Introduction
Acute massive pulmonary embolism (MPE) is a critical
disease associated with high mortality in clinical practice.
Approximately 79% of patients have coincident deep vein thrombosis
(1). Clinically, the disease
mainly manifests as shock and hypotension, and only ∼10% of
patients have syncope as the initial symptom (2,3). We
report on the diagnosis and treatment of a patient with agnogenic
MPE with syncope as the initial symptom.
Case report
A 41-year-old previously healthy female was admitted
to the Department of Neurology, Taizhou People’s Hospital in March
2012, for two transitory episodes of syncope during a 5-h period.
The patient had an unhealthy lifestyle of physical inactivity. No
urinary and fecal incontinence, general fatigue, chest pain,
breathing difficulty, hemoptysis or fever were observed during the
course of disease. Following admission, physical examinations
revealed a body weight of 75 kg, body height of 159 cm, body
temperature of 36.0°C, pulse of 80 bpm, respiratory rate of 23 bpm
and blood pressure of 120/60 mmHg. The patient had a slightly
haggard expression, no cyanosis of the lips and no jugular vein
distention. Bilateral respiratory movements were identical and
vocal fremitus was equal. Dullness was heard in the right lower
lung on percussion. Breath sounds were diminished and no moist
rales were heard. The patient’s heart rhythm was regular, P2>A2
(pulmonary second sound was higher than aortic second heart sound)
and there was no edema in the lower extremities.
A complete blood test revealed a white cell count of
11.21×109 cells/l and the percentage of large white
blood cells was 57.2%. Biochemical tests revealed 1.4 mmol/l
triglycerides, 0.75 mmol/l high-density lipoprotein and 3.61 mmol/l
low-density lipoprotein. Blood gas analysis revealed a pH of 7.471,
61.1 mmHg PaO2, 23.5 mmHg PaCO2 and 18.2
mmol/l HCO3− (under the condition of a low
flow rate of oxygen inhalation). Chest radiographs revealed
pulmonary hilar enlargement and a broadened shadow on the right
superior pulmonary artery. An electrocardiogram revealed a flat
V1–V3 T wave and magnetic resonance angiography of the head
revealed ∼60% luminal stenoses of the right posterior cerebral
artery and the left external carotid artery.
After admission, ‘reflex syncope’ was suspected and
the patient was administered oral calcium antagonists (Nimotop 30
mg qd) and intravenous Alprostadil for injection (Alprostadil 10
μg qd) to boost the cerebral circulation, without effect. A
further episode of syncope occurred during the 18 h after admission
and the patient was transferred to the Department of Respiratory
Medicine for a D-dimer assay, which indicated a value of 1,200
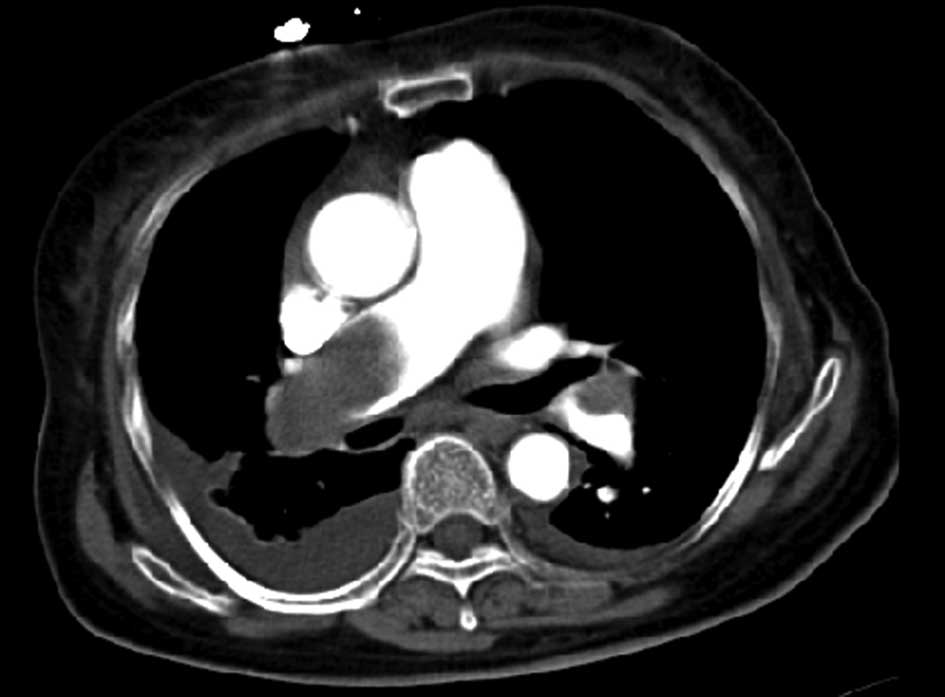
μg/l. An enhanced chest computed tomography (CT) scan
revealed filling defects in the right main pulmonary and left
inferior pulmonary arteries, as well as bilateral pleural effusion
(Fig. 1). Color ultrasonography of
the heart revealed a dilated right ventricle and right heart
overload, severe tricuspid regurgitation and severe pulmonary
hypertension and the systolic pulmonary arterial pressure was 130
mmHg (Fig. 2). The patient was
finally diagnosed with MPE.
