Introduction
Infusion therapy via a subcutaneously implanted
venous port system is an attractive alternative to infusion via
peripheral veins, peripherally inserted central catheters or
tunneled catheters (1). The use of
subcutaneous infusion ports has become standard practice to obtain
long-term venous access for the administration of chemotherapy,
antibiotics or parenteral nutrition (2). First surgically implanted by
Niederhuber and colleagues in 1982, subcutaneous venous chest ports
were subsequently placed by Morris and coworkers with radiological
guidance (3,4). Subcutaneous venous chest ports can be
placed into jugular and subclavian veins by landmark and
radiological methods. Complication rates have been variously
reported depending on approach sites and methods (1–22).
To the best of our knowledge, few studies have been
published which compare patency periods of port catheters placed
into jugular and subclavian veins using radiological techniques
(3). Our objective was to examine
whether patency times, including complications of subcutaneous
venous chest port insertion using ultrasonography (US) guidance,
are different via jugular and subclavian venous access.
Patients and methods
Patients and ports
Between December 2008 and July 2010, subcutaneous
venous chest ports were placed under US guidance in 347 patients.
From December 2008 to July 2009, our guiding principle was to place
the ports via the subclavian vein. We subsequently changed our
preference to jugular entry due to the greater ease of this
technique. The mean age of the patients was 53.8±13.9 years (range,
16–84). Of the patients, 145 (41.8%) were female and 202 (58.2%)
were male. All except 1 patient with Behçet's disease had
malignancies with or without metastases. The features of the
patients and the procedures recorded in this retrospective cohort
study were age, gender, access method (jugular or subclavian
route), location of primary malignancy, coagulation parameters and
complications.
The titanium chambered ports were single-lumen;
standard size (7.2 F) port systems with lock mechanisms for
catheter attachment. The port type used was Polysite®
(Perouse Laboratoires, Ivry-Le-Temple, France). The ports were
usually placed on the right side, but were placed on the left if
the right side veins had thromboses. The coagulation parameters
were tested prior to each port placement (11) and included platelet count,
prothrombin time, international normalized ratio (INR) and
activated partial thromboplastin time. An effort was made to
correct the deficiencies if any coagulopathy was detected.
Prophylactic antibiotics were not administered to any patient,
including those with fever, until positive culture results.
Exclusion criteria were active systemic or local infections,
coagulopathy (defined as platelet count <50/nl and/or
prothrombin time >18 sec and/or INR>1.5) and the inability to
provide informed consent (23).
Technique of the procedure
Two of the skilled interventional radiologists had
21 years of experience in interventional radiology, including
venous catheterization. The other 6 radiologists performed the
procedure under their observation. The single-lumen port catheters
were placed into the jugular and subclavian veins under US and
fluoroscopy guidance in an interventional radiology suite. Patients
were placed in the supine position. The pectoral and neck regions
were cleansed with povidone-iodine twice. Preprocedural sedation
was not administered, except to uncooperative patients. Sterile
technique was used, in which the skin at the insertion site was
extensively cleansed on the neck or chest. We performed in full
surgical scrubs, wearing surgical caps and masks. US guidance
(Famio 8; Toshiba, Japan) was performed in all procedures. A
high-resolution (11 MHz) linear-array transducer was used with
standard accords in all procedures as B-gain, 80 dB; dynamic range,
55; frame per sec (fps), 15 and standard depth, 5.3 cm. Sterile US
gel and sterile drapes were used to cover the US probe and cable. A
skin incision of 1 cm was made over the jugular or subclavian vein
site following local anesthesia administration. Principally, the
subclavian vein was punctured in the mid or lateral third of the
clavicle to avoid pinch-off. In all patients, venous entry was
performed with an 18 G Seldinger needle and the tip of the
guide-wire was advanced into the vena cava. After puncture, the
subcutaneous pocket was dissected. Following local anesthesia with
2% prilocaine (Citanest®; Eczacıbaşı, Turkey), a 2.5- to
3-cm incision was made ∼3 cm caudal to the clavicle with a number
15 bistoury. The pocket site was the same for jugular and
subclavian access. Using sharp and blunt dissection, a pocket was
created under the fascia of the pectoral muscle and caudally
dissected with a clamp and finger. A sponge was placed into the
pocket for hemostasis prior to port placement. The catheter
connected to the port chamber was tunneled with a trochar to the
venous entry site. The catheter was flushed with diluted heparin
solution using a Huber needle. The Huber needle remained in the
port chamber to prevent flip-over until the end of the procedure.
