Introduction
Comminuted intercondylar fractures of the distal
humerus in young adults are difficult to treat due to the complex
anatomy of the elbow, small fracture fragments and the limited
amount of subchondral bone (1,2).
These fractures in young adults often occur as a result of
high-energy trauma and usually require early operative treatment
with accurate anatomic reduction of the joint fragments and stable
fixation to provide early mobilization and satisfactory results
(3,4). Open reduction and internal fixation
using plates have demonstrated satisfactory clinical outcomes for
the treatment of intercondylar fractures of the distal humerus and
various plating methods have been described to achieve firm
stabilization (5–8). One study demonstrated that
double-plate fixation provides more stable fixation than other
methods (9). However, controversy
remains concerning plate positions in terms of providing optimal
stability for intercondylar distal humerus fractures. The widely
used double-plate fixation methods involve: i) placing plates
parallel to each other in the sagittal plane, with two plates on
each supracondylar ridge; ii) placing plates perpendicular to each
other, with one on the medial supracondylar ridge and the other on
the lateral posterior; and iii) placing plates in a Y shape in the
coronal plane, with two plates on the medial and lateral posterior
surfaces of the distal humerus. Although a number of studies have
compared the first two methods in terms of clinical outcomes or
biomechanism (10–12), few studies have compared the
clinical outcomes of the last two methods when used to treat
intercondylar fractures of young adult distal humeri. The purpose
of the present study was to compare the clinical outcomes and
complications of perpendicular and Y-shaped double-plating in young
adults with intercondylar fractures of the distal humerus.
Subjects and methods
Subjects
From October 2008 to October 2011, 29 consecutive
patients with intercondylar fractures of the distal humerus were
treated with open reduction and double-plate fixation in the Second
Hospital Affiliated to Anhui Medical University (Hefei, China).
Four patients were lost to follow-up and the remaining 25 patients
were followed up for a minimum of 12 months. Patients included in
this study were selected based on the following criteria: distal
humeral fractures classified as type C according to the Association
for Osteosynthesis/Association for the Study of Internal Fixation
(AO/ASIF) classification system (13), and a minimum follow-up after
surgery of 12 months. Exclusion criteria were: i) suspicion of
primary or metastatic tumors with a pathological fracture and ii)
age <18 or >60 years.
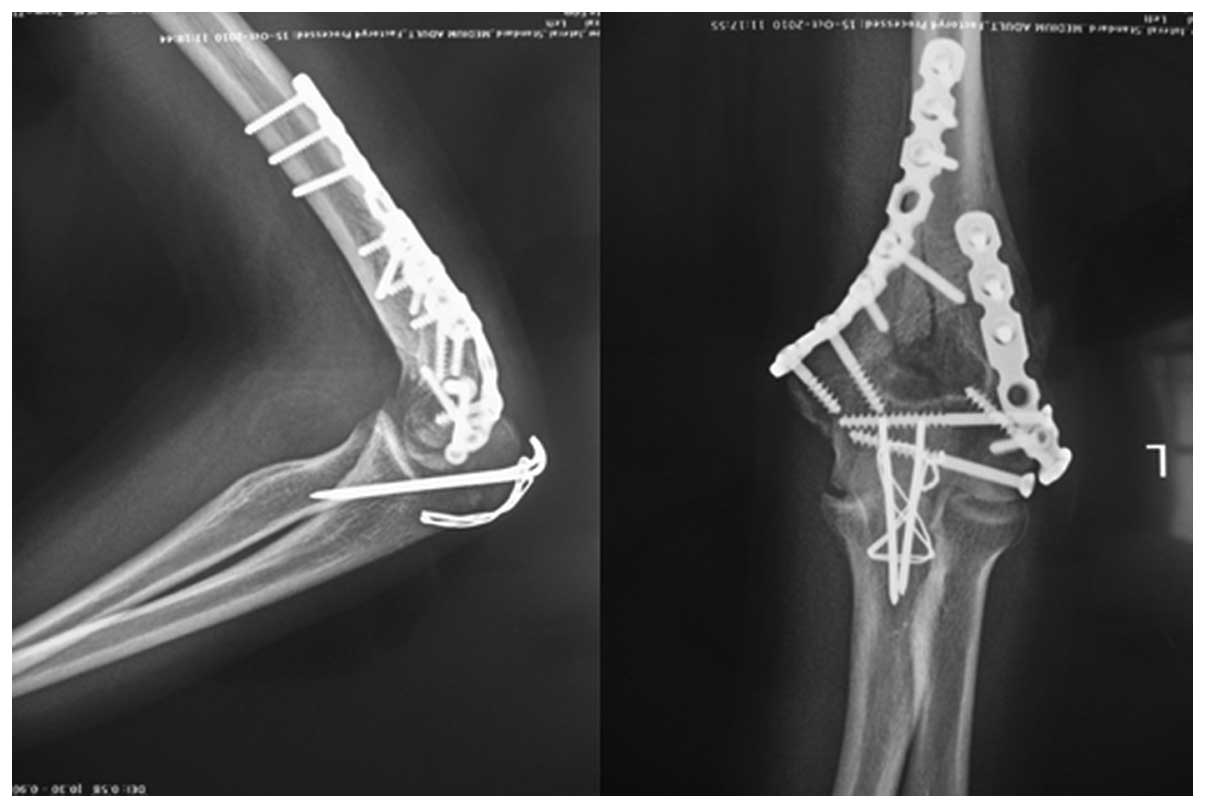
The 25 patients were randomly assigned to two groups
based on plate position. Thirteen patients were treated using two
orthogonal plates (group I): one plate was placed along the medial
supracondylar ridge and the other placed postero-laterally, with
the plates approximately perpendicular to each other (Fig. 1). Twelve patients were treated
using Y-shaped double-plating (group II): plates were placed in a Y
shape in the coronal plane, with the two plates on the medial and
lateral posterior surfaces of the distal humerus (Fig. 2).
