Introduction
Essential thrombocythemia (ET) is a chronic clonal
myeloproliferative disorder, which is characterized by persistent
thrombocytosis and complicated by arterial or venous thrombosis and
idiopathic bleeding diathesis. These complications are the primary
causes of mortality in patients with ET (1–3).
Although ET-related thrombosis is uncommon in coronary arterial
thrombosis, it is more common in extremity vascular thrombosis and
may subsequently cause acute myocardial infarction (AMI). Cases of
ET complicated with AMI have been reported previously, but have not
been treated with surgical therapy (4–6). The
present case study reports a patient with ET complicated by AMI,
leading to ventricular aneurysm following interventional therapy
for 3 years and subsequent in-stent restenosis. Following careful
examination, a ventricular aneurysm resection and coronary artery
bypass graft were carried out.
Case report
The present patient was a 48-year-old female who had
been admitted to Beijing Tiantan Hospital (Beijing, China) 2 years
previously and had complained of a persistently congested chest and
radiated pain in her left shoulder for a period of 6 hours.
Electrocardiography revealed AMI of the anterior wall. The
biomarkers of myocardial injury were significantly increased
(troponin I, 12.27 ng/ml; creatine kinase, 1,548 IU/l; and creatine
kinase isozyme CK-MB, 189.0 U/l) compared with the normal range
(troponin I, <0.04 ng/ml; creatine kinase, 24–170 IU/l; and
CK-MB, 0.97–2.88 ng/ml). Laboratory tests revealed that levels of
leukocytes (7.1×109/l), hemoglobin (128 g/l), high
density lipoprotein (1.20 mmol/l), low density lipoprotein (2.51
mmol/l) and fasting blood-glucose (5.4 mmol/l) were in the normal
range. However, platelet levels (8.89×1011/l) were
higher than the normal range (1–3×1011/l). The patient
was treated using primary percutaneous coronary intervention.
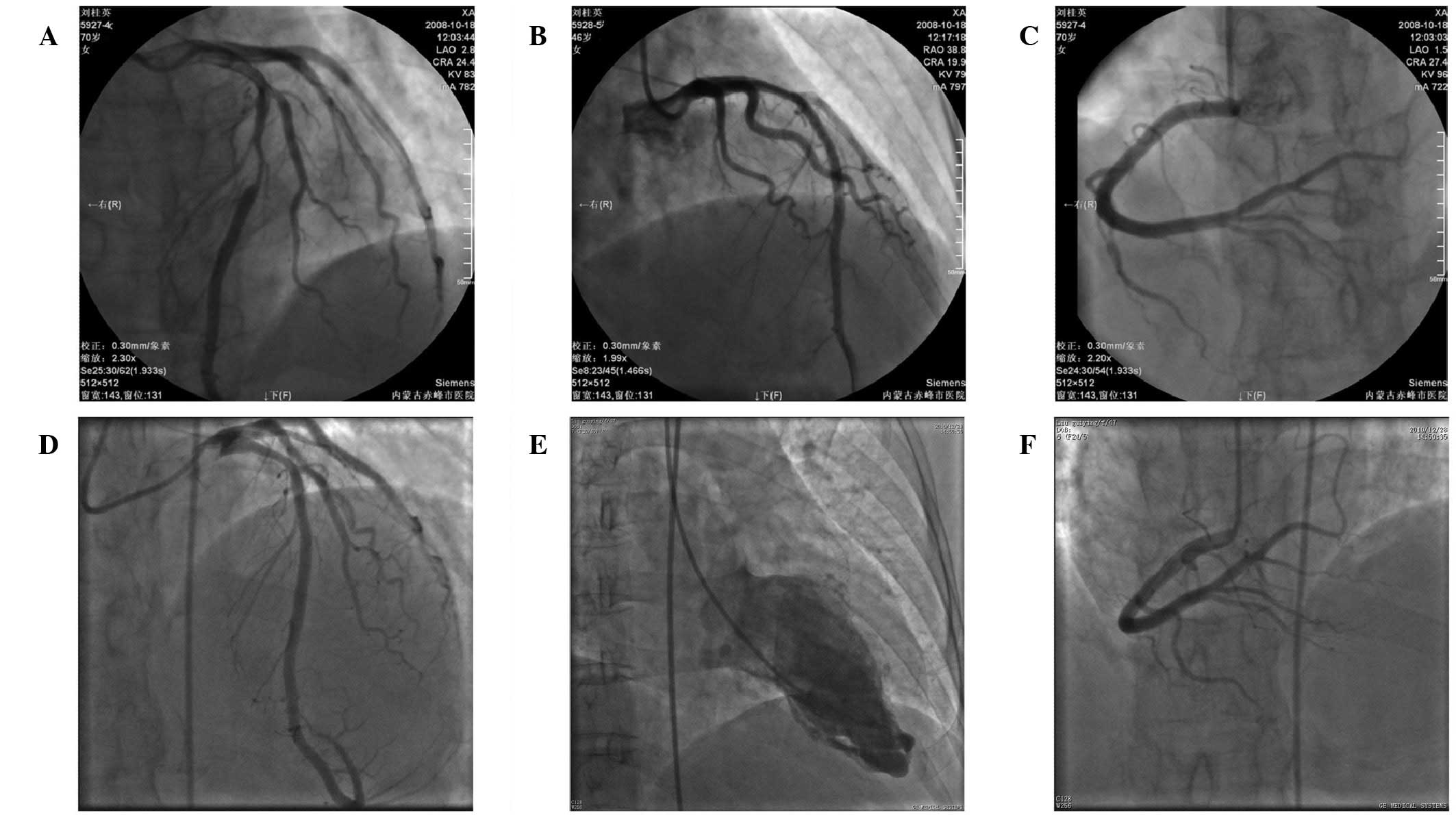
Intraoperative observations indicated that 90% of the near front
descending branch was narrowed and the remainder of the aortic wall
was smoothed. Subsequently, a rapamycin-eluting stent (3.5×29 mm)