Stay sutures for the port base were not used in any patient, even
if the patient had loose subcutaneous tissue. The port catheter was
advanced through the peel-away sheath into the vena cava-right
atrium junction. After insertion, the catheter tip was evaluated
using fluoroscopy. Port efficacy was checked with an aspiration of
blood, and the reservoir was flushed with heparinized saline
solution (9 cc 0.9% NaCl plus 1 cc heparin) to show any leakage.
The incision was closed with resorbable 3-0 vicryl subcutaneous
sutures. The skin of the pocket and venous puncture site was closed
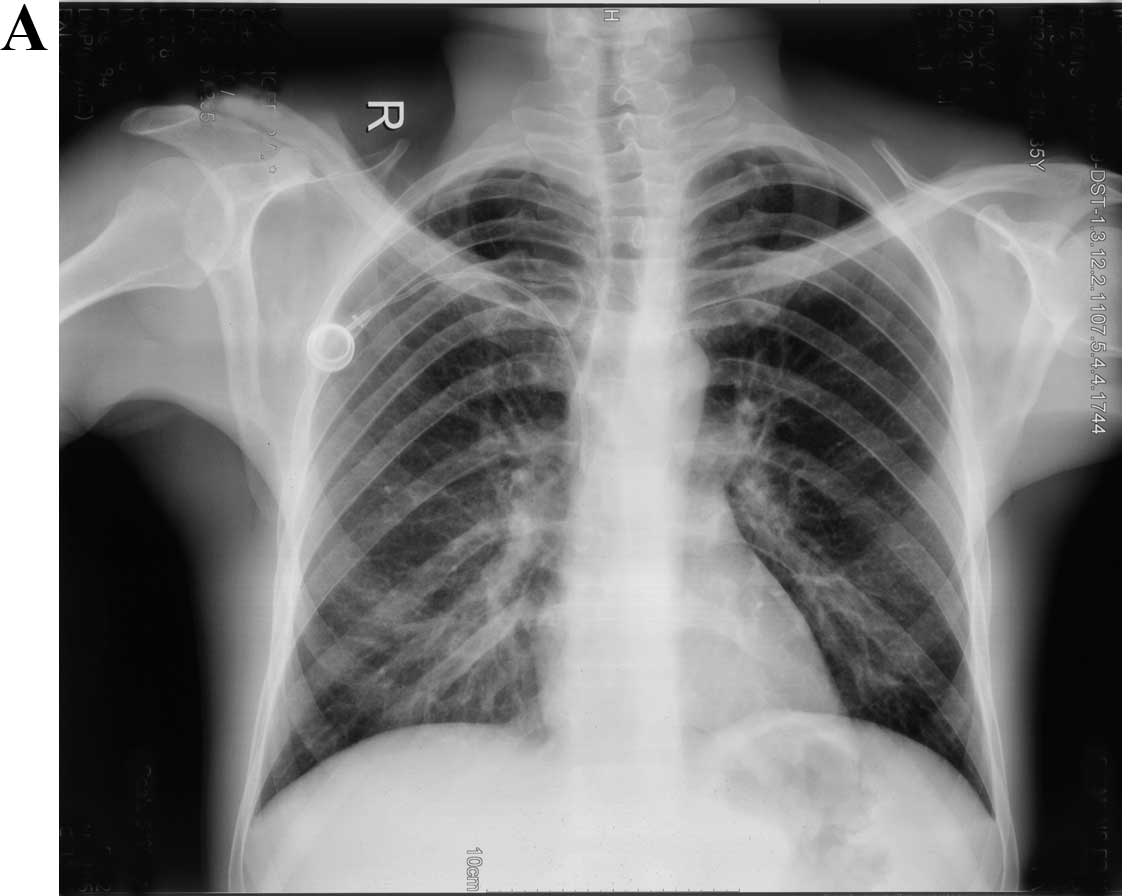
with 2.0 silk sutures. A digital lung graph was used at the
completion of the procedure to evaluate for pneumothorax, catheter
kinking and catheter tip position in accordance with the guidelines
(23). The port was used for
treatment 3 h after the procedure. Port catheters were flushed with
heparinized saline solution after each use and, thereafter, monthly
if not used.
