Introduction
Tuberculosis is an infectious disease, but its
incidence rate has exhibited a gradual decrease (1). There are often reports on laparoscopy
results of abdominal tuberculosis peritonitis. When a patient
presents with unexplained ascites, laparoscopy may contribute to
the diagnosis of this disease (2).
In this study, we describe the apparent changes in the laparoscopy
results from a female with tuberculous peritonitis during the
16-month illness.
Materials and methods
General data
On January 12, 2010, a 78-year-old female with a
fever of 39°C and abdominal distention symptoms was transferred
from the Emergency Department to the Department of Tuberculosis,
The First Affiliated Hospital of Xinxiang Medical College (Weihui,
China). Upon hospitalization, physical examination results of the
patient were as follows: body temperature, 38°C; blood pressure,
163/73 mmHg; heart rate, 89 beats/min; and stable vital signs. The
following results indicated the presence of inflammation in the
body: leukocyte count, 34×109/μl; rod nuclear
cells, 85.5%; erythrocyte sedimentation rate (ESR), 28 mm/h;
C-reactive protein (CRP), 75 mg/l; yet normal liver and kindey
functions. In addition, the tuberculin test diameter was 10×9 mm.
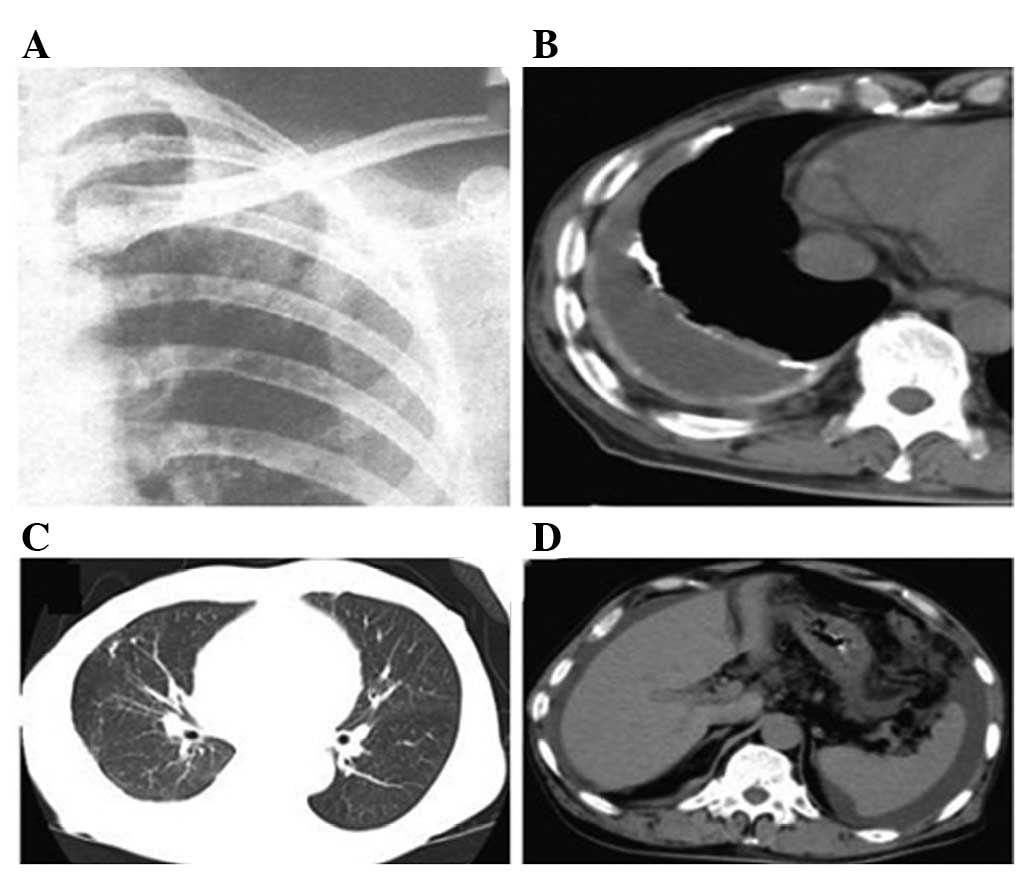
However, chest X ray and pectoral and abdominal CT demonstrated
that there was hydrops in the chest and abdomen. As the patient had
previously suffered from pulmonary tuberculosis at 27 years of age,
the lung presented with calcification foci caused by previous
pulmonary tuberculosis (Fig. 1).
