Introduction
The upper cervical spine is an anatomically and
biomechanically unique area. Metastatic involvement in this region
is uncommon and few studies have been published to direct the
treatment of it. Although the improvement in adjuvant therapy has
led to a reduction in the number of patients requiring surgery for
metastatic disease, surgery remains critical in the treatment of
metastatic spinal tumors (1). The
indications that surgical intervention of upper cervical lesions is
required include evidence of gross instability due to fracture or
bony destruction, gross malalignment, neurologic compromise due to
malalignment or tumor compression, and a life expectancy of >3
months. Due to the close proximity to the neurovascular and soft
tissues of the upper cervical spine, the resection and
reconstruction of a metastatic tumor is challenging for spinal
surgeons.
The majority of C2 metastatic tumors invade the
vertebral body and the anterior approach often represents the most
direct route to the lesion (2).
Consequently, a transoral approach (3) or a transmandibular approach (4) is often employed, which provides
direct access to the upper cervical region. However, the transoral
approach has a high risk of infection, and it is difficult to
perform the fixation extended to C3 due to the obstruction of the
tongue and the jaw. The transmandibular approach is inappropriate
for patients with a limited life expectancy due to the long time
period required for bone healing. Furthermore, due to the limited
life expectancy of patients with metastatic tumors, the main
purpose of surgery is to improve life quality, and an approach with
numerous complications and large trauma does not satisfy this
requirement.
The high anterior retropharyngeal approach is an
extension of surgical exposure to the lower cervical spine,
allowing exposure from the ventral arch of C1 continuously to the
lower cervical spine (5–7). It is entirely extraoral and
extramucosal and is used for decompression of the spinal canal as
well as for stabilization. The present study reports a successful
outcome following a single-stage combined anterior retropharyngeal
and posterior approach for resection of a C2 metastatic tumor and
reconstruction of spinal stability.
Case report
A 44-year-old male was admitted to the Affiliated
Hospital of Medical College, Qingdao University (Qingdao, China)
after experiencing severe neck pain for one month. The patient
complained of intolerable pain in the occipitocervical area. The
pain did not radiate to the upper extremities, and cervical motion
was limited in all directions by pain and muscle spasm. Examination
identified a spasmodic neck muscle and the neurological examination
was normal. This study was conducted in accordance with the
Declaration of Helsinki and with approval from the Ethics Committee
of the Affiliated Hospital of Medical College, Qingdao University.
Written informed consent was obtained from the participant.
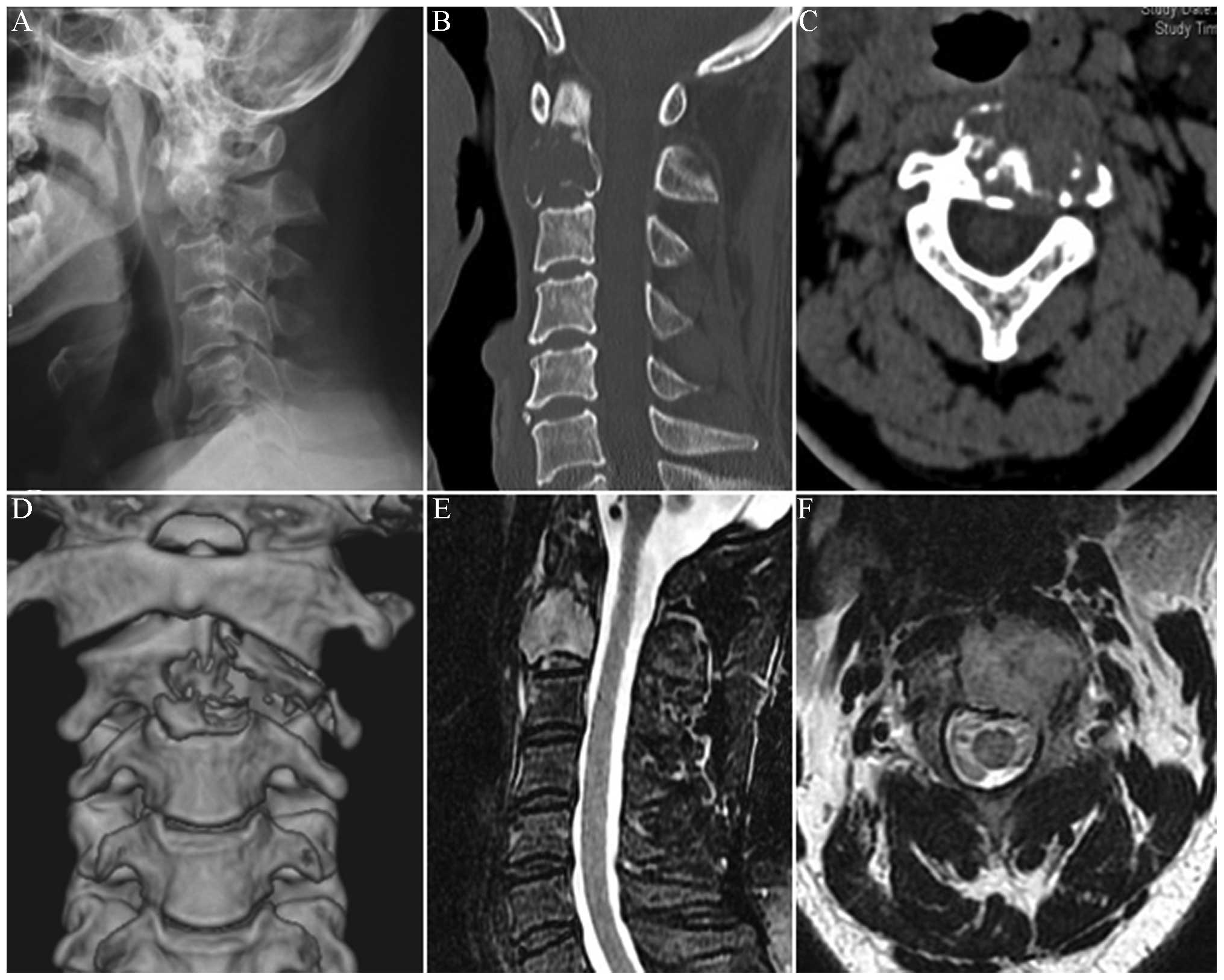
X-ray showed a poorly demarcated lesion of the C2
vertebral body (Fig. 1A). Computed
tomography (CT) scanning and CT three-dimensional (3D)
reconstruction confirmed an erosive lesion of the left C2 vertebral
