Introduction
Acupuncture has been performed in Korea for
thousands of years and is still actively practiced in clinics
today. In particular, acupuncture is known to be useful due to its
pain relieving effects; however, at present, it is also studied and
used for the treatment of broader symptoms, such as urinary
incontinence. Urinary incontinence is a common condition, affecting
~25% of premenopausal and 40% of postmenopausal women. While it may
not be a critical problem, it reduces the quality of life; however,
only approximately one in four women with urinary incontinence
consult a doctor about their condition (1).
Stress and urge incontinence are the two most common
types of urinary incontinence, and mixed incontinence, which is a
combination of the two, is also prevalent. Stress incontinence
occurs when the bladder pressure exceeds urethral resistance as a
result of an increased abdominal pressure, for example due to
sneezing or coughing (2). Stress
incontinence is defined as an involuntary leakage when the
abdominal pressure increases, whereas urge incontinence occurs as a
result of uncontrolled abnormal detrusor contractions that exceed
the urethral pressure (2). The
etiology of the urinary urgency that causes urge incontinence has
not yet been fully elucidated, although some peripheral nerves, as
well as the central nervous system, may be involved in muscle
hypersensitivity and the reduced effectiveness of smooth muscle
relaxation (3).
Acupuncture was initially described as a successful
treatment for certain overactive bladder symptoms in the 1980s
(4,5), and, since then, a number of clinical
trials on incontinence have been carried out (6–8).
There have been numerous clinical trials and some randomized
controlled trials (RCTs) on urinary incontinence due to bladder
instability or stress incontinence; however, the results are
limited and there have been no systematic reviews to date.
The acupoints used in the studies were selected
based on Korean Medicine theory, and their mechanism may be
understood with reference to the autonomic and somatic nerve
innervations to the bladder. Certain studies have indicated that
acupuncture may influence the autonomic nerve system (9). There has not been sufficient
consideration of the depth of the acupuncture insertion into the
body in previous studies, and, therefore, this review aimed to
provide information as to why insertion depth is necessary as a
differential factor.
In this review, we examined the efficacy of
acupuncture with regard to urinary incontinence, and assessed the
levels of the autonomic efferent and afferent pathways and the
depth of the needle insertion in the acupuncture.
There is a complex rationale behind the choice of
acupuncture points for incontinence. The muscles controlling
micturition are controlled by the autonomic and somatic nervous
system. The detrusor muscle is relaxed by sympathetic stimulation
that originates from the lumbar spinal cord T11-L2 region, and
contracted by parasympathetic stimulation from the sacral spinal
cord S2-4 region. The external urethral sphincter is under somatic
control (10). Therefore, the
coordination of the autonomic and somatic nerves to the bladder and
urethra is important not only in micturition, but also in
incontinence.
The points that are most commonly used in
acupuncture are BL31, BL32 and BL33, which are located above the
first, second and third sacral foramina, which lie over the first,
second and third sacral nerve roots, respectively. These points are
frequently used, due to the fact that they correspond with the
segmental innervation of the parasympathetic nerve supply to the
bladder.
The acupuncture points that are known to affect the
micturition center and parasympathetic innervation to the urinary
system include BL23, BL28 and several points on one of the eight
extra meridians in the lower abdomen (11). BL23 is located at the L2 level,
BL28 is located paravertebrally from the second sacral foramina and
points three, four and six on the CV are located in between the
pubic and the umbilical cord.
In Korean Medicine, acupoints SP6, ST36 and KI3,
located on the legs, are also considered to assist bladder function
by invigorating energy. Furthermore, these acupoints on the legs
correspond to the skin dermatomes from L4-S2 innervation, which
means that stimulation of these points may influence bladder
function. Similarly, points three, four and six on the CV
correspond to the skin dermatomes from T11-L1.
Since the afferent and efferent innervations of the
bladder are affected by the sympathetic nerves originating at
T11-L2, as well as the parasympathetic and somatic nerves
originating at S2-4, these acupoints appear to be strongly
organized segmentally.
In the majority of the remaining studies on bladder
dysfunction, the stimulation points (not restricted to acupuncture)
were selected in accordance with the segmental innervation of the
nerves. Electrical nerve stimulation (TENS) applied over the pubic
area, which pertains to the sacral dermatome, has exhibited certain
positive effects (12), while
other animal studies have also demonstrated that stimulation on the
perineal area affects the bladder and sphincter function (13).
The locations of BL31, BL32 and BL33 correspond with
the origin of the somatic fibers of the pudendal nerve, which
provide excitatory innervation to the pelvic floor muscles and the
sphincter so that they are able to remain in a contracted state. A
previous study has described the beneficial effects of
transcutaneous stimulation of the pupendal nerve on incontinence
(14). The authors hypothesized
that sacral nerve stimulation depended on the stimulation of
afferent axons (which was by electrical stimulation in this
particular study) in the spinal roots, and that this led to the
modulation of the voiding and continence reflex pathways in the
central nervous system (14).
