Introduction
Chronic kidney disease (CKD) has received increased
focus in healthcare in recent years. There is a marked positive
correlation between kidney dysfunction and cardiovascular disease
(CVD) (1,2). Diabetes is recognized as a major risk
factor for the development of CKD. CKD-associated diseases,
including diabetes, have been proposed as coronary disease
equivalents (3,4).
In certain kidney diseases, improving glomerular
filtration rate (GFR) should be performed whenever serum creatinine
(SCr) is measured. The most common method used to obtain an
estimated GFR (eGFR) value is based on SCr. Early detection of
kidney dysfunction in subjects with diabetes is of vital
importance, as appropriate interventions have been shown to slow
the progression to end-stage renal disease (ESRD) and reduce the
incidence of CVD (5). SCr
concentration is affected not only by GFR but also by a number of
factors that are independent of GFR, including age, ethnicity,
muscle mass, gender, use of medication and catabolic state
(6–8).
Serum cystatin C is a low molecular weight protein
that functions as a cysteine protease inhibitor and has been
proposed to be a reliable marker of GFR for certain diseases
associated with CVD (9). Serum
cystatin C is a more effective indicator of GFR than SCr (10–12).
At present, a number of serum cystatin C-based equations have been
identified and proposed as alternative filtration markers to
SCr-based equations (13–17).
Clinically, the SYNTAX score (SXscore) is capable of
accurately detecting the severity and complexity of coronary artery
lesions (18,19). The SXscore may also predict major
adverse cardiac events (MACEs) and periprocedural myocardial
infarction (MI) in patients undergoing elective percutanous
coronary intervention (PCI) (20–24).
In addition, a novel coronary artery bypass graft (CABG) SYNTAX
score was identified by Farooq et al (25), which was capable of calculating the
SYNTAX score in patients with prior bypass surgery.
Although numerous studies have investigated the
correlation between renal dysfunction and the severity of coronary
artery disease (CAD), these studies evaluated renal function using
GFRs based on SCr concentration (3,4,25,26).
Furthermore, CAD severity was based on the number of stenotic
coronary arteries. To the best of our knowledge, the correlation
between the cystatin C-based estimated GFR (eGFRcys) and
SXscore in patients with diabetes has not been previously reported.
Therefore, the aim of the present study was to evaluate the
association between eGFRcys and SXscore, and to explore
the applicable value of eGFRcys in patients with
diabetes.
Materials and methods
Subjects
A total of 612 patients with diabetes were recruited
to the study between July 2010 and March 2012 from the Department
of Endocrinology, The Third Xiangya Hospital of Central South
University (Changsha, China). All patients underwent coronary
angiography (CAG) and were angiographically diagnosed with CAD.
Patients with the following diseases were excluded from the study:
Congenital heart disease, valvular heart disease, congestive heart
failure and cardiomyopathy. In addition, patients that had
undergone surgical revascularization were excluded.
The study design was approved by the Ethics
Committee of the Third Xiangya Hospital, and informed consent was
provided by all subjects.
Renal function assessment
Prior to CAG, blood samples were collected from the
antecubital vein while the patients were resting in the supine
position. The serum concentration of cystatin C was measured using
the particle-enhanced immunonephelometric method.
eGFRcys was calculated using the Chronic Kidney Disease
Epidemiology Collaboration (CKD-EPI) cystatin C formula, as
follows: eGFRcys (ml/min/1.73 m2) = [127.7 ×
cystatin C−1.17 (mg/l) × age−0.13 × 0.91 (if
female) × 1.06 (if African-American)] (27,28).
The eGFRcys values were used to classify
the patients into four groups, as follows: Group 1
(eGFRcys ≥90 ml/min/1.73 m2); group 2 (60≤
eGFRcys <90ml/min/1.73m2); group 3 (30≤
eGFRcys <60 ml/min/1.73m2) and group 4
(eGFRcys <30 ml/min/1.73 m2).
Detection of cardiovascular risk
factors
Patients were fasted overnight prior to the blood
samples being obtained. The levels of total cholesterol (TC),
triglycerides (TG), low/high-density lipoprotein cholesterol
(LDL/LDH), creatinine, hemoglobin A1c (HbA1c), fasting plasma
glucose, C-reactive protein (CRP) and body mass index (BMI) were
measured in everyday practice.
