Introduction
Oral squamous cell carcinoma is a type of cancer
that usually develops on the squamous or epithelial cells that
cover the lips and oral cavity. The malignant or cancerous cells
are usually located on the floor of the mouth or on the surface of
the tongue. These cancerous cells also originate on the lower lips
and palate or the tonsillar area of the oral cavity (1). It is considered that squamous cell
carcinoma develops from the keratinizing or malpighian epithelial
cells, as the presence of keratin has been observed in the
malignant cells. It is one of the most prevalent types of oral and
pharyngeal cancers (2). Squamous
cells are the main component of the epidermis of the skin and this
cancer is one of the major forms of skin cancer. Squamous cell
carcinoma is the second-most common cancer of the skin (3). Squamous cell cancers of the skin in
individuals on immunotherapy or suffering from lymphoproliferative
disorders tend to be much more aggressive, regardless of their
location (4).
Imprinting control region (ICR) mice are widely used
in cancer studies. Animal models facilitate the development and
testing of new approaches of research on disease prevention and
treatment, identification of early diagnostic markers and novel
therapeutic targets, as well as provide an understanding of the
in vivo biology and genetics of tumor initiation, promotion,
progression and metastasis (5).
The U14 mouse tumor is a squamous cell carcinoma that was
ectopically induced by treating the uterine cervix with
20-methylcholanthrene. The tumor was established and maintained by
the Chinese Academy of Medical Sciences and Peking Union Medical
College in 1958 (6). Following
transplantation of U14 cells, the incidences of lymphatic and
pulmonary metastasis were 95 and 80%, respectively, and the average
survival time of mice with the tumor was 27 days. U14 cells are
widely used in studies of tumor invasion, metastasis, recurrence
and drug screening. Establishment of a cultured tumor cell line,
which forms a tumor in vivo, would be helpful for the study
of tumor biology on a cellular and molecular level (7–9).
In this study, we established an animal model by
inducing mice with U14 squamous cell carcinoma cells, for in
vivo evaluation of buccal mucosa cancer. The model successfully
induces buccal mucosa cancer in mice and the application of the
