Introduction
In the clinic, intervention-related vascular spasms
are common in percutaneous coronary intervention (PCI) due to the
mechanical stimulation caused by balloon dilatation or stent
release (1). Injections of a
vasodilator into the coronary artery are able to mitigate these
spasms and consequently, the prognosis is good. However, clinical
occurrences of non-intervention-related vascular spasms following
coronary stenting are rare. It is also unclear as to whether the
clinical manifestation and pathogenesis of non-intervention-related
vascular spasms are different from those of intervention-related
vascular spasms. In the present study, the clinical features and
medical treatments of 2 cases of non-intervention-related vascular
spasms are reported and the potential causes are discussed.
Informed consent was ontained from the patient or family
members.
Case reports
Case 1
The first patient was a 73-year-old male, whose
cardiovascular risk factors included smoking for 30 years, an
impaired glucose tolerance for 2 years and hypertension for >30
years. On September 9, 2009, the patient was admitted to the Subei
People’s Hospital Affiliated to Yangzhou University, Jiangsu,
China, due to repeated exertional chest pain. Selective coronary
angiography (CAG) showed that the proximal left anterior descending
(LAD) artery had a 90% segmental stenosis, while the circumflex
artery and the right coronary artery (RCA) were normal. Following
the implantation of a 4.0×15-mm Yinyi stent (Liaoning Biomedical
Materials R&D Center Co., Ltd., Dalian, China) into the LAD
lesion, there was no post-operative chest pain. On May 8, 2012, the
patient was admitted again to the hospital due to unstable angina
pectoris. CAG showed that the stenosis had reoccurred in 70–80% of
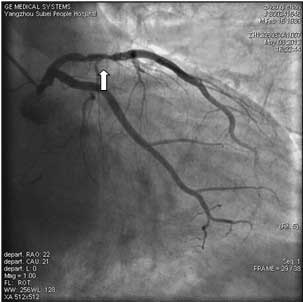
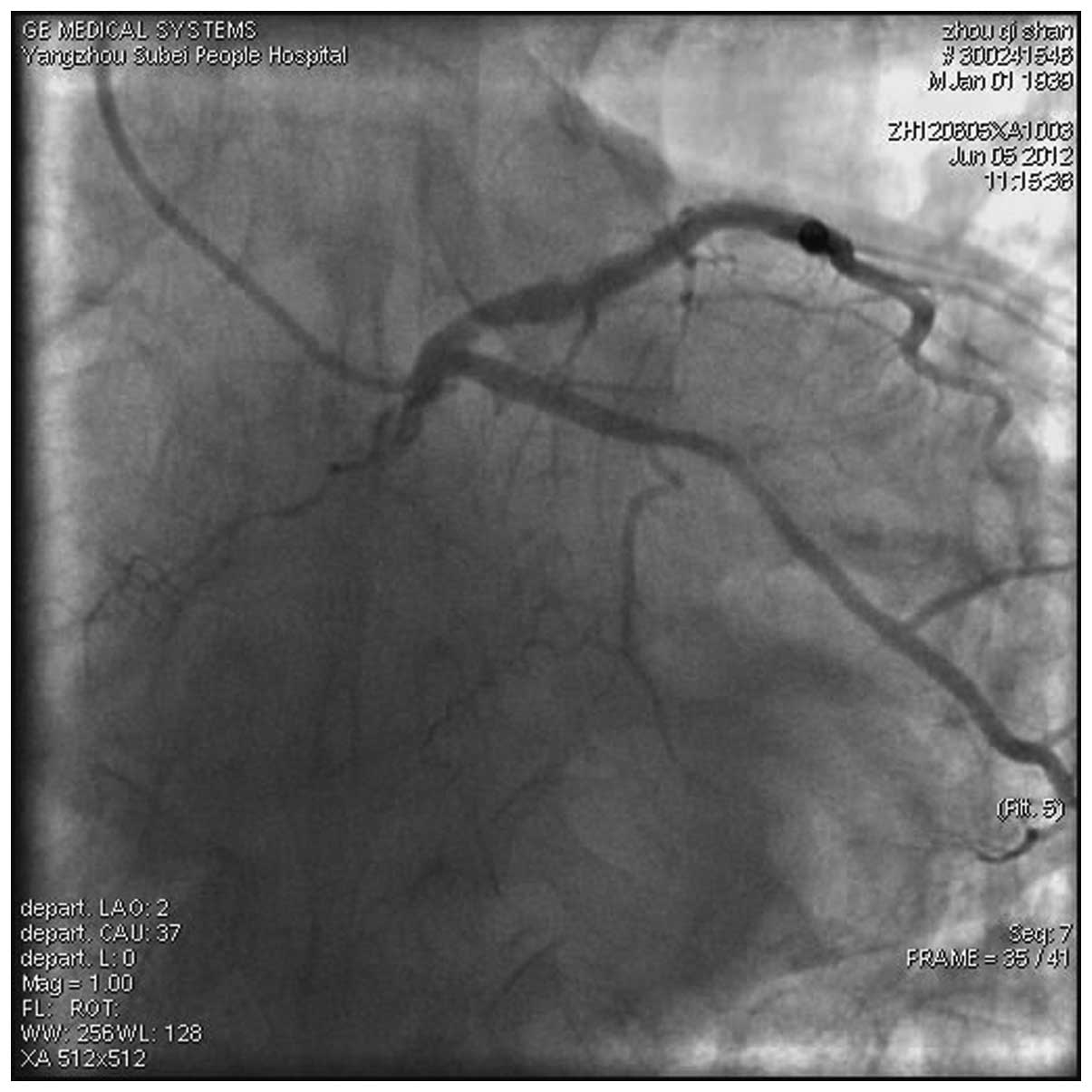
the LAD stent (Fig. 1). The
