Introduction
Pelvic floor dysfunction includes pelvic organ
prolapse (POP) and stress urinary incontinence (SUI). POP is a
common condition among adult vaginally parous females of all ages,
with a prevalence of up to 37% (1,2).
Investigations in China found that the morbidity of POP among
females aged >60 years was 25% (3). Dysfunctions in extracellular matrix
(ECM) content form the molecular and biochemical basis for POP.
However, the exact underlying molecular and cellular mechanisms
remain poorly understood. Previous studies have shown that POP and
other collagen-associated disorders, including varicose veins and
joint hypermobility, may have a common etiology and originate at
the molecular level of collagen (4–6).
Collagen is a ubiquitous biomaterial and the main
component of connective tissues that provide robustness and
resilience, supporting the stability and plasticity of the vagina.
Type I collagen has a thick diameter and is associated with
hardness, whereas Type III collagen has a fine diameter and is
associated with organizational flexibility (7).
The aim of the present study was to analyze the
association between POP and collagen disorders. We hypothesized
that changes in the ultrastructure and content of collagen are
associated with the angiogenesis of POP. Collagen content, fiber
diameter and collagen ultrastructure were investigated in the
cardinal ligament, uterosacral ligament and paraurethral tissues of
patients with POP. The results were compared with those of the
control group in order to identify the changes in collagen
metabolism in POP and to determine the association between POP and
collagen changes.
Materials and methods
Subjects and grouping
A total of 90 patients who underwent abdominal or
vaginal hysterectomy between March 2009 and March 2011 at the
Department of Gynecology, Second Hospital of Jilin University
(Changchun, China) were selected for the study. The patients were
divided into three groups. The control group (n=30) had a median
age of 60.52±6.58 years, body mass index (BMI) of 24.82±4.32
kg/m2, gravidity of 3.14±0.78 and parity of 1.83±0.92.
The POP group (n=30) had a median age of 63.24±4.84 years, BMI of
25.66±3.56 kg/m2, gravidity of 5.21±0.67 and parity of
3.75±0.68. Finally, the POP with SUI group (n=30) had a median age
of 63.24±4.84 years, BMI of 25.66±3.56 kg/m2, gravidity
of 5.21±0.67 and parity of 3.75±0.68. The groups exhibited no
statistically significant differences in BMI and age (P>0.05).
The participants had not received hormone drugs for almost 3 months
and postoperative pathology results confirmed no ectopic
endometrium, uterine fibroids and ovarian function of
estrogen-associated diseases, including cancer. Candidates with
dysfunctional uterine bleeding, uterine myoma or endometrial
premalignant lesions comprised the control group. Patients who
passed the diagnostic criteria for POP and POP with SUI, according
to their medical history, examination results, pressure tests and
urodynamic inspection, comprised the POP and POP with SUI groups.
The study was conducted with approval from the Ethics Committee of
Jilin University (Changchun, China) and informed written consent
was provided by all participants.
Sample
Samples of ~500 mg cardinal ligaments, 500 mg
uterosacral ligaments and 500 mg paraurethral tissues were
collected from the patients who underwent an abdominal or vaginal
hysterectomy. Specimen preparation for election microscopy included
fixation of tissue in 2.5% glutaraldehyde in 0.1 M sodium
cacodylate buffer at 4°C.
Electron microscopy
Tissues were fixed in 2.5% glutaraldehyde and 0.1 M
sodium cacodylate, and dehydrated in a propylene oxide/epoxy resin
mixture (50:50). Under a JEM-1010 transmission electron microscope
(JEOL, Co., Ltd., Tokyo, Japan) with a magnification of
×10,000–15,000, the morphologies and structures of the collagen
fibers were observed and the diameters were measured. The samples
were meshed into three groups and further divided into three
sections. Ten collagen fibers from each section were observed under
the microscope. The cross-section perpendicular to the long axis of
collagen fibers was selected and the mean values were
calculated.
Light microscopy
Specimens for light microscopy were fixed with 10%
neutral formalin and then embedded in paraffin. Micron sections
were mounted on glass slides and allowed to dry at 37°C for 12 h
then specimens were prepared for hematoxylin and eosin (H&E)
(Solarbio Bioscience & Technology Co., Ltd., Shanghai, China)
and Masson’s trichrome staining using Trichrome Stain (Masson) kit
(Sigma-Aldrich Co,. LLC, St Louis, MO, USA).