The acupoint ST36 is predominantly used in the
treatment of gastrointestinal symptoms, although it may also be
used for urinary disorders. In a study investigating the ST36
acupoint, functional magnetic resonance imaging (fMRI) results
indicated activation in the hypothalamus and bilateral prefrontal
cortex, suggesting that acupoint ST36 activated the neural
brainstem-thalamus-cortex reticular system and increased the
neurotransmitter concentrations (15). It is for this reason that
acupuncture has been proposed to affect micturition through the
descending serotonergic system. At present, there are numerous
experimental and clinical data supporting the theory that the
serotonergic input facilitates glutamate-induced activation of the
pudendal nerve, and thereby helps to maintain the external urethral
sphincter in a closed state (8).
However, there are also physiological similarities between muscle
training and acupuncture, and there have been suggestions that
acupuncture may be regarded as an artificial method of muscle
training (16).
With regard to the insertion depth of the
acupuncture needles, it has been observed that the majority of the
studies concerning acupuncture have focused on the efficacy of the
acupoint itself. Although electroacupuncture is frequently studied,
there has been little investigation surrounding the insertion depth
or the thickness of the acupuncture needle. The area of acupuncture
that is predominantly focused upon is its analgesic effect on pain,
and therefore most of the studies or trials concerning the depth of
acupuncture have been restricted to its pain relieving effects
(17,18). However, even in consideration of
these studies, an appropriate penetration depth of the acupuncture
needle has not been suggested. In patients with lower back pain, it
has been observed that deep insertion into the muscle produced
greater efficacy than shallow insertion (19). Furthermore, it has been
demonstrated that, with regard to analgesic effects, the insertion
of acupuncture needles into the muscles affects the nociceptors,
while insertion purely into the skin does not (20). Therefore, it has been indicated
that acupuncture may have different effects, according to insertion
depth; however, as of yet, there is no standard regarding the depth
of insertion.
While there have been relatively few clinical trials
concerning incontinence that have considered the insertion depth of
the acupuncture, those trials that have mentioned the depth of
insertion lack consistency, as well as an explanation regarding the
reason for changing the depth of insertion (8,21,22).
For the purpose of skin dermatome stimulation, the
acupuncture needle has to be inserted shallowly, so that it only
penetrates the skin. With regard to urinary dysfunction, the
acupoints on the limbs are associated with the skin dermatomes from
the spinal innervation that influence bladder function, as are the
acupoints on the lower abdomen (CV 3, 4 and 6). Therefore, when
acupuncture is applied to these acupoints, in order to influence
bladder function, it is necessary for the depth of insertion to be
no deeper than the skin. However, if the purpose is to stimulate
the muscle or nerve, a deeper insertion is required. Therefore, it
is necessary for the needles at the acupoints on the spinal part of
the BL meridian to be inserted deeper than those at other BL
points. In addition, it is necessary that the application of
acupuncture to strengthen the muscle that assists the act of
urination has a penetration that is sufficiently deep for the
muscle to be reached.
Therefore, aside from the acupuncture point itself,
there is a requirement for the insertion depth of the acupuncture
needle to differ according to the intention of the stimulation.
Materials and methods
Data sources
The following sources were researched up to August
2012: Korean electronic databases (which included KISS, JISTI,
DBPIA and the Korean Traditional Knowledge Portal), MedLine, The
Cochrane Library and the Cumulative Index to Nursing and Allied
Health Literature (CINAHL).
The key words used in the search for RCTs were
‘acupuncture’ AND ‘bladder’ OR ‘incontinence’ OR ‘overactive’ OR
‘urgency’ OR ‘urinary’. In Korean, Acupuncure AND (‘Urinary
incontinence’ OR ‘Bladder’) were used. Each database was manually
searched, independently.
Study selection
Types of studies
The review was restricted to RCTs on humans that
compared acupuncture or acupressure with a control group and that
included pharmacological treatment, nonpharmacological treatment,
such as pelvic floor muscle exercises, sham acupuncture and placebo
acupuncture (relaxation point acupuncture). Articles written in
English or Korean were included with language restriction.
Types of participants
The review included participants of all ages who
suffered from urinary incontinence. The exclusion criteria
comprised individuals who had original underlying diseases or had a
secondary illness, such as diabetic bladder dysfunction or a
hysterectomy.
Types of intervention
Clinical trials evaluating acupuncture treatments,
including acupressure, were included. The types of control
interventions considered in this review included pharmacological
treatment, nonpharmacological treatment, such as pelvic floor
muscle exercises, sham acupuncture and placebo acupuncture
(relaxation point acupuncture).