Follow-up, analysis of results and
statistical analysis
Informed consent was obtained from each patient at
the time of the intervention, in accordance with the Helsinki
Declaration. All data were obtained from our files and the hospital
electronic database system after receiving the permission of the
Institutional Review Board (IRB). The follow-up term was from
placement until removal of the port, the last follow-up of the
patient or mortality date. Patients were censored due to mortality
and the last follow-up. Groups were divided by entry methods, which
were the jugular and subclavian access groups. Age, gender, access,
site of malignancy and coagulation parameters were the variables in
the multivariable analysis. The sites of primary malignancies were
divided into four regions, which were head-neck, breast-thorax,
abdominopelvic and extremity involving >1 region. These regions
were grouped together since they were individually small in
number.
Complications were defined according to the
guidelines of the Society of the Interventional Radiology Standards
of Practice Committee (5). Major
complications result in admission to a hospital for therapy (for
outpatient procedures), an unplanned increase in the level of care,
prolonged hospitalization, permanent adverse sequelae or mortality
(5). Complications were divided
into early (<30 days) and late (>30 days) as in the reporting
standards (23).
Event (failure) was defined as unplanned port
removal due to complications, so the groups were divided into
failure and success. Patency times of the ports via these routes
were compared using univariate Kaplan-Meier survival analysis and
the multivariable Cox regression test. P<0.05 and 95% confidence
interval (CI) in the analysis were considered to indicate a
statistically significant difference. Survival plots for catheter
patency were obtained from the statistical analysis. Statistical
analysis was performed by a mathematician (Ö.A.).
Results
Nine patients, of which 1 was in the subclavian
group, had abnormal bleeding parameters; these were corrected
before their ports were implanted. No major complications were
detected during the procedure. Two major complications occurred
following the procedure in the jugular group; a late complication
after 132 days in a 69-year-old male patient, who experienced
infection by skin necrosis, and an early complication on the second
day, which was bleeding due to prolonged INR (1.70) in a
29-year-old male patient to whom blood was administered before the
port was removed. Patient features and patency periods of
subclavian and jugular catheters are shown in Table I. Port catheters were placed into
jugular and subclavian veins in 248 (71.5%) and 99 patients
(28.5%), respectively. The mean number of catheter days was larger
in the subclavian than in the jugular access groups, 270.4 vs.
199.2 days. Ports were placed on the left side in 4 patients;
jugular in 2 and subclavian in the remaining 2 patients.
 | Table IDemographic features of patients. |
Table I
Demographic features of patients.
| Characteristics | Total | Jugular group | Subclavian group |
|---|
| Age (years)a | 53.8±13.9 | 53.0±14.0 | 55.7±13.7 |
| Genderb | | | |
| Female | 145 (41.8) | 110 (44.4) | 35 (35.4) |
| Male | 202 (58.2) | 138 (55.6) | 64 (64.6) |
| Access veinb | 347 (100) | 248 (71.5) | 99 (28.5) |
| Platelet
count/nla | 307.9±120.2 | 306.9±123.9 | 310.4±110.8 |
| Prothrombin time
(sec)a | 11.8±1.5 | 11.4±1.2 | 12.8±1.7 |
| International
normalized ratio (INR)a | 0.980±0.137 | 0.946±0.111 | 1.068±0.157 |
| Activated partial
thromboplastin time (sec)a | 28.2±4.5 | 28.1±4.5 | 28.3±4.7 |
| Localization of
primary malignanciesb | | | |
| Head-neck | 62 (17.9) | 45 (18.2) | 17 (17.2) |
| Breast-thorax | 29 (8.4) | 21 (8.5) | 8 (8.1) |
| Abdominopelvic | 237 (68.3) | 170 (68.8) | 67 (67.7) |
|
Extremity-otherc | 18 (5.2) | 11 (4.5) | 7 (7.1) |
| Mortalityb | | | |
| Positive | 20 (5.8) | 12 (4.8) | 8 (8.1) |
| Negative | 327 (94.2) | 236 (95.2) | 91 (91.9) |
| Patency periods
(days)d | 219.5±145.0
(1–550) | 199.2±122.5
(1–471) | 270.4±180.9
(1–550) |
Complications without port removal were observed in
4.9% of patients (17 patients). These included erythema and itching
in 2 patients, opening of sutures in 3 patients and bleeding in 12
patients. Ports were explanted due to the end of treatment in 5
patients and 20 mortalities were observed during follow-up, which
were censored. Port removal due to complications was observed in 15
patients, 9 in the jugular group and 6 in the subclavian group
(Table II).
 | Table IIComplications leading to port
removal. |
Table II
Complications leading to port
removal.
