Introduction
Pulmonary arterial hypertension (PAH) is a
progressive disorder characterized by abnormally high blood
pressure in the pulmonary artery caused by functional and
structural alteration to the pulmonary vasculature resulting in an
increase in pulmonary vascular resistance (1). Numerous therapies have been proven
useful in decreasing pulmonary arterial pressure, but an effective
therapy for the long-term outcome in this disorder is lacking
(2–4). Monocrotaline (MCT), a pyrrolizidine
alkaloid extracted from the seeds of Crotalaria spectabilis,
used in the model of MCT-induced pulmonary hypertension is known to
represent similar pathology to that of primary PAH (5).
Bone marrow mesenchymal cells (BMSCs) are
multipotent progenitor cells derived from fetal bone marrow, which
have the ability to differentiate into bone, cartilage, muscle,
bone marrow stroma, endothelial cells, vascular smooth muscle cells
(6,7) and other connective tissues. Studies
also suggest that BMSCs secrete a variety of growth factors, such
as vascular endothelial growth factor (VEGF) (8,9).
Recently, BMSC transplantation has become a potential therapy for
PAH.
Materials and methods
Animals
A total of 30 healthy adult Sprague-Dawley (SD) rats
weighing 200–250 g were purchased from The Animal Experimental
Center of Shandong University, China. The study protocol was
reviewed and approved by the Institutional Animal Care and Use
Committee, The Second Hospital of Shandong University, and the
experiments were conducted according to the Guidelines of the
American Physiological Society.
Isolation, culture, immunophenotype
analysis and labeling of BMSCs
Bone marrow cells were isolated by flushing the
cavity of femurs and tibias, and transferred to a tissue culture
dish 90 mm in diameter (10,11).
To separate BMSCs and other cells, the Ficoll (1.077) density
gradient centrifugation method was used. The white layer composed
of mononuclear cells from the upper layer and interface was
carefully collected and washed three times. Flow cytometric
immunophenotyping was performed using methods described previously
(12,13). Briefly, 5×105 cells were
suspended with trypsin and were washed twice in phosphate-buffered
saline (PBS). Cells were stained with antibodies against CD44,
CD29, CD34 and CD90 (BD Biosciences, Franklin Lakes, NJ, USA) for
30 min at 4°C. The percentage of positive cells was determined by
fluorescent activated cell sorting (FACS) analysis. Prior to
implantation, the cells were labeled with the cross-linkable
membrane dye CM-DiI (2 μg/ml, Invitrogen Corp., Carlsbad, CA, USA)
(14). The male SD rats were
randomly assigned to 3 groups (n=10 in each group) as follows:
control group, animals that received a sublingual vein injection of
0.9% saline instead of BMSCs; PAH group, animals that received a
subcutaneous injection of 50 mg/kg MCT; BMSC group, animals that
received 5×105 labeled BMSC implantation one week after
MCT injection.
BMSC transplantation
One week after MCT injection, the rats were
anesthetized by subcutaneous injection of pentobarbital,
5×105 CM-DiI labeled BMSCs were resuspended in 100 μl
saline and administered via the sublingual vein.
Establishment and evaluation of the
pulmonary arterial hypertension model
MCT was prepared as described (2) and was dissolved in 1 N HCl,
neutralized to pH 7.4 with 0.5 N NaOH, and diluted with saline
before injection. Male SD rats (n=10) were randomly assigned to 2
groups as follows: PH group, animals that received a subcutaneous
injection of 50 mg/kg MCT; control group, animals that received a
subcutaneous injection of 0.9% saline instead of MCT. One week
after MCT injection, the rats were anesthetized and fitted with a
3F-Millar Mikro-Tip catheter via the right jugular vein into the
right ventricle to obtain base line measurements of hemodynamics,
including right ventricular systolic pressure (RVSP), mean right
ventricular pressure (MRVP) and mean pulmonary arterial pressure
(MPAP). The rats were sacrificed after hemodynamic measurements,
and the lung and heart were quickly harvested and fixed in
situ via the trachea cannula with buffered 4% formaldehyde, and
embedded in paraffin. The sections were cut into 4–5 μm slices and
were stained with streptavidin peroxidase and hematoxylin and eosin
(H&E). The structural changes in the pulmonary vascular wall
were observed by immunofluorescence microscopy and wall thickness
(MT), blood vessel diameter (ED), pulmonary artery lumen area (VA)
and vascular area (TAA) were measured to calculate MT% (=MT/ED) and
VA% (=VA/TAA). The ratio of right ventricular weight to body weight
(RV/BW) was calculated to measure right ventricular hypertrophy.