Angiographic and SXscore analysis
From the baseline diagnostic angiogram, each
coronary lesion producing a ≥50% diameter stenosis in vessels ≥1.5
mm was scored separately and summed together to provide the overall
SXscore, which was calculated using the SXscore algorithm (18,19).
All angiographic variables pertinent to the SXscore calculation
were computed by two of three experienced cardiologists who were
blinded to the study of the angiograms. In the case of a
disagreement, the opinion of the third observer was obtained and
the final decision was made by consensus. Occluded infarct-related
arteries in patients with acute MI were scored as occlusions of
<3 months duration. Patients with in-stent restenosis lesions
were scored in the same manner to those with de novo
lesions. Patients with an SXscore >0 were angiographically
defined as exhibiting CAD.
Statistical analysis
In the present study, all of the data were processed
using SPSS software 20.0 (SPSS, Inc., Chicago, IL, USA). A
two-sided P-value of <0.05 was considered to indicate a
statistically significant difference. Intergroup differences of
categorical variables were compared using χ2 tests.
Pearson and partial correlation coefficients were calculated
between the eGFR and SXscore with adjustment for age, gender and
other traditional risk factors. The ordinal logistic regression was
employed to control for multiple covariates when analyzing the
association between eGFRcys and SXscore.
Results
The average age of the 612 patients included in this
study was 64.8±9.7 years. The mean eGFRcys was 69.7±13.4
ml/min/1.73m2 (range, 8.4–154.3 ml/min/1.73
m2). Only 12 (5.7%) patients had an eGFRcys
<30 ml/min/1.73m2. The SXscore ranged between 1.0 and
53 with a mean of 17.4±7.5. Patients with renal dysfunction were
older, more often female and more likely to have a history of
hypertension when compared with those patients with normal renal
function (Table I).
 | Table IBaseline data. |
Table I
Baseline data.
| Characteristic | Group 1 (n=66) | Group 2 (n=242) | Group 3 (n=279) | Group 4 (n=25) | P-value |
|---|
| Age (years) | 55.78±8.12 | 64.14±6.78 | 68.37±5.69 | 72.02±7.15 | <0.001 |
| Male (n) | 57 (86.3) | 191 (78.9) | 125 (44.8) | 7 (28.0) | <0.001 |
| Hypertension (n) | 37 (56.1) | 181 (74.8) | 224 (80.1) | 23 (92.0) | <0.001 |