Immunohistochemistry
Antibodies against Type I and Type III collagen,
Strept Avidin Biotin Complex kits and SP-9,000 kits were purchased
from Boster Biological Technology, Ltd. (Wuhan, China). Results
were analyzed by randomly selecting five fields of vision
(magnification, ×400) for each specimen. Five images of each vision
were recorded.
Statistical analysis
Mean values were compared with the Student’s t-test
or χ2 analysis using SSPS software, version 14.0 (SPSS,
Inc., Chicago, IL, USA). Two-tailed P-values of <0.05 were
considered to indicate a statistically significant difference.
Results
Light microscope observations
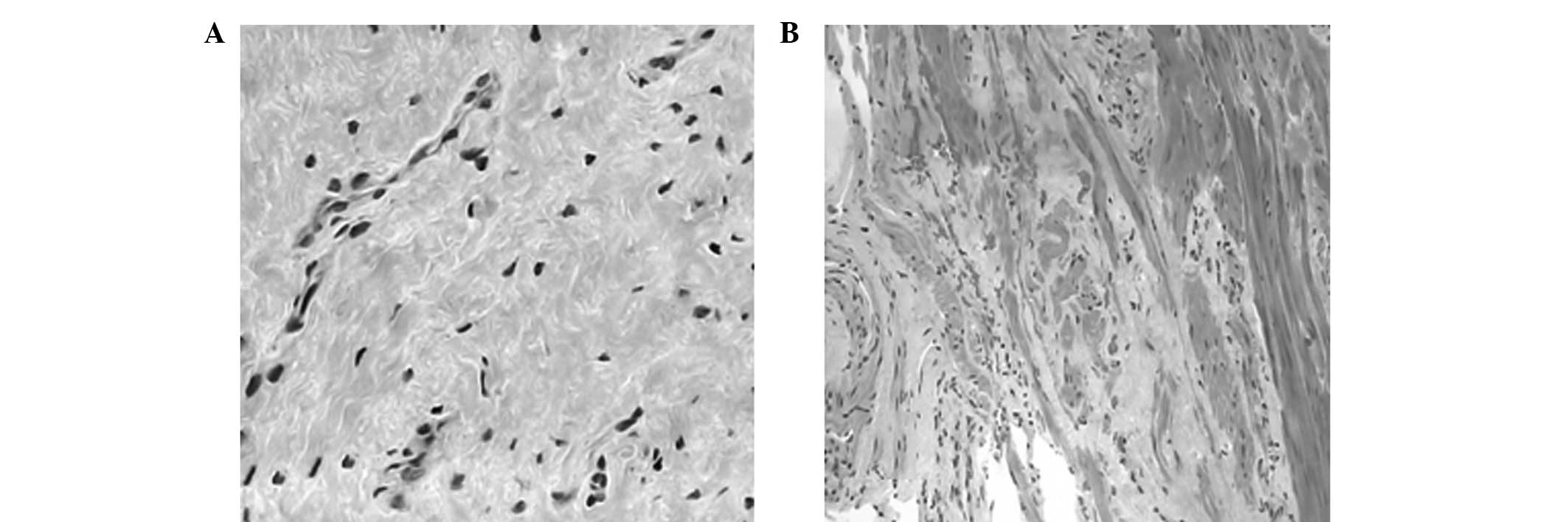
In the POP and POP with SUI groups, Masson’s
trichrome and H&E staining results showed diffuse atrophy of
smooth muscles and a partial fracture. Other observations included
hyaline or mucoid degeneration in sections of muscle tissues, parts
of focal fibrosis distributed as an island, disorder of collagen
fibers arranged in bundles, partial dissolution, swelling of
microvascular endothelial cells, infiltration of peripheral
inflammatory cells and irregular arrangement (Fig. 1A). In the control group, smooth
muscle fibers showed a gross structure, collagen fibers were
arranged in tiny bundles and microvascular cells showed normal
morphology (Fig. 1B).
