Introduction
Primary immunodeficiencies are disorders in which
part of the body’s immune system is missing or does not function
correctly. Most primary immunodeficiencies are genetic disorders
and the majority are diagnosed in children under the age of one,
although milder forms may not be recognized until adulthood
(1). The diagnostic criteria for
primary immunodeficiencies were established in 1999 and distinguish
between ‘definitive’, ‘probable’ and ‘possible’ in the diagnosis of
primary immunodeficiency. A ‘definitive’ diagnosis is made when the
patient has a >98% chance of the same diagnosis being made in
the following 20 years; this level of diagnosis is achievable with
the detection of a genetic mutation or very specific circumstantial
abnormalities. A ‘probable’ diagnosis is made when a genetic
diagnosis is not applicable, although the patient has all the other
characteristics of a particular disease; the chance of the same
diagnosis being made 20 years later is estimated to be 85–97%. A
‘possible’ diagnosis is made when the patient exhibits some of the
characteristics of a disease, but not all (2). The treatment of primary
immunodeficiency depends foremost on the nature of the abnormality.
This may range from immunoglobulin replacement therapy in antibody
deficiencies, in the form of intravenous immunoglobulin (IVIG), to
hematopoietic stem cell transplantation for severe immunodeficiency
(3). In the current study, we
describe the case of a successful diagnosis of primary
immunodeficiency and the treatment of the patient with
prednisone.
Case report
A 23-year-old male was admitted to the Second
Affiliated Hospital of Nanjing Medical University (Nanjing, China),
complaining of chronic diarrhea. The patient had suffered from
chronic diarrhea without blood or mucus for almost two years. The
diarrhea took the form of unshaped, liquid stools and occurred two
to four times a day. The patient had lost ∼8 kg in weight, despite
having a healthy appetite, and had received long-term treatment in
other university hospitals, based on the diagnosis of
protein-losing gastroenteropathy. Following the transferral of the
patient to the Second Affiliated Hospital of Nanjing Medical
University, apparent edema was observed in the lower limbs, in
addition to a medium volume of ascites. Routine laboratory tests
revealed that the counts of white blood cells (including accurate
lymphocyte and granulocyte counts), hemoglobin and platelets were
generally normal. The erythrocyte sedimentation rate was 21 mm/h
and the C-reactive protein level was 1 mg/l. The values for liver
enzymes, urea nitrogen, creatinine, glucose and electrolytes were
normal. The total protein level in the serum was 33 g/l, with 15
g/l albumin and 18 g/l globulin. Thyroid function [reverse
triiodothyronine (rT3), reverse tetraiodothyronine (rT4), total T3
(TT3), total T4 (TT4) and thyroid-stimulating hormone (TSH)] and
coagulation tests were normal and the standard autoantibody screen
[antinuclear antibodies (ANA), anti-double-stranded DNA
(anti-dsDNA) and antineutrophil cytoplasmic antibodies (ANCA)] was
negative. The levels of immunoglobulin (Ig) G, IgM and IgA were
7.32, 0.28 and 1.55 g/l, respectively, and urinalysis and 24
h-urine protein measurements were normal. The microbiological test
results excluded certain viral infections (hepatitis B and C and
HIV), while repeated stool cultures, parasites and ova, and occult
blood in the stool were all normal. The size of the liver was
normal, while the spleen appeared marginally enlarged when examined
using ultrasound. A chest radiograph and abdomino-pelvic computed
tomography (CT) scan did not reveal anything of note. In order to
investigate the cause of the gastrointestinal symptoms, an upper
gastrointestinal endoscopy, colonoscopy and double-balloon
enteroscopy were performed. Biopsy specimens revealed villus
blunting and flattening/atrophy in the duodenum, while nodular
lymphoid hyperplasia and villus blunting and flattening/atrophy
were observed in the ileum.
