Introduction
Cerebral venous thrombosis (CVT) is a rare type of
cerebrovascular disease, which accounts for approximately 0.5–2% of
all stroke cases (1,2). CVT has varied and atypical clinical
manifestations, as a result of which misdiagnosis and missed
diagnosis often occur (3). The
majority of CVT cases are accompanied by intracranial hypertension
(4). CVT principally manifested as
headaches, focal neurological deficits, seizure disorders and
impaired consciousness; other symptoms include papilledema,
abnormal vision, nausea, emesis, cranial nerve lesion and coma
(5). These varied and atypical
clinical manifestations often pose difficulty in early diagnosis of
CVT, as a consequence of which necessary treatment is delayed.
Early treatment can greatly improve the prognosis of CVT, save
patients’ lives, improve their life quality, and reduce family and
social burdens. In recent years, with the development and wide
adoption of neuroimaging, the diagnosis rate of CVT has markedly
increased. Some CVT patients can be diagnosed using computed
tomography (CT), most can be confirmed by magnetic resonance
imaging (MRI) combined with magnetic resonance venography (MRV),
and only a small number require diagosis by further digital
subtraction angiography (DSA).
The current study was based on case analyses of 18
CVT patients who received treatment between September 2009 and
August 2011, as well as the experiences of their treatments.
Patients and methods
General data
A total of 18 CVT patients including 5 males and 13
females were involved. Their ages ranged from 22 to 65 years with a
meane age of 39. The time from disease onset to admission to
hospital ranged from 1 day to 45 days with an average of 7 days.
The causes included late trimester of pregnancy (one case),
puerperium (four cases), upper respiratory tract infection (three
cases), brain trauma (one case), abnormal immune system (two
cases), oral administration of contraceptives (two cases), and
uncertain causes (five cases).
The current study was conducted in accordance with
the Declaration of Helsinki and approved by the Ethics Committee of
Yantai Yuhuangding Hospital. Written informed consent was obtained
from each participant.
Clinical manifestations
Headaches were found in 15 patients, which was the
primary symptom among the recruited participants. Other symptoms
included papilledema in 12 patients, abnormal eye movements and
diplopia in one, emotional disturbance in one, unconsciousness in
five, seizure disorders in six, language disorders in two, limb
paralysis in six, and positive meningeal irritation signs in
six.
Auxiliary examinations
CT was performed for 15 patients: five patients were
normal; one was suspected of an ‘Δ’, three were observed with lobar
hemorrhage, one with embolic infarction in the left parietal lobe,
one with hypodensity in the right frontal and parietal lobes, one
with a large area of mixed densities in the left frontal lobe, two
with hypodensity in the bilateral thalamic basal nuclei, and one
with subarachnoid hemorrhage. MRI and MRV were performed for 16
patients. No abnormality was observed in one patient, superior
sagittal sinus thrombosis was observed in seven, inferior
longitudinal and straight sinus thrombosis in three, bilateral
transverse and sigmoid sinus thrombosis in two, and great cerebral
venous thrombosis in three. MRI alone was performed for one
patient: the patient presented with a large area of bleeding in the
left temporal lobe, a median line malposition, a brain herniation,
and absence of the flow void signals in the right jugular vein and
the left transverse and sigmoid sinuses (enhancement scanning did
not show enhanced images in these veins). One patient who was
observed as normal according to MRI + MRV also received DSA and the
result disclosed partial visualization of the cerebral venous and
venous sinuses and cerebral circulation time prolonging by 13 sec
[less than 9 sec is the normal value, and longer circulation time
indicates a poorer prognosis (6)].
DSA for the patient with subarachnoid hemorrhage confirmed
bilateral transverse and sigmoid sinus thrombosis. Lumbar puncture
for cerebrospinal fluid (CSF) examination was performed for 14
patients: three had CSF pressures between 200 and 250
mmH2O (1 mmH2O = 0.098 kPa), six had CSF
pressures between 250 and 350 mmH2O, and five had CSF
pressures of >350 mmH2O, one of whom had uniform
bloody CSF; eight had basically normal CSF cell counts as well as
normal protein concentrations; four had protein concentrations
between 0.9 and 1.2 g/l; and two had abnormal white blood cell
counts (15×106/l and 34×106/l), which were
mainly represented by monocytes, and protein concentrations of 0.68
g/l and 0.87g/l but with normal glucose and chloride
concentrations.