Of the 25 patients, there were 15 males and 10
females (8 males in group I and 7 males in group II; Table I). The mean age at the time of
injury was 39.1±12.4 years (range, 19–55 years) in group I and
38.8±12.5 years (range, 18–56 years) in group II. The average time
between injury and internal fixation was 6.7±2.9 days in group I
and 7.4±2.7 days in group II. According to the AO/ASIF
classification system, two fractures were type C1, six type C2 and
the remaining five type C3 in group I. Three of the patients in
group I had compound injuries of Gustilo type 1 (one patient) or
type 2 (two patients) and three patients presented clinical signs
of ulnar nerve injury. Among the patients in group II, three were
type C1, five were type C2 and the remaining four were type C3. One
patient presented compound clinical signs of ulnar nerve injury. No
significant differences were observed in terms of demographic data
and operative procedures between the patients in the two groups.
This study was conducted in accordance with the Declaration of
Helsinki and with approval from the Ethics Committee of Qilu
Hospital Affiliated to Shandong University. Written informed
consent was obtained from all participants.
 | Table I.Patient demographics in the two
groups. |
Table I.
Patient demographics in the two
groups.
| Variable | Perpendicular plating
(group I, n=13) | Y-shaped plating
(group II, n=12) | P-value |
|---|
| Age (years) | 39±12.4 (19–55) | 38.8±12.5
(18–56) | 0.953 |
| Male : female | 8:5 | 7:5 | 1 |
| Right : left | 4:9 | 5:7 | 0.688 |
| Time to surgery
(days) | 6.7±2.9 (0–12) | 7.4±2.7 (5–14) | 0.539 |
| Fracture type
(AO) | C1, 2; C2, 6; C3,
5 | C1, 3; C2, 5; C3,
4 | 0.834 |
Pre-contoured anatomical plates and 3.5-mm
reconstruction plates were used in this study and all plates were
made of titanium. All but two of the patients underwent surgery
within 10 days of injury. The surgery of one patient with compound
injuries of Gustilo type 2 in group I was delayed until 14 days
after injury, and that of one patient in group II with compound
craniocerebral trauma was delayed until 12 days after injury. For
all patients, computed tomography (CT) was performed preoperatively
to identify comminution and to locate fracture fragments
accurately, in addition to the conventional two- plane
radiography.
All 25 patients included in this study followed the
same postoperative rehabilitation protocol. Early controlled
passive mobilization was started 48 h postoperatively after the
removal of the drainage and a long arm cast was placed with the
elbow in 80° flexion for 2 weeks during the interval of
mobilization. All patients received celecoxib postoperatively (200
mg every 12 h) for 2 weeks in order to prevent heterotopic
ossification and to ease pain. Clinical and radiological
evaluations were performed regularly at 3 days, 1 month, 3 months,
6 months and 1 year, then at 6-month intervals. Standard
anteroposterior and lateral radiographs were obtained to assess
fixation conditions and determine the incidences of nonunion, metal
failure and heterotopic ossification. Clinical evaluations
consisted of recording the incidences of complications and
determining Mayo Elbow Performance Scores (MEPS; Table II) (14).
 | Table II.Mayo Elbow Performance Score. |
Table II.
