Introduction
Liver cancer is one of the most common type of
malignant tumor and is associated with a high mortality rate.
Primary treatment methods include surgery, chemotherapy and
ablation therapy. Radiofrequency ablation (RFA) therapy is
considered to be a minimally invasive and localized treatment
approach and its efficiency has been confirmed in a number of
studies (1–3). With regard to early primary liver
cancer, the effect of RFA treatment is comparable to that of
surgical treatment (4–7). However, whether RFA is able to
achieve the same therapeutic effect for metastatic liver cancer
(MLC) tumors that are <5 cm in diameter is unknown. Therefore,
the present study observed the treatment of patients with MLC and
analyzed ~8 years of treatment data and the long-term follow-up of
these patients.
Materials and methods
Patients and lesions
Between August 2005 and May 2013, 56 patients with
liver cancer underwent ultrasound (US)-guided RFA in the Department
of Ultrasound of Beijing Friendship Hospital (Beijing, China). The
patients included: i) 34 cases of hepatocellular carcinoma (HCC)
which consisted of 18 class-A, 14 class-B and two class-C cases,
based on the 2010 American Association for the Study of Liver
Diseases (AASLD) (8); ii) 22 cases
of MLC which consisted of primary tumors located in the
gastrointestinal tract (14 cases), kidney (two cases), lung (one
case) and five cases from other locations. Diagnostic procedures
were performed and included contrast-enhanced abdominal computed
tomography (CT) scans, magnetic resonance imaging (MRI) and/or a
liver tumor biopsy employing US guidance. There were 43 male and 13
female patients, aged between 25 and 83 years (average age,
56.3±6.5 years) with tumor sizes ranging from 1.2 to 4.7 cm
(average size, 3.2±0.8 cm). The exclusion criteria were as follows:
i) The patient suffered from severe jaundice or ascites; ii) the
patient suffered from severe liver and kidney dysfunction; iii)
huge liver cancer (>5 cm) or patients with diffuse liver cancer
and iv) the patient suffered from coagulation dysfunction or severe
bleeding tendencies. This study was conducted in accordance with
the Declaration of Helsinki. Approval was obtained from the Ethics
Committee of Beijing Friendship Hospital. All patients provided
written informed consent for participation in this study.
RFA procedure and treatment
A pre-operative US or CT scan was performed to
determine the tumor location, size and number. RFA was performed
using a multitined RITA® StarBurst® device
(RITA Medical Systems, Inc., Mountain View, CA, USA). Following
routine disinfection procedures and an intravenous general
anesthetic (propofol), the US-guided radiofrequency needle (with
numerous fine-needle electrodes capable of expanding between 2.0
and 5.0 cm in diameter) was applied to the surface of the tumor.
Gradual expansion of the needle, according to the size of the
tumor, occurred until a pre-defined temperature (105°C) was
reached. Hyperechoic changes within the tumor and the surrounding
tissue were observed after ~15–20 min at which point the electrode
was removed, and then heat to seal the needle tract. For tumors
<3 cm in diameter, a single needle puncture at a single point
was sufficient. However, for a tumor with a diameter of >3 cm,
the treatment was required to extend beyond the tumor foci and the
surrounding 1.0–2.0 cm; therefore, multi-point puncturing was
conducted in order to ensure complete tumor ablation.
Evaluation of therapeutic effect
Two weeks following the RFA treatment, an enhanced
CT scan review was carried out. If the images of the ablated
lesions on the arterial and portal regions of the liver exhibited
no significant increases, it was determined that complete ablation
had been achieved. If the edges of ablated lesions exhibited
abnormal enhancement and color Doppler US examination demonstrated
partial blood flow of the ablated lesion, then incomplete ablation
was diagnosed and further treatment was required. Following 1 month
of treatment, regular blood tests (for detection of liver function
and α-fetoproteins) and imaging studies (abdominal enhanced CT
and/or US imaging) were performed as a basis for the evaluation of
tumor development. Subsequent to complete ablation of the lesion,
the re-emergence of the blood supply and contrast enhancement at
the location of the original lesion was considered to indicate
localized tumor recurrence. Abnormal enhancement showing the
presence of lesions outside the region occupied by the primary
tumors was considered to indicate distant tumor recurrence. The
follow-up period ranged between 1 and 93 months.