model may improve the experimental results of future research on
buccal mucosa cancer.
Materials and methods
Animals
Seven-week-old male ICR mice (n=60) were purchased
from the Experimental Animal Center of Chongqing Medical University
(Chongqing, China). They were maintained in a
temperature-controlled facility (temperature 23±1°C, relative
humidity 50±5%) with a 12-h light/dark cycle. The mice had
unlimited access to a standard mouse chow diet and water.
Cancer cell preparation
U14 squamous cell carcinoma cells were obtained from
the Chinese Academy of Medical Sciences (Beijing, China). The
cancer cells were cultured in RPMI-1640 medium (Gibco Services
Inc., Birmingham, MI, USA) supplemented with 10% fetal bovine serum
(FBS) and 1% penicillin-streptomycin (Gibco Services Inc.) at 37°C
in a humidified atmosphere containing 5% CO2 (model 311,
Thermo Forma Inc., Waltham, MA, USA). The medium was changed 2–3
times each week. The in vitro-cultured U14 cells
(5×106 cells/mouse) were inoculated into the abdominal
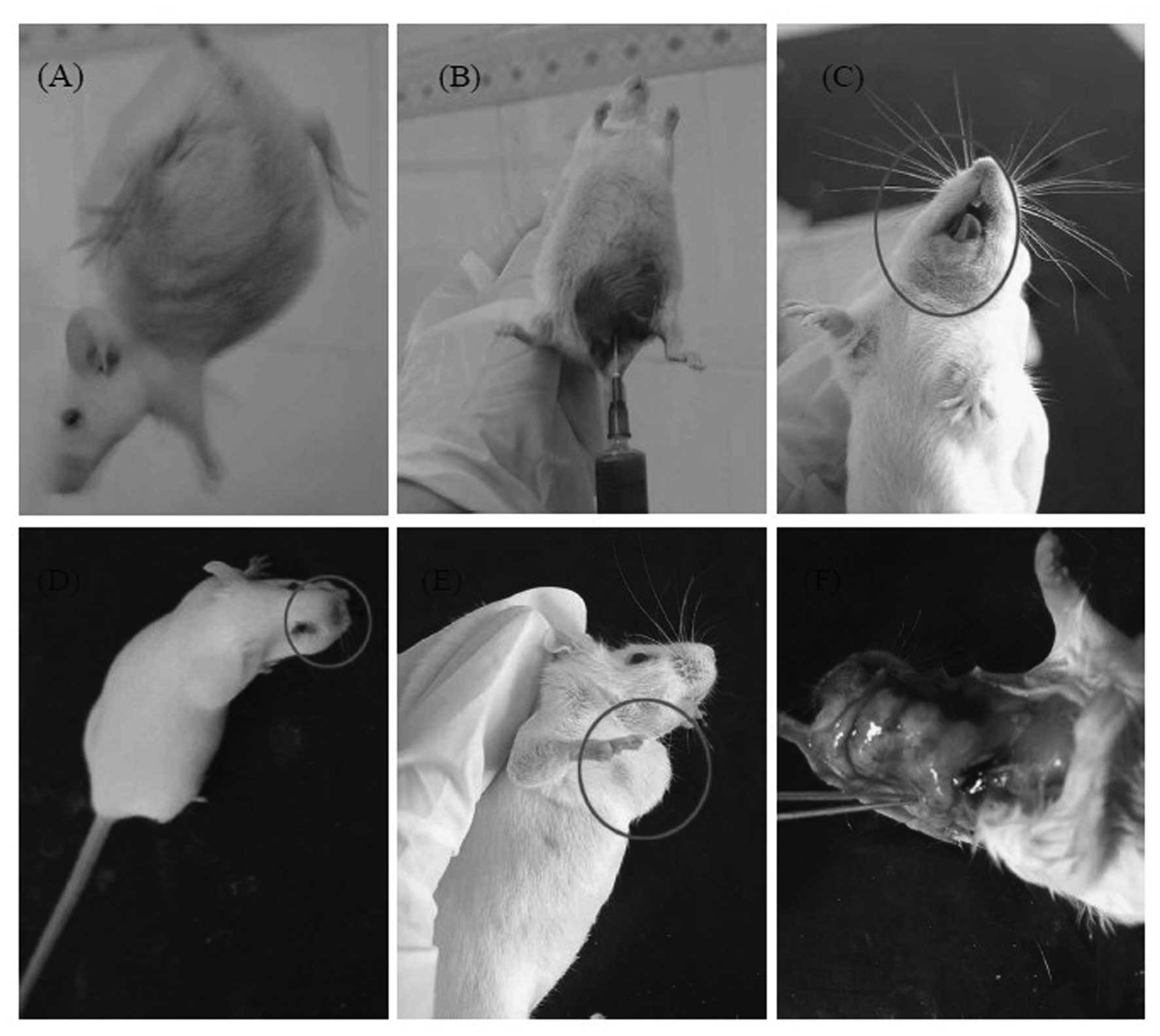
cavity of 7-week-old female ICR mice (Fig. 1A). After 1 week, the carcinoma
ascites were collected and diluted in sterile saline at a
concentration of 1×107 cells/ml (Fig. 1B).
Induction of buccal mucosa cancer
To establish the buccal mucosa cancer animal model,
50 mice were inoculated with 0.05 ml U14 cancer cell suspension
(1×107 cells/ml) on the buccal mucosa. Ten mice were
bred as normal and acted as controls. Mice that succumbed to
natural causes were collected and their buccal mucosa and lymph
node tissues were determined. These experiments followed a protocol
approved by the Animal Ethics Committee of Chongqing Medical
University.
Histological analysis of buccal mucosa
cancer
Buccal mucosa and lymph node tissues were removed
and embedded in paraffin for histological analysis with hematoxylin
and eosin staining, as previously described (10).
Reverse transcription-polymerase chain
reaction (RT-PCR)
The mRNA expression of B cell lymphoma 2 (Bcl-2),
Bcl-2-associated X protein (Bax), caspase-3, caspase-9, nuclear
factor (NF)-κB, IκB-α, inducible nitric oxide synthase (iNOS),
cyclooxygenase (COX)-2, matrix metalloproteinases (MMPs) and tissue
inhibitors of MMPs (TIMPs) was assessed using RT-PCR. Total RNA was
isolated using TRIzol reagent (Invitrogen Life Technologies,
Carlsbad, CA, USA) according to the manufacturer’s instructions.