Mayo Elbow Performance Score.
| Function | Points | Definition
(points) |
|---|
| Pain | 45 | None (45) |
| | Mild (30) |
| | Moderate (15) |
| | Severe (0) |
| Motion | 20 | Arc >100°
(20) |
| | Arc 50–100° (15) |
| | Arc <50° (5) |
| Stability | 10 | Stable (10) |
| | Moderate instability
(5) |
| | Gross instability
(0) |
| Function | 25 | Comb hair (5) |
| | Feed (5) |
| | Perform hygiene
(5) |
| | Put on shirt (5) |
| | Put on shoe (5) |
| Total | 100 | |
Surgical procedures
All surgery was performed under general anesthesia.
With the patient in a supine position, a tourniquet was applied
high up on the arm and the shoulder and elbow were flexed 90°. A
straight posterior approach with slight radial deviation over the
olecranon was used; the ulnar nerve was routinely identified and
mobilized ≥6 cm proximal and distal to the cubital tunnel. Every
effort was made to avoid nerve injury during surgery and anterior
subcutaneous transposition of the ulnar nerve was usually performed
to prevent ulnar nerve tension or impingement over the plate
following surgery. Following blunt dissection of the triceps at the
medial and lateral intermuscular septum, medial visualization of
the olecranon joint was performed to identify the bare area. Prior
to osteotomy, two K-wire holes for refixation were drilled from the
olecranon tip to the ulna coracoid process and holes were drilled
in the ulna for subsequent tension band wiring. Using a thin
oscillating saw, a V-shaped olecranon osteotomy was created ∼2.5 cm
distal to the olecranon tip. The osteotomy was completed by
fracturing the last third of the ulna, creating an irregular
osteochondral fracture line for improved interdigitation and
facilitated reduction. Through a V-shaped olecranon osteotomy, the
distal humerus articular joint was exposed. With the articular
fragment of the distal block in view, the trochlea was reduced
first. Large fragments were fixed with transverse cannulated screws
and small fragments with 1-mm K-wires. Special attention was made
to restore the normal length and width of the trochlea for type C3
fractures. Then, the remaining fragments were reducted and K-wires
were passed for temporary fixation. Definitive fixation of the
articular fragments to the bone columns was based in the use of
strategically placed osteosynthesis, preserving as much soft-tissue
attachment to bone as possible. In group I, bone columns were
reduced and stabilized with two plates: usually a 3.5-mm
reconstruction plate or a pre-contoured anatomical plate placed
along the medial supracondylar ridge and another 3.5-mm
reconstruction plate or a pre-contoured anatomical plate in the
posterior aspect of the lateral column. Two plates were contoured
to fit the reduced distal humeral column during surgery. In group
II, two 3.5-mm reconstruction plates were applied on the medial and
lateral posterior surfaces of the distal humerus, in a Y shape in
the coronal plane. Fracture lines in the coronal plane and small
articular fragments were stabilized using 2.7-mm cannulated screws.
Following definitive fixation, all K-wires were removed as far as
possible. The olecranon osteotomy was fixed at the end with two
K-wires and tension band wiring in all cases.
Statistical analysis
Statistical analyses were performed with Statistical
Package for Social Science (SPSS version 16.0; SPSS, Inc., Chicago,
IL, USA). All continuous variable values are expressed as mean ±
standard deviation (SD). A two-sample t-test was used for
continuous variables (range of motion, flexion, extension, MEPS,
age and time to surgery) and Fisher’s exact test for dichotomous
variables to compare demographic data (rate of excellent and good
MEPS, fracture type, male to female ratio and right to left ratio).
The level of statistical significance was defined as P=0.05.
Results
All patients were followed up for 12 to 38 months
with an average of 19.2±7.1 months in group I and 18.3±4.0 months
in group II. All the osteotomies and fractures healed
radiographically without a step-off at the articular margin >2
mm or an angular deformity >10° at the last follow-up. Nineteen
screws were used in group I and 22 in group II. No complications
associated with the olecranon osteotomies were encountered. The
majority of patients achieved bony union at 6 months (fourth
radiological evaluation) postoperatively and only one patient had
delayed bony union until 8 months after surgery in group II. No
screw loosening, plate breakage or deep infection was observed.