Fever, CT examination results and inflammation symptoms suggested
that the patient suffered from tuberculosis.
Laboratory examination
The Rivalta test result of the ascites was positive
and the adenosine deaminase (ADA) level was high (117.8 U/l).
However, the conventional staining and culture test results of
Mycobacterium tuberculosis in the ascites were negative, and
bacteria or tumor cells were undetectable.
Treatment
Continuous antituberculous drugs isoniazid (INH; 0.4
g/day), rifampin (RFP; 0.45 g/day), pyrazinamide (PZA; 1.5 g/day)
and ethambutol (EB; 1 g/day), and antibiotics imipenem/cilastatin
(IPM/CS) were administered for treatment. The following day, the
fever disappeared. After IPM/CS administration was stopped, the
body temperature of the patient increased. Therefore, antibiotic
treatment was conducted continuously and ascites gradually reduced.
After one month, the febrile symptom recurred, and EB
administration was stopped and replaced with streptomycin (SM)
treatment (1 g, 3 days/week). Subsequently, the body temperature
was restored to the normal level, and systemic conditions were
improved and became gradually stable.
Results
Laparoscopy
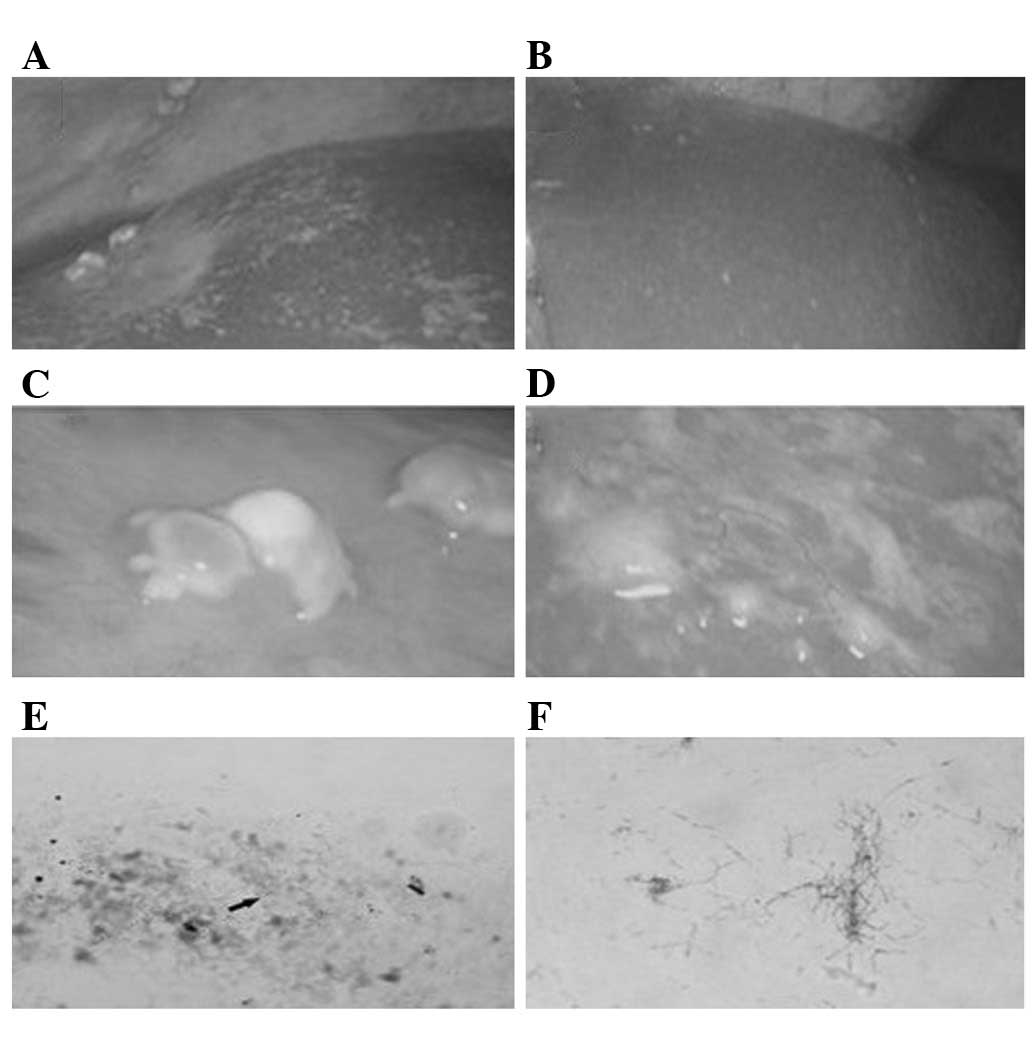
As shown in Fig. 2,
it was clear that the liver capsule became white in the right and
left lobes of the liver (Fig. 2A and
B, respectively). The left lobe of the liver also had typical
yellow-white nodules (Fig. 2C) and
numerous white small nodules (Fig.
2D). Fig. 2E and F shows that
the Mycobacterium tuberculosis Gram staining result of
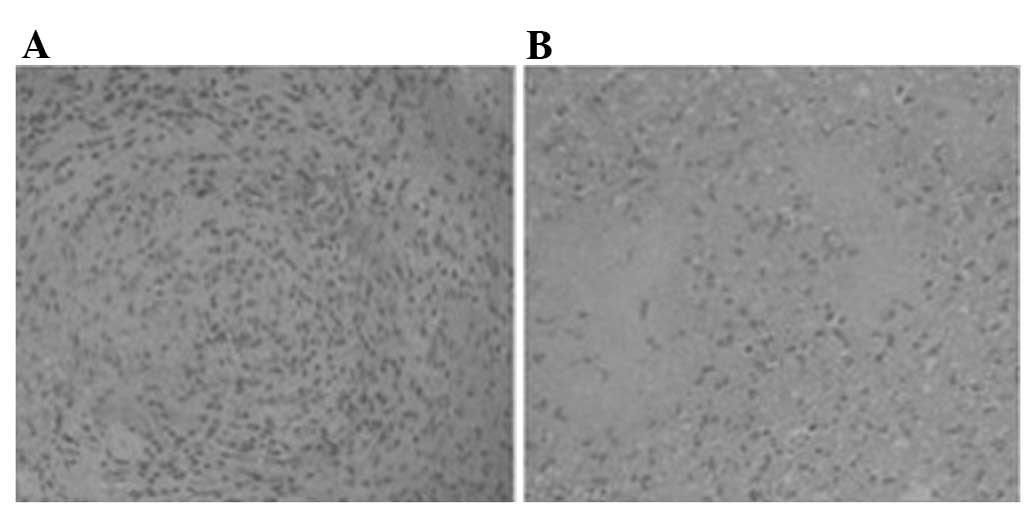
nodules selected under the laparoscope was positive. Fig. 3A and B shows epithelioid cell
granuloma and caseous necrosis, repectively. These results were in
agreement with the diagnosis of tuberculous peritonitis.