Electron microscope observations
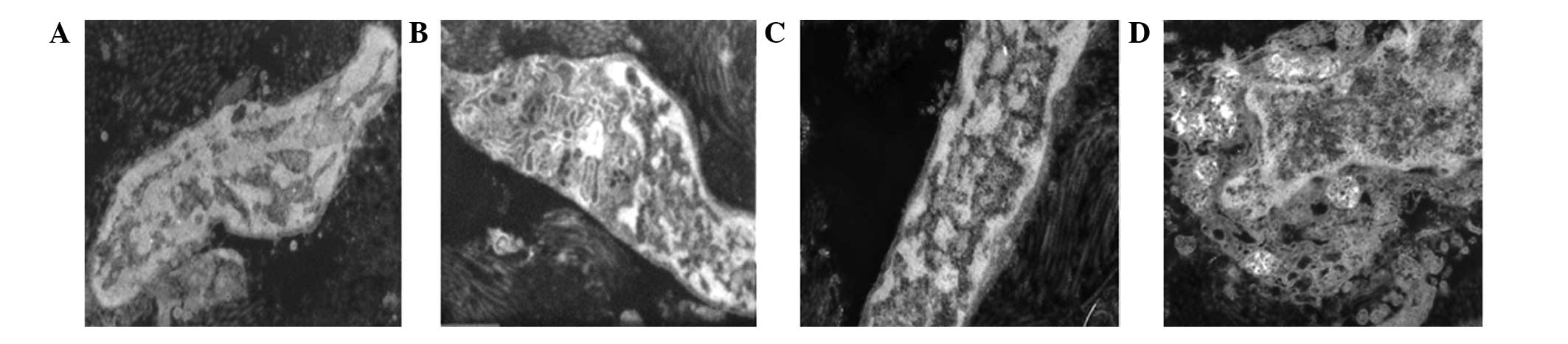
In the POP and POP with SUI groups, fibroblast
metabolism was active and muscle fibroblasts were visible. Cell
vacuoles in the mitochondria were swollen, the crest had decreased
or disappeared and part of the mitochondrial myelin-like structure
had dissolved (Fig. 2A). In
addition, fibroblasts showed normal morphology, cell membrane
integrity was smooth, organelles were plentiful, mitochondria were
clearly visible and the ridge and microvascular endothelial cells
exhibited normal morphology (Fig.
2B). The nuclear size of the fibroblast cells was relatively
large and the rough endoplasmic reticulum in the cytoplasm
increased. The number of mitochondria also increased and the Golgi
apparatus were visible (Fig. 2C).
Muscle fiber cells were saw-tooth-like, branched and ridged or had
a burr-like formation. Nuclear membrane invagination, cell nuclear
pyknosis and heterochromatin were increased. The diameter of
collagen fibrils around the cells differed and larger gaps were
visible. Immature microvascular endothelial cell aggregation was
discontinuous. Cells were swollen and the cytoplasm was increased
(Fig. 2D).
Collagen fibril diameter
In the POP and POP with SUI groups, the collagen
fibril diameters in the cardinal ligaments, uterosacral ligaments
and paraurethral tissues were significantly greater compared with
those in the control group (P<0.01; Table I).
 | Table ICollagen fibril diameter of groups
(nm). |
Table I
Collagen fibril diameter of groups
(nm).