Treatment and turnover
After final diagnosis, each patient was given a
combined modality therapy such as anticoagulation, thrombolysis,
platelet inhibition, intracranial pressure reduction through
cerebral edema remission, and complication prevention, depending on
his/her condition. Patients with seizure disorders were
administered anti-epileptic treatment and those with concurrent
infections were administered anti-infective therapy. A total of 14
patients exhibited stable pathogenetic conditions and were
discharged from the hospital, with eight completely recovered, two
with varying degrees of carryover limb paralysis (one still with
language disorders), one with diplopia, two with slow response, and
one in a vegetative state. After the discharge, 11 patients were on
oral warfarin based on a moderate international normalized ratio
(INR) between 2.0 and 3.0. One patient was administered bayaspirin
(Bayer Health Care Company Ltd, Germany) as a replacement for
warfarin for platelet inhibition due to inaccessible prothrombin
time monitoring. Among the 18 patients, 2 succumbed to their
condition during hospital stay, one was transferred to a higher
level hospital due to a serious condition but succumbed to their
condition the next day, and one discontinued the treatment and left
the hospital.
Results
Clinical characteristics
The CVT cases in the present study were analyzed and
the characteristics were summarized as follows: i) CVT tends to
occur among young adults, has an average onset age of 39 years, and
females are more likely to suffer from this disease than males with
a 1:2.5 gender ratio; ii) the majority of CVT cases exhibit acute
onset and progressive aggravation; iii) CVT is principally
manifested by headaches, emesis, papilledema, and sometimes blurred
vision; iv) neurological impairments such as limb paralysis and
language disorders may or may not be present; v) seizure disorders
or emotional disturbance may occur in company; and vi) the majority
of CVT cases occur during pregnancy and puerperium, but some are
caused by unknown reasons.
Misdiagnoses
There were eight misdiagnosed patients in this
study: one was misdiagnosed with cerebral hemorrhage, one with
hemorrhagic cerebral infarction, one with cerebral infarction, one
with subarachnoid bleeding, one with increased intracranial
pressure, two with viral encephalitis, and one was misdiagnosed
with intracranial space-occupying lesion and received neurosurgical
treatment, but was later transferred to the Department of Neurology
after the disclosure of superior sagittal sinus thrombosis by MER +
MRV. The misdiagnosed cases are reported briefly as follows:
Case 1.A patient was hospitalized for more
than 20 days of headaches. Medical examination revealed that
papilledema was more popular than other neurological focal signs.
CT and MRI + MRV were performed successively, but no abnormalities
were observed. Lumbar puncture disclosed a CSF pressure of 280
mmH2O, and thus he was preliminarily diagnosed with
increased intracranial pressure. After the doctors’ consultation,
DSA was performed. The results revealed that the patient had
partial visualization of the great cerebral vein and prolonged
cerebral circulation time.
Cases 2 and 3. CVT in two patients initially
manifested as headaches and fevers, with one accompanied by mental
symptoms and the other by meningeal irritation signs. Lumbar
puncture disclosed that they had increased intracranial CSF
pressures and mildly increased cell counts and CSF protein
concentrations. MRI did not display any abnormality in one patient
but revealed hypointensity on the T1-weighted image (WI) and
hyperintensity with small foci at the midst of the T2 WI of the
left temporal lobe in the other. The patients were diagnosed
preliminarily with viral meningitis. After hospitalization, they
received antiviral and dehydration treatments, but their conditions
were aggravated. One patient was subjected to lumbar puncture. The
results showed that her CSF pressure increased, albeit without
noticeable routine or biochemical changes. Cerebral MRV was
subsequently performed, and the results showed superior sagittal
sinus thrombosis. The patient received active of anticoagulation
and thrombolysis treatments, and was cured one month later. The
pathogenetic condition of the other patient deteriorated abruptly
and symptoms of consciousness disorders, convulsion, and anisocoria
appeared. Emergency MRI was performed for her, and the result
showed she had a large area of bleeding in the left temporal lobe,
a median line malposition, a brain herniation, and absence of the
flow void signals in the right jugular vein left and the transverse
and sigmoid sinuses (enhancement scanning further confirmed this
result). All rescue measures proved ineffectual and the patient
succumbed to her condition.