Mild occasional pain was reported by six patients in group I and
five in group II, and none of the patients in either group reported
severe or constant pain.
The arc of motion averaged 106.2±22.0°
postoperatively with a mean elbow flexion of 120.8±12.6° (range,
100–135°) and extension of 14.6±10.5° (range 0–40°) in group I
(Table III). In group II, the arc
of motion was 105.0±21.7° with a mean elbow flexion of 119.6±13.6°
(range, 95–135°) and extension of 14.6±10.8° (range 0–40°)
postoperatively. The average MEPS was 89.6±11.8° (range, 70–100°)
in group I and 90.0±12.3° (range, 70–100°) in group II. According
to MEPS, 84.6% of patients in group I and 83.3% in group II had
excellent or good scores. No statistically significant inter-group
differences were evident in terms of clinical outcomes.
 | Table III.Clinical comparison between two
different plating methods. |
Table III.
Clinical comparison between two
different plating methods.
| Variable | Perpendicular plating
(group I) | Y-shaped plating
(group II) | P-value |
|---|
| Range of motion
(°) | 106.2±22.0 | 105.0±21.7 | 0.892 |
| Flexion (°) | 120.8±12.6
(100–135) | 119.6±13.6
(95–135) | 0.821 |
| Extension (°) | 14.6±10.5 (0–40) | 14.6±10.8 (0–40) | 1.00 |
| MEPS (°) | 89.6±11.8
(70–100) | 90.0±12.3
(70–100) | 0.935 |
| Rate of excellent and
good scores (%) | 84.6 | 83.3 | 1.00 |
Complications developed in four patients in group I
and three patients in group II. According to the scale of Knirk and
Jupiter (15) for the assessment
of post-traumatic arthritis, two elbows in group I and one in group
II were grade 1. One patient in group II (a 22-year-old male with a
C3 fracture) who had grade I heterotopic ossification, per the
Hastings and Graham classification (16), presented no functional impairment.
Transient ulnar nerve neuropathy developed in one patient in group
I (a 32-year-old male with a C3 fracture). Ulnar nerve symptoms in
all patients, including four patients suffering from the symptoms
preoperatively, had subsided completely 6 months after surgery. Two
patients had an unfavourable arc of motion (60 and 65°) in the
final follow-up. One patient in group I (a 50-year-old female with
a C3 fracture) was mentally handicapped and one patient in group II
(a 56-year-old female with a C3 fracture) had surgical neck
fractures of the humerus.
Discussion
The aim of treatment for distal humerus fractures is
to make the elbow stable and painless with satisfactory function.
This requires anatomic reconstruction of the articular surface,
restitution of the overall geometry of the distal humerus and
stable fixation of the fracture fragments to allow early and full
rehabilitation. Although these goals are now widely accepted by the
orthopedic community (8,11,12,17,18),
they may be technically difficult to achieve, particularly in the
presence of substantial comminution.
Within the last several years, a two-column theory
of the anatomy of the distal humerus has been advocated whereby the
coronal plane of the distal humerus is considered to be in the
shape of a triangle, with the coronoid fossa and olecranon fossa
accounting for the majority of the central area and the medial and
lateral condyles forming two strong columns by proximal extension
(8,19). Fixation of the distal humerus must
not only restore the capitulum-trochlea joint, but also the
integrity of the medial and lateral columns. Despite controversies
concerning the appropriate treatment of distal humerus fractures,
double-plate fixation has been widely reported to produce
satisfactory clinical outcomes, even in patients with complex
intra-articular fractures (7,20). A
number of studies have compared the clinical outcomes of parallel
and perpendicular plating systems for distal humerus fractures
(12,21). Additionally, another study reported
the clinical outcomes of perpendicular or Y-shaped double-plating
systems for distal humerus fractures (22). Fewer studies have compared the
clinical outcomes of the perpendicular and Y-shaped double-plating
systems for distal humerus fractures. In the present study, we
compared the clinical outcomes of the perpendicular and Y-shaped
double-plating methods when applied to type C distal humerus
fractures in young adults. Postoperative analyses revealed no
significant differences between the two plating modalities in terms
of arc of flexion, function, rate of excellent and good MEPS and
other clinical results. No screw loosening or plate breakage was
observed in any of our patients during the follow-up. Zero
incidence of fixation loss indicates that the two methods of
placing plates result in an equally stable fixation. The following
two points are important: i) the anatomic reconstruction of the
intercondylar fractures and use of transverse cannulated screws
allows improvement of the fracture from type C to type A; and ii)
the plate should be made to fit the shape of the distal humerus and
the screws should be tightened one at a time, as far as
possible.