| | Jugular
| Subclavian
| | |
|---|
| Complication | n (%)a | n (%) | P-value | n (%) | P-value | Term (days) | Rate/100 catheter
days |
|---|
| Thrombosisb | 7 (2.0) | 5 (2.0) | 0.0101 | 2 (2.0) | 0.0074 | 375 | 0.0092 |
| Malposition | 4 (1.2) | 1 (0.4) | 0.0020 | 3 (3.0) | 0.0112 | 833 | 0.0053 |
| Flip-over | 1 (0.3) | 1 (0.4) | 0.0020 | 0 | 0 | 312 | 0.0013 |
| Hemorrhage | 1 (0.3) | 1 (0.4) | 0.0020 | 0 | 0 | 1 | 0.0013 |
| Infectionc | 2 (0.6) | 1 (0.4) | 0.0020 | 1 (1.0) | 0.0037 | 142 | 0.0026 |
| Skin
necrosisc | 1 (0.3) | 1 (0.4) | 0.0020 | 0 | 0 | 132 | 0.0013 |
| Totald | 16 (4.4) | 10 (4.0) | 0.0182 | 6 (6.1) | 0.0224 | 1,795 | 0.0197 |
Thrombosis occurred in 2 patients, malposition in 3
(Fig. 1) and infection in 1
patient when subclavian access was used, whereas there was
thrombosis in 5 patients (3 catheter thromboses, 1 jugular and the
other brachiocephalic vein thrombosis) and 1 case each of
malposition, bleeding, reservoir flip-over and skin necrosis with
wound infection in the jugular access group. Of the complications,
6 were early (4 in the jugular and 2 in the subclavian group) and 9
were late (5 in the jugular and 4 in the subclavian group).
The port removal rate due to complication per 100
port catheter days was 0.00182 in the jugular and 0.00224 in the
subclavian entry groups. Also, the port infection rate per 100 port
catheter days regarding the procedure was 0.0020 in the jugular vs.
0.0037 in the subclavian group.
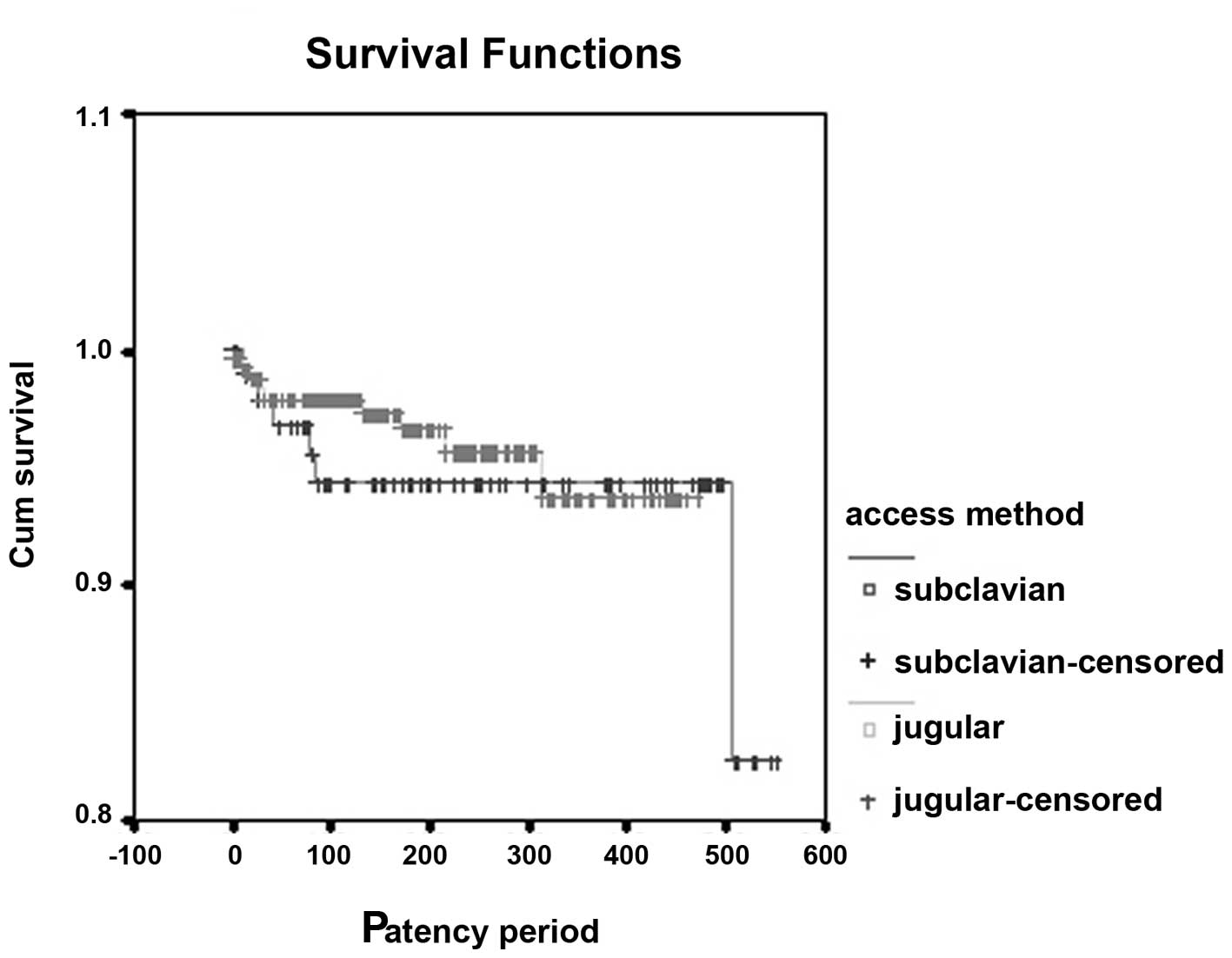
The graph in Fig. 2
shows the cumulative survival for catheter patency times of the
jugular and subclavian access groups in the Kaplan-Meier survival
analysis. Log-rank test did not detect any significant differences
between the groups (P=0.662).
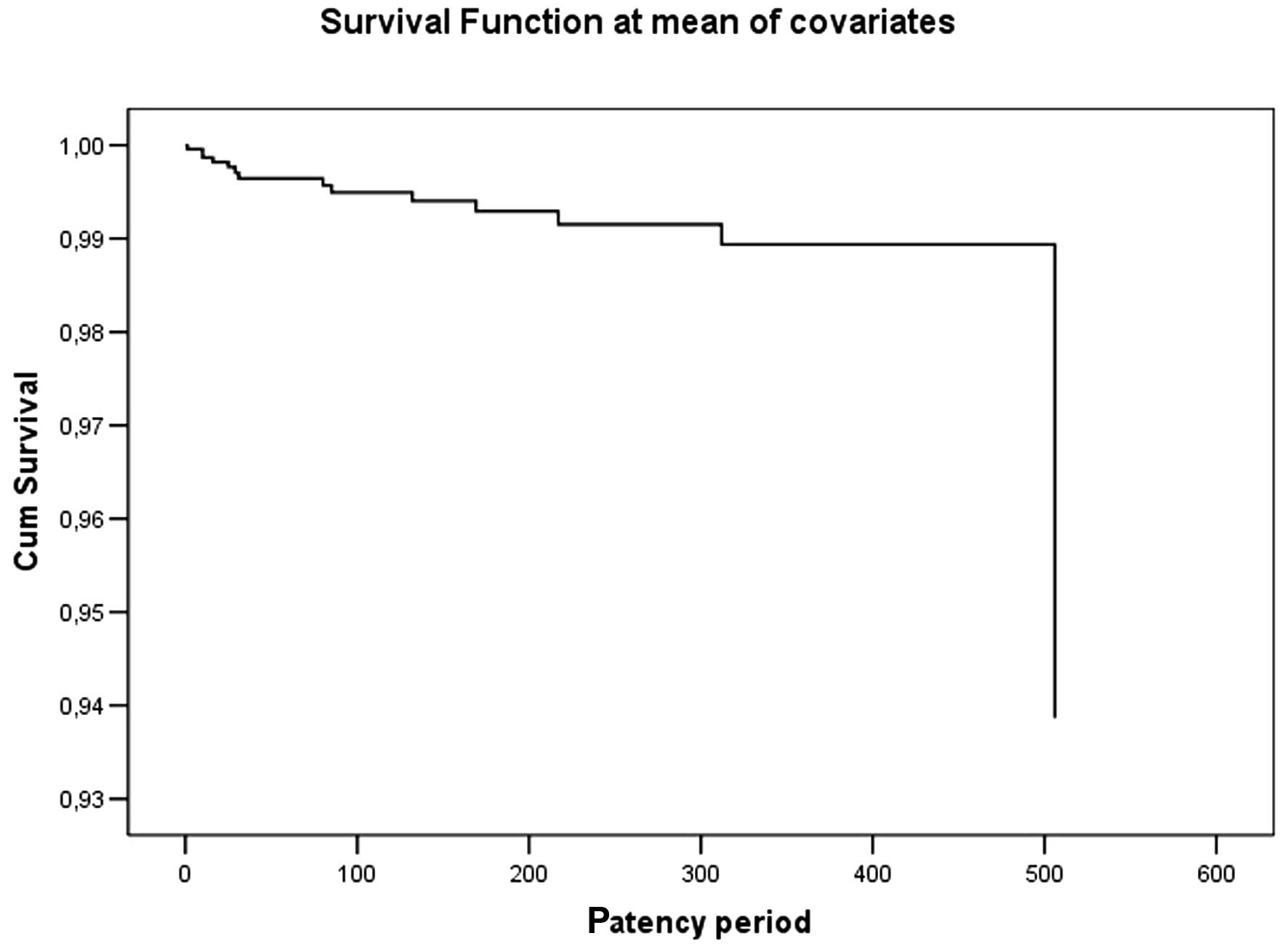
The graph in Fig. 3
shows the total cumulative survival for mean catheter patency time