Case 4. A patient was hospitalized for left
limb weakness. Cerebral CT showed hypointensity in her right
frontal parietal lobe. The patient was first diagnosed with
cerebral infarction. However, the patient later presented with
aggravated symptoms with apparent headaches and projectile
vomiting. MRI + MRV exhibited superior sagittal sinus thrombosis
and bilateral parietal venous infarctions accompanied by
hemorrhage.
Case 5. A male patient was hospitalized after
three days of a headache and one day of right limb weakness. CT
showed cerebral hemorrhage in his left fronto-parietal junctional
region. The patient was treated according to the symptoms of
cerebral hemorrhage. However, the curative effect was poor: his
headache was aggravated and consciousness disorders manifested.
Further MRI + MRV revealed superior sagittal sinus thrombosis, an
expanded fronto-parietal bleeding size, and a median line
malposition.
Case 6. A patient presented with a headache
and left-side paralysis. CT showed that the patient had a right
parietal hemorrhagic infarction. Following treatment, the patient’s
condition deteriorated. Further MRI + MRV disclosed superior
sagittal sinus thrombosis and bilateral fronto-parietal venous
infarctions accompanied by hemorrhage, with the right side more
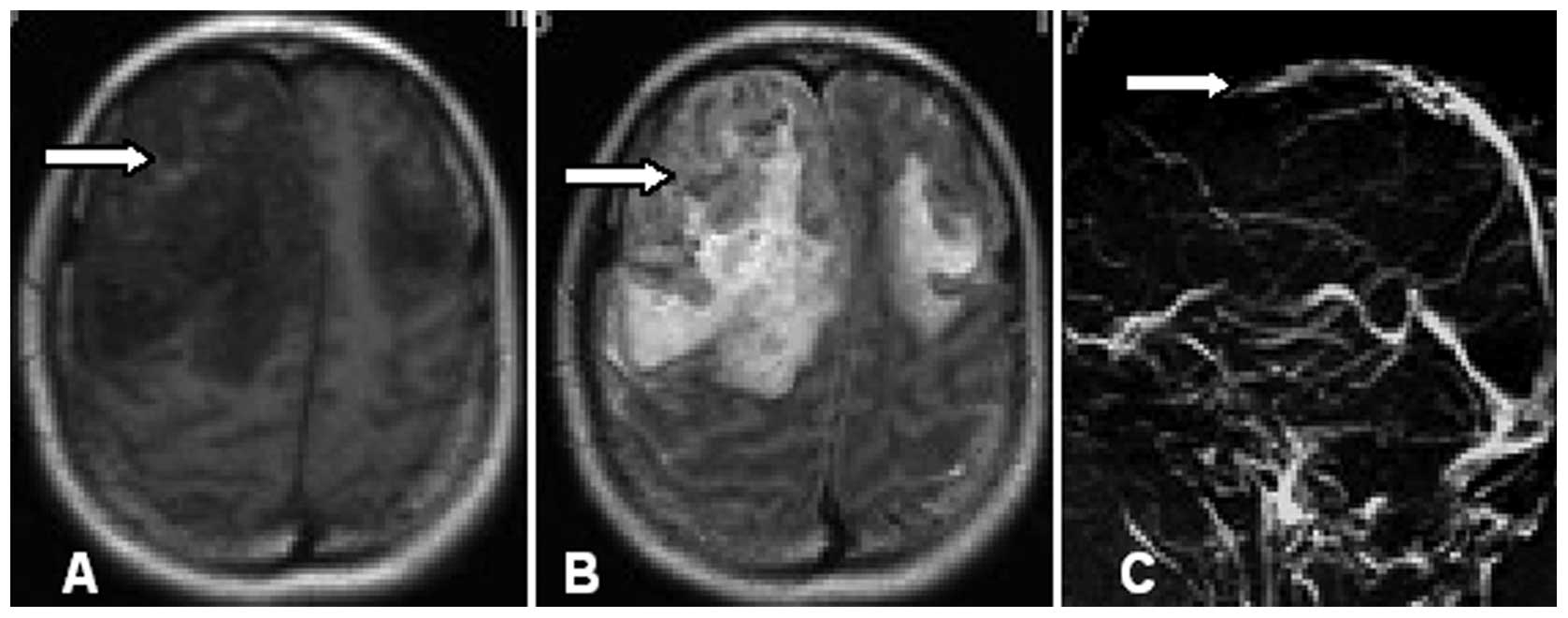
serious (Fig. 1).