was embedded in the front descending branch (Fig. 1A, B and C). Postoperatively, chest
congestion was relieved and the patient was discharged. The patient
was initially administered with clopidogrel (75 mg per day) to
reduce the platelet count, which was subsequently replaced with
enteric aspirin 1 year later (100 mg per day).
The patient complained of palpitations and shortness
of breath one month prior to the second admission. During this
period, the patient experienced paroxysmal nocturnal dyspnea and
was unable to lie in a horizontal position at night. High blood
pressure, diabetes or hyperlipoidemia were not observed or a
history of smoking. The patient had been diagnosed with ET in the
Beijing Tiantan Hospital 15 years previously. All routine test
references were within the normal range, with the exception of the
platelet count (5.52×1011/l). Color doppler
echocardiography was performed and identified a ventricular
aneurysm. Furthermore, coronary arteriography revealed a 50%
narrowing in the front descending stent and the formation of a left
ventricular aneurysm (Fig. 1D and
E). The symptoms of cardiac insufficiency disappeared following
symptomatic treatment. The patient was administered hydroxyurea
(100 mg per day) for a week in order to reduce platelet count to
325×109/l. The ventricular aneurysm was resected under
general anesthesia and cardiopulmonary bypass. Bypass surgery was
performed between the left internal mammary artery and the front
descending stent. The patient recovered well and no complications,
for example hemorrhage or thrombosis, occurred. The platelet count
was controlled using hydroxyurea (100 mg per day) and aspirin (100
mg per day). At ~15 days following surgery, the platelet count was
286×109/l and the patient was discharged. At the 3-month
follow-up, the patient showed no signs of heart insufficiency or
angina. An ultrasonic cardiogram showed that the left ventricular
aneurysm had disappeared. Furthermore, no heart-related symptoms
were detected at a 2-year follow-up. The study was approved by The
Ethics Committee of Being Military Region General Hospital,
Beijing, China. Written informed patient consent was obtained from
the patient or the patient’s family.