Types of outcome measure
The assessed outcomes were a reduction in the
percentage of all daytime or urge accidents, in addition to changes
in the Visual Analog Scale (VAS) symptom scores, self-reported
severity of urine leakage and number of urine leakage episodes. The
assessment of the treatments was performed using bladder diaries,
the Medical Outcome Short-Form (MOS SF-36), the Incontinence Impact
Questionnaire (IIQ), the Urogenital Distress Inventory (UDI),
symptom questionnaires, VAS, VAS side-effects, the Psychosocial
Adjustment to Illness Scale (PAIS), urodynamic assessments,
cystometric tests, perineometry, four-day frequency volume charts,
four-day scales, pad tests and the Chinese version of the King’s
Health Questionnaire (CKHQ). The secondary outcomes assessed were
the occurrence of adverse events.
Data extraction and assessment of the risk of
bias
The full texts of the selected articles were
obtained and read in full by reviewers independently. The risk of
bias was assessed using the Cochrane criteria, which comprised
sequence generation, allocation sequence concealment, blinding of
participants, blinding of assessors, incomplete outcome data and
selective outcome reporting. The assessment was based on the
statement from the authors of each article (Table I).
 | Table ISummary of acupuncture treatment
administered in each trial. |
Table I
Summary of acupuncture treatment
administered in each trial.
| First author (yr)
[country] (ref) | Experience of
acupuncturist | De-qi | Body posture of
patients | Acupuncture
point | Treatment
frequency | F/U | Type of needle | Stimulation
method |
|---|
| Engberg (2009)
[USA] (20) | Not mentioned
(licensed by the Commonwealth of Pennsylvania) | Considered | Lay prone or sat in
massage chair | KI3, SP6, BL23,
BL31, BL32, BL33 | Twice a week | 6 weeks, treatment;
4 weeks later | Extremity points:
32 gauge, 3 cm long disposable needles Paraspinal points: 32 gauge,
4 cm long disposable needles | Extremity points:
Inserted to a depth of 20–30 mm Paraspinal points: Inserted to a
depth of 30–40 mm. Needles remained in place for 25 min |
| Kelleher (1994)
[England] (8) | Experienced | Not mentioned | Not mentioned | SP6, ST36, CV3 or
4, BL23, BL28. 2 paravertebral, lumbar, segmental points, 4 sacral,
segmental points | Weekly
treatments | 6 weeks, treatment;
3 months later | 36 gauge, 3 cm
long, disposable needles | Minimal stimulation
technique: Needles were merely flicked into the skin, left in
situ a few millimetres below the skin without further
stimulation for 10 min |
| Emmons (2005) [USA]
(21) | Not mentioned
(obstetrician- gynecologist) | Considered | Not mentioned | SP6, BL39, BL28,
CV4 | Weekly
treatments | 4 weeks, treatment;
2–4 weeks later | Not mentioned | Needles were placed
and rotated clockwise until the patient reported the sensation of
de-qi, then were retained without further stimulation for 20
min |
| Chang (2011) [Hong
Kong] (22) | One-month training
and practice for the trial | Considered | Not mentioned | CV3, CV4, CV6,
ST36, SP6, L23, BL28, BL32 | 3 weekly
treatments | 10 weeks treatment,