Case 7. A patient suffered from headaches and
emeses. Medical checkup showed positive meningeal irritation signs
in the patient. Lumbar puncture and cerebral CT were performed. The
results showed that the patient had uniform bloody CSF with a
pressure of 310 mmH2O and subarachnoid bleeding. Two
days later, DSA disclosed bilateral transverse and sigmoid sinus
thromboses in the patient.
Case 8. The patient who was transferred from
the Department of Neurosurgery to the Department of Neurology
received cerebral CT for headaches and one-sided limb weakness. The
result showed a large area of mixed densities in her left frontal
lobe. The patient was misdiagnosed with intracranial
space-occupying lesion.
Discussion
CVT is a rare type of ischemic stroke. Its clinical
manifestations are varied and atypical due to lack of fixed
diseased regions, varying degrees of lesion severity, and different
progression velocities; these characteristics render definite
diagnosis of CVT difficult (7).
CVT can be induced by a variety of factors, such as
severe dehydration, external injuries, hematological diseases,
heart diseases, pregnancy, infections, immune abnormalities and
oral contraceptives; in addition, 20% of CVT cases are due to
unknown causes (8). Consequently,
in patients with CVT of unknown causes, the rates of misdiagnosis
and delayed diagnosis are also higher. In the present study, 4 of
the 8 misdiagnosed cases were due to uncertain causes.
Females are more likely to suffer from CVT,
accounting for 70–80% of all CVT patients (9). In this study, 13 of the 18 CVT
patients were females. Furthermore, among the 13 cases, one
occurred during gestational period and four occurred during
puerperium. Women in the perinatal period are the high-risk
population for CVT, as the concentrations of multiple blood
coagulation factors and fibrinogen increase and the blood stays in
a hypercoagulable state in this period, together with various
factors at the time of delivery such as a blood loss, greater
perspiration, hypovolemia, increased blood viscosity, and a
decelerated speed of blood flow. Bearing this in mind, in most
circumstances, clinicians are alert for the occurrence of CVT
whenever patients in perinatal period show symptoms of headaches
and emeses with or without focal neurological deficits. Therefore,
misdiagnosis of CVT in this population is rare.
Headache is the most common symptom of CVT, or even
the only symptom in some cases (10), with an incidence of 75–95% in
patients with CVT (6). The site of
headache bears no direct correlation with the site of sinus
thrombosis, except that approximately 61% of patients with sigmoid
sinus thrombus alone or with transverse sinus thrombus have pains
in the occipital and neck regions (7,11).
In addition, headaches may have varying degrees of severity in CVT
patients. Generally, a severe headache attracts attention more
easily from the patient and clinician. However, when headache
represents the only symptom without other neurological symptoms or
signs, misdiagnosis tends to occur, as in the first case in this
study, which was misdiagnosed for increased intracranial pressure.
For patients with symptoms of headache and upper respiratory tract
infection, misdiagnosis as viral meningitis frequently occurs
(there were two cases of such misdiagnosis in this study).
Furthermore, in addition to the common symptoms such as headache
and papilledema, certain CVT patients may present with focal
neurological impairments such as limb paralysis and language
disorders, or with seizure disorders and emotional disturbance. For
these patients, especially those whose imaging results show
cerebral infarction, cerebral hemorrhage, or intracranial space
occupation, misdiagnosis as a certain disease according to the
imaging result is also likely to occur. In this study, this factor
was responsible for the majority of the misdiagnosed cases.
The direct signs of cerebral CT reflect empty
triangle and cord signs, thereby providing important clues for
early diagnosis of CVT. However, although these signs have high
specificity, they have the drawback of a low positive rate. In this
study, only 1 out of 18 patients presented with an atypical empty
triangle sign. The indirect signs of cerebral CT can disclose focal
oedema or infarction and hemorrhage.
MRI combined with MRV is currently the preferred
atraumatic and effective diagnostic method for CVT (12,13).
MRI combined with MRV has even been considered as the gold standard
for diagnosis of CVT by certain investigators (14). In this study, more than 90% of the
patients were observed with abnormalities using this method.
