weeks | Before | 1 week | 6 weeks |
|---|
| Surgery | 165±7 | 131±12a–c | 167±4 |
113.8±5.4a,b | 127±5.1a–c | 114.8±6.6 |
| Sham | 165±8 | 164±9 | 170±6 | 111.9±3.7 | 111.7±3.4 | 112.1±7.8 |
| Control | 162±8 | 163±7 | 168±5 | 112.8±6.0 | 112.5±5.8 | 113.4±3.8 |
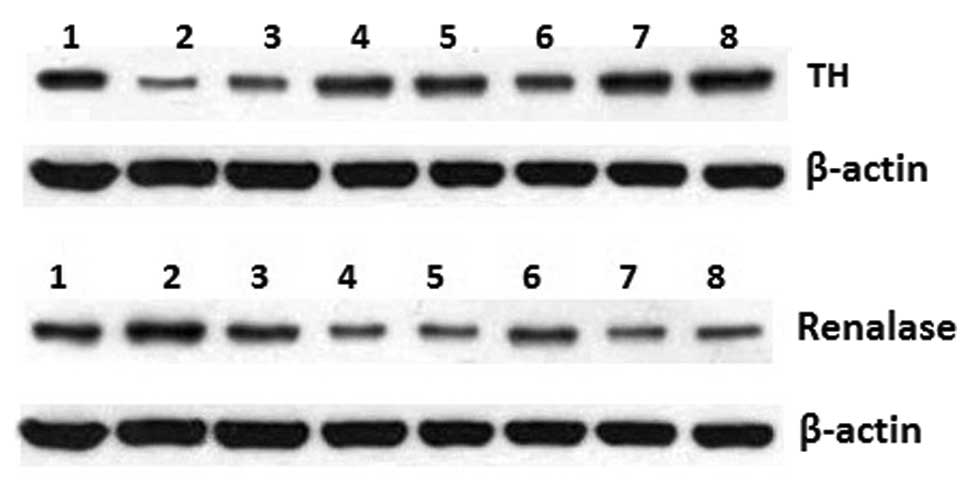
Expression of TH and renalase in the
kidney in the different groups
When compared with the WKY rats, the TH expression
in the kidney of SH rats of the baseline group was markedly
increased while the renalase expression dramatically reduced
(P<0.05). One week after surgery, the TH expression in the
surgery group was markedly reduced and lower than that in the sham
and control groups (P<0.05), while the renalase expression was
dramatically increased (P<0.05). Six weeks after surgery, the TH
expression increased while the renalase expression was reduced as
compared to these values at week 1 but both were comparable to
those in the sham and control groups (P>0.05). There was no
significant difference in the expression of TH and renalase between
the sham or control groups and the baseline group. In addition, no
marked difference was noted between the sham and control groups and
between before and after surgery in both groups (P>0.05)
(Fig. 1 and Table III).
 | Table IIIExpression of TH and renalase in the
kidney in the different groups (mean ± SD). |
Table III
Expression of TH and renalase in the
kidney in the different groups (mean ± SD).
| | | Surgery group
| Sham group
| Control group
|
|---|
| Group | WKY rats | SH rats in baseline
group | 1 week | 6 weeks | 1 week | 6 weeks | 1 week | 6 weeks |
|---|
| TH | 0.241±0.02 | 0.492±0.04a |
0.312±0.02b–d | 0.478±0.01 | 0.507±0.03 | 0.538±0.01 | 0.499±0.04 | 0.555±0.02 |
| Renalase | 0.698±0.01 | 0.403±0.05a |
0.608±0.01b–d | 0.455±0.01 | 0.401±0.03 | 0.405±0.01 | 0.408±0.02 | 0.406±0.01 |
Discussion
The activity of the renal sympathetic nervous system
is a determinant to the occurrence and development of hypertension.
TH is a rate-limiting enzyme in the synthesis of catecholamine and
can reflect the activity of focal sympathetic nerves. Burgi et
al (4) found that TH
expression in the kidney of SH rats was higher than that in
age-matched WKY rats and was positively related to blood pressure.
Our results showed that TH expression in the kidney and blood
pressure of SH rats in the baseline group were higher than those of
the WKY rats, which was consistent with the findings of Burgi et
al (4). This demonstrated that
TH expression can reflect the relationship between the sympathetic
nervous system and blood pressure.
The renalase protein consists of a secretory signal
peptide, a flavin adenine dinucleotide-binding region, and an amine
oxidase domain. Renalase can degrade catecholamine, regulate blood
pressure and protect the myocardium and has been an important
factor in the field of heart and kidney research. Basic research
demonstrated that reduction in renalase contributes to the
occurrence of hypertension (3,4).
Studies revealed that renalase is related to primary hypertension.
In renalase-deficient mice, the SBP, DBP and catecholamine in the
plasma and urine were found to be markedly increased (5–7).
After injection of renalase siRNA, the renalase expression was
markedly reduced accompanied by a significant increase in blood
pressure, which suggests that renalase deficiency contributes to an
increase in blood pressure (8). In
the present study, when compared with the age-matched WKY rats with
normal blood pressure, the renalase expression in the plasma and
kidney was markedly reduced in the SH rats, which was consistent
with previously reports and further confirmed the close
relationship between renalase deficiency and hypertension.
