Introduction
Coronary heart disease (CHD) is a common
cardiovascular disease. The recent increasing incidence of the
disease, as well as being a serious risk to human health, has led
to CHD becoming a leading cause of mortality worldwide. CHD is
myocardial damage caused by changes in coronary circulation,
resulting in an imbalance between myocardial demand and coronary
blood flow. CHD is caused by functional changes and organic
diseases. Clinical exercise with ECG testing, ultrasound
echocardiography and radionuclide myocardial scans are used to
diagnose CHD. Coronary angiography (CAG) is considered the ‘gold
standard’ for diagnosing CHD. However, it was previously found that
the fine coronary angiographic observations of certain patients did
not explain their recurrent angina, which may have resulted from
tiny vascular lesions caused by defects in myocardial perfusion.
Coronary macrovascular and microvascular disease lead to angina due
to poor myocardial perfusion. Thus, myocardial perfusion has
attracted significant attention (1). In 1929, Werner Forssmann
self-administered the first cardiac catheterization procedure; the
procedure has since developed rapidly and become one of the most
important medical advances in the 20th century. Judkins improved
several aspects of the catheterization, allowing its wide use in
clinical CAG. The process involves puncture of a major blood vessel
(e.g., the femoral or radial artery) using a percutaneous needle
and then insertion of a small catheter into the heart. CAG
accurately and intuitively shows all coronary arteries. However,
inadequacies in the process remain. Firstly, the procedure is
traumatic, invasive and entails a certain degree of risk, which
prevents patients with no marked symptoms from readily undergoing
such an examination. Secondly, understanding the structure of the
vascular wall and the features of atheroma is challenging. Thirdly,
the procedure may not provide pathological and physiological
information, including myocardial perfusion, metabolism and tissue
activity. Furthermore, it does not provide information about
microangiopathy myocardial perfusion blood flow, as well as a
simple operation. Therefore, a safe, effective and noninvasive
screening method for diagnosing CHD and assessing myocardial
perfusion requires development (2).
Advanced Flash dual-source CT (DS-CT) uses two sets
of ball-tube detector systems. A post-processing workstation and
the corresponding software are used to obtain images of myocardial
perfusion and determine myocardial ischemia, while simultaneously
obtaining a surface reconstruction diagram to evaluate the coronary
arteries. Studies have shown that coronary imaging using Flash
DS-CT has a success rate of 100%. Myocardial perfusion imaging also
meets the demands of clinical diagnosis. Ruzsics et al
(3,4) evaluated the coronary arteries and
myocardial perfusion of 35 patients using dual-energy CT.
Myocardial perfusion imaging using CAG and single photon emission
computed tomography (SPECT) under dual-energy mode revealed a
sensitivity of 84%, specificity of 84% and accuracy of 92% for
diagnosing stenosis of >50%. The corresponding values for DS-CT
and SPECT were 92, 92 and 93%, which indicated the potential of
Flash DS-CT scans for comprehensively evaluating coronary vascular
stenosis and myocardial perfusion. With the clinical application of
a new generation of dual-energy CT, Flash DS-CT may complete
coronary imaging and myocardial perfusion imaging at the same time,
resulting in a limited amount of radiation exposure (4,5). As
a noninvasive examination, Flash DS-CT has been widely used for
screening and diagnosing suspected coronary artery diseases
(6–8). DS-CT reveals the anatomy of coronary
arteries, as well as exhibiting the regional myocardial perfusion
of coronary lesions (9,10). The present study aimed to determine
the accuracy of DS-CT coronary imaging and myocardial perfusion for
diagnosing CHD.
Materials and methods
Inclusion criteria
This study was conducted in accordance with the
Declaration of Helsinki and with approval from the Ethics Committee
of the Central Hospital of Baotou (Baotou, China). Written informed
consent was obtained from all participants. There were 60 subjects,
consisting of 38 males and 22 females aged 36–75 years (54.25±7.02
years). All subjects had clinical considerations or known CHD and
were patients of the Central Hospital of Baotou between 2010 and
2011. All patients underwent DS-CT examinations and had a body mass
index of 23.2±4.5 kg/m2 and a heart rate between 55 and
78 bpm (64±8 bpm).