The imaging results showed that most lesions
affecting the superior sagittal sinus were located in the frontal
and parietal lobes, and the affection was either unilateral or
bilateral (Fig. 1); lesions
affecting the transverse and sigmoid sinuses were primarily located
in the temporal lobe or in the tempo-occipital junctional region
and were manifested by localized edema, infarction (ischemic or
hemorrhagic, which does not comply with the distribution law of
arterial blood vessels), intracranial or cerebral ventricular
hemorrhage, and subarachnoid hemorrhage. Furthermore, this study
showed that disappearance of the flow void signals in venous
sinuses and changes in signal intensity are both capable of
indicating venous thrombosis. MRV can display not only the absence,
constriction, edge unsharpness, and filling defects of the blood
flow signals in the affected venous sinuses, but also the
conditions of the relevant collateral pathways. Being a noninvasive
blood vessel examination method, MRI + MRV is considered to be an
effective measure for CVT diagnosis. However, MRI + MRV has a
limitation, namely that anatomical variations and defective
development of a venous sinus often lead to the appearance of false
positivity. DSA can effectively overcome such a limitation and
therefore has been widely accepted as the gold standard for CVT
diagnosis. This method can clearly demonstrate a thrombosed site as
well as the scope of the thrombus and dynamically monitor venous
abnormal back flow and compensatory circulation. However, as DSA is
invasive, it has not been applied in routine examination to
date.
CSF examination through lumbar puncture can also
provide important information for CVT diagnosis. CVT patients have
increased intracranial CSF pressure, which is an important sign. In
addition, the majority of patients have normal or slightly
increased protein concentrations and cell counts. For patients in
whom these indices significantly increase, due attention should be
given to the possible occurrence of other diseases or CVT
complicated by other diseases, such as infections and tumors.
Currently, anticoagulation therapy is the primary
form of CVT treatment, which is also applicable to CVT patients
accompanied by intracranial hemorrhage. Specifically, anticoagulant
therapy can take the following forms: heparin is administered
subcutaneously or intravenously to double the activated partial
thromboplastin time; or warfarin is administered orally and the INR
of the treatment is adjusted to 2.0–3.0 (the recommended
application duration is three months to half a year, which can be
adjusted according to patients’ conditions). Other medical
treatments include dehydration to reduce intracranial pressure, and
active treatments of seizure activity and emotional disturbance.
Furthermore, the causes of CVT, such as immunological and