In recent years, renalase has been found to be
closely related to the activity of the renal sympathetic nerves and
blood pressure (9). Clinical and
animal studies (8,10,11)
have shown that the increased activity of the sympathetic nerves
and elevation of blood pressure are usually accompanied by
reduction in renalase expression, and that renalase deficiency may
cause an increase in blood pressure and activity of the sympathetic
nerves. In the present study, the SH rats receiving renal
denervation were used for experiments one week after surgery.
Results showed that MAP and TH expression in the kidney were
markedly reduced in the SH rats one week after surgery while these
values in the sham and control groups were continuously maintained
at a high level, which suggested that renal denervation resulted in
reduction in the activity of renal sympathetic nerves and that the
surgery was successful. In addition, our findings also revealed
that the plasma renalase content and renalase expression in the
kidney one week after surgery were dramatically higher than those
in the sham and control groups. This indicates that renal
denervation lowers blood pressure via affecting renalase
expression.
The nerves in the kidney have important
physiological functions. To date, the mechanism of renal
denervation in lowering blood pressure is still unclear and
renalase may be a participant in this mechanism. Xu et al
(3) intravenously administered
renalase to SD rats, and the results showed a reduction in SBP, DBP
and MAP in these rats. This was also confirmed by our findings.
However, the long-term effect of renal denervation on hypertension
is still poorly understood. As shown in our findings, 6 weeks after
surgery, blood pressure and TH expression increased to a certain
extent in SH rats, while the plasma renalase content and renalase
expression in the kidney reduced to a nearly normal level. Although
differences were found between the surgery and sham groups or the
control group, statistical significance was absent due to the small
sample size. The cause of this finding is still unclear. Following
renal denervation, the autocrine, paracrine or systemic sympathetic
nervous system participates in this feedback, or the nerve
regeneration affects the therapeutic efficacy. Thus, in future
studies, a larger sample size is required to confirm the findings
of the present study.
Taken together, in SH rats, the increased activity
of the renal sympathetic nerves and deficient secretion of renalase
are involved in the pathogenesis of hypertension, and the blocking
of renal sympathetic nerves by denervation may increase the
renalase expression in the kidney and the blood pressure. Our
findings demonstrate that renalase is involved in the reduction of
blood pressure following renal denervation. In recent years,
studies have focused on the development of recombinant or synthetic
renalase as a novel blood pressure-lowering drug (12), which may provide a new strategy for
the treatment of hypertension and other cardiovascular
diseases.
References
|
1.
|
Symplicity HTN-2 Investigators; Esler MD,
Krum H, Sobotka PA, Schlaich MP, Schmieder RE and Böhm M: Renal
sympathetic denervation in patients with treatment-resistant
hypertension (The Symplicity HTN-2 Trial): a randomized controlled
trial. Lancet. 376:1903–1909. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Doumas M, Faselis C and Papademetriou V:
Renal sympathetic denervation and systemic hypertension. Am J
Cardiol. 105:570–576. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Xu J, Li G, Wang P, et al: Renalase is a
novel soluble monoamine oxidase that regulates cardiac function and
blood pressure. J Clin Invest. 115:1275–1280. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Burgi K, Cavalleri MT, Alves AS, et al:
Tyrosine hydroxylase immunoreactivity as indicator immunoreactivity
as indicator of sympathetic activity: simultaneous evaluation in
different tissues of hypertensive rats. Am J Physiol Regul Integr
Comp Physiol. 300:R264–R271. 2011. View Article : Google Scholar
|
|
5.
|
Zhao Q, Fan Z, He J, et al: Renalase gene
is a novel susceptibility gene for essential hypertension: a
two-stage association study in northern Hall Chinese population. J
Mol Med. 85:877–885. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Desir GV: Role of renalase in the
regulation of blood pressure and the renal dopamine system. Curr
Opin Nephrol Hypertens. 20:31–36. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Medvedev AE, Veselovsky AV and Fedchenko
VI: Renalase, a new secretory enzyme responsible for selective
degradation of catecholamines: achievements and unsolved problems.
Biochemistry (Mosc). 75:951–958. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Ghosh SS, Gehr TWB, Sica DA, et al: Effect
of renalase inhibition on blood pressure. J Am Soc Nephrol.
17:208A2006.
|
|
9.
|
Xu J and Desir GV: Renalase, a new renal
hormone: its role in health and disease. Curr Opin Nephrol
Hypertens. 16:373–378. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Desir GV: Regulation of blood pressure and
cardiovascular function by renalase. Kidney Int. 76:366–370. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Schlaich M, Socratous F, Ekelis N, et al:
Renalase plasma levels are associated with systolic blood pressure
in patients with resistant hypertension. J Hypertens. 28:e4372010.
View Article : Google Scholar
|
|
12.
|
Peng M and Jiang XJ: Novel
Renin-angiotensin-aldosterone-system-related targets for
antihypertensive therapy. Adv Cardiovas Dis. 32:13–16. 2011.
|