Discussion
The annual incidence of ET is ~1.5 per 100,000
individuals worldwide (7). The
principal causes of morbidity and mortality in ET are thrombosis,
hemorrhage and progression to myelofibrosis or acute myelogenous
leukemia (8). Only 9.4% of
patients with ET have myocardial infarction (9). Although the median age of patients
with ET is 60 years, 10–25% of patients are <40 years of age and
one-third of patients are asymptomatic (10–13).
With the exception of a history of thrombosis, cardiovascular
disease risk factors, including smoking, high blood pressure,
hyperlipidemia and diabetes, are also risk factors for thrombosis
(12).
In the present report, we describe an ET case
complicated with AMI and the formation of a ventricular aneurysm.
Preoperative examinations showed no cardiovascular disease risk
factors and the vital organs were healthy. Therefore, a history of
ET was the only surgical risk. Although the incidence rate of
thrombosis is higher than bleeding for ET cases, the risk of
bleeding is relatively higher in surgical cases (14). Regardless of the complications of
thrombosis or hemorrhage, the monitoring and control of the
platelet count, preoperatively or postoperatively, is key for a
successful surgery. In this case, the patient maintained a
relatively normal platelet count as a result of treatment with
hydroxyurea and the platelet count in the perioperative period was
consistent with previous case reports (15–17).
Meanwhile, such alteration of the platelet count may also be
controlled postoperatively.
Similar cases have been reported in previous
studies. However, the majority of such cases were treated with an
interventional approach and rarely via surgical methods. ET,
complicated by coronary artery thrombosis, has no uniform treatment
guidelines worldwide and therefore clinical treatment is difficult.
As well as utilizing anti-platelet drugs, including aspirin and
clopidogrel, it is important to use platelet-cytoreductive therapy
for ET patients (18–20). In the case of coronary artery stent
restenosis, we recommend a combined treatment of hydroxyurea and
aspirin to prevent thrombosis.
In conclusion, surgical treatment for ET with
myocardial infarction is rare and no uniform treatment guidelines
are currently available worldwide. Therefore, ET is a key risk in
surgery. It is important to prevent thrombosis and hemorrhage, as
well as monitor and control the platelet count preoperatively and
postoperatively in order to achieve a successful surgery.
References
|
1
|
Besses C, Cervantes F, Pereira A, Florensa
L, Solé F, Hernández-Boluda JC, Woessner S, Sans-Sabrafen J, Rozman
C and Montserrat E: Major vascular complications in essential
thrombocythemia: a study of the predictive factors in a series of
148 patients. Leukemia. 13:150–154. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Weng S, Zhu X, Jin Y, Wang T and Huang H:
Protective effect of erythropoietin on myocardial infarction in
rats by inhibition of caspase-12 expression. Exp Ther Med.
2:833–836. 2011.PubMed/NCBI
|
|
3
|
Schafer AI: Thrombocytosis. N Engl J Med.
350:1211–1219. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mizuta E, Takeda S, Sasaki N, Miake J,
Hamada T, Shimoyama M, Tajima F, Igawa O, Shigemasa C and Hisatome
I: Acute myocardial infarction in a patient with essential
thrombocythemia: successful treatment with percutaneous
transluminal coronary recanalization. Circ J. 69:1000–1002. 2005.
View Article : Google Scholar
|
|
5
|
Pick RA, Glover MU, Nanfro JJ, Dubbs WF,
Gibbons JA and Vieweg WV: Acute myocardial infarction with
essential thrombocythemia in a young man. Am Heart J. 106:406–407.
1983. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhang Z, Wan X, Liu Y, Lin X, Ni Z, Yang X
and Zhang L: Non-ST-segment elevation myocardial infarction in a
patient with essential thrombocythemia treated with glycoprotein
IIb/IIIa inhibitor: a case report. Clin Appl Thromb Hemost.