no f/u | | |
Results
Study description
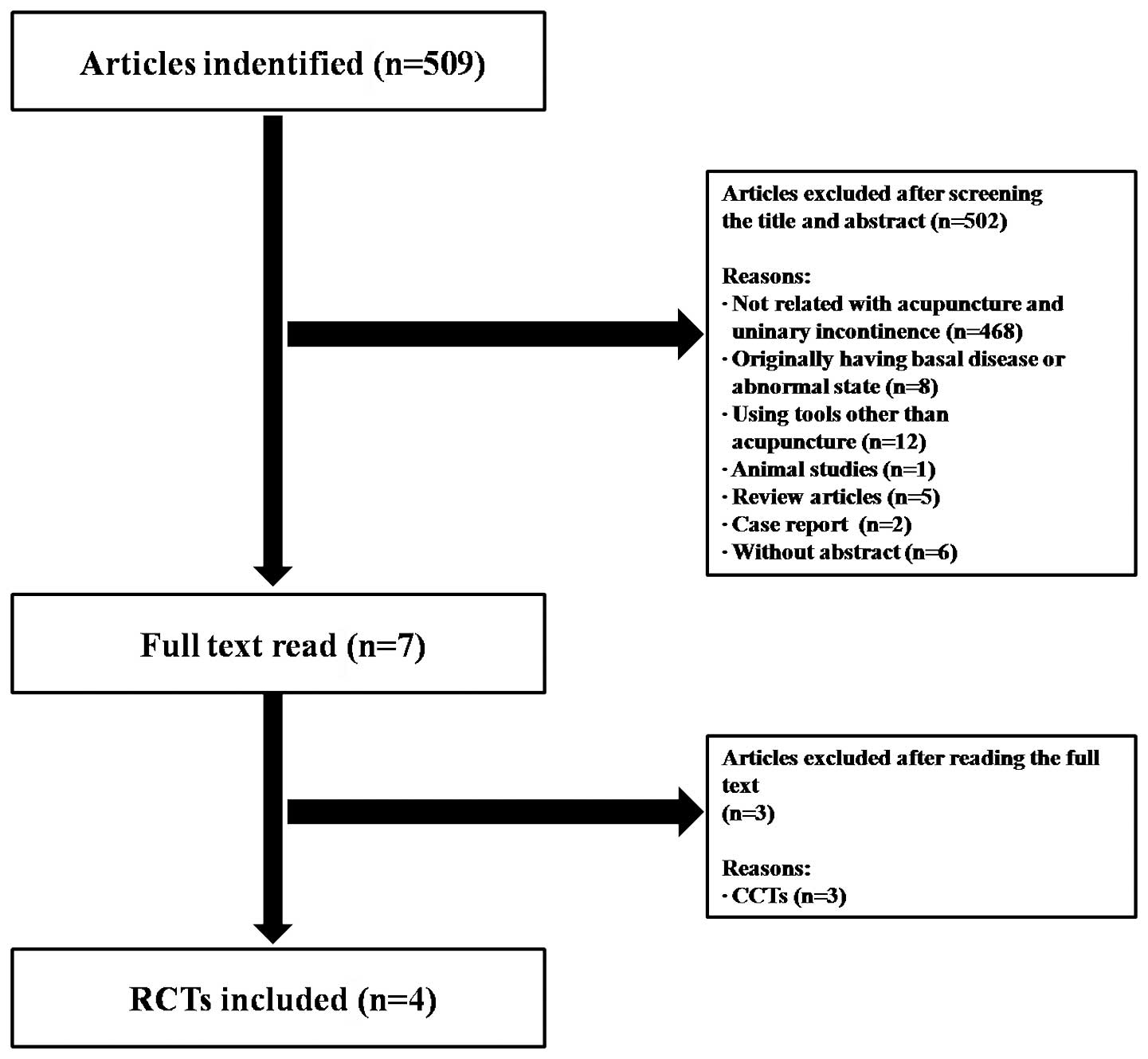
The first search identified 509 potentially relevant
articles, of which four met our inclusion criteria. Data extracted
from the four RCTs are summarized in Table I. Trials which applied acupuncture
were included. Three of the trials (8,21,22)
followed a two-arm parallel group design, while one trial (23) followed a three-arm parallel group
design. The trials only included manual acupuncture or acupressure,
while laser- and electroacupuncture were excluded. Various
acupoints for the acupuncture treatment were used in the included
RCTs: SP6 was commonly selected in all four RCTs, while CV4 and
BL23 were also included in two of the RCTs. Sham acupuncture
treatment was conducted in three trials (20–22)
and one trial (8) compared
acupuncture treatment with oral medication (oxybutynin). One of the
three sham acupuncture trials (23) compared combinations of acupuncture
treatment and pelvic floor muscle training, sham acupuncture and
pelvic floor muscle training, and pelvic floor muscle training by
itself. Three of the trials (21–23)
mentioned de-qi (the sensation of the acupuncture needle
stimulating the tissue, or a feeling of numbness, heaviness or
light pain that spreads around the needle) and two trials (8,21)
mentioned the depth of insertion. The direction of rotation of the
acupuncture needle (22) and the
patients’ body posture (21) were
each mentioned in one trial. Two trials originated in the USA
(21,22), one in England (8) and one in Hong Kong (23). There were no statistically
significant differences between the intervention and the control
groups. The included studies were all in the English language and
dissertations were excluded (Fig.
1).
Quality of Methodology
Sequence generation
Two studies (8,22)
referred to a random number table for sequence generation. The
remaining two studies (21,23)
used computer-generated randomization.
Allocation concealment
Three (8,21,23)
of the four trials received allocation scores of ‘Unclear’ as they
did not provide clear descriptions of the method of allocation
concealment used. The remaining trial (22) ensured that allocations were
concealed with the use of sealed, opaque and sequentially numbered
envelopes.
Blinding
The participants in one trial (8) out of the four were not blinded. The
remaining studies performed participant blinding using sham
acupuncture (21) or by
stimulating irrelevant acupoints (22,23).
The assessors of two of the trials were blinded to the group
assignments, while the assessors in one of the trials (23) were not blinded and the blinding
status in the remaining trial (8)
was unclear.
Incomplete outcome data
Intention-to-treat (ITT) analysis was adopted by one
trial (23). In this study, the
missing outcome data were unlikely to have an effect on the true
outcome, due to the fact that the withdrawals from the study were
imputed from the data measured at the baseline. Two of the trials
(21,22) excluded dropouts from the
statistical analysis. The risk of bias in one of the trials
(8) was unclear.