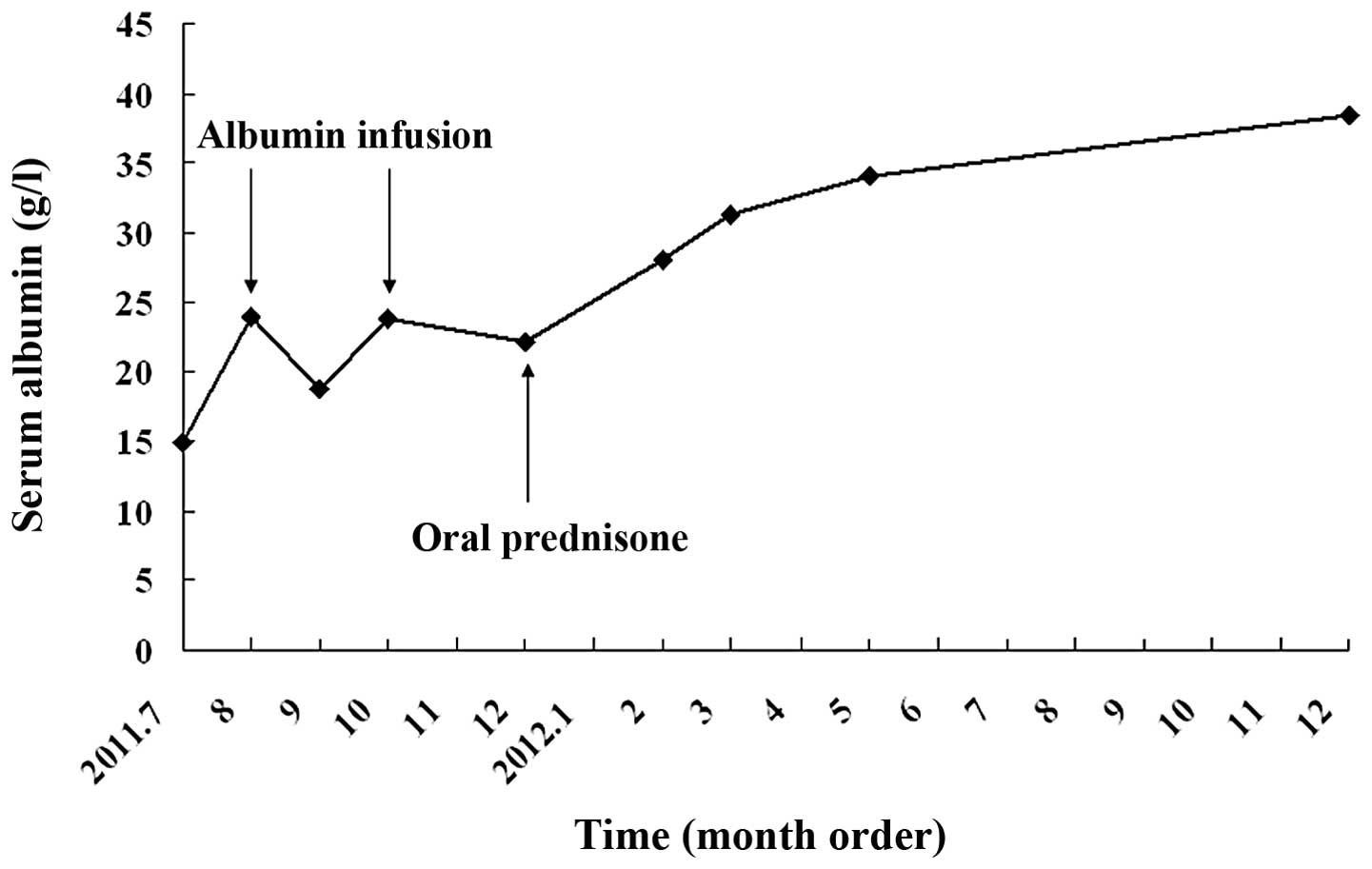
According to these clinical and laboratory findings,
the patient was diagnosed with possible primary immunodeficiency
due to IgM deficiency. Considering the patient’s low serum albumin
level, albumin infusion therapy was prescribed. Following this, it
was decided to initiate treatment with 30 mg/day oral prednisone
for one month, prior to weekly tapering by 5 mg until withdrawal.
This led to a progressive clinical improvement. In addition, the
patient was supplied with calcium, zinc and vitamin supplements.