| Parameter | Cardinal
ligament | Uterosacral
ligament | Paraurethral
tissues |
|---|
| Control group | 57.72±2.61a | 55.95±3.61b | 43.73±2.51c |
| POP group | 78.83±8.28a′d | 77.72±7.32b′d | 60.72±5.29c′d |
| POP with SUI
group | 82.23±8.49a″d | 85.28±7.31b″d | 63.39±5.34c″d |
| t-value | a:a′
9.333 | b:b′
10.575 | c:c′
11.424 |
| a:a″
10.837 | b:b″
14.247 | c:c″
13.219 |
| P-value | a:a′
<0.01 | b:b′
<0.01 | c:c′
<0.01 |
| a:a″
<0.01 | b:b″
<0.01 | c:c″
<0.01 |
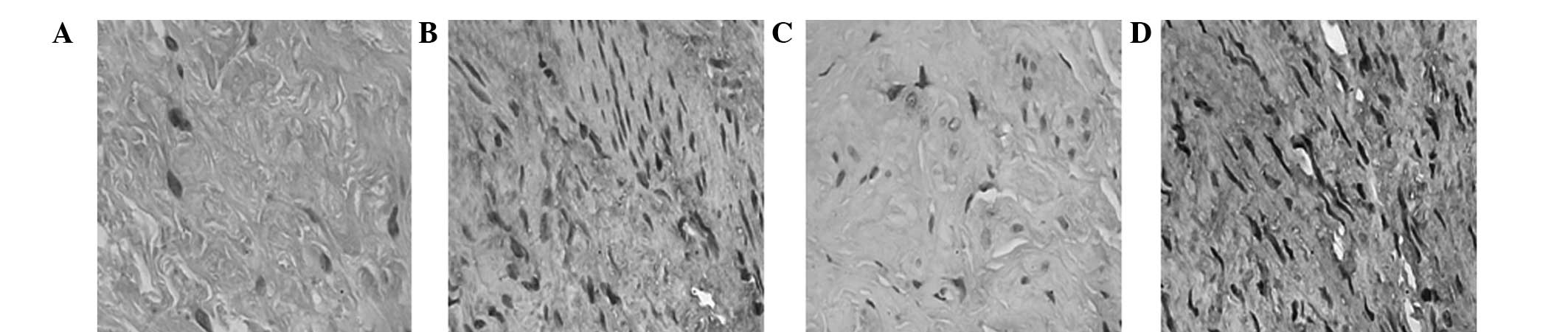
Expression of Type I collagen
protein
In the control group, Type I collagen proteins in
the cardiac ligaments, sacral ligaments and paraurethral tissues
were asymmetrically stained. The proteins were arranged as ribbons
with diffuse distribution or focal adhesion (Fig. 3A). In the POP or POP with SUI
groups, Type I collagen proteins in the cardiac ligaments, sacral
ligaments and paraurethral tissues were stained and distributed in
unusual fractions (Fig. 3B).
The measurements from the image analysis system
Image-Pro Plus 6.0 (IPP 6.0)revealed that the expression levels of
Type I collagen in the cardiac ligaments of the POP group were
26.47% lower compared with the control group. However, in the POP
with SUI group, the expression levels were 36.24% lower than the
level in the control group (P<0.01). The expression levels of
Type I collagen in the sacral ligaments of the POP group were
29.03% lower than the expression levels in the control group, but
in the POP with SUI group, the expression levels were 41.89% lower
compared with the control group (P<0.01). When compared with the
control group, the expression levels of Type I collagen in the
paraurethral tissues of the POP group were 24.43% lower, while in
the POP with SUI group, the levels were 31.14% lower (P<0.01;
Table II).
 | Table IIExpression of Type I collagen in all
groups (OD). |
Table II
Expression of Type I collagen in all
groups (OD).
| Groups | Cardiac ligament | Sacral ligament | Paraurethral
tissue |
|---|
| Control (n=30) | 124.56±5.39 | 123.74±5.65 | 116.57±5.22 |
| POP (n=30) | 91.59±3.28a | 87.83±3.87a | 88.10±3.90a |
| POP with SUI
(n=30) | 79.42±6.12ab | 71.91±4.86ab | 80.28±4.76ab |
| F-value | 346.27 | 423.71 | 255.63 |
Expression of Type III collagen
protein
In the control group, Type III collagen proteins in
the cardiac ligaments, sacral ligaments and paraurethral tissues
were stained with diffuse distribution or focal adhesion (Fig. 3C). In the POP and POP with SUI
groups, Type III collagen proteins in the cardiac ligaments, sacral
ligaments and paraurethral tissues were marginally stained
(Fig. 3D).