Exclusion criteria
Patients with hypersensitivity to iodinated contrast
material, serious arrhythmia, respiratory distress, serious liver
and kidney dysfunctions and decompensated ventricular dysfunction
were excluded from the study.
Flash DS-CT
The time resolution of the Flash Spiral scanning
technology (Flash DS-CT; Somatom Definition Flash, Siemens
Healthcare, Erlangen, Germany) was 75 msec and the entire heart
scan lasted 0.25 sec. The technology clearly depicts diameters ≥1.5
mm of two to three branches of the coronary artery, without
controlling the patient’s heart rate, to accurately determine the
degree of stenosis. Reconstruction of the images was divided into
two parts, one for dual-source CT coronary angiography (DS-CTA)
analysis and another for dual-source CT myocardial perfusion
imaging (DS-CTP) analysis. The DS-CTA images were analyzed and
vessel branches were regarded as single units, with two heart
imaging physicians estimating the coronary arteries. The DS-CTP
images were analyzed using the 17 segment method recommended by the
American Heart Association (AHA) (11). Two specialized cardiac imaging
physicians completed the DS-CTP evaluation. Myocardial perfusion
was evaluated in terms of normal perfusion and perfusion defects.
The combination of DS-CTA and DS-CTP was compared with CAG for
diagnosing CHD, using the method by Kachenoura et al
(12), to elucidate the
correlation of coronary stenosis with the myocardial ischemic
region. Coronary artery stenosis was diagnosed as ≥2 defects in
myocardial segment perfusion in the DS-CTP image.
CAG
CAG was conducted by experienced interventional
physicians following the Judkins method (13), whereas the images were analyzed by
two experienced cardiologists. Based on the AHA classification
system, the right coronary artery (RCA) was divided into segments
1–4 (proximal, middle, distal and posterior descending artery,
respectively). The left main branch (LM) was segment 5, whereas the
left anterior descending artery (LAD) was divided into segments
6–10 (the proximal, middle, distal and the first and second
diagonal branch, respectively). The left circumflex artery (LCX)
was divided into segments 11 to 15 (circumflex artery nearly
segments, middle, distal and first and second obtuse marginal
branch, respectively). Stenosis was defined as ≥50% occlusion.
Grouping and comparison
CAG was used to classify the patients into groups
according to the degree of stenosis: <50% and ≥50%. It was also
used as the reference standard for detecting stenosis of ≥50% and
determined whether its positive coincidence rate corresponded with
that of DS-CT coronary imaging. The sensitivity, specificity and
accuracy of DS-CT for diagnosing CHD was calculated, as well as the
diagnostic sensitivity, specificity, positive and negative
predictive value of DS-CTA combined with DS-CTP for diagnosing
CHD.
Statistical analysis
Data were analyzed using SPSS version 17.0 (SPSS,
Inc., Chicago, IL, USA). The measurement data are expressed as mean
± SD and the count data were analyzed using a χ2 test.
P≤0.05 was considered to indicate a statistically significant
difference. CAG was regarded as the reference standard. The
sensitivity, specificity, positive predictive value and negative
predictive value of Flash DS-CT for diagnosing vascular stenosis
were calculated using the following formulae: Sensitivity = true
positive results/(true positive results + false negative results);
specificity = true negative results/(true negative results + false
positive results); positive predictive value = true positive
results/(true positive results + false positive results); and
negative predictive value = true negative results/(true negative
results + false negative results).
Results
General information
Of the 60 patients who underwent DS-CTA and DS-CTP,
1 case was excluded due to patient obesity which affected the image
quality. The remaining 59 patients fulfilled the diagnostic
requirements. The coronary angiograms of the 60 patients indicated
that 86 of the 240 coronary arteries had ≥50% stenosis. Among the
patients, 6 had one vascular lesion, 22 had two vascular lesions
and 12 had three vascular lesions. The DS-CTA showed that 81
coronary arteries had stenosis of ≥50%, whereas DS-CTA combined
with DS-CTP indicated 92 coronary arteries had stenosis of
≥50%.