Results of the hemodynamic parameters, right ventricular
hypertrophy, and pulmonary arterial pathological changes were used
to evaluate whether the model of pulmonary arterial hypertension
was successfully established.
Immunological and immunohistochemical
analysis
Two weeks after BMSC transplantation the rats were
anesthetized and the lungs were inflated with OCT compound and
quickly frozen in liquid nitrogen and stored at −80°C. Sections
were cut into 4 μm slices and fixed in acetone for 10 min at −20°C.
The survival of BMSCs was demonstrated by observing the presence of
DiI-labeled cells. Immunofluorescence was then performed with goat
anti-mouse monoclonal surfactant associated protein C (SP-C, 1:100)
IgG antibody, rabbit anti-human von Willebrand Factor (vWF, 1:100)
antibody and VEGF (1:100) antibody. FITC-conjugated antiserum was
used as a secondary antibody.
Results
The analysis of MCT-induced hemodynamics
and RV weight
One week after MCT injection, RVSP, MRVP and MPAP
were significantly elevated in the PAH group compared with the
control (P<0.05), and the ratio of RV/BW was significantly
higher in the PAH group compared with the control group (0.49±0.03
vs. 0.57±0.06, P<0.05). These results indicated that MCT led to
severe right ventricular hypertrophy and the PAH model was
successfully established (Table
I).
 | Table IEffect of MCT on hemodynamics and