Second laparoscopy
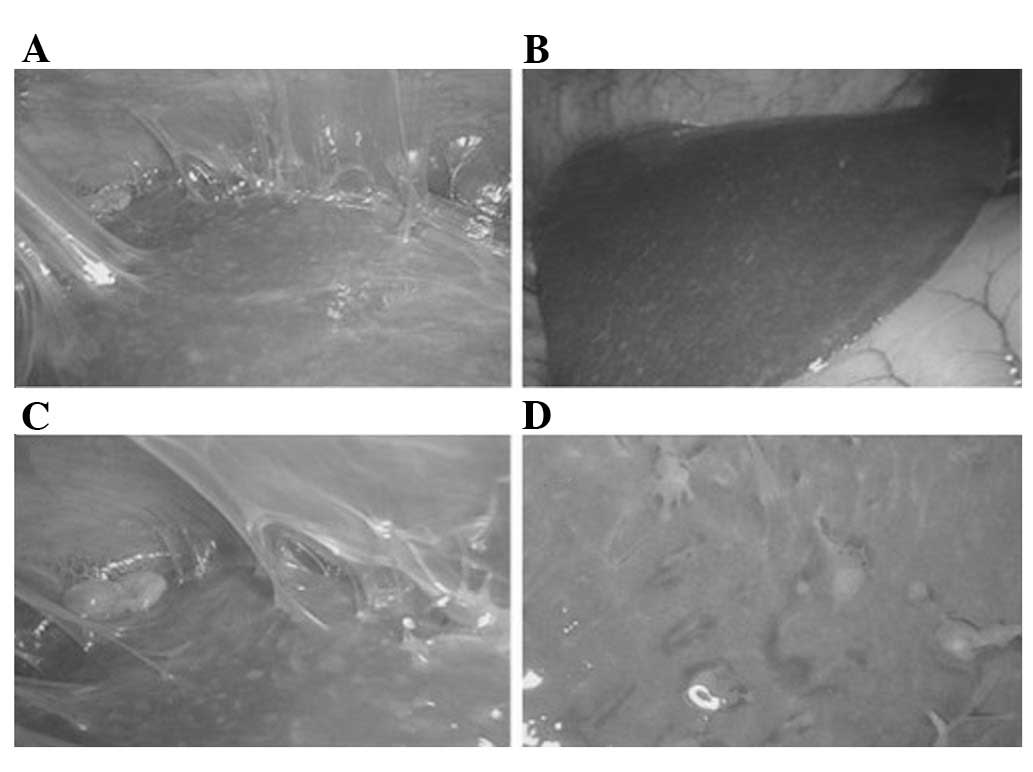
After antituberculous drug treatment was conducted,
the patient left hospital on May 1, 2010, and the disease condition
was stable. The patient received a second laparoscopy before
termination of antituberculous drug treatment to confirm that the
disease status was improved. The patient was hospitalized at the
Department of Tuberculosis (The First Affiliated Hospital of
Xinxiang Medical College) and the laparoscopy was conducted in
early May 2011. At this time, macroscopic examination results were
improved (Fig. 4). Tuberculous
peritonitis symptoms of the right lobe of the liver (Fig. 4A) and the left lobe of the liver
(Fig. 4B) were impoved. White
nodules were greatly reduced (Fig.
4D). In addition, yellow-white nodules on the liver surface
were greatly reduced, and the extent of whitening of liver capsules
was also improved. However, the left lobe adhesions of the liver
presented a fibrin network (Fig.
4C). Numerous fibrin networks adhering to the peritoneum
(typical symptoms of tuberculous peritonitis) caused by the early
inflammation were still present.
Table I shows the
clinical progress of CRP level normalization after the patient was
treated with antituberculosis drugs INH, RFP, PZA and SM. One week
after the second laparoscopy, the patient was released from the
hospital, and the antituberculous drug treatment was terminated.
According to the data of this case, we suggest that laparoscopy may
be used to examine the development of tuberculous peritonitis.
 | Table IComparison of reaction time between
the intervention and surgical treatment CRP (mg/l). |
Table I
Comparison of reaction time between
the intervention and surgical treatment CRP (mg/l).
| Time (months)
|
|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 12 | 16 |
|---|
| CRP mg/l | 75 | 16 | 12 | 11 | 11 | 10 | 9 | 5 |
Discussion
Tuberculous peritonitis may be diagnosed by directly
coating the ascites sample onto a slide to conduct Gram staining or
culture Mycobacterium tuberculosis from the ascites sample.