Three months later, the patient was producing 1 or 2 stools/day,
had gained ∼10 kg in body weight and was not observed to have any
edema of the limbs. During the subsequent nine months follow-up,
the patient was able to work without suffering any effects from the
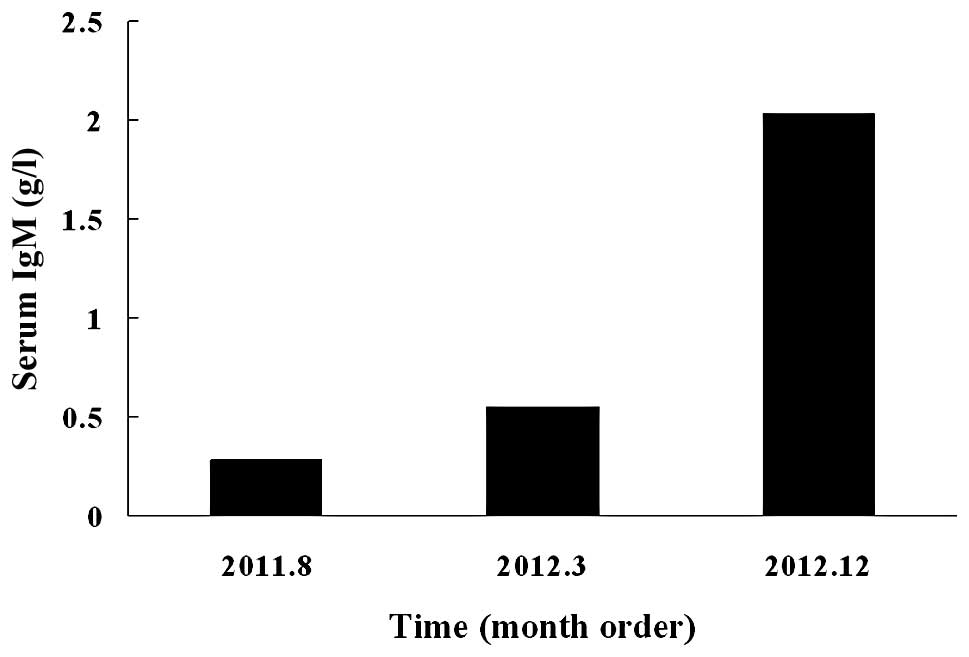
illness. A significant increase in the patient’s serum albumin
level was observed following the prednisone treatment (Fig. 1) and the serum IgM level also
returned to normal (Fig. 2). This
study was approved by the Ethics Committee of Nanjing Medical
University. Written informed consent was obtained from the
patient.
Discussion
A survey of 10,000 American households revealed that
the prevalence of diagnosed primary immunodeficiency approaches
1:1,200 (4). This figure does not
take into account individuals with mild immune system defects who
have not received a formal diagnosis. Milder forms of primary
immunodeficiency, such as selective IgA deficiency, are fairly
common, with random groups of individuals (such as otherwise
healthy blood donors) exhibiting a rate of 1:600. Other disorders
are distinctly more uncommon, with incidences between 1:100,000 and
1:2,000,000 (1). Since the
diseases are particularly rare in Asia, the incidence rate in Asia
is much lower than that in America and Europe. There may be a
requirement for gastroenterologists in Asian countries to obtain a
greater recognition of this disease.
IgM deficiency, which is not very frequently
encountered, may be classified as one of the primary
immunodeficiency diseases. The prevalence of gastrointestinal
disorders in patients with primary immunodeficiency diseases ranges
from 5 to 50% (5,6). Gastrointestinal disorders
(particularly diarrhea and malabsorption) may be the most prominent
or the sole complaints in certain patients (7,8).
Common variable immunodeficiency (CVID) is the most
frequently-encountered primary immunodeficiency (9). The IgG concentrations in CVID are at
least two standard deviations below the mean for the age of the
patient and, in the majority of cases, are accompanied by low
concentrations or an absence of IgA, IgM or the two combined.
Patients with CVID typically present with atypical inflammatory
gastrointestinal disease, resulting in diarrhea, malabsorption and
weight loss (10). Nodular
lymphoid hyperplasia and loss of villi are frequently observed in
the biopsies of patients with CVID. It has been revealed that up to
60% of patients with untreated CVID develop diarrhea, with 10%
developing idiopathic malabsorption with weight loss (11). The mainstay treatment is
replacement therapy with IVIG (12–15),
and this reduces the number of bacterial infections (16) and most likely enhances survival
(17). However, the immunoglobulin
therapy has little effect on gastrointestinal symptoms.
In the present case, diarrhea, malabsorption and
weight loss were the main clinical manifestations. Furthermore, the
patient’s serum albumin level was too low, resulting in edema in
the lower limbs. The absorption of albumin may be associated with
villus blunting and flattening/atrophy in the small intestine.
According to the clinical features and laboratory tests, the
patient was diagnosed with primary immunodeficiency, a CVID-like
disorder, due to the presence of low IgM with normal IgG levels.
Thus, selective IgM deficiency was apparent in this case, for which
the common treatment is IVIG. However, IVIG is reported to have
little effect on gastrointestinal symptoms (7). Despite the fact that the patient had
normal IgG levels and was undergoing intravenous replacement
therapy every 3 weeks, the diarrhea continued (18). It has been demonstrated that
corticosteroid therapy improves diarrhea in patients with CVID
through the inhibition of the immune inflammatory response
(8). In the present case, oral
prednisone was used. The initial dose was 30 mg/day for one month,
and this was then tapered weekly by 5 mg until withdrawal.
Following the prednisone therapy, the patient’s symptoms
dramatically improved. However, it must be noted that it was
necessary to consider and treat the potential side-effects during
long-term treatment with corticosteroids. The further follow-up
confirmed the diagnosis and the success of the treatments.
Although the majority of patients with primary
immunodeficiency are able to obtain a good efficacy in the
short-term following treatment, relapse is common. Further
investigations into the etiology of the disease and novel
treatments are required. Interestingly, the recent emerging
application of fecal microbiota transplantation has shown its
promising value as a simple treatment for primary immunodeficiency
with intestinal symptoms and other refractory intestinal diseases,
since previous studies highlighted these aspects (19,20).