| Hyperlipidemia
(n) | 35 (53.0) | 119 (49.2) | 127 (45.5) | 11 (44.0) | 0.544 |
| Fasting glucose
(mg/dl) | 135.8±2.8 | 137.2±18.6 | 134.9±17.4 | 137.7±25.1 | 0.405 |
| HbA1c (%) | 7.7±2.5 | 7.4±2.7 | 7.5±1.2 | 7.6±1.8 | 0.624 |
| TC (mg/dl) | 228.5±21.4 | 231.4±23.2 | 235.6±17.3 | 237.6±22.5 | 0.082 |
| LDL (mg/dl) | 125.3±15.6 | 131.1±21.3 | 124.7±19.1 | 126.3±18.5 | 0.058 |
| HDL (mg/dl) | 54.5±11.4 | 55.1±16.3 | 53.4±15.6 | 57.1±11.5 | 0.083 |
| TG (mg/dl) | 112.9±21.7 | 113.7±20.3 | 116.8±11.9 | 118.6±22.3 | 0.205 |
| BMI
(kg/m2) | 23.3±4.8 | 24.6±4.8 | 23.1±4.5 | 21.9±5.7 | <0.001 |
| CRP (mg/dl) | 2.0±0.6 | 2.2±0.5 | 2.5±0.4 | 2.7±0.6 | <0.001 |
| Cr (mg/dl) | 0.7±0.1 | 1.0±0.3 | 1.4±0.1 | 1.8±0.4 | <0.001 |
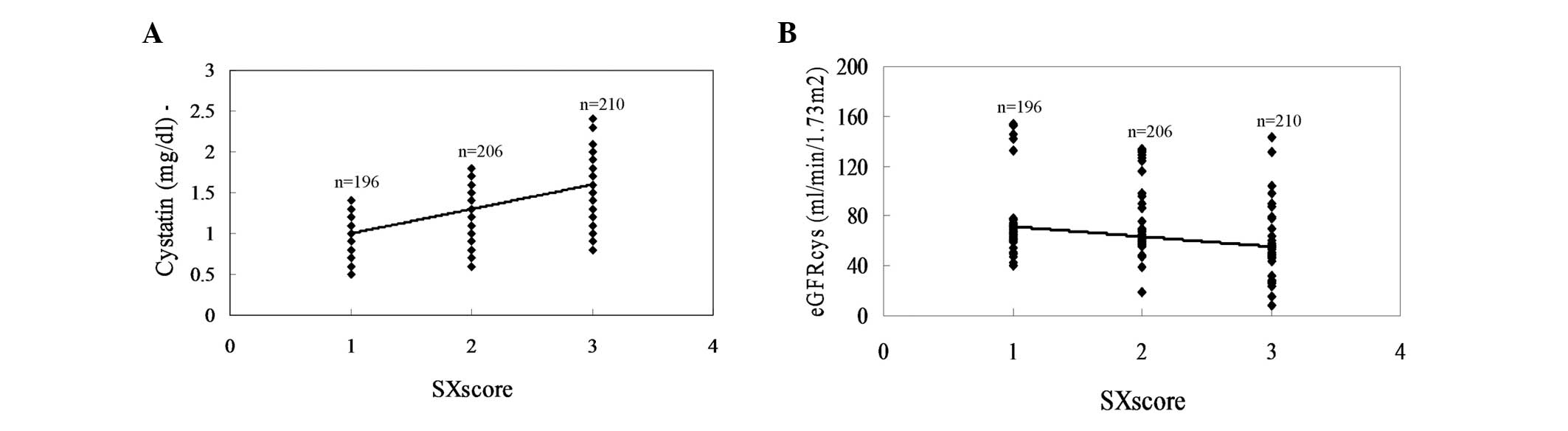
By detecting a number of risk factors, it was found
that age, gender, systolic blood pressure (SBP), diastolic blood
pressure (DBP), fasting glucose, HbA1c, TC, LDL, HDL, TG, BMI, CRP
and incidences of hypertension and hyperlipidemia were not
different between one group and another (data not shown). However,
from the data in Table II, it was
observed that eGFRcys values were significantly lower
and the levels of cystatin C were significantly higher in the
highest SXscore group than those in other groups (P<0.001).
Therefore, in combination with the results of Table I, the correlation between cystatin
C level, eGFRcys and the SXscore (including SXlow,
SXmid, and SXhigh) was analyzed.
 | Table IIComparison of parameters according to
the SXscore. |
Table II
Comparison of parameters according to
the SXscore.
| Characteristic | SXlow (n=196) | SXmid (n=206) | SXhigh (n=210) | P-value |
|---|
| Cystatin C
(mg/dl) | 1.0±0.2 | 1.3±0.1 | 1.6±0.2 | <0.001 |
| eGFRcys
(ml/min/1.73m2) | 69.9±20.8 | 62.0±19.4 | 54.3±22.5 | <0.001 |
| eGFRcys
(n) | | | | <0.001 |
| ≥90 | 30 (15.3) | 25 (12.1) | 14 (6.6) | |
| ≥60 and
<90 | 91 (46.4) | 90 (43.7) | 65 (31.0) | |
| ≥30 and
<60 | 73 (37.2) | 85 (41.3) | 119 (56.7) | |
| <30 | 2 (2.1) | 6 (2.9) | 12 (5.7) | |
The results of the correlation analysis indicated
that there was a significant positive correlation between the
levels of cystatin C and the SXscore (r=0.8891, P<0.001;
Fig. 1A). In addition, the
eGFRcys was negatively correlated with the SXscore
(r=−0.7918, P<0.001; Fig.
1B).