right ventricular weight one week after administration. |
Table I
Effect of MCT on hemodynamics and
right ventricular weight one week after administration.
| Variable | Control | PAH |
|---|
| RVSP (mmHg) | 34.38±1.86 | 50.33±1.39b |
| MPAP (mmHg) | 20.18±2.19 | 40.28±3.27b |
| MRVP (mmHg) | 19.43±3.17 | 42.64±4.25b |
| RV/BW | 0.49±0.03 | 0.57±0.06b |
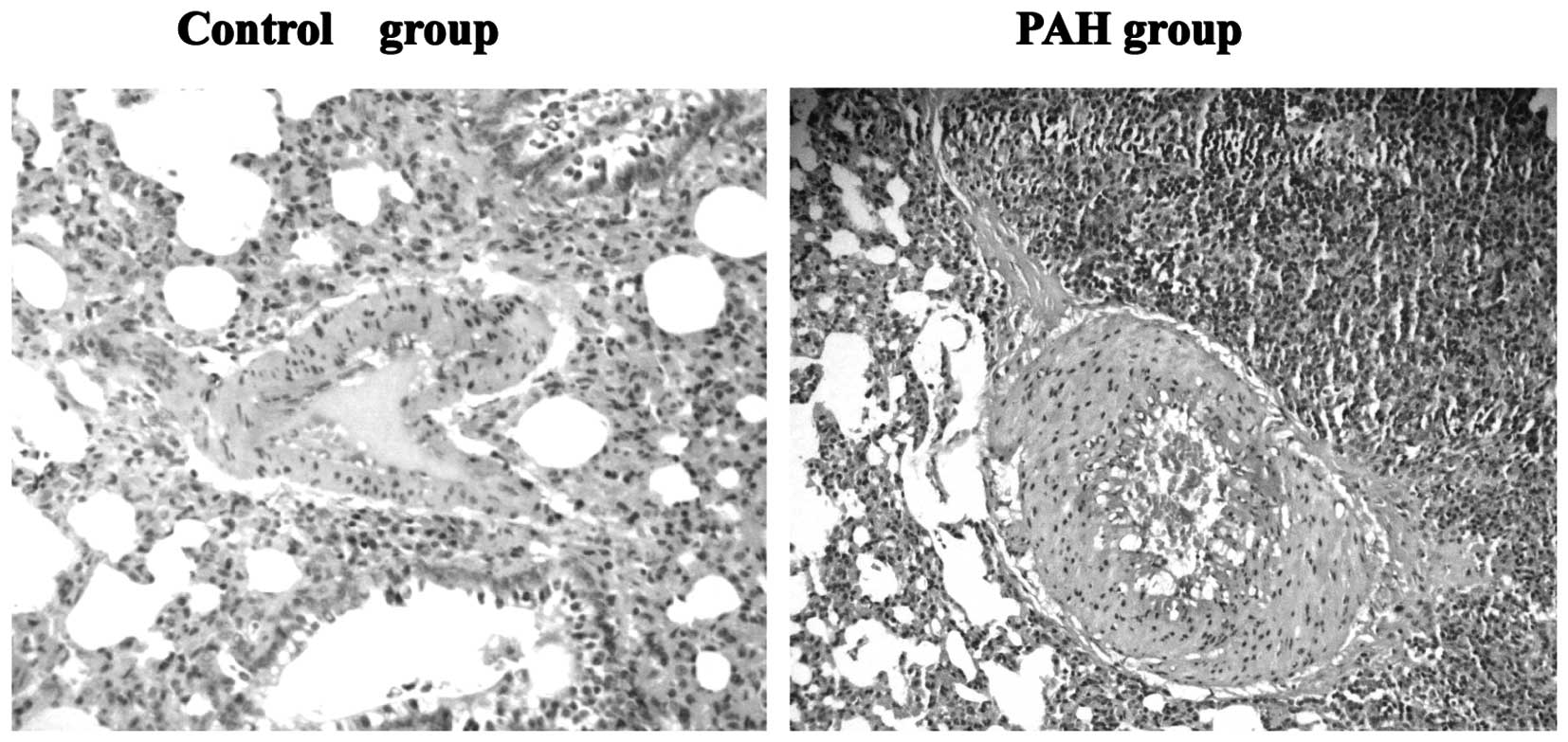
Analysis of MCT-induced structural
changes in the pulmonary artery wall
H&E staining demonstrated significant intima
thickening and luminal stenosis in the PAH group compared with the
control group. The MT% of muscular arteries was significantly
increased and the VA% was significantly decreased in the PAH group
compared with control group (P<0.01, Table II, Fig. 1).
 | Table IIEffect of MCT on the pulmonary artery
wall one week after administration. |
Table II
Effect of MCT on the pulmonary artery
wall one week after administration.
| Variable | Control | PAH |
|---|
| MT% | 13.05±1.33 | 38.27±4.55b |
| VA% | 44.09±4.17 | 33.39±6.63b |
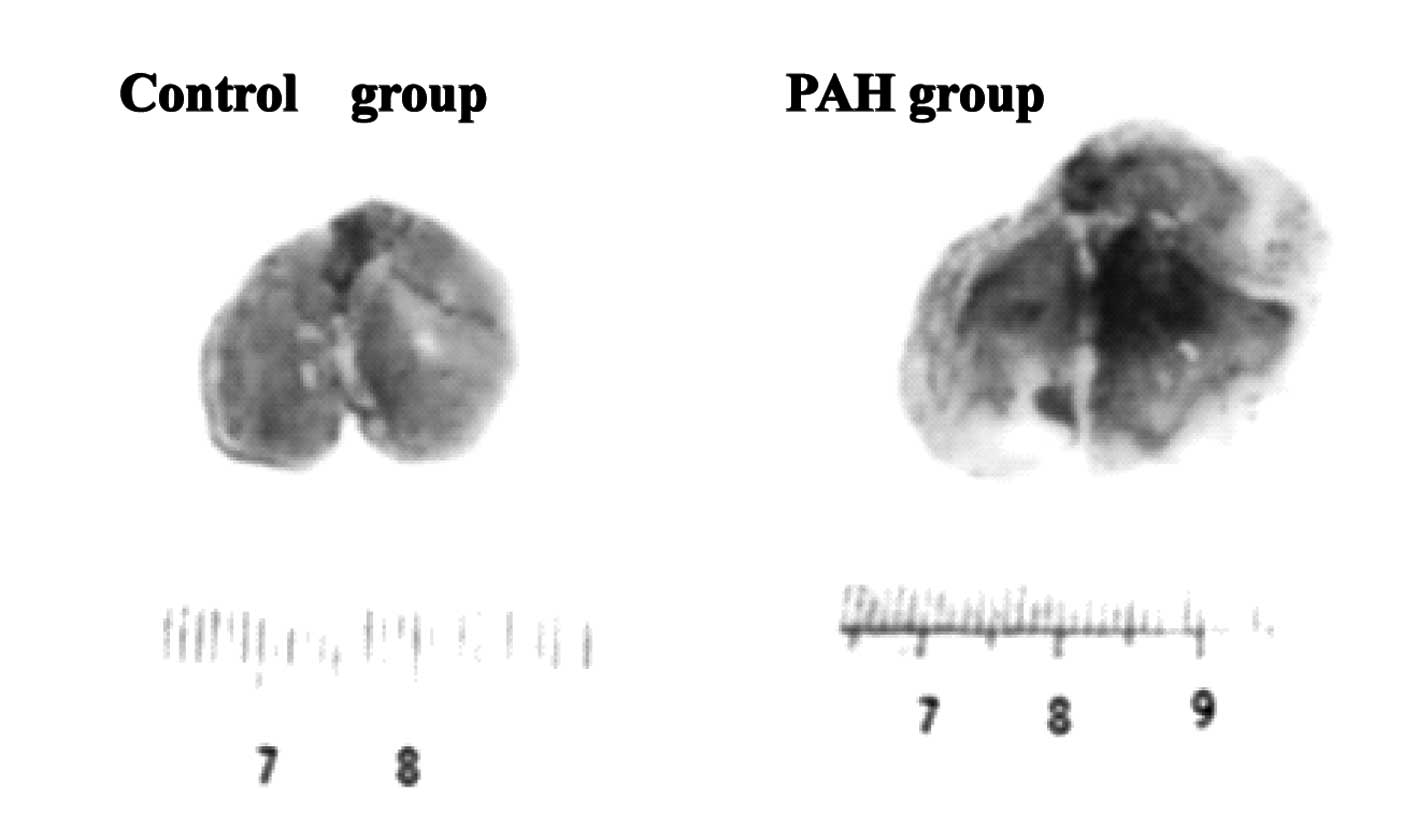
MCT-induced lung morphological
observation
Two weeks after operation, gross observation showed
that enlarged volume, purple color, uneven surface, poor elasticity
and partial visible blood stasis were present in the PAH group
compared with the normal control group (Fig. 2).