The RNA was digested with RNase-free DNase (Roche, Basel,
Switzerland) for 15 min at 37°C and purified using an RNeasy kit
(Qiagen, Hilden, Germany) according to the manufacturer’s
instructions. cDNA was synthesized from 2 μg total RNA and
incubated at 37°C for l h with AMV reverse transcriptase (GE
Healthcare, Uppsala, Sweden) with random hexanucleotides, according
to the manufacturer’s instructions. The primers used to
specifically amplify the genes were as follows: forward, 5′-AAG CTG
AGC GAG TGT CTC CGG CG-3′ and reverse, 5′-CAG ATG CCG GTT CAG GTA
CTC AGT C-3′ for Bax; forward, 5′-CTC GTC GCT ACC GTC GTG ACT
TGG-3′ and reverse, 5′-CAG ATG CCG GTT CAG GTA CTC AGT C-3′ for
Bcl-2; forward, 5′-CAA ACT TTT TCA GAG GGG ATC G-3′ and reverse,
5′-GCA TAC TGT TTC AGC ATG GCA-3′ for caspase-3; forward, 5′-GGC
CCT TCC TCG CTT CAT CTC-3′ and reverse, 5′-GGT CCT TGG GCC TTC CTG
GTA T-3′ for caspase-9; forward, 5′-CAC TTA TGG ACA ACT ATG AGG TCT
CTG G-3′ and reverse, 5′-CTG TCT TGT GGA CAA CGC AGT GGA ATT TTA
GG-3′ for NF-κB; forward, 5′-GCT GAA GAA GGA GCG GCT ACT-3′ and
reverse, 5′-TCG TAC TCC TCG TCT TTC ATG GA-3′ for IκB-α; forward,
5′-AGA GAG ATC GGG TTC ACA-3′ and reverse, 5′-CAC AGA ACT GAG GGT
ACA-3′ for iNOS; forward, 5′-TTA AAA TGA GAT TGT CCG AA-3′ and
reverse, 5′-AGA TCA CCT CTG CCT GAG TA-3′ for COX-2; forward,
5′-CTT CTT CAA GGA CCG GTT CA-3′ and reverse, 5′-GCT GGC TGA GTA
CCA GTA-3′ for MMP-2; forward, 5′-TGG GCT ACG TGA CCT ATG AC-3′ and
reverse, 5′-GCC CAG CCC ACC TCC ACT CC-3′ for MMP-9; forward,
5′-GTC AGT GAG AAG CAA GTC GA-3′ and reverse, 5′-ATG TTC TTC TCT
GTG ACC CA-3′ for TIMP-1; forward, 5′-TGG GGA CAC CAG AAG TCA AC-3′
and reverse, 5′-TTT TCA GAG CCT TGG AGG AG-3′ for TIMP-2. The
internal control gene, glyceraldehyde 3-phosphate dehydrogenase
(GAPDH), was amplified with the following primers: forward, 5′-CGG
AGT CAA CGG ATT TGG TC-3′ and reverse, 5′-AGC CTT CTC CAT GGT CGT
GA-3′. Amplification was performed in a thermal cycler (Eppendorf,
Hamburg, Germany) with cycles of denaturation. The amplified PCR
products were run on 1.0% agarose gels and visualized by ethidium
bromide (EtBr) staining (11).
Western blot analysis
Total tissue protein was obtained with
radioimmunoprecipitation assay (RIPA) buffer as described by Kim
et al (12). Protein
concentrations were determined using a Bio-Rad protein assay kit
(Hercules, CA, USA). For western blot analysis, aliquots of the
lysate containing 30–50 μg protein were separated by sodium
dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and
then electrotransferred onto a nitrocellulose membrane (Schleicher
and Schuell Bioscience Inc., Keene, NH, USA). The membranes were
subjected to immunoblot analysis and proteins were visualized by an
enhanced chemiluminescence (ECL) method (GE Healthcare). The cell
lysates were separated by 12% SDS-PAGE, transferred onto a
polyvinylidene fluoride membrane (GE Healthcare), blocked with 5%
skimmed milk and hybridized with primary antibodies (diluted
1:1,000). Antibodies against Bax, Bcl-2, caspase-3, caspase-9,
NF-κB, IκB-α, iNOS, COX-2, MMPs and TIMPs were obtained from Santa
Cruz Biotechnology Inc. (Santa Cruz, CA, USA), then incubated with
the horse-radish peroxidase-conjugated secondary antibody (Santa
Cruz Biotechnology Inc.) for 1 h at room temperature. Blots were
washed three times with phosphate-buffered saline with Tween-20
(PBS-T) and then developed by ECL (Amersham Life Science, Arlington
Heights, IL, USA).
Results
Changes following inoculation with U14
cells
Swelling was observed on the cheeks of ICR mice
immediately after inoculation of U14 cells into the buccal mucosa
of ICR mice (Fig. 1C). The
swelling was observed on the inoculation area of the cheeks of ICR
mice on days 1–5 and a similar inflammatory response was observed.
On days 6–10, partial distention were observed on the inoculation
area of the cheeks of ICR mice, with palpable masses; however, the
lymph nodes on the necks were nonpalpable. In addition, primary
foci gradually formed on the cheeks of ICR mice. Ulceration
occurred on the cheek surface of certain mice and cervical lymph
node swelling was identified in several ICR mice on days 11–15
(Fig. 1D). On days 16–20, the
primary foci were further developed on the cheeks of ICR mice and
cervical lymph node swelling was observed in certain mice (Fig. 1E). After 20 days, the inoculated
cheek was larger than the cheek on the other side. Skin surface
erosion occurred on certain mice and primary foci of the carcinoma
were present. In addition, lymph node enlargement was observed in
88.8% of ICR mice to varying extents. Tumors were formed in the
cheek of all ICR mice following inoculation, with no regression in
all cases. The average survival time of ICR mice following
inoculation was 16.40±4.45 days; the longest survival time was 25
days (Table I). Lymph node
enlargement was observed on the necks of partial ICR mice 15 days
after inoculation. Lymph node enlargement to varying extents was
observed on all tumor-formed ICR mice on day 20 and the
pathological results revealed that 8 ICR mice presented lymph node
metastasis at a rate of 53% (Table
II and Fig. 1F).
 | Table IOverall observations of mice
inoculated with U14 squamous cell carcinoma cells. |
Table I
Overall observations of mice
inoculated with U14 squamous cell carcinoma cells.