by the multivariable Cox regression test. Age (P=0.252), gender
(P=0.775), access vein groups (P=0.369), site of primary malignancy
(P=0.607) and coagulation parameters, with the exception of
platelet count (P=0.043), were not significant variables in this
multivariable test. Coagulation parameters were platelet count
(P=0.043), prothrombin time (P=0.526), INR (P=0.289) and activated
partial thromboplastin time (P=0.087) in the multivariable test.
Their platelet counts (/nl) were 275.5±96.8 in the failure group
and 309.4±121.0 in the successful group.
Discussion
Image-guided insertion of subcutaneous chest ports
has a number of advantages compared with unguided insertion,
resulting in a higher success rate and fewer complications
(6). The major difference between
the techniques is the use of fluoroscopy and US (7,8). US
guidance reduces the number of mechanical complications, the number
of catheter placement failures and the time required for insertion.
However, US guidance use during subclavian venous catheterization
has had mixed results in clinical trials, probably due to
anatomical reasons (9).
Our complication rate was low due to the use of
imaging guidance, compared with the complication rates of the
landmark method, as reported in the literature. The use of
two-dimensional ultrasound (2D-US) guidance during internal jugular
catheterization has been demonstrated to lead to a reduction in the
rates of unsuccessful cannulation, carotid artery puncture and
hematoma formation when compared with the anatomical landmark
technique (10–13).
In the literature, the most common complications
after implantation were thrombosis, catheter dysfunction and
infections (2). Catheter-related
thrombosis is one of the most significant complications; its
frequency ranges from 0.67 to 5% (2). Our thrombosis rate was within this
range at 2% (0.0092 per 100 catheter days) and was slightly higher