Effect of BMSCs on hemodynamics and RV
impairment
Two weeks after BMSC administration, RVSP, MRVP and
MPAP were significantly lower in the BMSC group compared with the
PAH group, the ratio of RV/BW was significantly lower in the BMSC
group compared with the PAH group (P<0.05, Table III).
 | Table IIIEffect of BMSCs on the hemodynamics
and right ventricular weight 2 weeks after implantation. |
Table III
Effect of BMSCs on the hemodynamics
and right ventricular weight 2 weeks after implantation.
| Variable | Control | PAH | BMSCs |
|---|
| RVSP (mmHg) | 35.17±1.86 | 56.84±1.54b | 43.83±2.13e |
| MPAP (mmHg) | 20.36±2.13 | 41.37±2.24b | 26.82±3.42e |
| MRVP (mmHg) | 19.74±5.23 | 41.68±6.17b | 28.34±1.98e |
| RV/BW (%) | 0.472±0.035 | 0.613±0.072a | 0.547±0.041d |
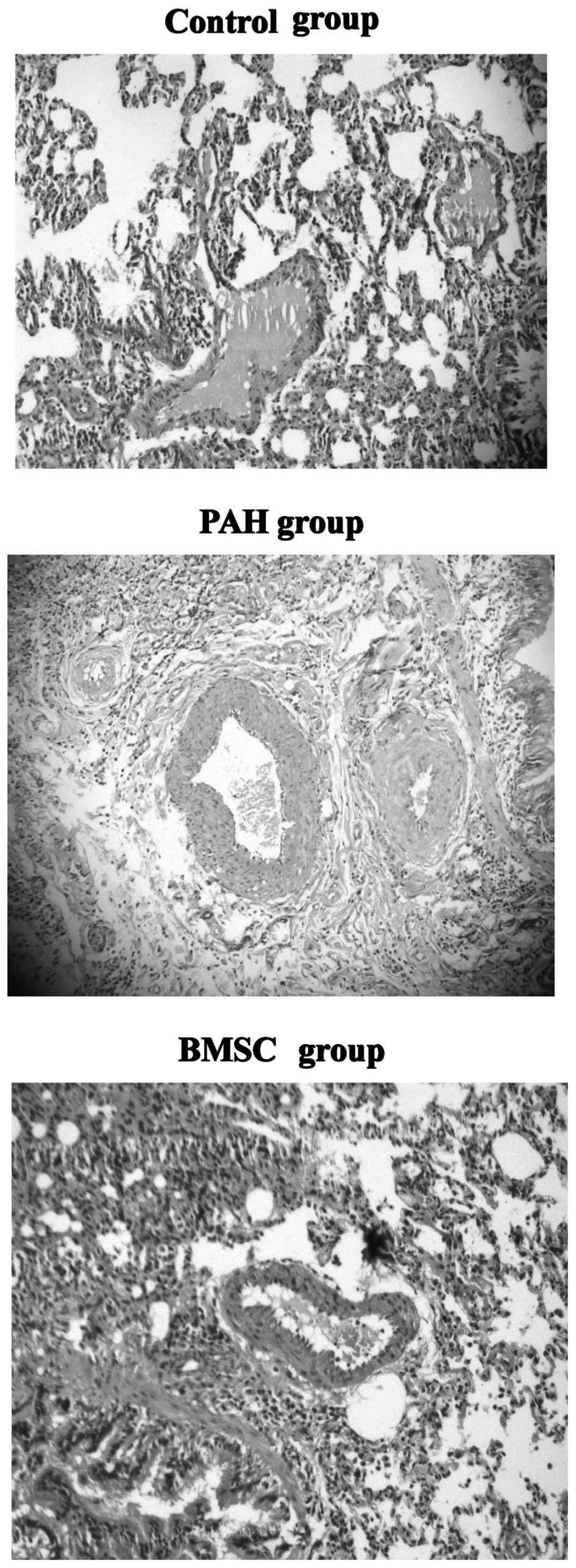
Effect of BMSCs on pulmonary artery
wall
H&E staining demonstrated that intima thickening
and luminal stenosis were significantly decreased in the BMSC group
compared with the PAH group. The MT% and VA% of muscular arteries
was significantly improved in the BMSC group compared with the PAH
group (P<0.05, Table IV,
Fig. 3).
 | Table IVEffect of BMSCs on the pulmonary
artery wall 2 weeks after implantation. |
Table IV
Effect of BMSCs on the pulmonary
artery wall 2 weeks after implantation.
| Variable | Control | PAH | BMSCs |
|---|
| MT% | 12.08±1.30 | 45.21±4.37b | 20.83±5.49d |