hemorheological abnormalities, should also be targeted in
treatment.
Endovascular interventional treatment may also
employ local thrombolysis. Drugs that can be used in this type of
therapy include urokinase and recombinant tissue type plasminogen
activator. Many investigators hold the view that local thrombolysis
therapy can achieve a greater curative effect than anticoagulant
therapy (15,16), on severe and progressive CVT in
particular (17,18). Nevertheless, other therapies, such
as balloon or catheter embolectomy and endovascular stent plasty
can be used for CVT treatment. However, as these procedures are
difficult to operate, costly and invasive, they have not been
widely applied in clinical practice.
For patients with severe CVT, especially severe CVT
with signs of cerebral hernia, decompressive craniectomy is an
effective way to increase survival rates (19).
CVT is a relatively rare type of ischemic
cerebrovascular disease; in recent years, the mortality rate of CVT
has been reduced to 6–30% due to markedly improved diagnosis and
recovery rates (20). These
improvements appear to be directly creditable to the technical
development of medical imaging. However, dependence on medical
imaging alone may cause misdiagnosis for other diseases such as
cerebral infarction, cerebral hemorrhage, subarachnoid hemorrhage
and tumor. Therefore, based on the experience in the treatment of
CVT, to further increase the diagnosis and recovery rates, the
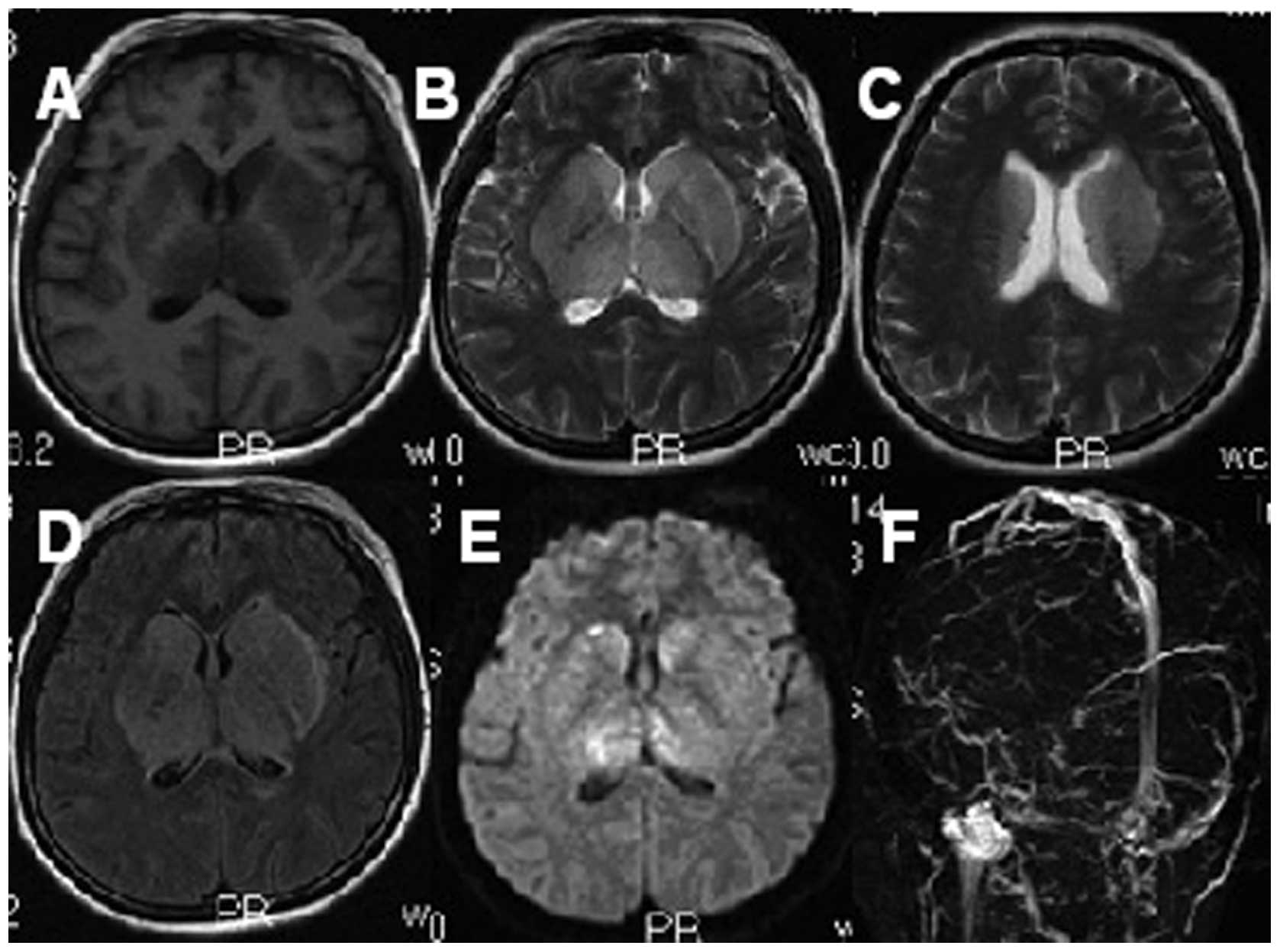
occurrence of CVT cannot be excluded in the following conditions:
when i) patients exhibit headache, fever, and increased CSF protein
concentration and cell count, and these symptoms cannot be improved
or are even aggravated following anti-infection treatment; ii)
cerebral hemorrhage does not fit with the distribution law of
arterial blood vessels, particularly in patients with non-seriously
restricted diffusion according to diffusion-weighted imaging
(vasogenic edema; Fig. 2), or
cerebral hemorrhage does fit with the characteristics of
hypertensive cerebral hemorrhage but these lesions fail to explain
the manifestations of intracranial hypertension such as headache
and fundus edema; iii) patients are observed with infarction foci
in the bilateral thalamus and basal ganglia regions according to CT
or MRI (high attention should be given to the possible occurrence
of great cerebral venous and straight sinus thromboses; Fig. 2); iv) patients are observed with
benign intracranial hypertension according to clinical examination
and with atypical intracranial space-occupying lesion according to
imaging; and v) patients, particularly adult patients, exhibit
headache and focal neurological deficits of uncertain causes, and
examination cannot completely explain the symptoms. Furthermore, CT
and MRI + MRV are simple and feasible methods in CVT diagnosis, and
further DSA can be performed when necessary.