CAG and CT coronary imaging
The coronary angiograms of the 60 patients indicated
that 86 of 240 vessels had stenosis of ≥50%. This degree of
stenosis was observed in 12 vessels in the RCA, 34 in the LCX, 38
in the LAD and 2 in the LM. The results of DS-CTA indicated that 81
arteries had coronary stenosis of ≥50%, of which 14 vessels were in
the RCA, 32 in the LCX, 34 in the LAD and 1 in the LM (Table I).
 | Table IComparison of CAG and CT coronary
imaging. |
Table I
Comparison of CAG and CT coronary
imaging.
| ≥50% stenosis
(n) |
|---|
|
|
|---|
| Lesion sites | CAG | CT |
|---|
| RCA | 12 | 14 |
| LCX | 34 | 32 |
| LAD | 38 | 34 |
| LM | 2 | 1 |
| Total | 86 | 81 |
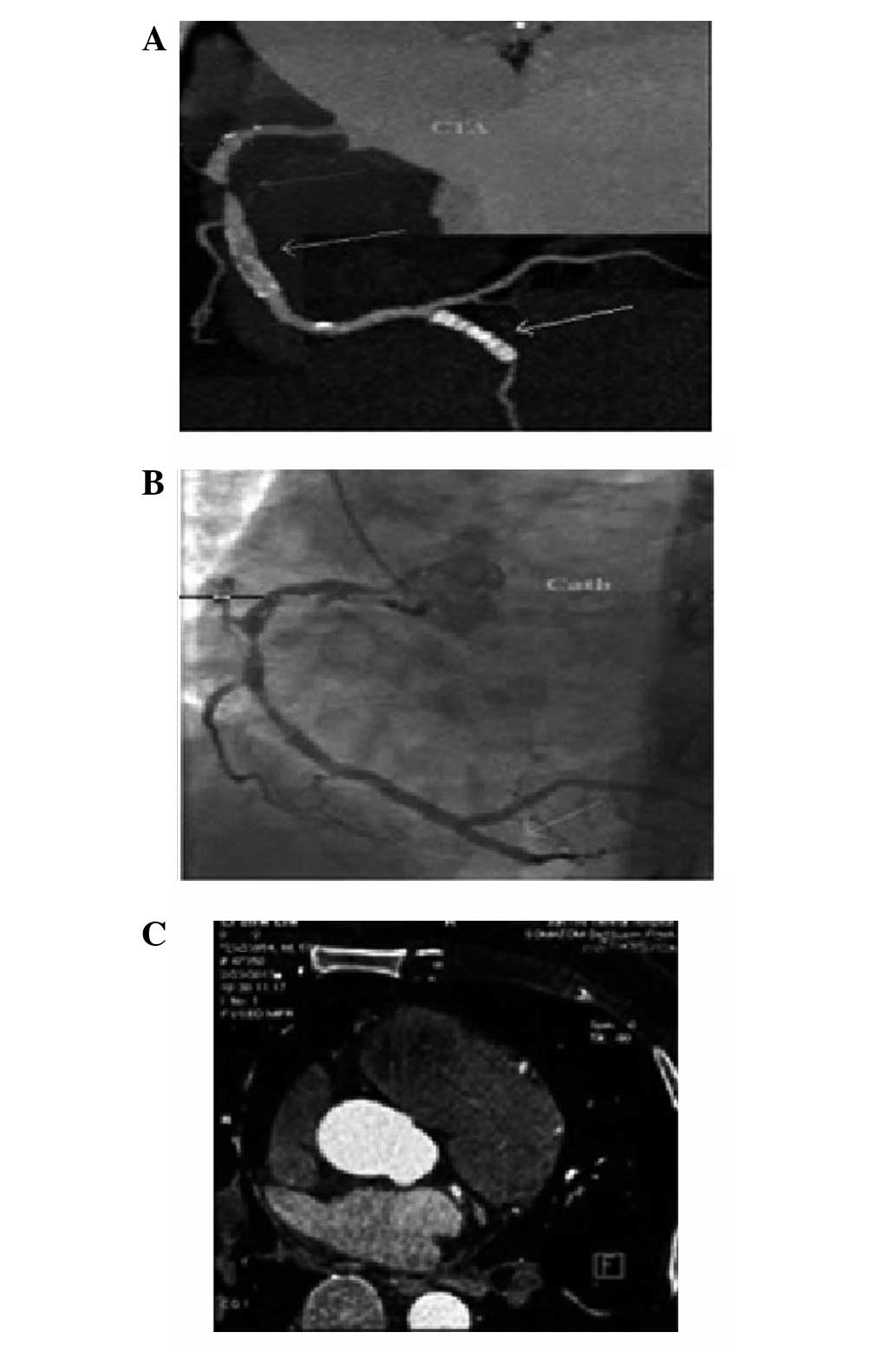
DS-CT and catheter angiography
Using CAG as the reference standard, the results
indicated that 86 coronary arteries had stenosis of ≥50%, whereas
the results from DS-CTA indicated that 81 branches had stenosis of
≥50%. The diagnostic sensitivity, specificity and positive and
negative predictive values of DS-CTA for stenosis of ≥ 50% were
83.7, 92.7, 88.9 and 89.1%, respectively. DS-CTA combined with
DS-CTP diagnosed ≥50% stenosis in 92 coronary arteries and had
diagnostic sensitivity, specificity and positive and negative
predictive values of 94.2, 91.1, 88.0 and 95.8%, respectively
(Table II; Fig. 1).
 | Table IICoronary stenosis observed with DS-CT
and catheter angiography. |
Table II
Coronary stenosis observed with DS-CT
and catheter angiography.
| | Catheter
angiography |
|---|
| |
|
|---|
| CT technique | CT result | Positive | Negative |
|---|
| DS-CTA | Positive | 72 | 9 |
| Negative | 14 | 115 |
| DS-CTA + DS-CTP | Positive | 81 | 11 |
| Negative | 5 | 113 |
Discussion
CAG is often considered the ‘gold standard’ for
diagnosing coronary artery stenosis, however, its invasiveness
limits its routine application. With the development of CT coronary