| VA% | 42.31±4.39 | 20.36±6.81b | 38.27±3.48d |
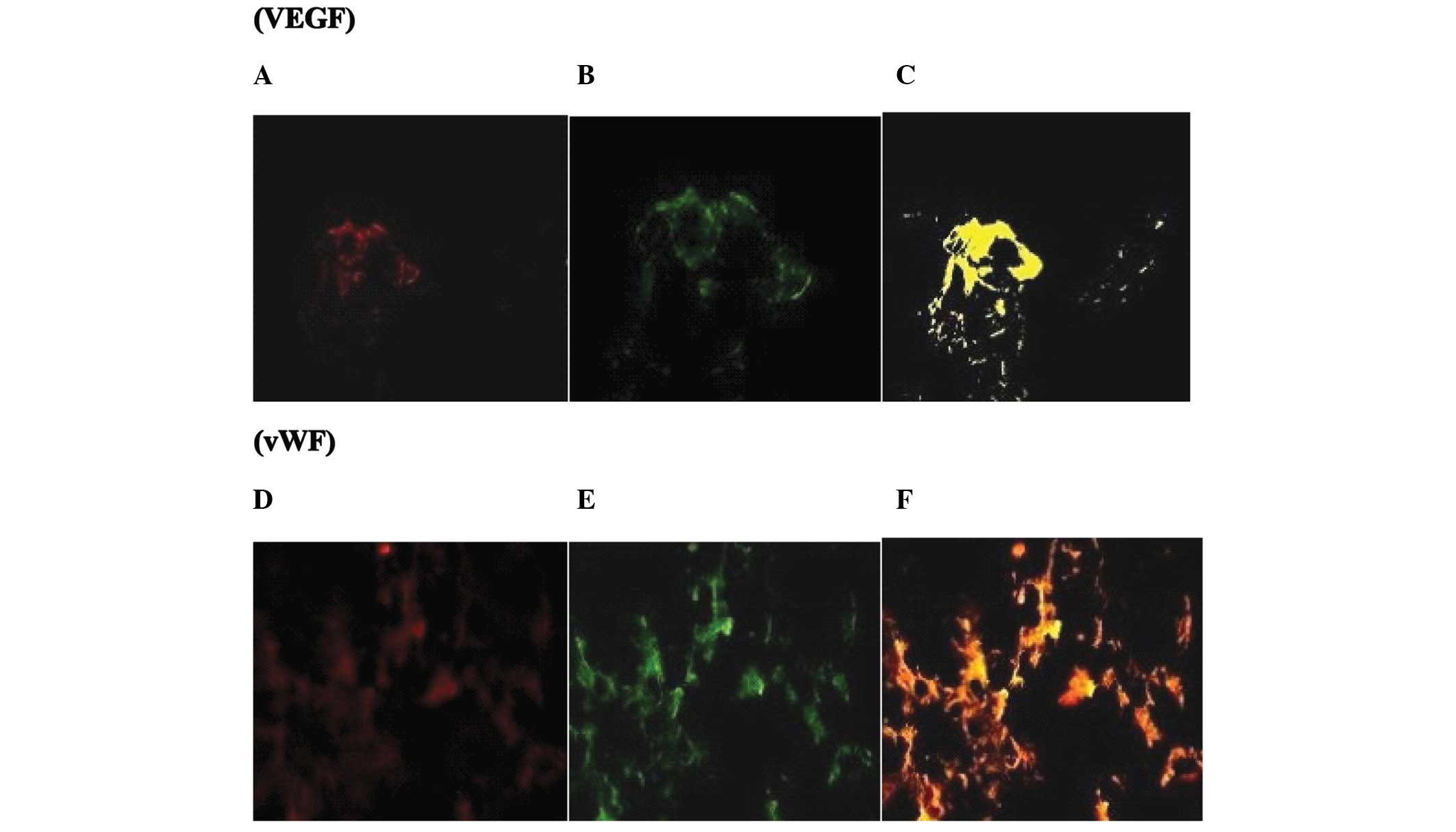
Identification of the transplanted
BMSCs
In numerous regions, the red fluorescence-positive
cells were observed coincident with the green fluorescence spots of
VEGF and vWF antibody but not SP-C antibody, which suggested that
the intravenous implantation of BMSCs resulted in their
differentiation into vascular endothelial cells in vivo
although they did not survive as lung cells. There was no evidence
of red or green fluorescence in the control and PAH groups
(Fig. 4).
Discussion
PAH is a progressive disorder characterized by the
progressive increase in pulmonary arterial pressure and resistance,
eventually leading to right heart failure and mortality in patients
with refractory disease. Although in the past ten years, the
treatment of PAH has achieved apparent progress, the prognosis
remains poor. Intravenous administration of drugs (e.g.
prostacyclin, endothelin receptor antagonists) or nitric oxide
inhalation may temporarily reduce PAH, but these effects are not
lasting. In recent years, regeneration and gene therapy has become
the research focus worldwide, however, stem cell research is still
in its initial stages and so far there is no uniform method to
treat PAH. Therefore, for further experimental studies,