Discussion
In the present study, it was demonstrated for the
first time, to the best of our knowledge, that eGFRcys
was markedly associated with the SXscore in patients with diabetes.
The results showed that renal function was correlated with the
severity of CAD in patients with diabetes. This conclusion may be
helpful to explain the increased risk of CVD-associated events and
mortality in patients with renal dysfunction (26). Usually, diabetes is recognized as a
major risk factor for the development of CKD. The cumulative
incidence of MI may approach 20% over 10 years (4) when patients present with CKD and
diabetes. Such effects of CKD and diabetes on mortality and MI have
been extensively studied (29).
Clinically, the measurement of SCr concentration has
been employed as an indirect method of estimating the renal
function. The creatinine concentration has become the most commonly
applied approximation of the GFR. However, this method has
presented increasing limitations during clinical practice.
Therefore, an improved method for the assessment of GFR is
required. Serum cystatin C is freely filtered across the glomerular
membrane, and is reabsorbed and completely metabolized in the
proximal tubule. It has been demonstrated that serum cystatin C
possesses a number of characteristics that make it an ideal
endogenous GFR marker (6).
Previous studies have shown that serum cystatin C is superior to
serum creatinine as a GFR marker in patients with a mild or
moderate reduction in GFR (11–13).
Meta-analyses have also demonstrated that serum cystatin C is
superior to creatinine in measuring renal function (10,30).
A previous study indicated that all serum cystatin C-based
equations, excluding the Larsson formula, were reliable markers of
GFR in patients with CKD (31).
Clinically, the SXscore is a comprehensive
angiographic scoring system that is capable of accurately detecting
the severity and complexity of coronary artery lesions (18,19).
The score was initially devised as a method to ensure that the
cardiologist and the cardiac surgeon accurately reviewed the
angiogram of patients with complex CAD, and it was important in
stratifying patients with complex CAD to aid revascularization
decisions (21). Further
evaluation of the score has also indicated its ability to predict
clinical outcomes in patients with three-vessel disease or
unprotected left main disease, even the patients with CAD (22,23,32).
The association between CKD and CAD has been investigated for a
number of years. Kilickesmez et al (33) demonstrated that CKD has an
independent influence on lesion morphology and complexity. Abaci
et al (34) concluded that
the eGFR was an independent predictor of the extension and severity
of CAD among patients with diabetes. Kiyosue et al (35) revealed that the number of stenotic
coronary arteries was higher in the CKD group compared with
individuals without CKD. The results of the present study indicated
that the correlation between eGFRcys and the SXscore was
significant, and that it may be an improved method of representing
the correlation between kidney function and CAD severity.
In conclusion, this study demonstrated that
eGFRcys is an independent predictor of the SXscore in
patients with diabetes. This may be beneficial in explaining the
increased risk of CVD-associated events and mortality in patients
with renal dysfunction. The eGFRcys-estimating method
may be considered important in the assessment of the SXscore in
patients with diabetes.
References
|
1
|
Mooney JF, Ranasinghe I, Chow CK, Perkovic
B, Barzi F, Zoungas S, et al: Preoperative estimates of glomerular
filtration rate as predictors of outcomes after surgery: a
systematic review and meta-analysis. Anesthesiology. 118:809–824.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kottgen A, Russell SD, Loehr LR,
Crainiceanu CM, Rosamond WD, Chang PP, et al: Reduced kidney
function as a risk factor for incident heart failure: the
atherosclerosis risk in communities (ARIC) study. J Am Soc Nephrol.
18:1307–1315. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yoshida T, Kato K, Yokoi K, Oguri M,
Watanabe S, Metoki N, et al: Association of genetic variants with
chronic kidney disease in Japanese individuals with or without
hypertension or diabetes mellitus. Exp Ther Med. 1:137–145.
2010.PubMed/NCBI
|
|
4
|
Debella YT, Giduma HD, Light RP and
Agarwal R: Chronic kidney disease as a coronary disease equivalent
- a comparison with diabetes over a decade. Clin J Am Soc Nephrol.