Statistical analysis
The 1-, 3- and 5-year survival rates of HCC and MLC
following RFA treatment were calculated using the Kaplan-Meier
method. The log-rank test was used to compare the survival curve
differences between the HCC and the MLC groups. Furthermore, the
differences in their complete ablation rates, recurrence rates and
distant recurrence rates were evaluated with the χ2 test
and continuity correction.
Results
Evaluation of therapeutic effect
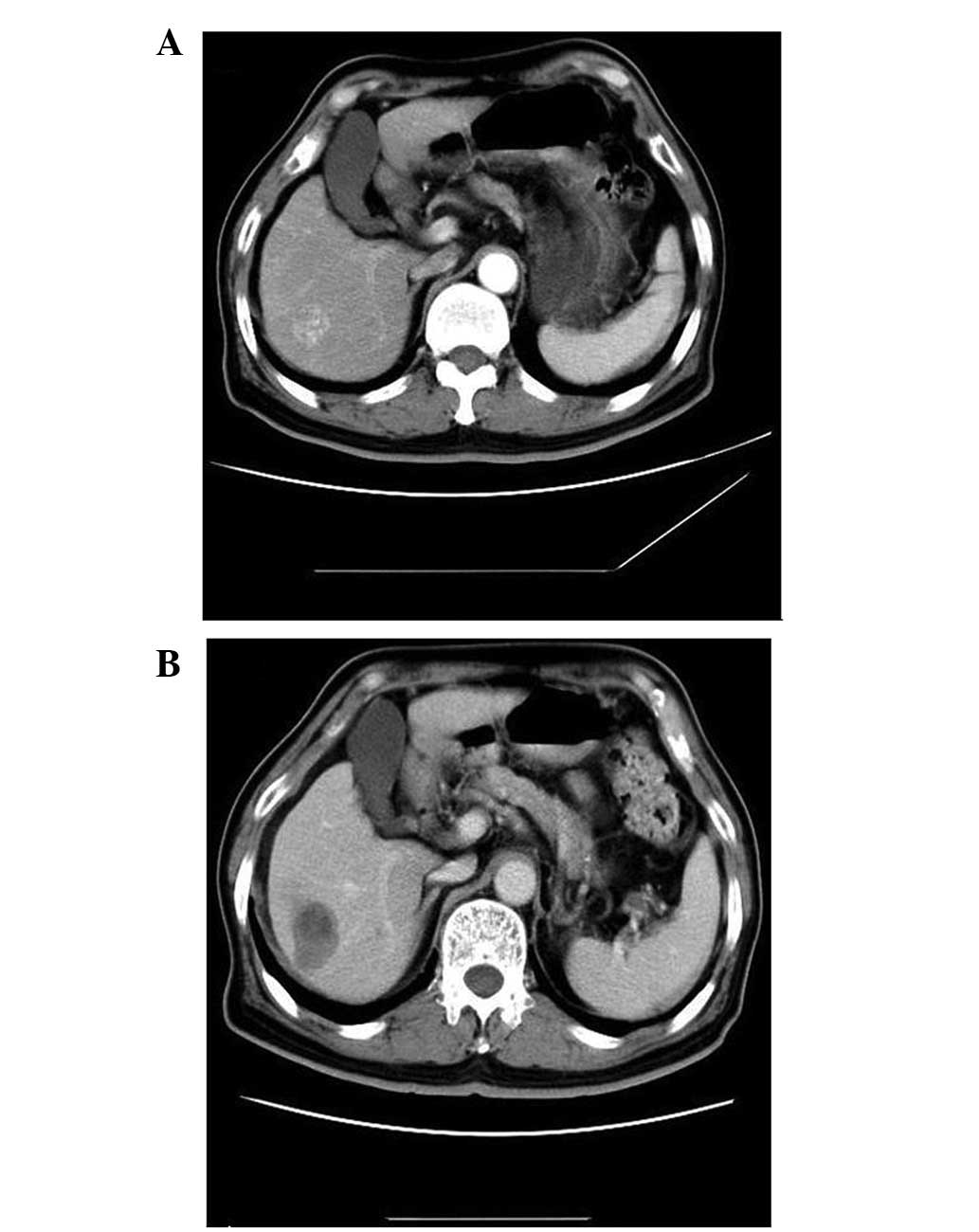
Two weeks following RFA treatment, enhanced CT scans
were conducted to observe the treated tumors. In the HCC group
(n=34), 32 patients exhibited complete ablation and in the MLC
group (n=22), 21 patients exhibited complete ablation. Enhanced CT
scans of these patients identified no significant enhancement in
the arterial region (Fig. 1). The
complete ablation rate was not identified to be statistically
significant between the two groups (P=1.000). The patients were
followed up for between 1 and 93 months. Five cases in the HCC
group (5/34, 14.7%) showed cancer recurrence and four cases (11.8%)
exhibited distant recurrence; in the MLC group, two cases (9.1%)
showed cancer recurrence and eight cases (36.4%) exhibited distant
recurrence (Table I). The
difference between the two groups was not identified to be
significant. The 1-, 3- and 5-year survival rates of HCC and MLC
groups as of May 2013 are shown in Table II.