Following confirmation, the patient underwent
interventional mechanical thrombectomy combined with local and
systematic thrombolytic therapy with low-dose urokinase.
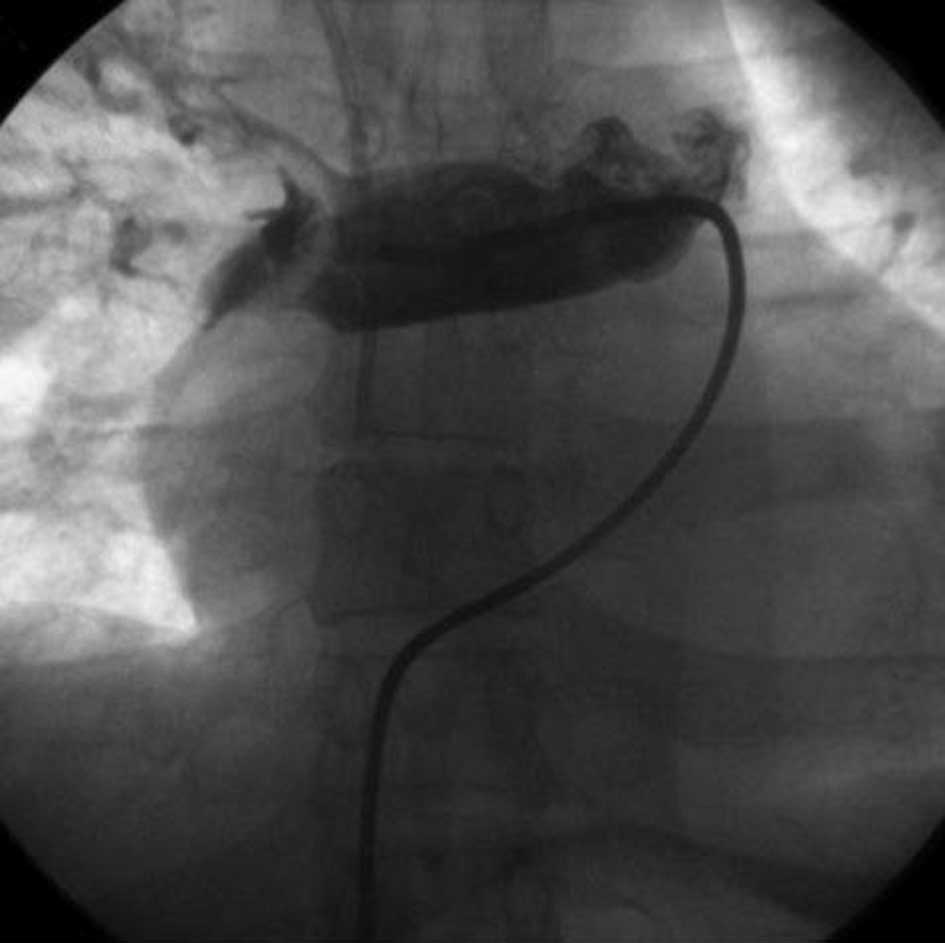
Following the above therapies, digital subtraction
angiography (DSA) of the deep veins of the lower limbs and the
inferior vena cava demonstrated unobstructed blood flow, with no
apparent thrombosis. A 4–5F double J tube was inserted through the
right femoral vein to the main pulmonary artery for DSA of the
pulmonary artery, to confirm the filling defect in the right main
pulmonary artery (Fig. 3). An
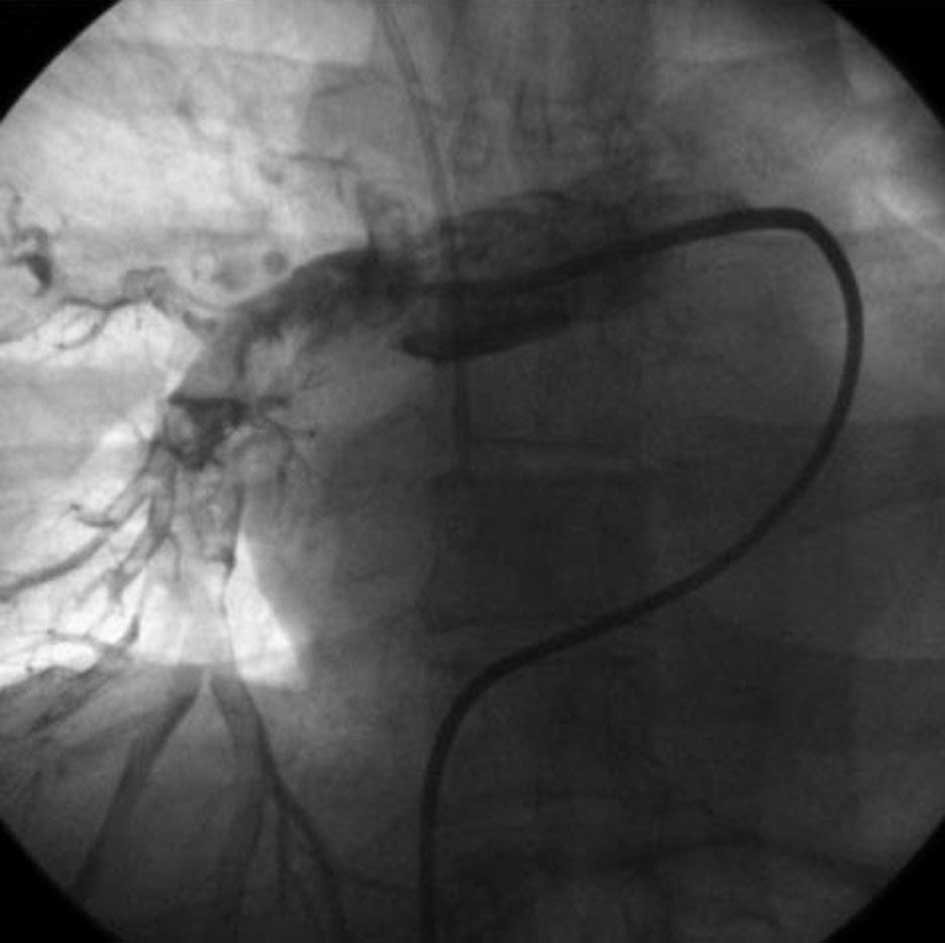
exchange guide wire was then inserted to coordinate with the tube
for twists and drags to disintegrate the embolus. Following
disintegration of the embolus, 500,000 units urokinase were
injected into the tube for thrombolysis over 30 min. Subsequent DSA
of the pulmonary artery indicated an improvement in the filling
defect compared with before treatment (Fig. 4). The patient’s condition was
significantly alleviated and the anoxia was reduced. A blood gas
assay performed 2 h after surgery indicated a pH of 7.51, 72 mmHg
PaO2, 29 mmHg PaCO2 and 23.1 mmol/l
HCO3− (under the condition of a low flow rate
of oxygen inhalation).