body and the left transverse process with surrounding soft tissue
mass (Fig. 1B–D). Magnetic
resonance imaging (MRI) showed that the lesion extended from the
vertebral body to the neural foramen and the transverse process.
The brainstem and the cervical spinal cord were not compressed
(Fig. 1E and F). Bone scan
demonstrated diffuse increased uptake of the isotope at the level
of the C2 vertebra, without other abnormalities elsewhere in the
skeleton (Fig. 2). CT angiography
identified that the left vertebral artery (VA) was topically
encapsulated by the tumor and displaced, but did not show any
pathological vascularization (Fig.
3). Enhanced CT of the upper abdomen identified a lesion in the
liver. The C2 metastatic tumor was distributed to layers A–D and
sectors 3–7 according to the Weinstein-Boriani-Biagini
classification (8), and was in
Category IV according to the Harrington classification system
(9).
Following consultation with the general surgeon and
medical oncologist and extensive discussion with the patient and
their family regarding the risks and benefits of surgery, the
decision was made to perform the surgery by a combined anterior
retropharyngeal and posterior cervical approach with somatosensory
evoked potential monitoring. Following endotracheal intubation, the
patient was positioned prone with skull traction to maintain spinal
stability and a conventional posterior cervical approach was taken
through a midline incision from the occiput to the C4 spinous
process. Care was taken not to detach the paraspinal musculature
from its insertion of the C2 spinal process. The left C2 facet and
part of the left lateral C2 lamina were resected to decompress the
C3 nerve root and to identify the destroyed left transverse process
and the tumor surrounding it. The left transverse process and part
of the tumor were resected in a piecemeal fashion to expose the
left VA. Gelfoam and absorbable hemostatic gauze (Ethicon, San
Lorenzo, PR, USA) were placed ventrally to the left VA and the left
C3 nerve root over the tumor bed to prevent their accidental injury
in the subsequent anterior approach. Posterior fixation was
fulfilled by the placement of a polyaxial screw of an appropriate
length into the right lateral mass of C1–4 and the left lateral
mass of C1 and C4. The wound was closed in layers over a suction
drain. Subsequently, the patient was turned to a supine position
and a high anterior retropharyngeal approach was taken. The skin
incision was made along the inferior edge of the mandible back to
the ventral edge of the sternocleidomastoid muscle. The tumorous C2
vertebral body was resected by corpectomy. The edges of the tumor
were identified and a intralesional extracapsulary resection was
performed. A 12-mm-diameter titanium cage (Medtronic, Memphis, TN,
USA) filled with polymethylmethacrylate cement was inserted in the
space between the anterior arch of C1 and the upper endplate of the
C3 vertebral body. A titanium cervical plate was then placed
between the C1 anterior arch and the C3 vertebral body. The wound
was closed in layers over a suction drain in the retropharyngeal
space. The surgery time was 5 h, and the estimated blood loss was
1,000 ml.