in the jugular access group. However, it is debatable whether
Plumhans et al (3) observed
vein thrombosis in 3% of the subclavian group and in 1% of the
jugular group when thrombosis was reported in 1% of subclavian
ports (8) and in 1.7% of jugular
placements (6) in other
studies.
Female patients and patients with lung cancer also
had an elevated risk of developing a thrombosis (2). We detected more frequent thrombosis
in female patients (71.4% compared with 28.6% in male patients) but
this was not significant in multivariable analysis. Also, we were
unable to differentiate thrombosis detection between patients with
various malignancy localizations.
The risk of catheter-related infection was
reportedly lower for subclavian vein access than for jugular or
other access sites; however, no randomized trial has satisfactorily
compared infection rates for catheters placed in jugular,
subclavian and femoral sites (9,11,13–15).
We could neither find a difference in the infection rates (0.0020
in jugular vs. 0.0037 in subclavian per 100 catheter days) nor
incubate the responsible microorganism in cultures of the two port
site infections due to the antibiotic treatments administered.
Catheter-related complications also include necrosis
of the skin, malpositioning of the catheter tip, dislocation,
embolization, rupture and compression of the catheter, although
these are rare (2). Catheter tip
position is less susceptible to migration when placed through the
internal jugular vein (3).
Accordingly, we detected this in the present study, and our
catheter malposition rate per 100 catheter days was 0.0020 in the
jugular vs. 0.0112 in the subclavian route. Skin necrosis may be
observed in port placement (2,4).
Skin erosion has been reported in 0 to 1% of cases in the
literature (1,4), and our rate was 0.3% (0.0013 per 100
catheter days).