However, further clinical studies with more samples are
required.
In conclusion, the diagnosis, treatment and
follow-up of the present case provided increased clinical
experience and recognition of patients with primary
immunodeficiency, particularly in patients from Asia.
Acknowledgements
The study was partially supported by a
grant from the National Natural Science Foundation of China (grant
no. 30900667).
References
|
1.
|
Lim MS and Elenitoba-Johnson KS: The
molecular pathology of primary immunodeficiencies. J Mol Diagn.
6:59–83. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Conley ME, Notarangelo LD and Etzioni A;
Representing PAGID (Pan-American Group for Immunodeficiency) and
ESID (European Society for Immunodeficiencies): Diagnostic criteria
for primary immunodeficiencies. Clin Immunol. 93:190–197. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Porta F, Forino C, De Martiis D, et al:
Stem cell transplantation for primary immunodeficiencies. Bone
Marrow Transplant. 41(Suppl 2): S83–S86. 2008. View Article : Google Scholar
|
|
4.
|
Boyle JM and Buckley RH: Population
prevalence of diagnosed primary immunodeficiency diseases in the
United States. J Clin Immunol. 27:497–502. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Wood P, Stanworth S, Burton J, et al:
Recognition, clinical diagnosis and management of patients with
primary antibody deficiencies: a systematic review. Clin Exp
Immunol. 149:410–423. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Lai Ping So A and Mayer L:
Gastrointestinal manifestations of primary immunodeficiency
disorders. Semin Gastrointest Dis. 8:22–32. 1997.PubMed/NCBI
|
|
7.
|
Kobrynski LJ and Mayer L: Diagnosis and
treatment of primary immunodeficiency disease in patients with
gastrointestinal symptoms. Clin Immunol. 139:238–248. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Elnachef N, McMorris M and Chey WD:
Successful treatment of common variable immunodeficiency
disorder-associated diarrhea with budesonide: a case report. Am J
Gastroenterol. 102:1322–1325. 2007. View Article : Google Scholar
|
|
9.
|
Park MA, Li JT, Hagan JB, et al: Common
variable immunodeficiency: a new look at an old disease. Lancet.
372:489–502. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Washington K, Stenzel TT, Buckley RH and
Gottfried MR: Gastrointestinal pathology in patients with common
variable immunodeficiency and X-linked agammaglobulinemia. Am J
Surg Pathol. 20:1240–1252. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Sneller MC: Common variable
immunodeficiency. Am J Med Sci. 321:42–48. 2001. View Article : Google Scholar
|
|
12.
|
Ammann AJ, Ashman RF, Buckley RH, et al:
Use of intravenous gamma-globulin in antibody immunodeficiency:
results of a multicenter controlled trial. Clin Immunol
Immunopathol. 22:60–67. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Pirofsky B: Intravenous immune globulin
therapy in hypogammaglobulinemia. A review. Am J Med. 76:53–60.
1984. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Cunningham-Rundles C, Siegal FP, Smithwick
EM, et al: Efficacy of intravenous immunoglobulin in primary
humoral immunodeficiency disease. Ann Intern Med. 101:435–439.
1984. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Orange JS, Hossny EM, Weiler CR, et al:
Use of intravenous immunoglobulin in human disease: a review of
evidence by members of the Primary Immunodeficiency Committee of
the American Academy of Allergy, Asthma and Immunology. J Allergy
Clin Immunol. 117(Suppl): S525–S553. 2006. View Article : Google Scholar
|
|
16.
|
Lucas M, Lee M, Lortan J, et al: Infection
outcomes in patients with common variable immunodeficiency
disorders: relationship to immunoglobulin therapy over 22 years. J
Allergy Clin Immunol. 125:1354–1360. 2010.PubMed/NCBI
|
|
17.
|
Hermaszewski RA and Webster AD: Primary
hypogammaglobulinaemia: a survey of clinical manifestations and
complications. Q J Med. 86:31–42. 1993.PubMed/NCBI
|
|
18.
|
Kalha I and Sellin JH: Common variable
immunodeficiency and the gastrointestinal tract. Curr Gastroenterol
Rep. 6:377–383. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Zhang F, Luo W, Shi Y, et al: Should we
standardize the 1,700-year-old fecal microbiota transplantation? Am
J Gastroenterol. 107:17552012.PubMed/NCBI
|
|
20.
|
Borody TJ and Khoruts A: Fecal microbiota
transplantation and emerging applications. Nat Rev Gastroenterol
Hepatol. 9:88–96. 2012. View Article : Google Scholar : PubMed/NCBI
|