Following the surgery, a Philadelphia collar was
applied to the patient and the severe neck pain disappeared.
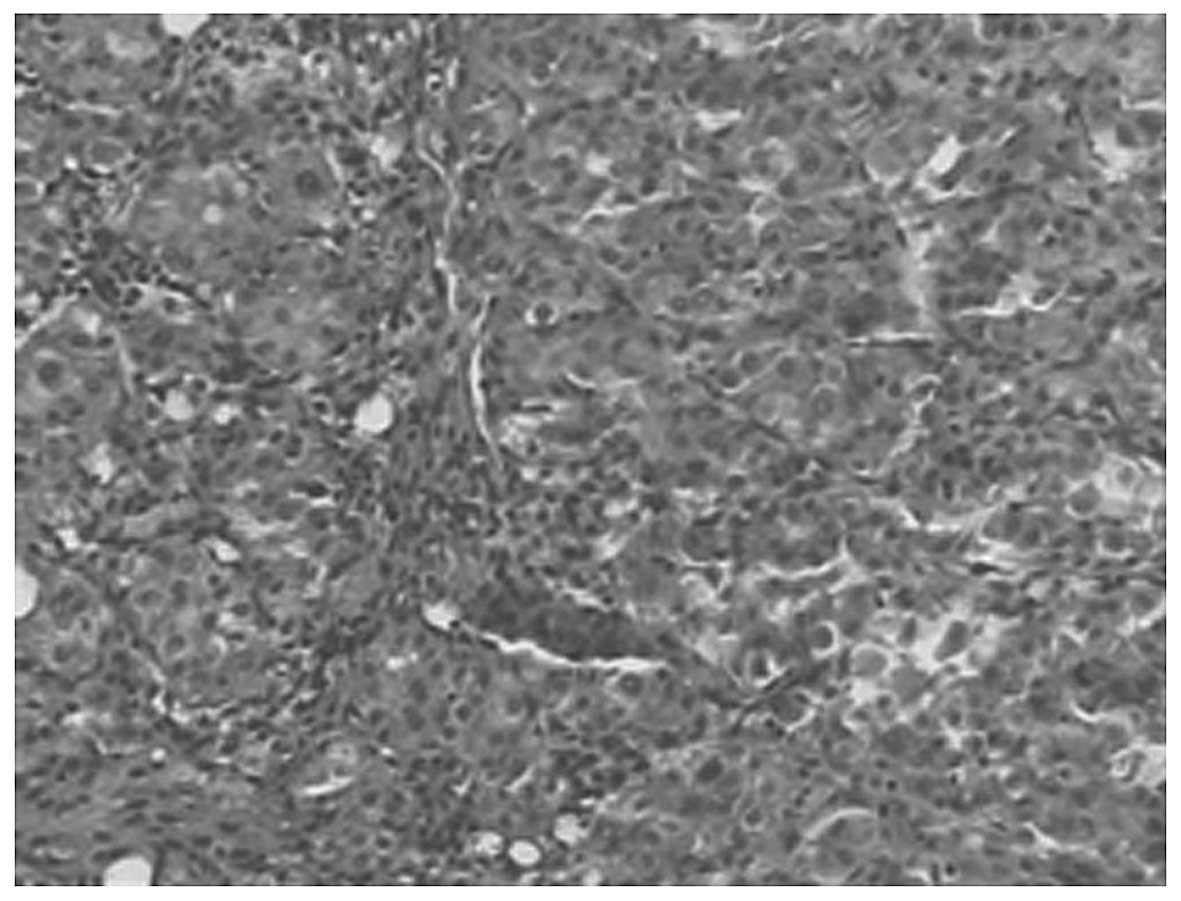
Pathological examination confirmed moderately differentiated
hepatocellular liver cancer (Fig.