| Time (days) | No. mice that
survived | Formation of enclosed
buccal mass | Lymphangiectasis |
|---|
| 1–5 | 48 | 12 | 0 |
| 6–10 | 42 | 38 | 0 |
| 11–15 | 29 | 26 | 2 |
| 16–20 | 15 | 15 | 9 |
| >20 | 9 | 9 | 8 |
 | Table IITumor formation rate and lymph node
metastasis rate in ICR mice inoculated with U14 squamous cell
carcinoma cells. |
Table II
Tumor formation rate and lymph node
metastasis rate in ICR mice inoculated with U14 squamous cell
carcinoma cells.
| Time (days) | Tumor formation
ratea (%) | Lymph node metastasis
rateb (%) |
|---|
| 11–15 | 79.3 (23/29) | 0 |
| 16–20 | 100 (15/15) | 53.3 (8/15) |
Histological staining
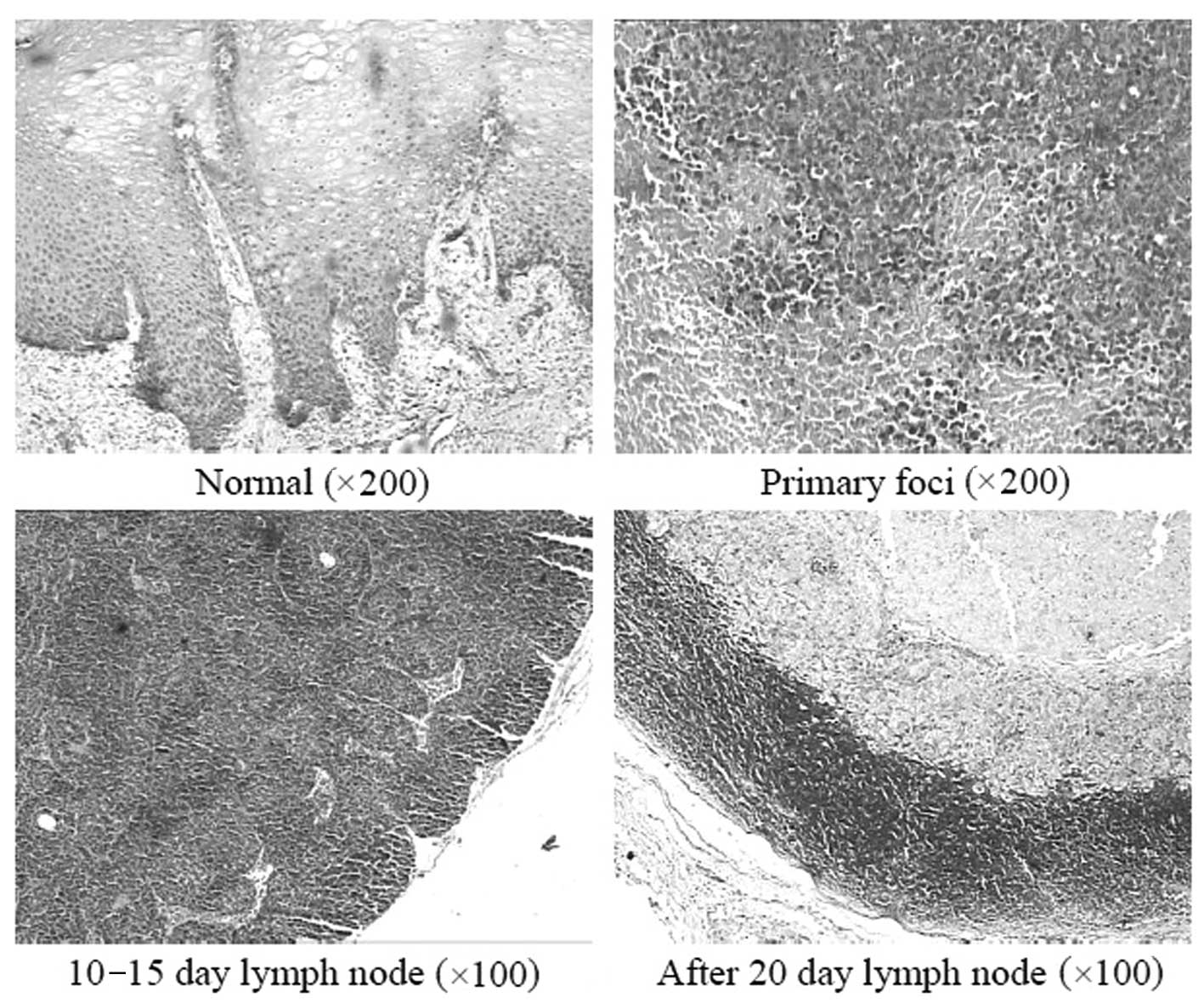
H&E staining revealed that U14 cells firstly
grew along the long axis of the muscle in the inter-muscular space,
then gradually infiltrated into the muscles surrounding the
intermusclar space and submucosa. Finally, the constant
infiltration damaged almost all the muscle tissue and the majority
of the submucosal tissue, and necrosis was observed in certain
tumor areas (Fig. 2).