 | Table ILocal therapeutic efficacy comparison
of the HCC group (n=34) and the MLC group (n=22) following RFA. |
Table I
Local therapeutic efficacy comparison
of the HCC group (n=34) and the MLC group (n=22) following RFA.
| Group | Complete ablation
rate (%) | Recurrence rate
(%) | Distant recurrence
rate (%) |
|---|
| HCC | 32/34 (94.1) | 5/34 (14.7) | 4/34 (11.8) |
| MLC | 21/22 (95.4) | 2/22 (9.1) | 8/22 (36.4) |
| P-value | 1.000 | 0.836 | 0.063 |
 | Table IISurvival rate of 56 patients following
RFA treatment. |
Table II
Survival rate of 56 patients following
RFA treatment.
| Survival rate
(%) |
|---|
|
|
|---|
| Group | 1 year | 2 year | 3 year |
|---|
| HCC | 86.2 | 71.4 | 60.0 |
| MLC | 73.9 | 45.4 | 37.5 |
| Total | 80.9 | 60.0 | 50.0 |
Survival rate comparison between the HCC
and MLC groups
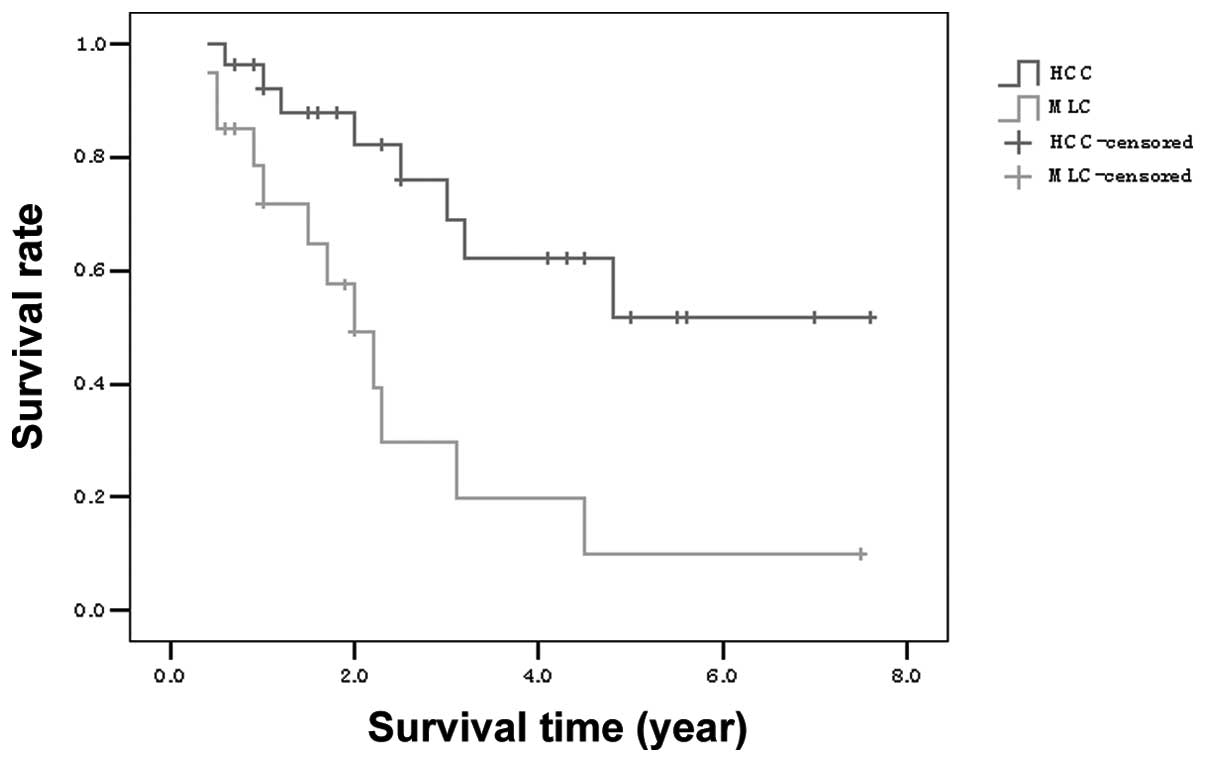
The 1-, 3- and 5-year survival rates were identified
to be significantly different between the two groups (P=0.002;
Fig. 2).