Subclavian venipuncture has been the most popular
route for transition and long-term central venous cannulation,
although perioperative complications occur in up to 12% of the
patients (11). Currently,
radiologists prefer the internal jugular vein since it is makes
catheterization easier (3,4,6,13).
The main advantages of jugular versus subclavian access are the
reduced periprocedural complications, better ultrasound control, no
pinch-off and lower migration and venous stenosis rate (3,10,16).
Also, Plumhans et al (3)
reported that their results demonstrated an approximately 50%
reduction of pain perception when the port-catheter was introduced
via the internal jugular vein. Conversely, Lorch et al
(1) preferred access through the
subclavian vein since the distance to the vena cava and right
atrium is short so no tunneling is necessary, thus shortening the
procedure time; it also requires no second incision at the neck,
which may be an advantage, especially in cachectic patients.
When possible, a lateral puncture of the subclavian
vein should be performed if subclavian access is chosen to avoid
pinch-off (1,14,15).
Fluoroscopic and/or ultrasound-guided access to the subclavian vein
also prevents catheter buckling or breakage due to ‘pinching’
between the first rib and the clavicle (17). The success rate of the technique
was higher in subclavian access in 55 patients for Brooks et
al (18) with US guidance.
Also, we did not observe visible catheter pinching, but some
pinch-off may have an effect on catheter thrombosis in subclavian
entry.
Previously, two studies (14,15)
revealed that port placement via the subclavian vein was as
successful as studies performed via the jugular vein reported in
the literature. Biffi et al (7) prospectively compared subclavian and
jugular port placements using the radiological and landmark methods
and found no differences in success. Furthermore, we did not find
any significant differences between catheter patency periods of
subclavian and jugular port placements, including complications,
using the same method.
Port inversion (turning over inside the port's
fibrous capsule) is an extremely rare complication (19,20).
Postulated risk factors for port inversion include loose or
redundant subcutaneous tissues and large pocket size (19). Thus, fixing the port chamber in the
subcutaneous tissue with sutures is not necessary if the port
pocket size is adequate (1). Also,
certain studies have, as we observed in the present study,
demonstrated that starting chemotherapy on the day of port catheter
implantation is safe, and does not increase the frequency of acute
or chronic complications (21).
This study has some restrictions. Among them, the
number of the patients was limited due to single center experience.
Also, the patients were not equally distributed between the two
access groups whereby the mean follow-up period of the subclavian
group, whose success would be expected at a lower rate, was longer
than that of the jugular group.
In our presented data, the periprocedural
complication rate was 0%. We would like to emphasize that skilled
interventional staff performed the procedure. Our experience has an
important role in the absence of periprocedural complication,
especially in subclavian entry. Thus, our choice of entry method
had a minimal effect on technique success.
We did not find any factor to be effective on
catheter patency times by multivariable analysis, with the
exception of platelet count. However, the difference in platelet
counts was approximately P=0.05. This may be due to the limitations
of our study. This may be examined in further studies.
The rate of symptomatic thrombosis in subclavian
access was higher in the study by Trerotola et al (22). However, US markedly decreased
failure and complication rates in subclavian entry in the study by
Brooks et al (18), which
was also true in our study. Data extracted from the current study
may increase the amount of evidence in the literature for the
positive effect of US in subclavian entry.
In conclusion, there was no significant difference
in patency times, including complications, between jugular vein and
subclavian vein access when using US. This should be considered
when selecting the access method.
References
|
1
|
Lorch H, Zwaan M, Kagel C and Weiss HD:
Central venous access ports placed by interventional radiologists:
experience with 125 consecutive patients. Cardiovasc Intervent
Radiol. 24:180–184. 2001. View Article : Google Scholar
|
|
2
|
Caers J, Fontaine C, Vinh-Hung V, et al:
Catheter tip position as a risk factor for thrombosis associated
with the use of subcutaneous infusion ports. Support Care Cancer.