Selective outcome data
The risk of bias in the selective outcome reporting
was low in three of the RCTs (8,20,21).
One trial (23) used a four-point
scale for evaluating the subjective severity of urine leakage;
however, the results were omitted.
Other sources of bias
Due to the small scale of the studies, there were
certain limitations to this review. The composition of the study
sample was not appropriate for generalization and a larger study
with a more diverse sample is required to confirm the results. For
example, one study (22) did not
meet the necessary number of patients to achieve an 80% power to
detect a reduction in incontinence episodes. Furthermore, the
participants in another study (23) were recruited from an urogynecology
clinic in one acute hospital, and therefore the results may not be
generalizable to other clinical settings (Table II).
 | Table IIResults of assessing the risk of
bias. |
Table II
Results of assessing the risk of
bias.
| First author (yr)
[country] (ref) | Sequence
generation | Allocation sequence
concealment | Blinding of
participants | Blinding of
assessor | Incomplete outcome
data | Selective outcome
reporting |
|---|
| Engberg (2009)
[USA] (20) | Y | U | Y | Y | N | Y |
| Kelleher (1994)
[England] (8) | Y | U | N | U | U | Y |
| Emmons (2005) [USA]
(21) | Y | Y | Y | Y | N | Y |
| Chang (2011)
[Hongkong] (22) | Y | U | Y | N | Y | N |
Outcomes
Acupuncture versus conventional drug therapy
One RCT (8)
compared acupuncture with the conventional drug treatment of 5 mg
oxybutynin, twice daily. There was no significant difference in the
improvement of urge incontinence between the two groups.
Acupuncture versus sham acupuncture
Three out of the four RCTs (21–23)
compared the effects of acupuncture with those of sham acupuncture
on the symptoms of incontinence. In the study by Engberg et
al(21), the acupuncture group
had a mean 67.47% reduction in all daytime urinary incontinence
episodes, as compared with a mean reduction of 16.67% in the sham
acupuncture group. Although the difference was not statistically
significant at 4 weeks (P=0.25), it is likely that a larger sample
size may yield a statistically significant difference. Similar
differences were observed in the reduction of urge urinary
incontinence episodes (75.20 versus 24.92%). In the study by Emmons
and Otto (22), the number of
incontinence episodes was reduced by 59 and 40% in the treatment
and placebo groups, respectively. However, the difference between
the two groups was not significant. The study by Chang et
al(23), which used
acupressure, failed to exhibit a reduction in the number of urine
leakage episodes. The results failed to demonstrate statistically
significant improvements in incontinence episodes, although
differences were found in some of the subjective general
evaluations of the treatments.
Adverse events
All the studies reported adverse events, although
none of these were serious. However, one RCT reported discomfort
due to the insertion of the needles and mild headache (8), while the other studies described
drowsiness and minor bleeding (21) and bruising and discomfort with
needle placement (22) (Table III).
 | Table IIISummary of randomized controlled
trials of acupuncture for the treatment of urinary
incontinence. |
Table III
Summary of randomized controlled
trials of acupuncture for the treatment of urinary
incontinence.
| First author (yr)
[country] (ref) | N (T/C) | Population age
range (mean), years |
Design/blinding | Type of
control | Intervention | Results | Assessment of the
treatment | Adverse events
(AE) |
|---|
| Engberg (2009)
[USA] (20) | 9 (4/5) | 44–66 (54.8) | Parallel/SB | Sham
acupuncture | Acupuncture | Percentage
reduction of all daytime accident
at 1 week: 63.30% vs. 18.88% NS
at 4 week: 67.47% vs. 16.67% NS
Urge accidents
at 1 week: 74.61 vs. 16.67 NS
at 4 week: 75.2 vs. 24.92 NS | 7-day bladder diary
(MOS SF-36)
IIQ and UDI | No serious
AE
Drowsy (P=0.05)
Minor bleeding site (P=0.05) |
| Kelleher (1994)
[England] (8) | 39 (20/19) | 24–72 (51.2) | Parallel/open | Oxybutynin 5 mg
twice daily | Acupuncture | Change in symptom
visual analogue scores: Urge incontinence: NS | Bladder
diary
Symptom questionnaire
VAS, PAIS
Urodynamic assessment | Light
headache
Discomfort due to insertion of needles |
| Emmons (2005) [USA]
(21) | 74 (38/36) | 22–82 (53) | Parallel/SB | Placebo acupuncture
(relaxation points) | Acupuncture | Percentage change
in incontinence: 59% vs. 40% NS | IIQ and
UDI
3-day voiding diary
Cystometric test | No significant
AE.
23% bleeding, bruising.