investigating reasonable and safe methods of treatment for PAH has
become urgent.
BMSCs, multipotent progenitor cells derived from
fetal bone marrow, could differentiate into distinctive end-stage
cell types, including bone, cartilage, muscle, endothelial cells,
vascular smooth muscle cells and other connective tissues. Studies
have also demonstrated that BMSCs have the pluripotent ability to
become endothelial progenitor cells and other cell lineages
(15,16). BMSCs are able to secrete a variety
of growth factors to promote angiogenesis, such as VEGF.
Transplantation of endothelial progenitor cells
(EPCs) into the MCT-injured lung could repair the damage, but the
treatment effect is not ideal. The studies on BMSC transplantation
for pulmonary hypertension are limited. In our previous research
(17), intravenous implantation of
BMSCs improved the progression of RV impairment caused by
MCT-induced PAH. The aim of this study was to further explore the
effect of BMSCs on lung and heart impairment. First, we
demonstrated that 2 weeks after sublingual vein administration of
BMSCs to PAH rats, the pulmonary arterial pressure was
significantly lower in the BMSC group compared with the nontreated
PAH group. RVSP, MRVP and MPAP were significantly lower in the BMSC
group compared with the PAH group, the ratio of RV/BW was
significantly lower in the BMSC group compared with the PAH group.