On days 10–15, there were lymphoid follicles in the
lymph node demonstrating lymph node hyperplasia in the mice. After
15 days, neck lymph node metastasis was observed and after 20 days,
the number of metastatic foci in the neck lymph nodes increased at
the rate of 53%. The early tumor cells were in dense piles or
aligned in the marginal sinus. In the later stage, they developed
from the marginal sinus to the intermediate sinus and modularly
sinus. The whole lymph node structure of the severe cases was
damaged, with little lymphatic tissue left and necrosis in the
central part of the carcinoma tissue. In addition, carcinoma cell
emboli were observed in afferent and efferent lymphatic vessels in
the lymph nodes of certain mice (Fig.
2).
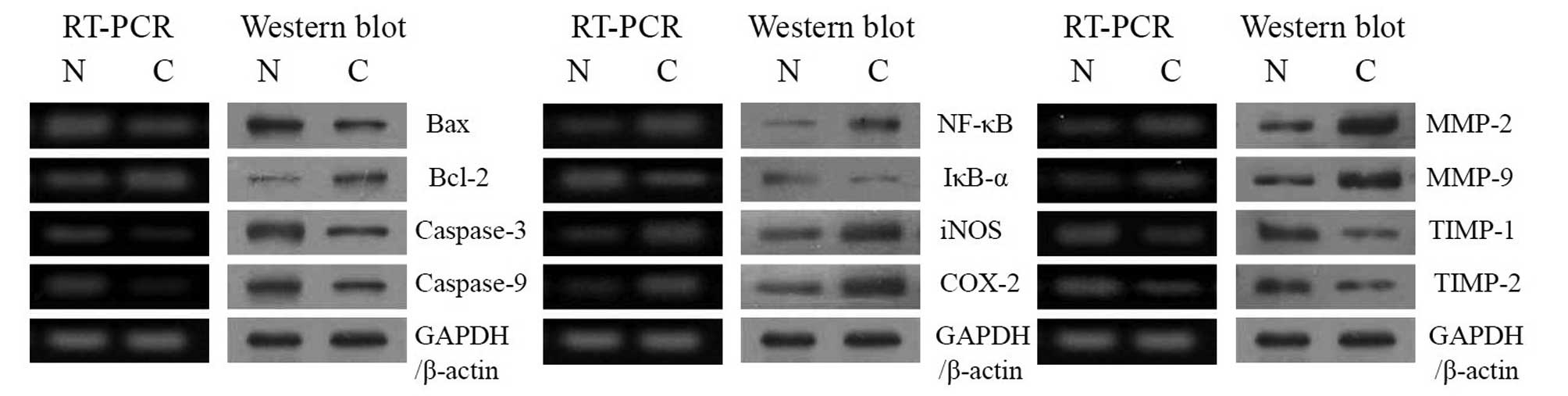
Bax, Bcl-2 and caspase expression
To determine the mechanisms of buccal mucosa cancer,
the expression of Bax, Bcl-2 and caspase genes in buccal mucosa
tissues was determined by RT-PCR and western blot analyses. As
shown in Fig. 3A, in the group
treated with U14 cells (cancer-induced group), the Bax, Bcl-2,
caspase-3 and caspase-9 genes demonstrated significant changes. We
identified a decrease in Bax, an increase in Bcl-2 and a decrease
in caspases in terms of mRNA and protein expressions, compared to
the normal groups.
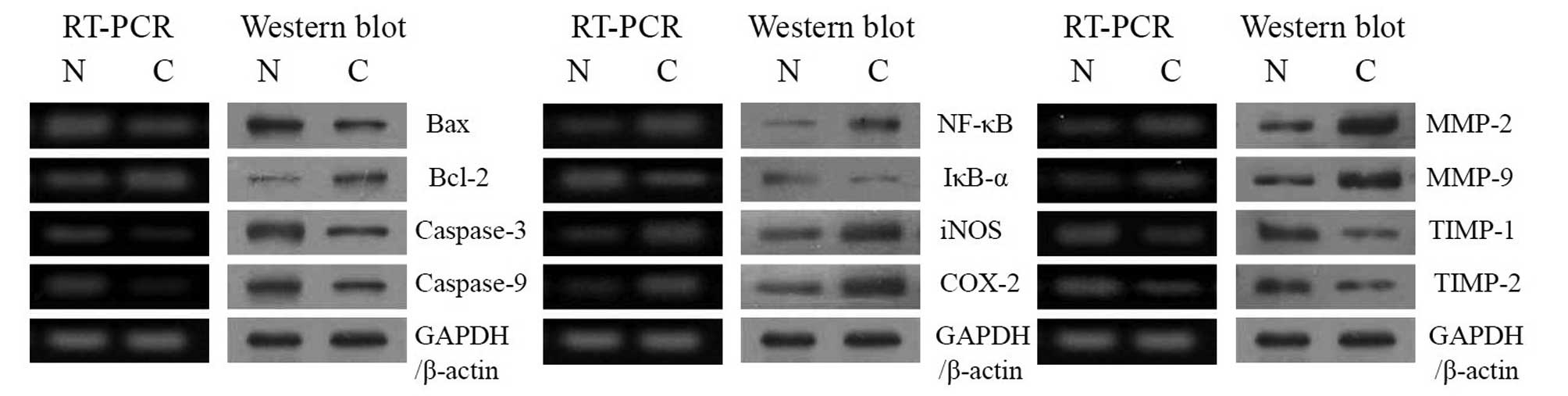 | Figure 3mRNA and protein expression of Bax,
Bcl-2, caspases, NF-κB, IκB-α, iNOS, COX-2, MMPs and TIMPs in
buccal tissues. N, normal group; C, cancer (inoculated with U14
squamous cell carcinoma cells) group. Bcl-2, B cell lymphoma 2;
Bax, Bcl-2-associated X protein; NF, nuclear factor; iNOS,
inducible nitric oxide synthase; COX cycooxygenase; MMP, matrix
metalloproteinase; TIMP, tissue inhibitors of MMPs; GAPDH,
glyceraldehyde 3-phosphate dehydrogenase. |
NF-κB, IκB-α, iNOS and COX-2
expression
RT-PCR and western blot analyses were also conducted
to investigate the level of inflammation resulting from gene
regulation of inflammatory mediators, including NF-κB, IκB-α, iNOS
and COX-2. As shown in Fig. 3B,
NF-κB, iNOS and COX-2 inflammatory mediators were hardly detected
in the normal group, while IκB-α was detected in the normal group.
The mRNA and protein expression of NF-κB was increased, while the
IκB-α mRNA level was decreased in the cancer-induced group.
Additionally, mRNA and protein expression of COX-2 and iNOS
gradually increased following inoculation of U14 cells.
MMP and TIMP expression
RT-PCR and western blot analyses were conducted to
determine whether metastasis in the buccal mucosa cancer model was
a result of gene regulation of metastatic mediators, specifically
MMPs (MMP-2 and MMP-9) and TIMPs (TIMP-1 and TIMP-2). As shown in
Fig. 3C, significantly increased
mRNA expression of MMP-2 and MMP-9 and decreased expression of
TIMP-1 and TIMP-2 was observed in the cancer-induced group.
These changes in mRNA and protein expression