25% minor discomfort with needle placement |
| Chang (2011) [Hong
Kong] (22) | 81 (27/27/27) | 18–60 (49.57) | Parallel/SB | Sham group: Sham
acupressure + pelvic floor muscle training
Control group: Pelvic floor of muscle training | Acupressure | Self-reported
severity of urine leakage and number of urine leakage episodes:
between 3 groups: NS
Self-reported severity urine leakage: intervention vs. control
group: statistically significant difference (U=−2.06,
P=0.04)
Self-reported severity of urine leakage: intervention vs. sham
group: statistically significant difference (U=−2.48,
p=0.01)
Number of urine leakages: NS |
Perineometry
4-day frequency volume chart, 4-point scale
Pad test, CKHQ | No serious AE |
Discussion
This review focused on RCTs that investigated the
efficacy of acupuncture or acupressure in the treatment of urinary
incontinence. Several methods of sham acupuncture have been used in
acupuncture RCTs, including the insertion of needles at
non-acupoints (24–26), superficially puncturing the skin at
non-acupoints (27–29) and the non-penetration of
non-acupoints (30). Of the four
RCTs selected, three trials applied sham acupuncture on the control
group. One of these studies (21)
used a typical sham acupuncture needle, where the needle appears to
have been inserted, despite the needle not actually piercing the
skin. Another study (22) selected
relaxation acupoints, while the remaining study (23) used acupoints that had no relevance
to urinary incontinence.
Needle stimulation causing de-qi has been
suggested to be important for achieving the maximum effect
(31,32). This sensation was considered in
three (21–23) of the four selected RCTs. As
mentioned previously, it has also been demonstrated that it is
important for the insertion depth of the acupuncture to be varied
according to the intention of the stimulation; however, none of the
included RCTs reasonably differentiated the depth of acupuncture.
Two trials (8,21) mentioned the depth of needle
insertion: In one of the studies (8) the needle penetrated only skin-deep,
while in the other study (21) the
insertion depth was differentiated according the region of the
body, such as whether it was the trunk or limb. It was implied that
these points were selected in a manner that corresponded to the
segmental innervation of the bladder, but the study did not provide
a reason as to why the insertion depth was varied, i.e. deep on the
trunk, and shallow on the limbs.
The majority of the included trials lacked adequate
allocation concealment and involved insufficient sample sizes for
meaningful conclusions to be drawn, with no inclusion of power
analysis. One RCT (22) employed
allocation concealment and two of the RCTs blinded the assessor.
The experience and the number of the acupuncture practitioners used
may be a factor affecting the results in acupuncture clinical
trials. Out of the included trials, one trial (8) described the acupuncturist as
‘experienced’, while another trial (21) simply mentioned the institution that
licensed the acupuncturist. In the study by Emmons and Otto
(22), the acupuncture was
performed by an obstetrics and gynecology doctor who had been
trained in acupuncture, instead of a specifically trained
acupuncturist. In one study with acupressure (23), the investigator had taken a
one-month training course on acupressure theory and practice,
solely for the purpose of the study. Therefore it was not fully
elucidated whether the acupuncture was administered by well-trained
practitioners.
All the included studies evaluated the adverse
events or possible risks of acupuncture, which were either mild or
not present. However, these results may not be generalizable, due
to the fact that the patients with a high or a medium risk of
experiencing adverse effects were excluded, the follow-up may have
been short-term and the sample sizes were relatively small
(33,34).
Together, the results of the evaluated studies
failed to statistically demonstrate the specific effects of
acupuncture on urinary incontinence. Two (21,22)
of the four RCTs suggested that a reduction in the number of
incontinence episodes was achieved, but did not reveal any
significant differences compared with the control group. The use of
statistics does not always guarantee validity, however. It is not
possible to clearly determine the effect of acupuncture from the
results of the four RCTs in this review.
Despite this fact, this review verified many
additional effects with regard to various overactive bladder
symptoms. In particular, one trial (8) revealed acupuncture to be equally
efficient compared with standard anticholinergic therapy in the
management of low bladder compliance, although with fewer
side-effects. In addition, this study (8) demonstrated that acupuncture exhibited
statistically significant effects on the symptom relief of urgency,
frequency, and nocturia, as revealed on a VAS and in a voiding
diary. Furthermore, there was an increase in bladder capacity and a
reduction in detrusor pressure rise on filling, although there was
no significant difference between the control and treatment groups
in the urodynamic results. In the treatment group in another study
(22), there were significant
reductions in frequency, a 30% reduction in the proportion of voids
correlated with urgency and a 13% increase in maximum voided volume
and maximum cystometric capacity. Moreover, one of the studies
(23) revealed a significant
difference in the increase of pelvic floor muscle strength across
three groups: intervention group (acupuncture and pelvic floor
muscle training) versus sham group (sham acupuncture and pelvic
floor muscle training) versus control group (pelvic floor muscle
training). Following intervention, the pelvic floor muscle strength
increased between the intervention and sham (U=−2.31) and between
the intervention and control groups (U=−2.25). With regard to the
self-reported severity of urine leakage, there were significant
differences between the intervention and sham (U=−2.06) and between
the intervention and control groups (U=−2.48) following
intervention. In addition, the studies revealed an improvement in
quality of life, as measured with numerous questionnaires. In one
study, which used PAIS (8), there
was an improvement in the quality of life, particularly with regard
to domestic, vocational and leisure activities; however, the small
number of subjects limited the value of statistical comparison.