Adverse effects
Following RFA treatment of the 48 patients, one
patient experienced hepatic subcapsular hematoma; however,
injection of prothrombin complex promoted hemostasis and the
bleeding stopped. Three patients exhibited abnormal liver function
following treatment, which was demonstrated by increased levels of
alanine aminotransferase (ALT) and aspartate aminotransferase
(AST). Diammonium glycyrrhizinate (a hepatoprotective drug) was
administered, resulting in a gradual return of ALT and AST to
normal levels. One patient developed a secondary infection, the
symptoms of which were eased by performing a US-guided percutaneous
catheter drainage. The remaining patients were closely observed
following RFA treatment, and no skin burns, bleeding, nausea,
vomiting or other symptoms were observed.
Discussion
Numerous clinical studies have demonstrated that RFA
is an effective treatment for focal liver tumors. In the present
study, the complete ablation rate, following initial RFA treatment,
in the HCC and MLC groups was 94.1% (32/34) and 95.4% (21/22),
respectively. The initial complete ablation rate was predominantly
related to tumor size; for small HCCs (≤3 cm), RFA has been found
to be an effective and safe first-line treatment (9,10).
In addition, the tumor location influenced the efficacy of RFA; the
treatment effect is generally poor on tumors which neighboring the
portal vein, diaphragm, gall bladder and bowel (11–14).
Surgical resection is often the preferred treatment
for HCC and MLC as the patient’s 5-year survival rate is >50%
(7). However, surgical resections
should not be performed on patients suffering from multiple
diseases, anatomical constraints, lack of hepatic functional
reserve and extrahepatic metastasis, amongst other complications;
RFA is therefore used as an alternative treatment. The development
of imaging techniques has enabled the early diagnosis of liver
lesions. Previous clinical studies have identified that RFA and
surgical resection have similar efficacies in the treatment of
small HCC; however, RFA treatment requires a shorter hospital stay
with fewer complications when compared with surgical resection
(15,16). Peng et al (17) analyzed 145 patients with small
HCCs; 74 patients received a surgical resection, while 71 patients
underwent RFA treatment. The study revealed that patients who
underwent RFA treatment exhibited 1-, 3- and 5- year survival rates
of 98.5, 87.7 and 71.9%, respectively, compared with 90.5, 70.9 and
62.1% for the patients who underwent resection. This was considered
to be due to the trauma, various complications and significant
side-effects associated with the surgery.
In the current study, following RFA treatment the
patients with HCC exhibited 1-, 3- and 5- year survival rates of
86.2, 71.4 and 60.0%, demonstrating that RFA is comparable with
surgical resection in the effective treatment of small HCC (<5
cm) tumors. Patients with MLC exhibited 1-, 3- and 5- year survival
rates of 73.9, 45.4 and 37.5%; the survival rates of the two groups
were significantly different. Veltri et al (6) observed that the survival rates 1, 3
and 5 years after RFA treatment were 84, 43 and 23% in patients
with liver metastases resulting from colorectal cancer. In the
previous study, the mortality of one MLC patient was observed to be
due to liver failure, hepatorenal syndrome and hepatic
encephalopathy and there were three fatalities as a result of
multiple organ metastases. The majority of patients receiving MLC
treatment have advanced stage cancer; therefore, the application of
RFA treatment in these cases avoids the trauma of surgery,
alleviates suffering and prolongs patient survival to a certain
extent (18,19).
In conclusion, RFA is a minimally invasive technique
that is economical, highly accurate, safe, effective, reliable and
reproducible. The reduced postoperative complications improve
patient quality of life and prolong lifespan; therefore, this
method may be beneficial if applied in clinical treatment.