demonstrate that inoculation of U14 cells effectively produces
cancer, inflammation and metastasis in vitro.
Discussion
U14 cells are a squamous cell carcinoma cell line
(6) that was ectopically induced
by treating the uterine cervix with methylcholanthrene thread. They
are able to induce cancer by implantation into the subskin of adult
mice (13). In the early stages,
its structure is similar to a carcinosarcoma. It is considered an
undifferentiated carcinoma, with a metastasis rate of 95% in the
lymph node and 80% in the lungs. Moreover, it is a bidirectional
metastasis tumor strain and an optimum model that is widely used in
studies on tumor metastasis, invasion, recurrence and drug
screening. This tumor strain is characterized by low cell
differentiation, high proliferation, extremely strong infiltration
and metastasis. Additionally, its animal inoculation survival rate
is capable of reaching 100% (6).
With the growth of tumor tissue, the number of open
and expanding peri-cancer lymphatic vessel increases. The vessel
wall has an incomplete structure with an evident gap or clearance.
This is usually observed in the area where tumor cells are
concentrated as it allows the tumor cells to enter into the
lymphatic lumen. This occurs in two ways: a single carcinoma cell
or clusters of carcinoma cells squeeze into the lymphatic lumen
through the open clearance of the complete vessel wall or carcinoma
cells enter into lymphatic lumen by damaging a part of or the
majority of the vessel wall (14).
The former is usually observed 15 days after tumor inoculation and
the latter, which is the main way that carcinoma cells enter the
lymphatic lumen, is observed 20 days after inoculation. In the
meantime, more metastasis foci occur on neck lymph nodes.
Apoptosis is a fundamental cellular event and
understanding its mechanisms of action is likely to enable this
process to be used in tumor diagnosis and therapy (15). In a healthy cell, the
anti-apoptotic protein Bcl-2 is expressed on the outer
mitochondrial membrane surface (16). Caspases form a proteolytic network
within the cell, whereby upstream initiator caspases are activated
early in the apoptotic process (caspase-9) and in turn activate
other downstream caspases (caspase-3). Cytochrome c and
procaspase-9 processing is highly dependent on caspase-3, placing
this caspase in a central position as a regulator of essential
apoptotic pathways in cancer cells (17). Caspase-3 also plays a role as an
amplifier of apoptotic signals, by cleaving Bcl-2 (18). COX-2 plays an important role in
colon carcinogenesis, and NOS, along with iNOS may be a good target
for the chemoprevention of cancer (19). NF-κB is one of the most ubiquitous
transcription factors and regulates the expression of genes
required for cellular proliferation, inflammatory responses and
cell adhesion (20). NF-κB is
present in the cytosol where it is bound to the inhibitory protein,
IκB.