There were specific areas associated with urinary symptoms that
also demonstrated several changes, as well as the general quality
of life. One of the true-acupuncture groups had a greater, although
nonsignificant, improvement in the urge-related distress subscale
of UDI than the sham acupuncture group (21). Another study revealed that the
scores on the UDI and IIQ improved in the treatment and control
groups, with significant differences between the two groups for the
two scores (22). In a different
trial (23), the intervention
group demonstrated a significant improvement in all domains of the
CKHQ.
The RCTs included in this review provided
insufficient evidence to enable assessment of the efficacy and
safety of acupuncture or acupressure in the treatment of urinary
incontinence for a number of reasons. Firstly, the results from the
analysis of the RCTs were limited as a result of their
methodological deficiencies. Only one study (22) demonstrated acceptable allocation
concealment. The details regarding the dropouts and withdrawals
were described in all trials, but it was not clearly mentioned
whether they were included in the final analysis. Furthermore, in
this review, the interpretation of the results was limited by the
different tools used in each trial. Two studies (8,21)
used a retrospective checklist for the assessment of changes in
symptoms. The assessment was made before and after four to six
weeks of intervention, which depended on the participants’ recall
memory. Retrospective accounts of participants regarding their
symptoms have been demonstrated to be unreliable in previous
studies. Moreover, one trial (22)
used a three-day voiding diary, which despite having been
demonstrated to be nearly as accurate as a seven-day diary for
studying urinary incontinence, may have been less precise.
In conclusion, although the included trials revealed
that acupuncture may be beneficial to patients with urinary
incontinence, there is insufficient evidence to support this
conclusion, due to the methodological flaws in the studies. These
included unknowns in sequence generation, concealment of
allocation, blinding and outcome measures. Further large,
well-designed RCTs with rigorous methods of randomization and
blinding and adequate allocation concealment, in addition to
validated outcome measures, are therefore required.
Acknowledgements
This study was supported by the Basic Science
Research Program through the National Research Foundation of Korea
(NRF), funded by the Ministry of Education, Science, and Technology
(grant no. 2005-0049404).
References
|
1
|
Nygaard IE and Heit M: Stress urinary
incontinence. Obstet Gynecol. 104:607–620. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Abrams P, Cadozo L, Fall M, et al;
Standardisation Sub-committee of the International Continence
Society. The standardisation of terminology of lower urinary tract
dysfunction: report from the Standardisation Sub-committee of the
International Continence Society. Neurourol Urodyn. 21:167–178.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Robinson D: Patholophysiology of female
lower urinary tract dysfunction. Obstet Gynecol Clin North Am.
25:747–756. 1998. View Article : Google Scholar
|
|
4
|
Philip T, Shah PJ and Worth PH:
Acupuncture in the treatment of bladder instability. Br J Urol.
61:490–493. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chang PL: Urodynamic studies in
acupuncture in women with frequency, urgency, and dysuria. J Urol.
140:563–566. 1988.PubMed/NCBI
|
|
6
|
Bergström K, Carlsson C, Lindholm C and
Widengren R: Improvement of urge- and mixed-type incontinence after
acupuncture treatment among elderly women - a pilot study. J Auton
Nerv Syst. 79:173–180. 2000.PubMed/NCBI
|
|
7
|
Honjo H, Kitakoji H, Kawakita K, et al:
Acupuncture for urinary incontinence in patients with chronic
spinal cord injury. Nippon Hinyokika Gakkai Zasshi. 89:665–669.
1998.(In Japanese).
|
|
8
|
Kelleher C, Filshie J, Khullar V and
Cardozo L: Acupuncture and the treatment of irritative bladder
symptoms. Acupunct Med. 12:9–12. 1994. View Article : Google Scholar
|
|
9
|
Knardahl S, Elam M, Olausson B and Wallin
BG: Sympathetic nerve activity after acupuncture in humans. Pain.