patient was hesitant whether to undergo PCI again, however on May
15, 2012, agreed to receive the treatment. The initial angiography
result is shown in Fig. 1.
Following pre-dilation with a 4.0×18-mm balloon at 8 atm for 10
sec, a 2.5×15-mm Resolute stent (Medtronic Inc., Galway, Republic
of Ireland) was implanted in the LAD lesions. The patient
immediately felt chest pain for ∼20 min following the stent
implantation. The CAG review showed no abnormalities. Subsequent to
the post-operative administration of a standard dual anti-platelet
and statin drug, the patient did not feel the chest pain again. On
May 20, 2012, on the night of the discharge day, the patient was
admitted as an emergency due to sudden chest pain for 1 h with
hypotension, syncope and ventricular tachycardia. On admission,
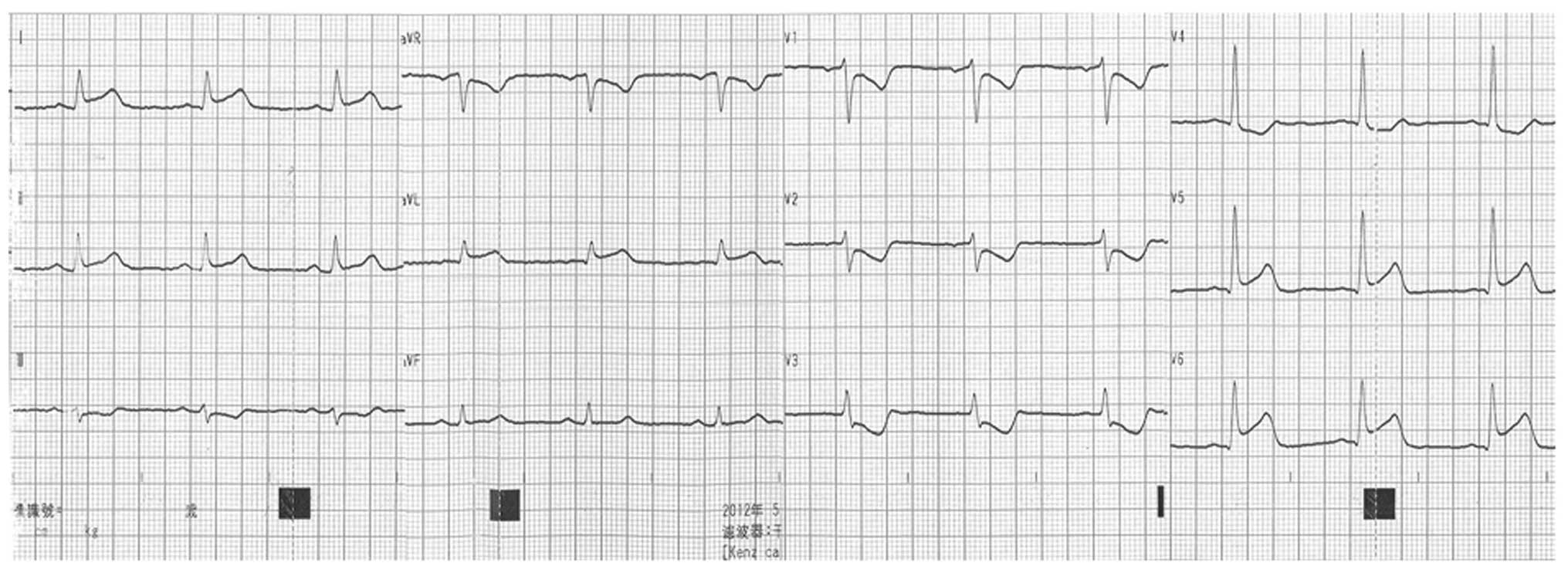
echocardiography (ECG) showed significant depression in the V1-4 ST
segment, inversion of the T wave and an elevation of the I, AVL and