Notably, in the case of the present study, we found that the
structural changes in the pulmonary vascular wall, such as VA and
TAA, were significantly improved. Although the underlying
mechanisms are complicated and not yet determined, several factors
are expected to contribute, including the role of stem cell
differentiation and para-secretion effects (3,18–23).
Our experiments also demonstrated that the red
fluorescence-positive cells were observed coincident with the green
fluorescence spots of VEGF and vWF antibody but not SP-C antibody
in numerous regions. These results suggest that the intravenous
implantation of BMSCs results in the ability of these cells to
differentiate into vascular endothelial cells in vivo but
not lung cells. Therefore, transplantation of BMSCs by homing to
the lung and transforming into vascular endothelial cells may
create a wide range of collateral circulation, increase the total
area of the pulmonary vascular bed, improve pulmonary blood supply
and effectively reduce the pulmonary hypertension.
In conclusion, our results showed that intravenous
implantation of BMSCs may improve not only the cardiac function and
hemodynamics, but also the pulmonary vascular wall damage in PAH
caused by MCT. Therefore, this study provides conslusive
information for the use of this new method in the treatment of
pulmonary arterial hypertension.
Acknowledgements
This work was supported by a grant
from Shandong Province Medical Health Science and Technology
Development Programs (2011HZ032) and Independent Innovation
Foundation of Shandong University, IIFSDU (grant number
2010TS051).
References
|
1
|
Morrell NW, Adnot S, Archer SL, Dupuis J,
Jones PL, MacLean MR, McMurtry IF, Stenmark KR, Thistlethwaite PA,
Weissmann N, Yuan JX and Weir EK: Cellular and molecular basis of
pulmonary arterial hypertension. J Am Coll Cardiol. 54:S20–S31.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kanki-Horimoto S, Horimoto H, Mieno S,
Kishida K, Watanabe F, Furuya E and Katsumata T: Implantation of
mesenchymal stem cells overexpressing endothelial nitric oxide
synthases improves right ventricular impairments caused by
pulmonary hypertension. Circulation. 114:I181–I185. 2006.
|
|
3
|
Baber SR, Deng W, Master RG, Bunnell BA,
Taylor BK, Murthy SN, Hyman AL and Kadowitz PJ: Intratracheal
mesenchymal stem cell administration attenuates
monocrotaline-induced pulmonary hypertension and endothelial
dysfunction. Am J Physiol Heart Circ Physiol. 292:H1120–H1128.
2007. View Article : Google Scholar
|
|
4
|
Patel KM, Crisostomo P, Lahm T, Markel T,
Herring C, Wang M, Meldrum KK, Lillemoe KD and Meldrum DR:
Mesenchymal stem cells attenuate hypoxic pulmonary vasoconstriction
by a paracrine mechanism. J Surg Res. 143:281–285. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Miura M, Hirose M, Endoh H, Wakayama Y,
Sugai Y, Nakano M, Fukuda K, Shindoh C, Shirato K and Shimokawa H:
Acceleration of Ca2+ waves in monocrotaline-induced
right ventricular hypertrophy in the rat. Circ J. 75:1343–1349.
2011.
|
|
6
|
Wang CH, Cherng WJ, Yang NI, Kuo LT, Hsu
CM, Yeh HI, Lan YJ, Yeh CH and Stanford WL: Late-outgrowth
endothelial cells attenuate intimal hyperplasia contributed by
mesenchymal stem cells after vascular injury. Arterioscler Thromb
Vasc Biol. 28:54–60. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Westerweel PE and Verhaar MC: Directing
myogenic mesenchymal stem cell differentiation. Circ Res.
103:560–561. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gehrke I, Gandhirajan RK, Poll-Wolbeck SJ,
Hallek M and Kreuzer KA: Bone marrow stromal cell-derived vascular
endothelial growth factor (VEGF) rather than chronic lymphocytic
leukemia (CLL) cell-derived VEGF is essential for the apoptotic
resistance of cultured CLL cells. Mol Med. 17:619–627. 2011.
View Article : Google Scholar
|
|
9
|
Crosswhite P and Sun Z: Nitric oxide,
oxidative stress and inflammation in pulmonary arterial
hypertension. J Hypertens. 28:201–212. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gao J, Dennis JE, Muzic RF, Lundberg M and
Caplan AI: The dynamic in vivo distribution of bone marrow-derived
mesenchymal stem cells after infusion. Cells Tissues Organs.