References
|
1
|
Santos GR, André R, Pereira SL, Parreira T
and Machado E: Cerebral venous thrombosis: retrospective analysis
of 49 cases. Acta Med Port. 24:21–28. 2011.(in Portuguese).
|
|
2
|
Leach JL, Strub WM and Gaskill-Shipley MF:
Cerebral venous thrombus signal intensity and susceptibility
effects on gradient recalled-echo MR imaging. AJNR Am J
Neuroradiol. 28:940–945. 2007.PubMed/NCBI
|
|
3
|
Poon CS, Chang JK, Swarnkar A, Johnson MH
and Wasenko J: Radiologic diagnosis of cerebral venous thrombosis:
pictorial review. AJR Am J Roentgenol. 189:S64–S75. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Crombé D, Haven F and Gille M: Isolated
deep cerebral venous thrombosis diagnosed on CT and MR imaging. A
case study and literature review. JBR-BTR. 86:257–261.
2003.PubMed/NCBI
|
|
5
|
Rodallec MH, Krainik A, Feydy A, et al:
Cerebral venous thrombosis and multidetector CT angiography: tips
and tricks. Radiographics. 26:S5–S18. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Masuhr F, Mehraein S and Einhäupl K:
Cerebral venous and sinus thrombosis. J Neurol. 251:11–23. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chiewvit P, Piyapittayanan S and
Poungvarin N: Cerebral venous thrombosis: diagnosis dilemma. Neurol
Int. 3:e132011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Koopman K, Uyttenboogaart M, Hendriks HG,
et al: Thromboelastography in patients with cerebral venous
thrombosis. Thromb Res. 124:185–188. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Canhão P, Ferro JM, Lindgren AG, Bousser
MG, Stam J and Barinagarrementeria F: Causes and predictors of
death in cerebral venous thrombosis. Stroke. 36:1720–1725.
2005.
|
|
10
|
Cumurciuc R, Crassard I, Sarov M, Valade D
and Bousser MG: Headache as the only neurological sign of cerebral
venous thrombosis: a series of 17 cases. J Neurol Neurosurg
Psychiatry. 76:1084–1087. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wasay M, Kojan S, Dai AI, Bobustuc G and
Sheikh Z: Headache in cerebral venous thrombosis: incidence,
pattern and location in 200 consecutive patients. J Headache Pain.
11:137–139. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sajjad Z: MRI and MRV in cerebral venous
thrombosis. J Pak Med Assoc. 56:523–526. 2006.PubMed/NCBI
|
|
13
|
Moreno-Ramos MD, Rodríguez-Romero R,
Piñero-González de la Peña P, Rodríguez-Uranga J and
Monreal-Monsalve C: Noninvasive diagnosis of cerebral venous
thrombosis. Radiologia. 48:79–86. 2006.(in Spanish).
|
|
14
|
Kawai N, Shindou A, Masada T, Tamiya T and
Nagao S: Hemodynamic and metabolic changes in a patient with
cerebral venous sinus thrombosis: evaluation using O-15 positron
emission tomography. Clin Nucl Med. 30:391–394. 2005. View Article : Google Scholar
|
|
15
|
Stam J: Thrombosis of the cerebral veins
and sinuses. N Engl J Med. 352:1791–1798. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wasay M, Bakshi R, Kojan S, Bobustuc G,
Dubey N and Unwin DH: Nonrandomized comparison of local urokinase
thrombolysis versus systemic heparin anticoagulation for superior
sagittal sinus thrombosis. Stroke. 32:2310–2317. 2001. View Article : Google Scholar
|
|
17
|
Mohammadian R, Sohrabi B, Mansourizadeh R,
et al: Treatment of progressive cerebral sinuses thrombosis with
local thrombolysis. Interv Neuroradiol. 18:89–96. 2012.PubMed/NCBI
|
|
18
|
Coutinho JM, Ferro JM, Zuurbier SM, et al:
Thrombolysis or anticoagulation for cerebral venous thrombosis:
rationale and design of the TO-ACT trial. Int J Stroke. Feb.
20–2012.(Epub ahead of print). View Article : Google Scholar
|
|
19
|
Ferro JM, Crassard I, Coutinho JM, et al:
Decompressive surgery in cerebrovenous thrombosis: a multicenter
registry and a systematic review of individual patient data.
Stroke. 42:2825–2831. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Smith R and Hourihan MD: Investigating
suspected cerebral venous thrombosis. BMJ. 334:794–795. 2007.
View Article : Google Scholar : PubMed/NCBI
|