6:1385–1392. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Macisaac RJ, Premaratne E and Jerums G:
Estimating glomerular filtration rate in diabetes using serum
cystatin C. Clin Biochem Rev. 32:61–67. 2011.PubMed/NCBI
|
|
6
|
National Kidney Foundation. K/DOQI
clinical practice guidelines of chronic kidney disease: evaluation,
classification and stratification. Am J Kidney Dis. 39(2 Suppl 1):
S1–S266. 2002.PubMed/NCBI
|
|
7
|
Levey AS: Measurement of renal function in
chronic renal disease. Kidney Int. 38:167–184. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Economidou F, Margaritopoulos G, Antoniou
KM and Siafakas NM: The angiogenetic pathway in malignant pleural
effusions; Pathogenetic and therapeutic implications. Exp Ther Med.
1:3–7. 2010.PubMed/NCBI
|
|
9
|
Coll E, Botey A, Alvarez L, Poch E, Quintó
L, Saurina A, et al: Serum cystatin C as a new marker for
noninvasive estimation of glomerular filtration rate and as a
marker for early renal impairment. Am J Kidney Dis. 36:29–34. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dharnidharka VR, Kwon C and Stevens G:
Serum cystatin C is superior to serum creatinine as a marker of
kidney function: a meta-analysis. Am J Kidney Dis. 40:221–226.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hojs R, Bevc S, Antolinc B, Gorenjak M and
Puklavec L: Serum cystatin C as an endogenous marker of renal
function in the elderly. Int J Clin Pharmacol Res. 24:49–54.
2004.PubMed/NCBI
|
|
12
|
Hojs R, Bevc S, Ekart R, Gorenjak M and
Puklavec L: Serum cystatin C as an endogenous marker of renal
function in patients with mild to moderate impaired kidney
function. Nephrol Dial Transplant. 21:1855–1862. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bevc S, Hojs R, Ekart R, Gorenjak M and
Puklavec L: Simple cystatin C formula compared to sophisticated
CKD-EPI formulas for estimation of glomerular filtration rate in
the elderly. Ther Apher Dial. 15:261–268. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Leiva E, Mujica V, Palomo I, Orrego R,
Guzman L, Nunez S, et al: High-sensitivity C-reactive protein and
liver enzymes in individuals with Metabolic Syndrome in Talca,
Chile. Exp Ther Med. 1:175–179. 2010.PubMed/NCBI
|
|
15
|
Rule AD, Bregstralh EJ, Slezak JM, Bergert
J and Larson TS: Glomerular filtration rate estimated by cystatin C
among different clinical presentations. Kidney Int. 69:399–405.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hojs R, Bevc S, Ekart R, Gorenjak M and
Puklavec L: Serum cystatin C-based equation compared to
serum-creatinine based equations for estimation of glomerular
filtration rate in patients with chronic kidney disease. Clin
Nephrol. 70:10–17. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tidman M, Sjöström P and Jones I: A
Comparison of GFR estimating formulae based upon s-cystatin C and
s-creatinine and a combination of the two. Nephrol Dial Transplant.
23:154–160. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sianos G, Morel MA, Kappetein AP, Morice
MC, Colombo A, Dawkins K, et al: The SYNTAX Score: an angiographic
tool grading the complexity of coronary artery disease.
EuroIntervention. 1:219–227. 2005.PubMed/NCBI
|
|
19
|
Serruys PW, Onuma Y, Garg S, Sarno G, van
den Brand M, Kappetein AP, et al: Assessment of the SYNTAX score in
the Syntax study. EuroIntervention. 5:50–56. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Valgimigli M, Serruys PW, Tsuchida K,
Vaina S, Morel MA, van den Brand MJ, et al: ARTS II: Cyphering the
complexity of coronary artery disease using the syntax score to
predict clinical outcome in patients with three-vessel lumen
obstruction undergoing percutaneous coronary intervention. Am J
Cardiol. 99:1072–1081. 2008. View Article : Google Scholar
|
|
21
|
Serruys PW, Morice MC, Kappetein AP,
Colombo A, Holmes DR, Mack MJ, et al: Percutaneous coronary
intervention versus coronary-artery bypass grafting for severe
coronary artery disease. N Engl J Med. 360:961–972. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yue X, Yu HS, Lin XL, Liu XL, Liu K, Wang
X, et al: Investigation into the optimal surgical conditions for
coronary artery ligation for establishing a myocardial infarction
model in mice. Exp Ther Med. 6:341–346. 2013.PubMed/NCBI
|
|
23
|
Hashimoto T, Yanaihara N, Okamoto A,
Nikaido T, Satito M, Takakura S, et al: Cyclin D1 predicts the
prognosis of advanced serous ovarian cancer. Exp Ther Med.