References
|
1
|
Ng KK, Poon RT, Lo CM, Yuen J, Tso WK and
Fan ST: Analysis of recurrence pattern and its influence on
survival outcome after radiofrequency ablation of hepatocellular
carcinoma. J Gastrointest Surg. 12:183–191. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kudo M: Radiofrequency ablation for
hepatocellular carcinoma: updated review in 2010. Oncology.
78(Suppl 1): 113–124. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tiong L and Maddern GJ: Systematic review
and meta-analysis of survival and disease recurrence after
radiofrequency ablation for hepatocellular carcinoma. Br J Surg.
98:1210–1224. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Livraghi T, Meloni F, Di Stasi M, et al:
Sustained complete response and complications rates after
radiofrequency ablation of very early hepatocellular carcinoma in
cirrhosis: Is resection still the treatment of choice? Hepatology.
47:82–89. 2008. View Article : Google Scholar
|
|
5
|
Naugler WE and Sonnenberg A: Survival and
cost-effectiveness analysis of competing strategies in the
management of small hepatocellular carcinoma. Liver Transpl.
16:1186–1194. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Veltri A, Guarnieri T, Gazzera C, et al:
Long-term outcome of radiofrequency thermal ablation (RFA) of liver
metastases from colorectal cancer (CRC): size as the leading
prognostic factor for survival. Radiol Med. 117:1139–1151. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tombesi P, Di Vece F and Sartori S:
Resection vs thermal ablation of small hepatocellular carcinoma:
What’s the first choice? World J Radiol. 5:1–4. 2013.PubMed/NCBI
|
|
8
|
Bruix J and Sherman M; American
Association for the Study of Liver Diseases. Management of
hepatocellular carcinoma: an update. Hepatology. 53:1020–1022.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Choi D, Lim HK, Rhim H, et al:
Percutaneous radiofrequency ablation for early-stage hepatocellular
carcinoma as a first-line treatment: long-term results and
prognostic factors in a large single-institution series. Eur
Radiol. 17:684–692. 2007. View Article : Google Scholar
|
|
10
|
Kim YS, Lim HK, Rhim H, et al: Ten-year
outcomes of percutaneous radiofrequency ablation as first-line
therapy of early hepatocellular carcinoma: analysis of prognostic
factors. J Hepatol. 58:89–97. 2013.PubMed/NCBI
|
|
11
|
Kariyama K, Nouso K, Wakuta A, et al:
Percutaneous radiofrequency ablation for treatment of
hepatocellular carcinoma in the caudate lobe. AJR Am J Roentgenol.
197:W571–575. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tang Z, Fang H, Kang M, et al:
Percutaneous radiofrequency ablation for liver tumors: Is it safer
and more effective in low-risk areas than in high-risk areas?
Hepatol Res. 41:635–640. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Huang HW: Influence of blood vessel on the
thermal lesion formation during radiofrequency ablation for liver
tumors. Med Phys. 40:0733032013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Morimoto M, Numata K, Kondo M, et al:
Radiofrequency ablation combined with transarterial
chemoembolization for subcapsular hepatocellular carcinoma: a
prospective cohort study. Eur J Radiol. 82:497–503. 2013.
View Article : Google Scholar
|
|
15
|
Sato M, Tateishi R, Yasunaga H, et al:
Mortality and morbidity of hepatectomy, radiofrequency ablation,
and embolization for hepatocellular carcinoma: a national survey of
54,145 patients. J Gastroenterol. 47:1125–1133. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Guo WX, Sun JX, Cheng YQ, et al:
Percutaneous radiofrequency ablation versus partial hepatectomy for
small centrally located hepatocellular carcinoma. World J Surg.
37:602–607. 2013. View Article : Google Scholar
|
|
17
|
Peng ZW, Lin XJ, Zhang YJ, et al:
Radiofrequency ablation versus hepatic resection for the treatment
of hepatocellular carcinomas 2 cm or smaller: a retrospective
comparative study. Radiology. 262:1022–1033. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Stang A, Fischbach R, Teichmann W,
Bokemeyer C and Braumann D: A systematic review on the clinical
benefit and role of radiofrequency ablation as treatment of
colorectal liver metastases. Eur J Cancer. 45:1748–1756. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wong SL, Mangu PB, Choti MA, et al:
American Society of Clinical Oncology 2009 clinical evidence review
on radiofrequency ablation of hepatic metastases from colorectal
cancer. J Clin Oncol. 28:493–508. 2010. View Article : Google Scholar : PubMed/NCBI
|