V6 ST segments (Fig. 2). Emergency
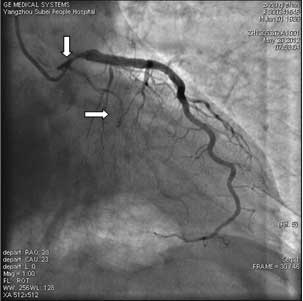
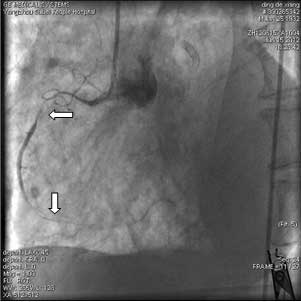
CAG showed that 80–90% of the blood vessel, which is from proximal
segment of the LAD stent to the LAD opening, appeared stenotic. The
LAD artery stent was unobstructed. The entire left circumflex (LCX)
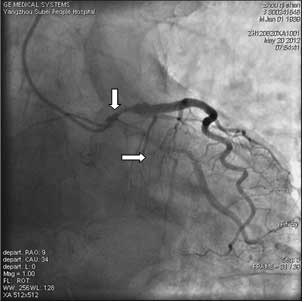
artery appeared to be in severe spasm (Fig. 3). Following repeated injections of
nitroglycerin into the coronary artery using a guiding catheter,
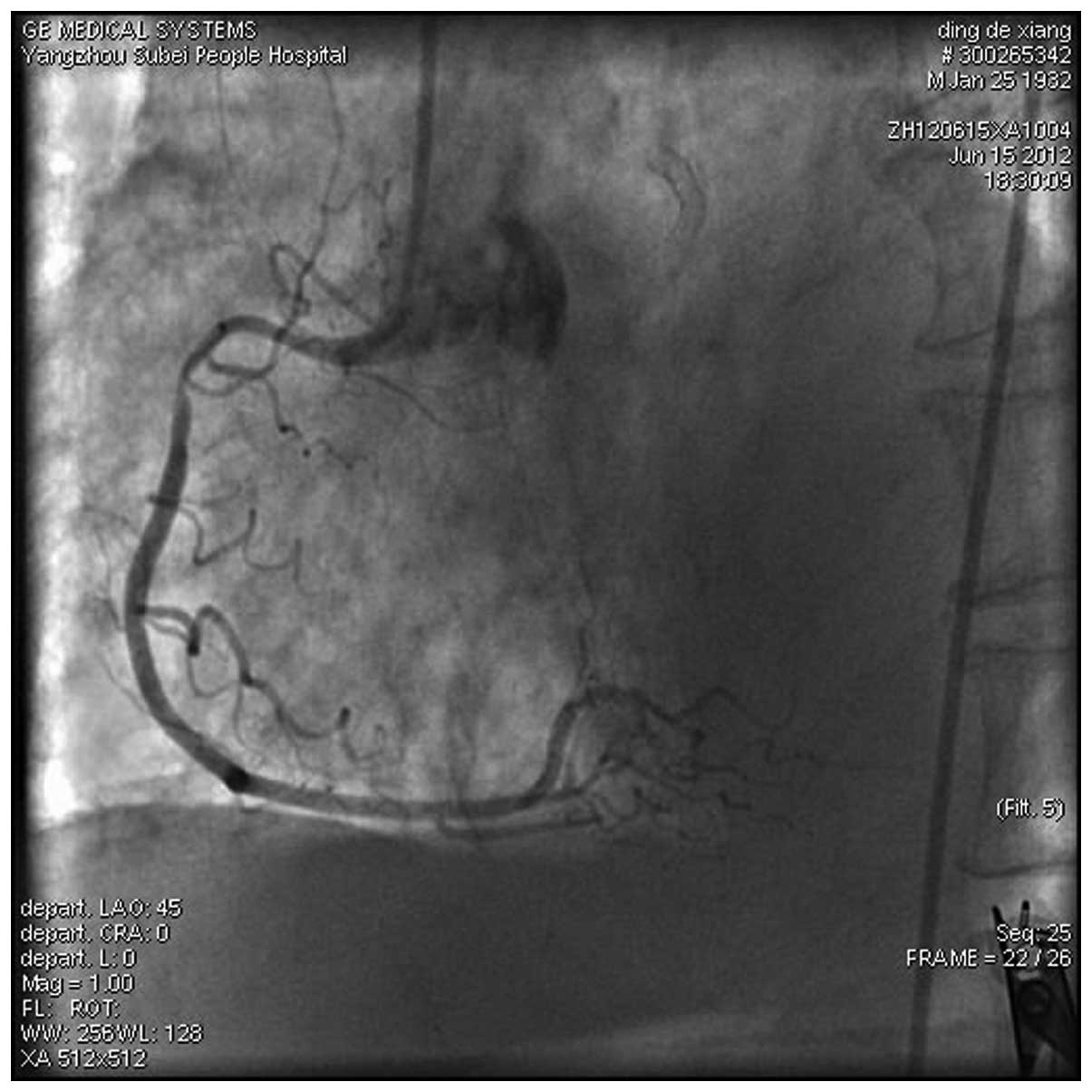
the LAD and LCX artery spasms were partially relieved (Fig. 4). Post-operatively, a mild chest
pain remained. Following the administration of a dual anti-platelet
and statin and the joint use of diltiazem, nifedipine and
anti-anxiety treatment for 4 days, the chest pain was totally
relieved. On June 5, 2012, a mild spasm remained detectable in the
middle of the circumflex artery, as shown by the CAG review
(Fig. 5).