169:12–20. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nagaya N, Fujii T, Iwase T, Ohgushi H,
Itoh T, Uematsu M, Yamagishi M, Mori H, Kangawa K and Kitamura S:
Intravenous administration of mesenchymal stem cells improves
cardiac function in rats with acute myocardial infarction through
angiogenesis and myogenesis. Am J Physiol Heart Circ Physiol.
287:H2670–H2676. 2004. View Article : Google Scholar
|
|
12
|
Choudhary M, Zhang X, Stojkovic P, Hyslop
L, Anyfantis G, Herbert M, Murdoch AP, Stojkovic M and Lako M:
Putative role of hyaluronan and its related genes, HAS2 and RHAMM,
in human early preimplantation embryogenesis and embryonic stem
cell characterization. Stem Cells. 25:3045–3057. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Luan Y, Liu XC, Zhang GW, Shi RF, Zhao XB,
Zhao CH, Liu TJ, Lü F, Yang Q and He GW: Mid-term effect of stem
cells combined with transmyocardial degradable stent on swine model
of acute myocardial infarction. Coron Artery Dis. 21:233–243. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang Y, Liu XC, Zhang GW, Zhao J, Zhang
JM, Shi RF, Huang YZ, Zhao CH, Liu TJ, Song CX, Lü F, Yang Q and He
GW: A new transmyocardial degradable stent combined with growth
factor, heparin, and stem cells in acute myocardial infarction.
Cardiovasc Res. 84:461–469. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jiang Y, Jahagirdar BN, Reinhardt RL,
Schwartz RE, Keene CD, Ortiz-Gonzalez XR, Reyes M, Lenvik T, Lund
T, Blackstad M, Du J, Aldrich S, Lisberg A, Low WC, Largaespada DA
and Verfaillie CM: Pluripotency of mesenchymal stem cells derived
from adult marrow. Nature. 418:41–49. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Oswald J, Boxberger S, Jørgensen B,
Feldmann S, Ehninger G, Bornhäuser M and Werner C: Mesenchymal stem
cells can be differentiated into endothelial cells in vitro. Stem
Cells. 22:377–384. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Luan Y, Zhang ZH, Wei DE, Zhao JJ, Kong F,
Cheng GH and Wang YB: Implantation of mesenchymal stem cells
improves right ventricular impairments caused by experimental
pulmonary hypertension. Am J Med Sci. 343:402–406. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Frid MG, Brunetti JA, Burke DL, Carpenter
TC, Davie NJ, Reeves JT, Roedersheimer MT, van Rooijen N and
Stenmark KR: Hypoxia-induced pulmonary vascular remodeling requires
recruitment of circulating mesenchymal precursors of a
monocyte/macrophage lineage. Am J Pathol. 168:659–669. 2006.
View Article : Google Scholar
|
|
19
|
Rochefort GY, Vaudin P, Bonnet N, Pages
JC, Domenech J, Charbord P and Eder V: Influence of hypoxia on the
domiciliation of mesenchymal stem cells after infusion into rats:
possibilities of targeting pulmonary artery remodeling via cells
therapies? Respir Res. 6:1252005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tang J, Xie Q, Pan G, Wang J and Wang M:
Mesenchymal stem cells participate in angiogenesis and improve
heart function in rat model of myocardial ischemia with
reperfusion. Eur J Cardiothorac Surg. 30:353–361. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Jiang S, Kh Haider H, Ahmed RP, Idris NM,
Salim A and Ashraf M: Transcriptional profiling of young and old
mesenchymal stem cells in response to oxygen deprivation and
reparability of the infarcted myocardium. J Mol Cell Cardiol.
44:582–596. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Al-Khaldi A, Al-Sabti H, Galipeau J and
Lachapelle K: Therapeutic angiogenesis using autologous bone marrow
stromal cells: improved blood flow in a chronic limb ischemia
model. Ann Thorac Surg. 75:204–209. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Guo Y, He J, Wu J, Yang L, Dai S, Tan X
and Liang L: Locally overexpressing hepatocyte growth factor
prevents post-ischemic heart failure by inhibition of apoptosis via
calcineurin-mediated pathway and angiogenesis. Arch Med Res.
39:179–188. 2008. View Article : Google Scholar
|