Postoperative complication rates of up to 48% have
been reported for type C distal humerus fractures (19,23,24).
In the present study, one patient in group II suffered from
transient ulnar nerve palsy following internal fixation of the
distal humerus fracture; however, no patients suffered permanent
nerve dysfunction. This may be attributed to anterior transposition
of the ulnar nerve. The reported prevalence of heterotopic
ossification following surgical treatment of distal humerus
fractures ranges from 4 to 49%, although no functional deficit was
involved in the majority of cases (25). In the present study, one patient
with heterotopic ossification was encountered in group II. This low
incidence (4%) of heterotopic ossification may be attributed to the
routine use of celecoxib postoperatively. Therefore, we suggest
that patients take a nonsteroidal drug routinely.
Reported total ranges of elbow motion vary from 103
to 112° following the double-plating fixation of type C distal
humerus fractures, regardless of the plate position (5,26).
In the present study, 21 of 25 patients (84%) obtained good or
excellent functional results with a mean range of elbow motion of
105.6±21.4° following double-plate fixation. No significant
difference was observed in the total range of elbow motion between
the two groups. Two patients suffered from an unfavourable arc of
motion (60 and 65°) in the final follow-up. The reason for this was
that the patients were unable to cooperate with exercise and
physical therapy postoperatively. Early and painless functional
exercise postoperatively is key to obtaining a good range of elbow
motion. However, there is a contradiction between immobility and
early functional exercise. All the patients in the two groups were
young adults with no osteoporotic bone. Stable fixation was
achieved during surgery in all patients and early functional
exercise was allowed postoperatively. We advise the initiation of
passive exercise after removal of the drainage tube, with the
forearm gravity driving the elbow joint to a continuous passive
stretch to maximum activity and the other hand supporting the
buckling to maximum activity. The exercise was performed for two
periods a day after half an hour of taking celecoxib for 20–30 min
per period. Plaster immobilization was used during the intervals of
exercise in the first weeks, then exercise intensity was increased
and a triangular bandage was used during the intervals of exercise.
The ideal state may be achieved at ∼6 weeks. The method was simple
with a slow and gentle action, causing only light pain and avoiding
further injury of the soft tissue and myositis ossificans by
violent passive flexion and stretching of the elbow joint.
The limitations of this study included a relatively
small number of patients for determination of clinical superiority
related to plate position and a lack of comparison of clinical
outcomes according to plate position using locking and unlocking
plates.
From a clinical perspective, no significant
differences were observed between the perpendicular and Y-shaped
double-plating methods for distal humerus fractures in terms of
clinical outcomes and complication rates. If appropriately applied
with suitable plates, the perpendicular and Y-shaped double-plating
methods provide adequate stability and anatomic reconstruction of
intercondylar fractures of young adult humeri.
References
|
1.
|
Cannada L, Loeffler B, Zadnik MB and
Eglseder AW: Treatment of high-energy supracondylar/intercondylar
fractures of the distal humerus. J Surg Orthop Adv. 20:230–235.
2011.PubMed/NCBI
|
|
2.
|
Schmidt-Horlohé K, Wilde P, Bonk A, Becker
L and Hoffmann R: One-third tubular-hook-plate osteosynthesis for
olecranon osteotomies in distal humerus type-C fractures: a
preliminary report of results and complications. Injury.
43:295–300. 2012.PubMed/NCBI
|
|
3.
|
Coles CP, Barei DP, Nork SE, Taitsman LA,
Hanel DP and Bradford Henley M: The olecranon osteotomy: a six-year
experience in the treatment of intraarticular fractures of the
distal humerus. J Orthop Trauma. 20:164–171. 2006.PubMed/NCBI
|
|
4.
|
Chen G, Liao Q, Luo W, Li K, Zhao Y and
Zhong D: Triceps-sparing versus olecranon osteotomy for ORIF:
analysis of 67 cases of intercondylar fractures of the distal
humerus. Injury. 42:366–370. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Doornberg JN, van Duijn PJ, Linzel D, et
al: Surgical treatment of intra-articular fractures of the distal
part of the humerus. Functional outcome after twelve to thirty
years. J Bone Joint Surg Am. 89:1524–1532. 2007.PubMed/NCBI
|
|
6.