Metastasis is defined as the spread of cancer cells
from one organ or area to another adjacent organ or location
(21). MMPs, a family of
zinc-dependent endopeptidases, play an important role in
tumorigenesis and metastasis. MMPs are able to cleave virtually all
extracellular matrix (ECM) substrates. Degradation of the ECM is a
key event in tumor progression, invasion and metastasis (22). Among the MMP family members, MMP-2
and -9 are important for cancer invasion (23). In fact, inhibition of MMP activity
is useful for controlling tumorigenesis and metastasis (24). TIMPs are naturally occurring
inhibitors of MMPs, which prevent catalytic activity by binding to
activated MMPs, thereby blocking ECM breakdown (25). Disturbances in the ratio between
MMPs and TIMPs have been observed during tumorigenesis (26). MMP-2 and -9 are key factors in
cancer cell invasion and metastasis in vitro (27). Spontaneous and experimental
metastasis to the liver is decreased in mice overexpressing TIMP1
and increased in mice expressing antisense TIMP-1 mRNA (28). Ectopic overexpression of TIMP-1 in
the brains of transgenic mice also reduces experimental metastasis
to the brain (29). In the present
study, the apoptotic, inflammatory and metastatic gene expression
results demonstrated that inoculation of U14 cells induces buccal
mucosa cancer in vivo.
In this study we identified that carcinoma
metastasis firstly encroaches on the marginal sinus, then
infiltrates to the cortex and medulla. The infiltration continues
until normal lymph node structure is completely damaged. Our
results are in agreement with previous studies. Furthermore,
experimental results revealed that, with the reactive hyperplasia
of the lymph node, degeneration and necrosis of large areas is
observed in the tumor area. The neck lymph node of the
cancer-induced mice increased as the experimental time increased
and it became significantly larger after day 15. However,
microscopic inspection revealed that not all the lymph nodes were
affected by metastasis or proliferation of tumor cells and more
than half of them were affected by the reactive hyperplasia of
lymph nodes. This indicates that lymph nodes experience immune
rejection of the tumor following tumor antigen stimulation
(30). However, further study is
required to determine the biological barrier impact of the lymph
node on tumor metastasis.
In this study, carcinoma neck lymph node metastasis
animal models were established. After 20 days, the cheek tumor
formation rate reached 100% and the neck lymph node metastasis rate
was 53%. The metastasis of the tumor to the lymph node occurs as
follows: the carcinoma encroaches on the marginal sinus; then
infiltrates the cortex and medulla. The infiltration continues
until the normal lymph node structure is completely damaged. This
animal model may be used in medical research on buccal mucosa
cancer and cervical lymph node metastasis.
Acknowledgements
This study was supported by the
Chongqing Education Committee [Yukejiao (2010) No.6 KJ100322],
China.
References
|
1
|
Chaturvedi AK, Engels EA, Anderson WF and
Gillison ML: Incidence trends for human papillomavirus-related and
-unrelated oral squamous cell carcinomas in the United States. J
Clin Oncol. 26:612–619. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hong WK, Lippman SM, Itri LM, Karp DD, Lee
JS, Byers RM, Schantz SP, Kramer AM, Lotan R, Peters LJ, Dimery IW,
Brown BW and Goepfert H: Prevention of second primary tumors with
isotretinoin in squamous-cell carcinoma of the head and neck. New
Engl J Med. 323:795–801. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Alam M and Ratner D: Cutaneous
squamous-cell carcinoma. New Engl J Med. 344:975–983. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Duvoux C, Delacroix I, Richardet JP,
Roudot-Thoraval F, et al: Increased incidence of oropharyngeal
squamous cell carcinomas after liver transplantation for alcoholic
cirrhosis. Transplantation. 67:418–421. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mognetti B, Carlo FD and Berta GN: Animal
models in oral cancer research. Oral Oncol. 42:448–460. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gu B, Feng HL, Dong JH, Zhang H, Bian XC
and Liu YQ: The establishment and characterization of a continuous
cell line of mouse cervical carcinoma. Chin J Clin Oncol. 5:44–48.
2008. View Article : Google Scholar
|
|
7
|
Liu XF, Ren LR, Su GY, Liu YQ, Gu B and
Dong JH: Establishment and characterization of a rabbit tumor cell
line VX2. Chinese J Pathol. 34:661–663. 2005.(In Chinese).
|
|
8
|
Su GY, Liu XF, Ren LR, Gu P, Zhang JB and
Liu YQ: Establishment and characterization of a continuous cell
line of mouse breast cancer. Chinese J Clin Oncol. 33:1150–1152.
2006.
|
|
9
|
Rattanasinganchan P, Leelawat K,
Treepongkaruna SA, Tocharoentanaphol C, Subwongcharoen S,
Suthiphongchai T and Tohtong R: Establishment and characterization
of a cholangio-carcinoma cell line (RMCCA-1) from a Thai patient.