imaging technology, particularly Flash DS-CT, CTA and CTP may be
performed without increasing the radiation dose, as well as
improving the accuracy of the diagnosis of coronary artery
stenosis. The most accurate method for diagnosing CHD is to obtain
coronary anatomical information and evaluate the changes in
coronary artery hemodynamics (14). The results obtained in the present
study for the diagnostic sensitivity, specificity and positive and
negative predictive values of DS-CT for vascular stenosis of ≥50%
were 83.7, 92.7, 88.9 and 89.1%, respectively. However, for DS-CTA
combined with DS-CTP for CHD, the subsequent values were 94.2,
91.1, 88.0 and 95.8%, respectively. Therefore, it was shown that
DS-CT had a high negative predictive value and specificity for
diagnosing coronary artery stenosis, which is consistent with the
findings of a previous international study (15). The high specificity indicates that
DS-CT has a similar diagnostic reliability to CAG. It was also
found that combining DS-CTA with DS-CTP further improved the
diagnostic sensitivity and accuracy. However, the combination had a
lower specificity than DS-CTA alone. Using DS-CTP, the coronary
perfusion defect did not indicate luminal stenosis for supplying
blood.
Three cases with normal coronary angiograms showed
perfusion defects under DS-CTP. The recurrent angina of certain
patients with normal coronary angiograms indicated that
microvascular disease was caused by poor myocardial perfusion;
thus, these patients were diagnosed with cardiac X syndrome
(13,16). The etiology and symptoms also
applied to numerous patients with normal CAG. The coronary
angiograms of specific patients showed vascular stenosis, mild
coronary lesions and critical lesions (stenosis of 50–70%).
However, the myocardial perfusion imaging results of these patients
were normal, which indicated that the stenoses did not diminish
myocardial perfusion (16).