|
Luegmair M, Timofiey E and Chirpaz-Cerbat
JM: Surgical treatment of AO type C distal humeral fractures:
internal fixation with a Y-shaped reconstruction (Lambda) plate. J
Shoulder Elbow Surg. 17:113–120. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Sanchez-Sotelo J, Torchia ME and
O’Driscoll SW: Complex distal humeral fractures: internal fixation
with a principle-based parallel-plate technique. J Bone Joint Surg
Am. 89:961–969. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Li SH, Li ZH, Cai ZD, et al: Bilateral
plate fixation for type C distal humerus fractures: experience at a
single institution. Int Orthop. 35:433–438. 2011. View Article : Google Scholar
|
|
9.
|
Doğramaci Y, Esen E, Kürklü M, Lirici Y,
Atahan AO and Kömürcü M: Double plate osteosynthesis provides
better biomechanical stabilization than double tension band
technique in distal humerus fractures. Eklem Hastalik Cerrahisi.
21:44–49. 2010.PubMed/NCBI
|
|
10.
|
Schwartz A, Oka R, Odell T and Mahar A:
Biomechanical comparison of two different periarticular plating
systems for stabilization of complex distal humerus fractures. Clin
Biomech (Bristol, Avon). 21:950–955. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Penzkofer R, Hungerer S, Wipf F, von
Oldenburg G and Augat P: Anatomical plate configuration affects
mechanical performance in distal humerus fractures. Clin Biomech
(Bristol, Avon). 25:972–978. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Shin SJ, Sohn HS and Do NH: A clinical
comparison of two different double plating methods for
intraarticular distal humerus fractures. J Shoulder Elbow Surg.
19:2–9. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Müller ME, Nazarian S, Koch P and
Schatzker J: The Comprehensive Classification of Fractures of Long
Bones. 1st edition. Springer-Verlag; Berlin: 1990
|
|
14.
|
Jupiter JB and Morrey BF: Fractures of the
distal humerus in the adult. The Elbow and its Disorders. Morrey
BF: 2nd edition. WB Saunders; Philadelphia: pp. 328–366. 1993
|
|
15.
|
Knirk JL and Jupiter JB: Intra-articular
fractures of the distal end of the radius in young adults. J Bone
Joint Surg Am. 68:647–659. 1986.
|
|
16.
|
Hastings H II and Graham TJ: The
classification and treatment of heterotopic ossification about the
elbow and forearm. Hand Clin. 10:417–437. 1994.PubMed/NCBI
|
|
17.
|
Jeong BO and Lee DK: Treatment for type C
fractures of the distal humerus with the LCP distal humerus system.
Eur J Orthop Surg Traumatol. 22:565–569. 2012. View Article : Google Scholar
|
|
18.
|
Kamrani RS, Mehrpour SR, Aghamirsalim MR,
et al: Pin and plate fixation in complex distal humerus fractures:
surgical technique and results. Int Orthop. 36:839–844. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Reising K, Hauschild O, Strohm PC and
Suedkamp NP: Stabilisation of articular fractures of the distal
humerus: early experience with a novel perpendicular plate system.
Injury. 40:611–617. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Celli A, Donini MT and Minervini C: The
use of pre-contoured plates in the treatment of C2-C3 fractures of
the distal humerus: clinical experience. Chir Organi Mov. 91:57–64.
2008. View Article : Google Scholar
|
|
21.
|
Arnander MW, Reeves A, MacLeod IA, Pinto
TM and Khaleel A: A biomechanical comparison of plate configuration
in distal humerus fractures. J Orthop Trauma. 22:332–336. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Gupta R and Khanchandani P: Intercondylar
fracture of the distal humerus in adults: a critical analysis of 55
cases. Injury. 33:511–515. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Gofton WT, Macdermid JC, Patterson SD,
Faber KJ and King GJ: Functional outcome of AO type C distal
humeral fractures. J Hand Surg Am. 28:294–308. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Lim R, Tay SC and Yam A: Radial nerve
injury during double plating of a displaced intercondylar fracture.
J Hand Surg Am. 37:669–672. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Douglas K, Cannada LK, Archer KR, Dean DB,
Lee S and Obremskey W: Incidence and risk factors of heterotopic
ossification following major elbow trauma. Orthopedics. 35:815–822.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Aslam N and Willett K: Functional outcome
following internal fixation of intraarticular fractures of the
distal humerus (AO type C). Acta Orthop Belg. 70:118–122.
2004.PubMed/NCBI
|