Case 2
The second patient was an 80-year-old male, with the
cardiovascular risk factors of hypertension and a history of heavy
smoking. On June 15, 2012 the patient had repeated chest pain
associated with a shortness of breath that had lasted for one month
and was admitted to the hospital following aggravation of these
symptoms for 13 h. ECG revealed acute extensive anterior myocardial
infarction with cardiac dysfunction, a decrease in the motion of
the anterior segmental chamber wall and a small amount of
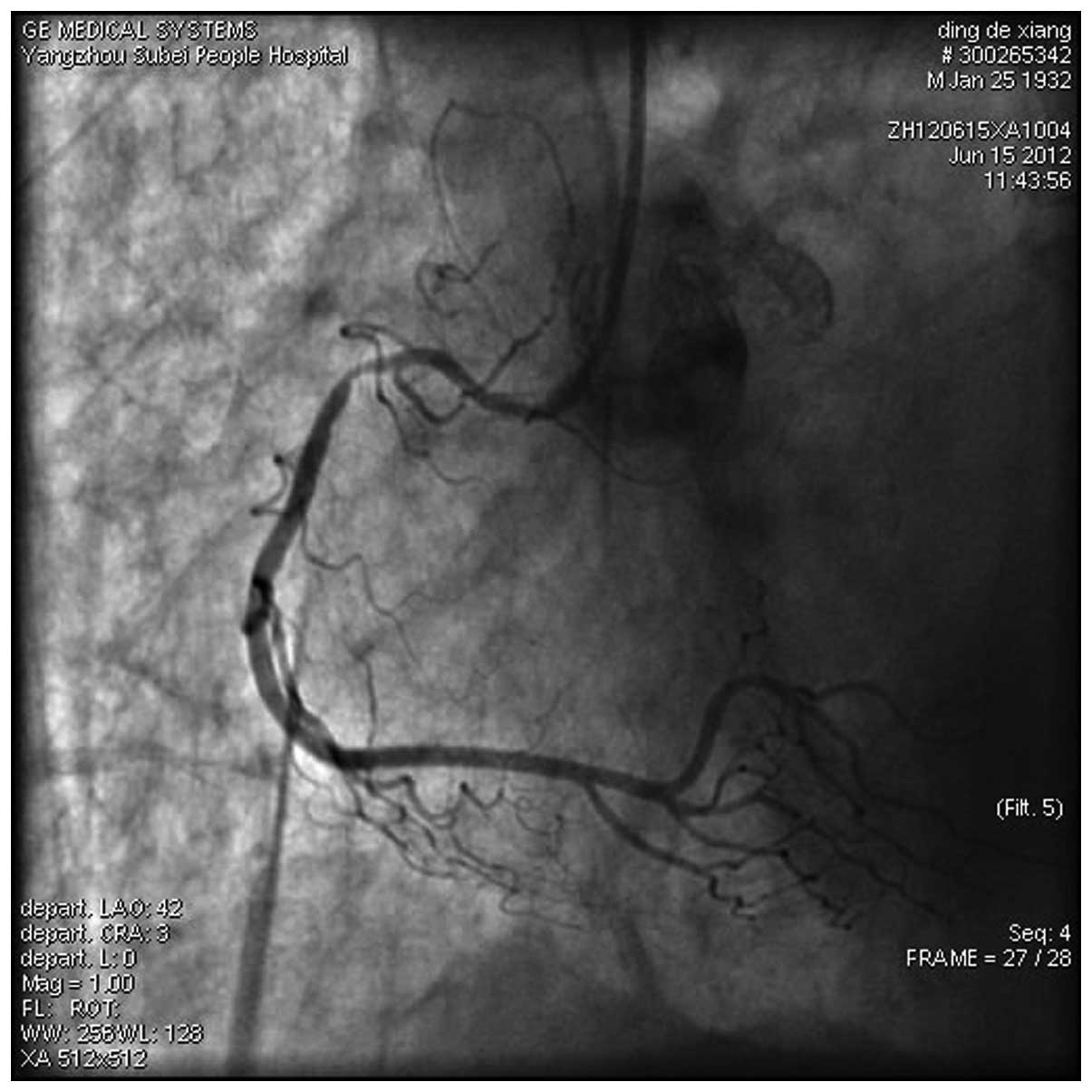
pericardial effusion. Emergency CAG revealed complete occlusion of
the proximal segment of the LAD artery. The LCX artery showed no
exception. The proximal segment of the RCA was shown to be 85%
stenotic (Figs. 6 and 7). Following pre-dilation with a
2.5×15-mm balloon at 8 atm for 10 sec, a 3.0×33-mm Firebird stent
(Shanghai MicroPort Medical Co., Ltd., Shanghai, China) was
implanted in the LAD lesions. CAG showed that the blood flow in the
LAD artery was between Thrombolysis In Myocardial Infarction (TIMI)
levels 2 and 3. At 4 h subsequent to the emergency PCI, the patient
felt a persistent chest pain again. Upon review, the ECG results
showed no significant dynamic changes when compared with the first
PCI. Emergency CAG showed blood flow in the LAD artery at TIMI
level 3 and a strong spasm in the entire RCA (Fig. 8). Following repeated injections of
nitroglycerin in the RCA using a guiding catheter, the coronary
spasms were relieved (Fig. 9).