4). Two weeks after the surgery, the patient received
transcatheter arterial chemoembolization. The six-month follow-up
X-ray (Fig. 5A) and CT 3D
(Fig. 5B and C) showed no signs of
implant dislocation and indicated persisting clinical success.
Discussion
To the best of our knowledge, involvement of the
upper cervical spine in metastases is uncommon and the literature
review information regarding C2 metastasis consists of only a few
case reports (14,17,18).
Surgical intervention of C2 metastasis is a significant challenge
for spinal surgeons.
Several approaches have been described for access to
the upper cervical spine. The transoral approach, which provides
the direct exposure for anterior decompression of the spinal cord
and brainstem of the upper cervical spine, is most useful for
resection of small, ventrally based tumors. However, it has a high
risk of infection and it is difficult to perform the fixation
extended to C3 due to the obstruction of the tongue and jaw
(10). The transmandibular
approach or its variations, which offer a wider exposure in the
upper cervical region, are alternatives to the transoral route
(3). However, it requires
splitting of the mandible and thus is inappropriate for patients
with limited life expectancy due to the long time period of bone
healing required. Furthermore, several complications, such as
velopharyngeal dysfunction, pharyngeal wound dehiscence, lingual
neuropathy and cosmetic deformity have been reported in certain
studies (11,12). The lateral retropharyngeal approach
obtained with the retrovascular approach is not as direct as the
anterior approach and it is difficult to perform long-segment
anterior reconstruction (13). The
posterior approach also has been reported to treat ventrally
located upper cervical spine tumors, yet it does not provide
adequate exposure of the tumor around the anterior midline. The
high anterior retropharyngeal approach is an extension of the
surgical exposure to the lower cervical spine, allowing exposure
from the ventral arch of C1 continuously to the lower cervical
spine. It has been demonstrated to be effective for C2 lesion
resection and fixation to treat trauma, deformity and chronic
inflammatory diseases. As far as C2 metastasis is concerned, few
cases have been reported (14).
In the present study, the posterior approach was
employed to resect part of the tumor and fulfill the posterior
fixation to reinforce spinal stability during the position change
of the patient. Subsequently the high anterior retropharyngeal
approach was chosen to resect the ventrally located metastatic
tumor and fulfill the reconstruction of the spinal alignment. It
has been suggested that concomitant anterior and posterior fixation
enhance the immediate stability of the spine (15). Preoperatively, it is important to
evaluate the vascularity of the tumor and the association of the
tumor mass with the vertebral arteries. As magnetic resonance
angiography or CT angiography is less invasive and easier to
conduct, digital subtraction angiography is rarely used to evaluate
the vascularity of the lesion. Preoperative embolization is helpful
in reducing intraoperative bleeding when an intralesional procedure
is planned, but it is performed only rarely due to common
vascularity with the cervical cord and should be only performed in
experienced institutions (16). In
the present study, CT angiography was used to evaluate the
vascularity of the tumor and the association of the tumor mass with
the vertebral arteries. There was no main arterial supply to the
tumor, so preoperative embolization was not performed. During the
surgery, Gelfoam and absorbable hemostatic gauze were placed
ventrally to the left VA over the tumor bed to prevent accidental
injury in the subsequent anterior approach.
The treatment of patients with metastatic disease of
the cervical spine requires multidisciplinary cooperation between
treatment team members, including a pathologist, medical and
radiation oncologists and the spinal surgeon. In the present study,
a combined posterior and high anterior retropharyngeal approach was
used to resect a C2 metastatic tumor. This does not signify that
other approaches are unsuitable for the resection and
reconstruction of C2 metastasis; each case should be considered
individually to determine the most appropriate surgical approach.