13:325–331. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Plumhans C, Mahnken AH, Ocklenburg C, et
al: Jugular versus subclavian totally implantable access ports:
catheter position, complications and intrainterventional pain
perception. Eur J Radiol. 79:338–342. 2011. View Article : Google Scholar
|
|
4
|
Cil BE, Canyiğit M, Peynircioğlu B, et al:
Subcutaneous venous port implantation in adult patients: a single
center experience. Diagn Interv Radiol. 12:93–98. 2006.PubMed/NCBI
|
|
5
|
Lewis CA, Allen TE, Burke DR, et al:
Society of Interventional Radiology Standards of Practice
Committee: Quality improvement guidelines for central venous
access. J Vasc Interv Radiol. 14:S231–S235. 2003.
|
|
6
|
Yip D and Funaki B: Subcutaneous chest
ports via the internal jugular vein. A retrospective study of 117
oncology patients. Acta Radiol. 43:371–375. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Biffi R, Corrado F, de Braud F, et al:
Long-term, totally implantable central venous access ports
connected to a Groshong catheter for chemotherapy of solid tumours:
experience from 178 cases using a single type of device. Eur J
Cancer. 33:1190–1194. 1997. View Article : Google Scholar
|
|
8
|
Funaki B, Szymski GX, Hackworth CA, et al:
Radiologic placement of subcutaneous infusion chest ports for
long-term central venous access. AJR Am J Roentgenol.
169:1431–1434. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
McGee DC and Gould MK: Preventing
complications of central venous catheterization. N Engl J Med.
348:1123–1133. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hind D, Calvert N, McWilliams R, et al:
Ultrasonic locating devices for central venous cannulation:
meta-analysis. BMJ. 327:3612003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Biffi R, Orsi F, Pozzi S, et al: Best
choice of central venous insertion site for the prevention of
catheter-related complications in adult patients who need cancer
therapy: a randomized trial. Ann Oncol. 20:935–940. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Di Carlo I, Pulvirenti E, Mannino M and
Toro A: Increased use of percutaneous technique for totally
implantable venous access devices. Is it real progress? A 27-year
comprehensive review on early complications. Ann Surg Oncol.
17:1649–1656. 2010.PubMed/NCBI
|
|
13
|
Karakitsos D, Labropoulos N, De Groot E,
et al: Real-time ultrasound-guided catheterisation of the internal
jugular vein: a prospective comparison with the landmark technique
in critical care patients. Crit Care. 10:R1622006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Akahane A, Sone M, Ehara S, Kato K, Tanaka
R and Nakasato T: Subclavian vein versus arm vein for totally
implantable central venous port for patients with head and neck
cancer: a retrospective comparative analysis. Cardiovasc Intervent
Radiol. 34:1222–1229. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sakamoto N, Arai Y, Takeuchi Y, Takahashi
M, Tsurusaki M and Sugimura K: Ultrasound-guided radiological
placement of central venous port via the subclavian vein: a
retrospective analysis of 500 cases at a single institute.
Cardiovasc Intervent Radiol. 33:989–994. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Teichgräber UK, Kausche S, Nagel SN and
Gebauer B: Outcome analysis in 3,160 implantations of
radiologically guided placements of totally implantable central
venous port systems. Eur Radiol. 21:1224–1232. 2011.
|
|
17
|
Shetty PC, Mody MK, Kastan DJ, Sharma RP,
Burke MW and Venugopal C: Outcome of 350 implanted chest ports
placed by interventional radiologists. J Vasc Interv Radiol.
8:991–995. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Brooks AJ, Alfredson M, Pettigrew B and
Morris DL: Ultrasound-guided insertion of subclavian venous access
ports. Ann R Coll Surg Engl. 87:25–27. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
McNulty NJ, Perrich KD, Silas AM, Linville
RM and Forauer AR: Implantable subcutaneous venous access devices:
is port fixation necessary? A review of 534 cases. Cardiovasc
Intervent Radiol. 33:751–755. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
de Costa BR, Dickey K and Greenwood L: A
practical approach for repositioning flipped venous access ports. J
Vasc Interv Radiol. 11:213–214. 2000.PubMed/NCBI
|
|
21
|
Ozdemir NY, Abali H, Oksuzoğlu B,
Budakoglu B, Akmangit I and Zengin N: It appears to be safe to
start chemotherapy on the day of implantation through subcutaneous
venous port catheters in inpatient setting. Support Care Cancer.
17:399–403. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Trerotola SO, Kuhn-Fulton J, Johnson MS,
Shah H, Ambrosius WT and Kneebone PH: Tunneled infusion catheters:
increased incidence of symptomatic venous thrombosis after
subclavian versus internal jugular venous access. Radiology.
217:89–93. 2000. View Article : Google Scholar
|
|
23
|
Silberzweig JE, Sacks D, Khorsandi AS and
Bakal CW; Society of Interventional Radiology Technology Assessment
Committee: Reporting standards for central venous access. J Vasc
Interv Radiol. 14:S443–S452. 2003. View Article : Google Scholar : PubMed/NCBI
|