Measurements from the image analysis system IPP 6.0
revealed that when compared with the control group, the expression
levels of Type III collagen in the cardiac ligaments of the POP
group were 21.49% lower, while in the POP with SUI group the levels
were 47.73% lower (P<0.01). The expression levels of Type III
collagen in the sacral ligaments of the POP group were 10.84% lower
compared with the control group. However, in the POP with SUI
group, the expression levels were 39.35% lower compared with the
control group (P<0.01). In addition, the expression levels of
Type III collagen in the paraurethral tissues of the POP group were
15.74% lower than the levels in the control group, while in the POP
with SUI group, the levels were 35.00% lower compared with the
control group (P<0.01; Table
III).
 | Table IIIExpression of Type III collagen in
all groups (OD). |
Table III
Expression of Type III collagen in
all groups (OD).
| Groups | Cardiac
ligament | Sacral
ligament | Paraurethral
tissue |
|---|
| Control (n=30) | 126.06±4.83 | 115.31±5.53 | 122.44±4.17 |
| POP (n=30) | 98.97±6.66a | 102.84±5.17a | 103.17±4.80a |
| POP with SUI
(n=30) | 65.90±4.11ab | 69.94±4.22ab | 79.59±3.83ab |
| F-value | 355.55 | 218.04 | 287.62 |
Discussion
We hypothesized that collagen status has an
important function in POP angiogenesis. The concentration of Type I
and III collagen was found to significantly decrease in POP
patients and active metabolism in the ultrastructure of collagen
resulted in a prolapse of the pelvic floor. In the POP group,
electron microscopy revealed that a number of mitochondria in
fibroblasts swelled to an empty bubble, whereas others transformed
into myelin-like structures. Smooth muscle bundles showed diffuse
atrophy and hyaline or mucinous degeneration. In addition, collagen
fibers exhibited a disorderly arrangement in partial solution.
Mitochondria are one of the most sensitive
organelles to various injuries. The formation of myelin-like
structures is a common sign of mitochondrial membrane damage. In
addition, extreme swelling and transformation to small bubble-like
structures are signs of cell necrosis. Thus, ultrastructural
changes in smooth muscle cells indicate a decrease or loss in cell
function, which is consistent with the results of a previous study
(8). Tseng et al compared
microarray gene expression profiles and demonstrated that an
increase in the expression of mitochondrial and ribosomal
protein-coding genes also increased apoptosis-associated genes in
patients with POP (9). Ferrari
et al investigated 233 females and analyzed polymorphisms at
the Type I collagen Sp1 site and functional polymorphisms in the
promoters of matrix metalloproteinase (MMP)-1, −3 and −9. The
results demonstrated that the MMP polymorphisms possibly contribute
in mediating susceptibility to POP (10), indicating that irreversible cell
damage of connective tissues and smooth muscles may be the result
of MMP function in patients with POP.
Electron microscopy also revealed discontinuous
gathering and swelling of immature microvascular endothelial cells
and increased cytoplasm in patients with POP, which were not
observed in the control group. However, novel microvascular
functions are unable to compensate for vascular lesions caused by
inadequate blood flow and hypoxia, resulting in increased smooth
muscle injury. Goepel et al analyzed the connective tissues
in the uterine artery wall of postmenopausal females with and
without POP and hypothesized that the ECM may change in response to
mechanical stretching (11).
In the present study, collagen fibrils surrounding
the cells were found to have varied sizes with large gaps between
each fibril. In the POP group, the collagen fibril diameter was
significantly greater compared with the control group, which was
consistent with the results of Abramowitch et al (12). The pelvic floor, organized by
resynthesis and degradation of elastic fibers, undergoes
significant changes (13). If the
pelvic floor is not remodeled, the elastic fiber network structure
becomes damaged, resulting in structural and functional defects of
the reproductive tract. Transforming growth factor-β pathways have
been shown to be involved in ECM degradation, which is modulated by
reproductive hormones and selective estrogen receptor modulators
(14). Decreased HOXA11 gene
expression is reportedly associated with decreased collagen and
increased MMP-2 expression levels in the uterosacral ligaments of
females with POP (15). In murine
vaginal stromal cells, fibulin-5 inhibits the β1
integrin-dependent, fibronectin-mediated upregulation of MMP-9.
Treatment of mice with β-aminopropionitrile, an inhibitor of matrix
cross-linking enzymes, induces subclinical POP (16).