If surgery is considered, the following factors should be taken
into consideration when choosing the surgical approach: The
experience of the surgeon, the life expectancy of the patient, the
location, size and extent of the tumor, the stability of the spine
and the neurological involvement.
References
|
1
|
Laufer I, Sciubba DM, Madera M, Bydon A,
Witham TJ, Gokaslan ZL and Wolinsky JP: Surgical management of
metastatic spinal tumors. Cancer Control. 19:122–128.
2012.PubMed/NCBI
|
|
2
|
Harrington KD: Anterior cord decompression
and spinal stabilization for patients with metastatic lesions of
the spine. J Neurosurg. 61:107–117. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hsu W, Wolinsky JP, Gokaslan ZL and
Sciubba DM: Transoral approaches to the cervical spine.
Neurosurgery. 66(Suppl 3): 119–125. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Logroscino CA, Casula S, Rigante M and
Almadori G: Transmandibular approach for the treatment of upper
cervical spine metastatic tumors. Orthopedics. 27:1100–1103.
2004.PubMed/NCBI
|
|
5
|
Smith GW and Robinson RA: The treatment of
certain cervical-spine disorders by anterior removal of the
intervertebral disc and interbody fusion. J Bone Joint Surg Am.
40-A:607–624. 1958.PubMed/NCBI
|
|
6
|
McAfee PC, Bohlman HH, Riley LH Jr,
Robinson RA, Southwick WO and Nachlas NE: The anterior
retropharyngeal approach to the upper part of the cervical spine. J
Bone Joint Surg Am. 69:1371–1383. 1987.PubMed/NCBI
|
|
7
|
Laus M, Pignatti G, Malaguti MC, Alfonso
C, Zappoli FA and Giunti A: Anterior extraoral surgery to the upper
cervical spine. Spine (Phila Pa 1976). 21:1687–1693. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Boriani S, Weinstein JN and Biagini R:
Primary bone tumors of the spine. Terminology and surgical staging.
Spine (Phila Pa 1976). 22:1036–1044. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Harrington KD: Metastatic disease of the
spine. J Bone Joint Surg Am. 68:1110–1115. 1986.
|
|
10
|
Balasingam V, Anderson GJ, Gross ND, et
al: Anatomical analysis of transoral surgical approaches to the
clivus. J Neurosurg. 105:301–308. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rhines LD, Fourney DR, Siadati A, Suk I
and Gokasla ZL: En bloc resection of multilevel cervical chordoma
with C-2 involvement. Case report and description of operative
technique. J Neurosurg Spine. 2:199–205. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Konya D, Ozgen S, Gerçek A, Celebiler O
and Pamir MN: Transmandibular approach for upper cervical
pathologies: report of 2 cases and review of the literature. Turk
Neurosurg. 18:271–275. 2008.PubMed/NCBI
|
|
13
|
Fong S and DuPlessis SJ: Minimally
invasive anterior approach to upper cervical spine: surgical
technique. J Spinal Disord Tech. 18:321–325. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yang X, Wu Z, Xiao J, et al: Sequentially
staged resection and 2-column reconstruction for C2 tumors through
a combined anterior retropharyngeal-posterior approach: surgical
technique and results in 11 patients. Neurosurgery. 69(2 Suppl
Operative): ons184–ons194. 2011.
|
|
15
|
Melcher RP and Harms J: Biomechanics and
materials of reconstruction after tumor resection in the spinal
column. Orthop Clin North Am. 40:65–74. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Deshmukh VR, Fiorella DJ, Albuquerque FC
and McDougall CG: Embolization techniques for neoplasms of the
spine and spinal cord. Spinal Cord and Spinal Column Tumors:
Principles and Practice. Dickman CA, Fehlings MG and Gokaslan ZL:
Thieme Medical Publishers, Inc; New York, NY: pp. 204–213. 2006
|
|
17
|
Eleraky M, Setzer M and Vrionis FD:
Posterior transpedicular corpectomy for malignant cervical spine
tumors. Eur Spine J. 19:257–262. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Colak A, Kutlay M, Kibici K, Demircan MN
and Akin ON: Two-staged operation on C2 neoplastic lesions:
anterior excision and posterior stabilization. Neurosurg Rev.
27:189–193. 2004. View Article : Google Scholar : PubMed/NCBI
|