A postoperative intravenous drip of low-dose
urokinase (200,000 units) was initiated and the patient was also
treated with 5,000 units low-molecular-weight heparin, administered
subcutaneously once every 12 h for three consecutive days. Warfarin
(2.5 mg) was administered orally once every 12 h on a daily basis.
The prothrombin time (PT) and international normalized ratio (INR)
were monitored; when the PT and INR were twice and 2.5 times their
respective normal levels, warfarin therapy was administered singly,
plus anti-infective, supportive and oxygen therapies.
Three days after surgery, the patient demonstrated a
distinctly improved mental condition with no further syncopal
attacks. An enhanced chest CT scan 10 days after surgery revealed
evident improvement of the thrombosis in the right main pulmonary
artery and left inferior pulmonary artery branch, as well as
disappearance of the pleural effusion, compared with the previous
chest CT scan (Fig. 5). Color
ultrasonography revealed a significant decrease of pulmonary artery
pressure and right heart load; the systolic pulmonary arterial
pressure was 71 mmHg. The patient was discharged from hospital 26
days after admission, with continued daily administration of 2.5 mg
warfarin. Based on the monitoring of PT and INR, the doctor
suggested discontinuation of warfarin 3 months after hospital
discharge. The study was approved by the Ethics Committee of
Taizhou People’s Hospital, Jiangsu, China and according to the
Declaration of Helsinki. Written informed consent was obtained from
the patient.
Discussion
MPE refers to an embolism of the main pulmonary
trunk and is associated with high mortality (4,5). The
main clinical manifestations usually include shock and hypotension
as the initial symptoms, commonly with comorbid right heart
dysfunction. The embolus mainly arises from the deep vein system of
the lower limbs or right heart system, or from the deep veins of
the upper limbs (6). MPE caused by
uncertain risk factors is rarely reported. The patient presented in
this study was otherwise healthy and had no predisposing factors to
embolism, with normal blood lipid levels. There were no distinct
signs of embolism on DSA of the deep lower limb veins or inferior
vena cava or in B-ultrasound examination of the upper limbs. A
complete enhanced CT scan of the abdomen revealed no abnormalities.
We consider that the possible causes may be: i) long periods of
time sitting everyday and an unhealthy lifestyle of physical
inactivity resulted in a higher risk of developing a
life-threatening blood clot in the lungs than that in active women
(7). ii) Although ∼79% of patients
who present with pulmonary embolism have evidence of deep venous
thrombosis in their legs, if deep venous thrombosis is not detected
in such patients, it is likely that the whole thrombus has already
detached and embolised (1).
Nonetheless, this patient represented a rare clinical presentation,
which is often neglected by clinicians as a result of missed and
incorrect diagnoses.
Syncope as the sole initial symptom has been
reported in MPE patients with comorbid hemodynamic disturbances
(3,8,9).
There are several possible causes: i) acute right heart failure and
damaged pulmonary blood perfusion causing decreased filling of the
left ventricle, with resulting hypotension, bradycardia and
cerebral circulation disturbance (10). ii) Reflex syncope caused by
bradycardia due to vagal stimulation and by peripheral vascular
distention due to suppression of sympathetic nerves (11) and iii) syncope caused by an
atrioventricular block induced by MPE (12). In the present case, the patient’s
clinical manifestation was transitory syncope closely associated
with activities. Considering its duration of onset, modes of relief
and basic conditions, the patient may easily have been misdiagnosed
with syncope due to a nervous system disease, thus missing the
precious opportunity for treatment. When the cause of syncope
remains unknown, timely D-dimer assay and blood gas analysis
effectively reduces the risk of a missed or inaccurate
diagnosis.
MPE combined with hemodynamic disturbance is an
absolute indication of thrombolysis; although thrombolytic therapy
via a peripheral vein has a delayed effect and a high risk of
hemorrhage. Certain patients are unable to benefit from this
treatment due to contraindications to thrombolysis. Surgical
thrombectomy of the pulmonary artery is also associated with high
mortality and disability risks (13). However, advances in interventional
therapies and instruments mean that the interventional treatment of
acute MPE has achieved satisfactory effects and has received
increasing attention (14). The
usual methods include local pulmonary thrombolysis via a catheter,
mechanical embolus disintegration and thrombectomy via a
catheter.