During the surgery, the chest pains were also relieved. The patient
did not adhere to the use of calcium antagonists following the
surgery and suffered a sudden drop in blood pressure with body
sweats and a slow heart rate, which showed a ventricular escape
rhythm and cardiac arrest at 20 h subsequent to the second CAG. ECG
revealed a pericardial effusion and cardiac rupture.
Discussion
Angina caused by a coronary artery spasm is called
vasospastic angina (VSA) (2). The
usual presentation of this is temporary chest pain at rest
(3). Certain cases may also
present with acute myocardial infarction, malignant arrhythmias,
sudden mortality and even cardiac rupture (4,5).
It is common for vascular spasms to occur due to
mechanical stimulation in a remote segment of a coronary artery
stent during implantation (1). An
intracoronary injection of nitroglycerin is always able to quickly
alleviate the spasms. There have also been studies reporting
spontaneous spasms at the stent edges following several months of
use (6). The prognosis of these
cases is usually good. There are also rare clinical occurrences of
non-intervention-related vascular spasm following coronary
stenting. Versaci et al reported one case with LAD and LCX
artery spasms following RCA stent implantation (7). In this report, the coronary spasm was
transient and did not cause serious consequences. Wong et al
reported one case with a sustained, serious and widespread spasm in
the entire left coronary system during LAD coronary artery
stenting. A coronary injection of vasodilator using a guiding
catheter was unsuccessful in this patient who suffered acute
pulmonary edema and cardiogenic shock. The coronary spasm was
finally relieved by an injection of nitroglycerin into the distal
segment of the spastic vessel through a micro-catheter (8).
The present study reported two cases of patients
with the following characteristics: i) The non-invasive vascular
system was involved in the coronary artery spasms. In case 1 the
left coronary system showed widespread spasms, involving the LAD
and LCX arteries following LAD artery stenting. In case 2, the RCA
showed spasms at all stages following LAD artery stenting. ii)
Strong spasms caused coronary artery lumen occlusion. The spasms
were long lasting, stubborn and only partially relieved following
multiple injections of nitroglycerin through the coronary artery;
furthermore, repeated attacks were observed within a short time. In
case 1, four days of post-operative joint administration of
diltiazem, nifedipine and anti-anxiety treatment were required to
fully control the chest pain. It was unfortunate that the patient
from case 2 did not adhere to the application of calcium
antagonists to prevent the cramps that recurred following reduction
of the spasms. iii) The risk of clinical symptoms: There were
widespread spasms in the LAD and LCX coronary arteries of case 1,
similar to a blockage in the left main coronary artery, resulting
in hypotension, syncope and ventricular tachycardia. The patient in
case 2 had persistent chest pain following LAD artery emergency
stenting. Emergency CAG showed that the blood flow in the LAD
artery was significantly improved but that a strong spasm remained
in the RCA. The patient subsequently succumbed to a cardiac
rupture. It is not possible to rule out the strong spasms in the
RCA as a factor in the patient’s mortality.
Coronary spasms are associated with a variety of
factors, including strenuous exercise, excessive expansion of the
coronary artery, gene polymorphisms of endothelial nitric oxide
synthase, hyperthyroidism, smoking, the use of dobutamine (9) and cocaine, and drinking. Stent
implantation may aggravate or cause endothelial dysfunction.