However, these methods are usually unreliable (3). The sensitivity of Gram staining
ranges from 0 to 6% and the majority of staining results of
tuberculous ascites are negative (4). Laparoscopy and biopsy are believed to
be extremely useful for the identification and diagnosis of
tuberculous peritonitis, cancer or infectious disease (5). Compared with the diagnosis rate of CT
imaging examination (69%), the definitive diagnosis rate of a
combination of three laparoscope examinations and a biopsy of
unknown-source ascites reaches 85–100%.
Another advantage of laparoscopy is that its result
is obtained far earlier than that of the traditional microbiology
approach, such as ascites culture or PCR method, which usually
require 2–4 weeks. For patients with tuberculous peritonitis, the
failure rate of laparoscopy may reach 16%, and is not completely
risk-free (6). Laparoscopy is able
to reveal the typical fibronectin forms of tuberculous peritonitis,
called a fibrin network. Intestinal perforation is a serious
complication and currently it is believed that intestinal
perforation usually appears in fibronectin-type tuberculous
peritonitis. In this study, the first laparoscopy revealed no
peritoneal adhesion, while the second laparoscopy showed fibrin
networks with obvious adhesion. This phenomenon suggests that early
laparoscopy examination was safer than the late stage for
tuberculous peritonitis.
The characteristics evident with tuberculous
peritonitis laparoscopy are the presence of multiple yellow-white
nodules and parietal peritoneum ascites on the visceral surface. It
is extremely difficult to differentiate these nodules from hepatic
sarcoidosis. In this study, this type of nodule on the liver
surface was present, and direct Gram staining of the nodule sample
showed Mycobacterium tuberculosis infection. In addition,
hepatic biopsy results demonstrated the presence of epithelioid
cell granuloma. These results confirmed the diagnosis of
tuberculous peritonitis. Laparoscopy and biopsy contribute to the
rapid and definitive diagnosis of tuberculous peritonitis.
Peritoneal or visceral adhesion and occasional peritoneal
inflammation and bleeding are possible symptoms of tuberculous
peritonitis. After the specific antituberculous drug treatment, the
second laparoscopy of the patient showed that the yellow-white
nodules on the liver surface disappeared. However, numerous fibrin
networks adhering to the peritoneum were still noted, which is the
typical symptom of tuberculous peritonitis and the result of early
inflammation. When the patient was nearly cured, the laparoscopy
results revealed that the yellow-white nodules on the liver surface
were greatly reduced. Therefore, laparoscopy may be used for the
evaluation of treatment efficiency. However, it is necessary to
consider the operation risk caused by Mycobacterium
tuberculosis-induced adhesion in the case of subsequent
laparoscopy.
References
|
1
|
Kaya M, Kaplan MA, Isikdogan A and Celik
Y: Differentiation of tuberculous peritonitis from peritonitis
carcinomatosa without surgical intervention. Saudi J Gastroenterol.
17:312–317. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kang HM, Oh TH, Kang GH, et al: A case of
Chlamydia trachomatis peritonitis mimicking tuberculous
peritonitis. Korean J Gastroenterol. 58:111–116. 2011.(In
Korean).
|
|
3
|
Ghosh B, Pande A, Ghosh A, Banerjee A and
Saha S: Membranous glomerulonephritis and tuberculous peritonitis:
a rare association. J Infect Dev Ctries. 5:550–552. 2011.PubMed/NCBI
|
|
4
|
Patel SM and Sweetser S: The wet-ascitic
form of tuberculous peritonitis. Hepatology. 54:364–365. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cho OH, Park KH, Park SJ, et al: Rapid
diagnosis of tuberculous peritonitis by T cell-based assays on
peripheral blood and peritoneal fluid mononuclear cells. Infect.
62:462–471. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wu D and Giri B: Haemophilus
paraphrophilus peritonitis followed by tuberculous peritonitis and
Pott’s disease. Am J Med Sci. 340:511–513. 2010.PubMed/NCBI
|