2:213–219. 2011.PubMed/NCBI
|
|
24
|
van Gaal WJ, Ponnuthurai FA, Selvanayagam
J, Testa L, Porto I, Neubauer S, et al: The Syntax score predicts
peri-procedural myocardial necrosis during percutaneous coronary
intervention. Int J Cardiol. 135:60–65. 2009.PubMed/NCBI
|
|
25
|
Farooq V, Girasis C, Magro M, Onuma Y,
Morel MA, Heo JH, et al: The CABG SYNTAX Score - an angiographic
tool to grade the complexity of coronary disease following coronary
artery bypass graft surgery: from the SYNTAX Left Main Angiographic
(SYNTAX-LE MANS) substudy. Eurolntervention. 8:1277–1285. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Schrier RW: Role of diminished renal
function in cardiovascular mortality: marker or pathogenetic
factor? J Am Coll Cardiol. 47:1–8. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Stevens LA, Coresh J, Schmid CH, Feldman
HI, Froissart M, Kusek J, et al: Estimating GFR using serum
cystatin C alone and in combination with serum creatinine: a pooled
analysis of 3,418 individuals with CKD. Am J Kidney Dis.
51:395–406. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Inker LA, Eckfeldt J, Levey AS,
Leiendecker-Foster C, Rynders G, Manzi J, et al: Expressing the
CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration)
cystatin C equations for estimating GFR with standardized serum
cystatin C values. Am J Kidney Dis. 58:682–684. 2011. View Article : Google Scholar
|
|
29
|
Sarnak MJ, Levey AS, Schoolwerth AC,
Coresh J, Culleton B, Hamm LL, et al; American Heart Association
Councils on Kidney in Cardiovascular Disease, High Blood Pressure
Research, Clinical Cardiology, and Epidemiology and Prevention.
Kidney disease as a risk factor for development of cardiovascular
disease: a statement from the American Heart Association Councils
on Kidney in Cardiovascular Disease, High Blood Pressure Research,
Clinical Cardiology, and Epidemiology and Prevention. Circulation.
108:2154–2169. 2003. View Article : Google Scholar
|
|
30
|
Roos JF, Doust J, Tett SE and Kirkpatrick
CM: Diagnostic accuracy of cystatin C compared to serum creatinine
for the estimation of renal dysfunction in adults and children – a
meta-analysis. Clin Biochem. 40:383–391. 2007.
|
|
31
|
Hojs R, Bevc S, Ekart R, Gorenjak M and
Puklavec L: Serum cystatin C-based formulas for prediction of
glomerular filtration rate in patients with chronic kidney disease.
Nephron Clin Pract. 114:c118–c126. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wang BJ, Sun SL, Liu GR, Li YC, Pang JX,
Zhang JF, et al: Correlation between aortic/carotid atherosclerotic
plaques and cerebral infarction. Exp Ther Med. 6:407–410.
2013.PubMed/NCBI
|
|
33
|
Kilickesmez KO, Abaci O, Okcun B, Kocas C,
Baskurt M, Arat A, et al: Chronic kidney disease as a predictor of
coronary lesion morphology. Angiology. 61:344–349. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Abaci A, Sen N, Yazici H, Tulmac M,
Türkoglu S, Tavil Y, et al: Renal dysfunction is the most important
predictor of the extent and severity of coronary artery disease in
patients with diabetes mellitus. Coron Artery Dis. 18:463–469.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kiyosue A, Hirata Y, Ando J, Fujita H,
Morita T, Takahashi M, et al: Relationship between renal
dysfunction and severity of coronary artery disease in Japanese
patients. Circ J. 74:786–791. 2010. View Article : Google Scholar : PubMed/NCBI
|