Vasoconstriction is enhanced at each end of the stent. The
implantation of a drug-eluting stent is more likely to induce a
vascular spasm (10,11). Kim et al reported a case
with acute inferior myocardial infarction. Drug-eluting stents were
implanted into the RCA and LAD and LCX arteries, and 10 h later the
wide spasms appeared in the left coronary artery and RCA. The main
cause of the multiple vasospasm induction was proposed to be an
endothelial injury during the process of drug stent implantation
(12). In the present study, the
patient in case 1 felt chest pain for ∼20 min immediately after
stent implantation in the LAD coronary artery. However, the CAG
results were normal. The strong coronary spasm on the fourth day
subsequent to stenting may have been related to the selection of a
larger stent and the stimulation of excessive traction in the
stenting segment of the LAD artery. Also, the patient demonstrated
an evident anxiety prior to the stent implantation, therefore, when
the review CAG showed in-stent restenosis, the patient did not
agree to receive the same level of PCI. We believe that emotional
anxiety in patients may be a factor that aggravates coronary
spasms. The patient in case 2 had an acute occlusion of the LAD
artery. The reason for the spasm in the RCA following stenting in
the LAD artery remains unclear. However, the reason may be that the
body was in a state of stress due to the release of catecholamines
and inflammatory mediators as a consequence of the acute myocardial
infarction.
In summary, there are rare clinical occurrences of
non-intervention-related vascular spasms following coronary
stenting. These spasms have the characteristics of a broad, strong
and long duration with repeated episodes. The clinical course has
dangers. In emergencies, repeated injections of vasodilator into
the coronary artery and rapid remission of the spasms are important
for salvage and therapy. Post-operative high-dose calcium
antagonists and a mechanism-focused treatment for the spasms may
also be extremely important.
References
|
1.
|
Fischell TA: Coronary artery spasm after
percutaneous transluminal coronary angioplasty: pathophysiology and
clinical consequences. Cathet Cardiovasc Diagn. 19:1–3. 1990.
View Article : Google Scholar
|
|
2.
|
Kusama Y, Kodani E, Nakagomi A, et al:
Variant angina and coronary artery spasm: the clinical spectrum,
pathophysiology, and management. J Nippon Med Sch. 78:4–12. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Prinzmetal M, Kennamer R, Merliss R, et
al: Angina pectoris. I. A variant form of angina pectoris;
preliminary report. Am J Med. 27:375–388. 1959. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Hillis LD and Braunwald E: Coronary-artery
spasm. N Engl J Med. 299:695–702. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Maseri A, L’Abbate A, Baroldi G, et al:
Coronary vasospasm as a possible cause of myocardial infarction. A
conclusion derived from the study of ‘preinfarction’ angina. N Engl
J Med. 299:1271–1277. 1987.PubMed/NCBI
|
|
6.
|
Kaku B, Kanaya H and Horita Y: Spontaneous
stent-edge spasm in a patient with myocardial infarction. Heart.
91:9372005. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Versaci F, Gaspardone A and Proietti I:
Left anterior descending and circumflex coronary artery spasm after
right coronary artery stent implantation. Heart. 88:5202002.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Wong A, Cheng A, Chan C, et al:
Cardiogenic shock caused by severe coronary artery spasm
immediately after coronary stenting. Tex Heart Inst J. 32:78–80.
2005.PubMed/NCBI
|
|
9.
|
Bonvini RF, Hendiri T and Sigwart U:
Angiographic documented dobutamine induced coronary spasm
successfully treated by stenting. Heart. 92:10542006. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Kitahara H, Kobayashi Y, Iwata Y, et al:
Effect of pioglitazone on endothelial dysfunction after
sirolimus-eluting stent implantation. Am J Cardiol. 108:214–219.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Ito S, Nakasuka K, Morimoto K, et al:
Angiographic and clinical characteristics of patients with
acetylcholine-induced coronary vasospasm on follow-up coronary
angiography following drug-eluting stent implantation. J Invasive
Cardiol. 23:57–64. 2011.
|
|
12.
|
Kim JW, Park CG, Seo HS and Oh DJ: Delayed
severe multivessel spasm and aborted sudden death after Taxus stent
implantation. Heart. 91:e152005. View Article : Google Scholar : PubMed/NCBI
|