World J Gastroenterol. 12:6500–6506. 2006.PubMed/NCBI
|
|
10
|
Schrader M and Laberke HG: Differential
diagnosis of verrucous carcinoma in the oral cavity and larynx. J
Laryngol Otol. 102:700–703. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bak SS, Kong CS, Rhee SH, Rho CW, Kim NK,
Choi KL and Park KY: Effect of sulfur enriched young radish kimchi
on the induction of apoptosis in AGS human gastric adenocarcinoma
cells. J Food Sci Nutr. 12:79–83. 2007. View Article : Google Scholar
|
|
12
|
Kim YA, Rhee SH, Park KY and Choi YH:
Antiproliferative effect of resveratrol in human prostate carcinoma
cells. J Med Food. 6:273–280. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gao J and Zhang JB: Tumor Invasion and
Metastasis. Science Publishing House; Beijing: pp. 531–532.
2003
|
|
14
|
Xuan M, Weng YM, Wang CM and Li XQ:
Pathologic changes of lymphatic capillaries after inoculation of
U14 cells in rat tongue perineoplastic area. West China J Stomatol.
18:5–8. 2000.PubMed/NCBI
|
|
15
|
Milanezi F, Leitão D, Ricardo S, Augusto I
and Schmitt F: Evaluation of HER2 in breast cancer: reality and
expectations. Expert Opin Med Diagn. 3:607–620. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chao DT and Korsmeyer SJ: Bcl-2 family:
regulators of cell death. Annu Rev Immunol. 16:395–419. 1998.
View Article : Google Scholar
|
|
17
|
Blanc C, Deveraux QL, Krajewski S, Jänicke
RU, Porter AG, Reed JC, Jaggi R and Marti A: Caspase-3 is essential
for procaspase-9 processing and cisplatin-induced apoptosis of
MCF-7 breast cancer cells. Cancer Res. 60:4386–4390.
2000.PubMed/NCBI
|
|
18
|
Kirsch DG, Doseff A, Chau BN, Lim DS, de
Souza-Pinto NC, Hansford R, Kastan MB, Lazebnik YA and Hardwick JM:
Caspase-3-dependent cleavage of Bcl-2 promotes release of
cytochrome c. J Biol Chem. 274:21155–21161. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Delić R and Štefanović M: Optimal
laboratory panel for predicting preeclampsia. J Maternal-Fetal
Neonatal Med. 23:96–102. 2010.PubMed/NCBI
|
|
20
|
Baeuerle PA: IkappaB-NF-kappaB structures:
at the interface of inflammation control. Cell. 95:729–731. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Klein CA: Cancer. The metastasis cascade
Science. 321:1785–1787. 2008.PubMed/NCBI
|
|
22
|
Vihinen P, Ala-Aho R and Kahari VM: Matrix
metalloproteinase as therapeurtic targets in cancer. Curr Cancer
Drug Targets. 5:203–220. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Davies B, Waxman J, Wasan H, Abel P,
Williams G, Krausz T, Neal D, Thomas D, Hanby A and Balkwill F:
Levels of matrix metalloproteinase in bladder cancer correlate with
tumor grade and invasion. Cancer Res. 53:5365–5369. 1993.PubMed/NCBI
|
|
24
|
Chen PN, Chu SC, Chiou HL, Kuo WH, Chiang
CL and Hsieh YS: Mulberry anthocyanins, cyanidin 3-rutinoside and
cyanidin 3-glucoside, exhibited an inhibitory effect on the
migration and invasion of a human lung cancer cell line. Cancer
Lett. 235:248–259. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Uzui H, Harpf A, Liu M, Dogerry TM, Shukla
A and Chai N: Increased expression of membrane type 3-matrix
metalloproteinase in human atherosclerotic plaque: role of
activated macrophage and inflammatory cytokines. Circulation.
106:3024–3030. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lambert E, Dasse E, Haye B and Petitfrere
E: TIMPs as multi-facial proteins. Crit Rev Oncol Hematol.
49:187–198. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Deryugina EI and Quigley JP: Matrix
metalloproteinases and tumor metastasis. Cancer Metastasis Rev.
25:9–34. 2006. View Article : Google Scholar
|
|
28
|
Krüger A, Fata JE and Khokha R: Altered
tumor growth and metastasis of a T-cell lymphoma in TIMP-1
transgenic mice. Blood. 90:1993–2000. 1997.PubMed/NCBI
|
|
29
|
Krüger A, Sanchez-Sweatman OH, Martin DC,
Fata JE, Ho AT, Orr FW, Rüther U and Khokha R: Host TIMP-1
overexpression confers resistance to experimental brain metastasis
of a fibrosarcoma cell line. Oncogene. 16:2419–2423.
1998.PubMed/NCBI
|
|
30
|
Liu S, Zhao F and Ben C: Evaluation of
clinical and pathological factors relating to lymph node metastasis
in carcinoma of the tongue. Zhonghua Kou Qiang Yi Xue Za Zhi.
31:259–262. 1996.(In Chinese).
|