17:532–534. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Johansson P: Epidemiology of the
myeloproliferative disorders polycythemia vera and essential
thrombocythemia. Semin Thromb Hemost. 32:171–173. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
McIntyre KJ, Hoagland HC, Silverstein MN
and Petitt RM: Essential thrombocythemia in young adults. Mayo Clin
Proc. 66:149–154. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rossi C, Randi ML, Zerbinati P, Rinaldi V
and Girolami A: Acute coronary disease in essential thrombocythemia
and polycythemia vera. J Intern Med. 244:49–53. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Alvarez-Larrán A, Cervantes F, Bellosillo
B, Giralt M, Juliá A, Hernández-Boluda JC, Bosch A, Hernández-Nieto
L, Clapés V, Burgaleta C, Salvador C, Arellano-Rodrigo E, Colomer D
and Besses C: Essential thrombocythemia in young individuals:
frequency and risk factors for vascular events and evolution to
myelofibrosis in 126 patients. Leukemia. 21:1218–1223. 2007.
|
|
11
|
Carobbio A, Finazzi G, Guerini V, Spinelli
O, Delaini F, Marchioli R, Borrelli G, Rambaldi A and Barbui T:
Leukocytosis is a risk factor for thrombosis in essential
thrombocythemia: interaction with treatment, standard risk factors,
and Jak2 mutation status. Blood. 109:2310–2313. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang Y, Zhang ZZ, Wu Y, Zhan J, He XH and
Wang YL: Honokiol protects rat hearts against myocardial ischemia
reperfusion injury by reducing oxidative stress and inflammation.
Exp Ther Med. 5:315–319. 2013.PubMed/NCBI
|
|
13
|
Wolanskyj AP, Schwager SM, McClure RF,
Larson DR and Tefferi A: Essential thrombocythemia beyond the first
decade: life expectancy, long-term complication rates, and
prognostic factors. Mayo Clin Proc. 81:159–166. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ruggeri M, Rodeghiero F, Tosetto A,
Castaman G, Scognamiglio F, Finazzi G, Delaini F, Micò C, Vannucchi
AM, Antonioli E, De Stefano V, Za T, Gugliotta L, Tieghi A,
Mazzucconi MG, Santoro C and Barbui T; Gruppo Italiano Malattie
Ematologiche dell’Adulto (GIMEMA) CHronis Myeloproliferative
Diseases Working Party. Postsurgery outcomes in patients with
polycythemia vera and essential thrombocythemia: a retrospective
survey. Blood. 111:666–671. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Das SS, Bose S, Chatterjee S, Parida AK
and Pradhan SK: Thrombocytapheresis: managing essential
thrombocythemia in a surgical patient. Ann Thorac Surg. 92:e5–e6.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jin D, Wu Y, Zhao L, Guo J, Zhang K and
Chen Z: Atorvastatin reduces serum HMGB1 levels in patients with
hyperlipidemia. Exp Ther Med. 4:1124–1126. 2012.PubMed/NCBI
|
|
17
|
Ohto T, Shihara H, Miyauchi Y and Nakajima
N: A case of coronary artery bypass surgery using left internal
thoracic artery and right gastroepiploic artery for a patient with
essential thrombocythemia. Jpn J Thorac Cardiovasc Surg.
46:767–771. 1998.(In Japanese).
|
|
18
|
Lv H and Ning B: Pathogenesis of
bloodstream infection in children with blood cancer. Exp Ther Med.
5:201–204. 2013.PubMed/NCBI
|
|
19
|
Harrison CN, Campbell PJ, Buck G, Wheatley
K, East CL, Bareford D, Wilkins BS, van der Walt JD, Reilly JT,
Grigg AP, Revell P, Woodcock BE and Green AR; United Kingdon
Medical Research Council Primary Thrombocythemia 1 Study.
Hydroxyurea compared with anagrelide in high-risk essential
thrombocythemia. N Engl J Med. 353:33–45. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Vannucchi AM, Guglielmelli P and Tefferi
A: Advances in understanding and management of myeloproliferative
neoplasms. CA Cancer J Clin. 59:171–191. 2009. View Article : Google Scholar : PubMed/NCBI
|