Subsequent treadmill tests revealed positive results. One study
showed that only a certain amount of exercise induced changes in
coronary artery blood flow, which in turn caused abnormalities in
myocardial perfusion; the myocardial perfusion defects were visible
in the images (13). Blankstein
et al (17) hypothesized
that poor myocardial perfusion was due to significant stenosis of
the coronary blood supply. Otherwise, the defect was a false
positive (18). These studies
(19) showed the mutual
correlation and the inherent differences between morphological and
functional examinations, which implied a correlation between
stenosis and ischemia. The seriousness of local narrowing was
insufficient to predict its effect on the dynamics of myocardial
blood flow. Specific cases revealed inconsistencies between
coronary anatomical narrowing and myocardial perfusion. Myocardial
perfusion was directly associated with the symptoms, signs and
prognosis of the patients. DS-CT was capable of diagnosing coronary
artery stenosis, as well as revealing all types of myocardial
perfusion defects. By combining morphological and functional
information on the coronary circulation, the accuracy of CHD
diagnosis may be increased, providing a reliable basis for the
corresponding treatment. In conclusion, Flash DS-CTA combined with
DS-CTP may reflect the two aspects of coronary atherosclerosis and
myocardial ischemia, therefore allowing a more accurate
identification of vessel lesions. The combination improved the
accuracy of diagnosing CHD and stratifying the prognostic risks,
which is likely to provide a reliable basis for further assessment
of the clinical situation and prognosis to select the best
treatment (20).
However, the present study had certain limitations.
Firstly, the study involved a single institution only; accurately
determining the diagnostic value of this imaging technology
requires multicenter studies. Also, the sample size of the present
study was relatively small and should be increased in future
studies. Secondly, the DS-CTP scans were obtained with the patients
in a resting state; further studies are required to be conducted in
the drug-loading state.
Flash DS-CT is a single stage examination,
overcoming the previous inability to simultaneously conduct CAG and
myocardial perfusion imaging. However, the present study is
prospective and in the initial stages. The current literature on
this subject is limited; thus, the observations may not be
clinically applied at present. Further studies are required to
promote DS-CT cardiac imaging technology for comprehensively
assessing patients with CHD or as a potential diagnostic method for
high-risk patients.
References
|
1
|
Sampson UK, Dorbala S, Limaye A, et al:
Diagnostic accuracy of rubidium-82 myocardial perfusion imaging
with hybrid positron emission tomography/computed tomography in the
detection of coronary artery disease. J Am Coll Cardiol.
49:1052–1058. 2007. View Article : Google Scholar
|
|
2
|
Go RT, Marwick TH, MacIntyre WJ, et al: A
prospective comparison of rubidium-82 PET and thallium-201 SPECT
myocardial perfusion imaging utilizing a single dipyridamole stress
in the diagnosis of coronary artery disease. J Nucl Med.
31:1899–1905. 1990.
|
|
3
|
Ruzsics B, Lee H, Zwerner PL,
Gebregziabher M, Costello P and Schoepf UJ: Dual-energy CT of the
heart for diagnosing coronary artery stenosis and myocardial
ischemia-initial experience. Eur Radiol. 18:2414–2424. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ruzsics B, Lee H, Powers ER, Flohr TG,
Costello P and Schoepf UJ: Images in cardiovascular medicine.
Myocardial ischemia diagnosed by dual-energy computed tomography:
correlation with single-photon emission computed tomography.
Circulation. 117:1244–1245. 2008. View Article : Google Scholar
|
|
5
|
Stolzmann P, Leschka S, Scheffel H, et al:
Dual-source CT in step-and-shoot mode: noninvasive coronary
angiography with low radiation dose. Radiology. 249:71–80.
2008.PubMed/NCBI
|
|
6
|
Abdulla J, Abildstrom SZ, Gotzsche O,
Christensen E, Kober L and Torp-Pedersen C: 64-multislice detector
computed tomography coronary angiography as potential alternative
to conventional coronary angiography: a systematic review and
meta-analysis. Eur Heart J. 28:3042–3050. 2007. View Article : Google Scholar
|
|
7
|
Hendel RC, Patel MR, Kramer CM, et al;
American College of Cardiology Foundation Quality Strategic
Directions Committee Appropriateness Criteria Working Group;
American College of Radiology; Society of Cardivascular Computed
Tomography; Society of Cardiovascular Magnetic Resonance; American
Society of Nuclear Cardiology; North American Society for Cardiac
Imaging; Society for Cardiovascular Angiography and Interventions;
Society of Interventional Radiology.
ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness
criteria for cardiac computed tomography and cardiac magnetic
resonance imaging: a report of the American College of Cardiology
Foundation Quality Strategic Directions Committee Appropriateness
Criteria Working Group, American College of Radiology, Society of
Cardivascular Computed Tomography, Society of Cardiovascular
Magnetic Resonance, American Society of Nuclear Cardiology, North
American Society for Cardiac Imaging, Society for Cardiovascular
Angiography and Interventions, and Society of Interventional
Radiology. J Am Coll Cardiol. 48:1475–1497. 2006.
|
|
8
|
Beck T, Burgstahler C, Reimann A, et al:
Technology insight: possible applications of multislice computed
tomography in clinical cardiology. Nat Clin Pract Cardiovasc Med.
2:361–368. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Johnson TR, Krauss B, Sedlmair M, et al:
Material differentiation by dual energy CT: initial experience. Eur
Radiol. 17:1510–1517. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Feuchtner G, Goetti R, Plass A, et al:
Adenosine stress high-pitch 128-slice dual source myocardial
computed tomography perfusion for imaging of reversible myocardial
ischemia: comparison with magnetic resonance imaging. Circ
Cardiovasc Imaging. 4:540–549. 2011.
|
|
11
|
Cerqueira MD, Weissman NJ, Dilsizian V, et
al; American Heart Association Writing Group on Myocardial
Segmentation and Registration for Cardiac Imaging. Standardized
myocardial segmentation and nomenclature for tomographic imaging of
the heart. A statement for healthcare professionals from the
cardiac imaging committee of the council on clinical cardiology of
the American Heart Association. Circulation. 105:539–542. 2002.
View Article : Google Scholar
|
|
12
|
Kachenoura N, Gaspar T, Lodato JA, et al:
Combined assessment of coronary anatomy and myocardial perfusion
using multidetector computed tomography for the evaluation of
coronary artery disease. Am J Cardiol. 103:1487–1494. 2009.
View Article : Google Scholar
|
|
13
|
Scheffel H, Alkadhi H, Plass A, et al:
Accuracy of dual source CT coronary angiography: first experience
in high pretest probability population without heart rate control.
Eur Radiol. 16:2739–2747. 2006.PubMed/NCBI
|
|
14
|
Crossman DC: The pathophysiology of
myocardial ischaemia. Heart. 90:576–580. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jayaweera AR, Wei K, Coggins M, Bin JP,
Goodman C and Kaul S: Role of capillaries in determining CBF
reserve: new insights using myocardial contrast echocardiography.
Am J Physiol. 277:H2363–H2372. 1999.PubMed/NCBI
|
|
16
|
Wang R, Yu W, Wang Y, et al: Incremental
value of dual-energy CT to coronary CT angiography for the
detection of significant coronary stenosis: comparison with
quantitative coronary angiography and single photon emission
computed tomography. Int J Cardiovasc Imaging. 27:647–656. 2011.
View Article : Google Scholar
|
|
17
|
Blankstein R, Shturman LD, Rogers IS, et
al: Adenosine-induced stress myocardial perfusion imaging using
dual-source cardiac computed tomography. J Am Coll Cardiol.
54:1072–1084. 2009.PubMed/NCBI
|
|
18
|
Schwarz F, Ruzsics B, Schoepf UJ, et al:
Dual-energy CT of the heart: principles and protocols. Eur J
Radiol. 68:423–433. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gaemperli O, Schepis T, Valenta I, et al:
Cardiac image fusion from stand-alone SPECT and CT: clinical
experience. J Nucl Med. 48:696–703. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Berman DS, Hachamovitch R, Shaw LJ, et al:
Roles of nuclear cardiology, cardiac computed tomography, and
cardiac magnetic resonance: assessment of patients with suspected
coronary artery disease. J Nucl Med. 47:74–82. 2006.
|