Compared with venous thrombolysis, local pulmonary
artery thrombolysis via a catheter elevates the focal drug
concentration and reduces the required dosage of thrombolytic
medications, thus enhancing the therapeutic effects and reducing
the incidence of hemorrhagic complications. The procedure of
mechanical embolus disintegration and thrombectomy by a catheter
permits the clearance of embolus fragments and entry into the
distal pulmonary artery, realizes the unblocking of the clogged
central pulmonary artery, improves pulmonary perfusion, reduces
pulmonary artery pressure and improves right ventricular function,
consequently resulting in an increased clinical treatment success
rate.
In conclusion, the occurrence of syncope as the sole
initial symptom in a previously healthy patient with no
predisposing factors to embolism and no hemodynamic instability
following admission is extremely rare, which may have been a factor
in the delayed diagnosis of pulmonary thromboembolism. In this
situation, the raised awareness of diagnosis and knowledge
concerning the clinical presentation of pulmonary thromboembolism
are key factors in ensuring an immediate diagnosis and adequate
intervention.
References
|
1.
|
Tapson V: Acute pulmonary embolism. N Engl
J Med. 358:1037–1052. 2008. View Article : Google Scholar
|
|
2.
|
Calvo-Romero JM, Pérez-Miranda M and
Bureo-Dacal P: Syncope in acute pulmonary embolism. Eur J Emerg
Med. 11:208–209. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Castelli R, Tarsia P, Tantardini C,
Pantaleo G, Guariglia A and Porro F: Syncope in patients with
pulmonary embolism: comparison between patients with syncope as the
presenting symptom of pulmonary embolism and patients with
pulmonary embolism without syncope. Vasc Med. 8:257–261. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Wood KE: Major pulmonary embolism: review
of a pathophysiologic approach to the golden hour of
hemodynamically significant pulmonary embolism. Chest. 121:877–905.
2002. View Article : Google Scholar
|
|
5.
|
Schoepf UJ, Kucher N, Kipfmueller F,
Quiroz R, Costello P and Goldhaber SZ: Right ventricular
enlargement on chest computed tomography: a predictor of early
death in acute pulmonary embolism. Circulation. 110:3276–3280.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Basat HC, Kalem M, Binnet MS and Demirtas
M: Pulmonary thromboembolism after surgical treatment of ulnar
pseudoarthrosis: a case report. Acta Orthop Traumatol Turc.
45:284–287. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Kabrhel C, Varraso R, Goldhaber SZ, Rimm E
and Camargo CA Jr: Physical inactivity and idiopathic pulmonary
embolism in women: prospective study. BMJ. 343:d38672011.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Mahboobi SK and Shohat EZ: Syncope: an
unusual presentation of acute pulmonary embolism. South Med J.
98:845–846. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Sarasin FP, Louis-Simonet M, Carballo D,
Slama S, Rajeswaran A, Metzger JT, et al: Prospective evaluation of
patients with syncope: a population-based study. Am J Med.
111:177–184. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Gossage JR: Early intervention in massive
pulmonary embolism. A guide to diagnosis and triage for the
critical first hour. Postgrad Med. 111:27–28. 2002.PubMed/NCBI
|
|
11.
|
Eldadah ZA, Najjar SS and Ziegelstein RC:
A patient with syncope, only ‘vagally’ related to the heart. Chest.
117:1801–1803. 2000.
|
|
12.
|
Elias J, Kuniyoshi R, Moulin B, et al:
Syncope and complete atrioventricular block related to pulmonary
thromboembolism. Arq Bras Cardiol. 83:438–441. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Pulido-Zamudio T, Reyes-Fuentes LF,
Beltrán-Gámez M, et al: Management of acute pulmonary
thromboembolism. Arch Cardiol Mex. 82:48–53. 2012.(In Spanish).
|
|
14.
|
Skaf E, Beemath A, Siddiqui T, Janjua M,
Patel NR and Stein PD: Catheter-tip embolectomy in the management
of acute massive pulmonary embolism. Am J Cardiol. 99:415–420.
2007. View Article : Google Scholar : PubMed/NCBI
|