75:19–25. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rajaofetra N, Passagia JG, Marlier L, et
al: Serotoninergic, noradrenergic, and peptidergic innervation of
Onuf’s nucleus of normal and transected spinal cords of baboons
(Papio papio). J Comp Neurol. 318:1–17. 1992.
|
|
11
|
Minni B, Capozza N, Creti G, De Gennaro M,
Caione P and Bischko J: Bladder instability and enuresis treated by
acupuncture and electro-therapeutics: early urodynamic
observations. Acupunct Electrother Res. 15:19–25. 1990.PubMed/NCBI
|
|
12
|
Nakamura M, Sakurai T, Tsujimoto Y and
Tada Y: Bladder inhibition by electrical stimulation of the
perianal skin. Urol Int. 41:62–63. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sato A, Sato Y, Shimada F and Torigata Y:
Changes in vesical function produced by cutaneous stimulation in
rats. Brain Res. 94:465–474. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chartier-Kastler EJ, Ruud Bosch JL,
Perrigot M, et al: Long-term results of sacral nerve stimulation
(S3) for the treatment of neurogenic refractory urge incontinence
related to detrusor hyperreflexia. J Urol. 164:1476–1480. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jiang H, Wang PJ, Zeng HW and Zhao XH:
Central mechanism of electric-acupuncture at Zusanli (ST36) for
gastric mucous membrane protection with FMRI. Zhonghua Yi Xue Za
Zhi. 90:1458–1462. 2010.PubMed/NCBI
|
|
16
|
Anderson S and Lundeberg T: Acupuncture -
from empiricism to science: functional background to acupuncture
effects in pain and disease. Med Hypotheses. 45:271–281. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Itoh K, Minakawa Y and Kitakoji H: Effect
of acupuncture depth on muscle pain. Chin Med. 6:242001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Silca ML, Silva JR and Prado WA: The
antinociceptive effect of electroacupuncture at different depths of
acupoints and under the needling surface. Chin Med. 7:32012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Itoh K, Katsumi Y and Kitakoji H: Trigger
point acupuncture treatment of chronic low back pain in elderly
patients - a blinded RCT. Acupunct Med. 22:170–177. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Itoh K, Okada K and Kawakita K: A proposed
experimental model of myofascial trigger points in human muscle
after slow eccectric exercise. Acupunct Med. 22:2–12. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Engberg S, Cohen S and Sereika SM: The
efficacy of acupuncture in treating urge and mixed incontinence in
women: a pilot study. J Wound Ostomy Continence Nurs. 36:661–670.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Emmons SL and Otto L: Acupuncture for
overactive bladder: a randomized controlled trial. Obstet Gynecol.
106:138–143. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chang KK, Wong TK, Wong TH, Leung AW and
Chung JW: Effect of acupressure in treating urodynamic stress
incontinence: a randomized controlled trial. Am J Chin Med.
39:1139–1159. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
de Azevedo RF, Cbiari BM, Okada DM and
Onishi ET: Impact of acupuncture on otoacoustic emissions in
patients with tinnitus. Braz J Otorhinolaryngol. 73:599–607.
2007.PubMed/NCBI
|
|
25
|
Okada DM, Onishi ET, Chami FI, Borin A,
Cassola N and Guerreiro VM: Acupuncture for tinnitus immediate
relief. Braz J Otorhinolaryngol. 72:182–186. 2006.PubMed/NCBI
|
|
26
|
Hansen PE, Hansen JH and Bentzen O:
Acupuncture treatment of chronic unilateral tinnitus - a
double-blind cross-over trial. Clin Otolaryngol Allied Sci.
7:325–329. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Vilholm OJ, Møller K and Jørgensen K:
Effect of traditional Chinese acupuncture on severe tinnitus: a
double-blind, placebo-controlled, clinical investigation with open
therapeutic control. Br J Audiol. 32:197–204. 1998. View Article : Google Scholar
|
|
28
|
Jeon SW, Kim KS and Nam HJ: Long-term
effect of acupuncture for treatment of tinnitus: a randomized,
patient- and assessor-blind, sham-acupuncture-controlled, pilot
trial. J Alter Complement Med. 18:693–699. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang K, Bugge J and Bugge S: A randomised,
placebo-controlled trial of manual and electrical acupuncture for
the treatment of tinnitus. Complement Ther Med. 18:249–255. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Marks NJ, Emery P and Onisiphorou C: A
controlled trial of acupuncture in tinnitus. J Laryngol Otol.
98:1103–1109. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ezzo J, Berman B, Hadhazy VA, Jadad AR,
Lao L and Singh BB: Is acupuncture effective for the treatment of
chronic pain? A systemic review. Pain. 86:217–225. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zaslawski CJ, Cobbin D, Lidums E and
Petocz P: The impact of site specificity and needle manipulation on
changes to pain pressure threshold following manual acupuncture: a
controlled study. Complement Ther Med. 11:11–21. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Loke YK, Derry S and Aronson JK: A
comparison of three different sources of data in assessing the
frequencies of adverse reactions to amiodarone. Br J Clin
Pharmacol. 57:616–621. 2004.PubMed/NCBI
|
|
34
|
Loke YK and Derry S: Reporting of adverse
drug reactions in randomised controlled trials - a systematic
survey. BMC Clin Pharmacol. 1:32001. View Article : Google Scholar : PubMed/NCBI
|