In the present study, the POP and POP with SUI
groups exhibited significantly lower expression levels of Type I
and III collagen when compared with the control group. The
reduction in collagen content in the connective tissues is
attributed to massive atrophy, degeneration, necrosis and fibrosis,
which may also be the possible causes of POP and SUI. Zhou et
al evaluated the elastogenic (a measure of stiffness) protein
expression of Type I and Type III collagen in the vagina and
demonstrated that vaginal wall tissues were stiffer in females with
POP (17). Iwahashi and Muragaki
found that decreased expression levels of Type III collagen have an
important function in determining the physiology and structure of
the uterine cervix tissues in POP (18). In connective tissues, the elastic
fiber content decreases, fibers are distributed fragmentally and
elastic fiber maturity manifests as declined desmosine levels and
reduced expression levels of Fibulin-5 and LOX (19–21).
Smooth muscle degeneration, ECM metabolism and apoptosis are
inhibited in patients with POP (22). This inhibition may be caused by
genetic factors that are associated with the original collagen
metabolism, cell cycle or apoptosis, which result in POP.
Furthermore, Pal et al concluded that moderate to severe POP
is an independent predictor of incident spine [hazard ratio (HR),
2.61; 95% confidence interval (CI), 1.04–6.56; P=0.042] and lower
arm fractures (HR, 1.87; 95% CI, 1.06–3.29; P=0.030) (23). Feola et al demonstrated that
worsening pelvic supportive ability was negatively correlated with
decreased collagen alignment (r2=−0.66) and mechanical
properties (r2=−0.67) (24). Moreover, Connell et al
reported that Type III collagen expression was directly associated
with the presence of prolapse rather than age or menopausal status,
and is suppressed with the use of hormone replacement therapy. If
these mechanisms are elucidated, supplementary therapeutic agents
with estrogens may assist in rebuilding these ligaments (25).
In conclusion, changes in collagen fibers and
microvascular cells result in cell apoptosis and necrosis, causing
abnormal ECM metabolism. POP is an acquired disorder of the ECM and
therapies targeting matrix proteases may be efficient for
preventing or ameliorating POP (7).
References
|
1
|
Swift S, Woodman P, O’Boyle A, et al:
Pelvic Organ Support Study (POSST): the distribution, clinical
definition, and epidemiologic condition of pelvic organ support
defects. Am J Obstet Gynecol. 192:795–806. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kerkhof MH, Hendriks L and Brölmann HA:
Changes in connective tissue in patients with pelvic organ prolapse
- a review of the current literature. Int Urogynecol J Pelvic Floor
Dysfunct. 20:461–474. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhou Y, Ling O and Bo L: Expression and
significance of lysyl oxidase-like 1 and fibulin-5 in the cardinal
ligament tissue of patients with pelvic floor dysfunction. J Biomed
Res. 27:23–28. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lammers K, Lince SL, Spath MA, et al:
Pelvic organ prolapse and collagen-associated disorders. Int
Urogynecol J. 23:313–319. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yucel N, Usta A, Guzin K, et al:
Immunohistochemical analysis of connective tissue in patients with
pelvic organ prolapse. J Mol Histol. 44:97–102. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cho HJ, Jung HJ, Kim SK, Choi JR, Cho NH
and Bai SW: Polymorphism of a COLIA1 gene Sp1 binding site in
Korean women with pelvic organ prolapse. Yonsei Med J. 50:564–568.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Budatha M, Roshanravan S, Zheng Q, et al:
Extracellular matrix proteases contribute to progression of pelvic
organ prolapse in mice and humans. J Clin Invest. 121:2048–2059.
2011. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Boreham MK, Wai CY, Miller RT, Schaffer JI
and Word RA: Morphometric analysis of smooth muscle in the anterior
vaginal wall of women with pelvic organ prolapsed. Am J Obstet
Gynecol. 187:56–63. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tseng LH, Chen I, Lin YH, Chen MY, Lo TS
and Lee CL: Genome-based expression profiles study for the
pathogenesis of pelvic organ prolapse: an array of 33 genes model.
Int Urogynecol J. 21:79–84. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ferrari MM, Rossi G, Biondi ML, Viganò P,
Dell’utri C and Meschia M: Type I collagen and matrix
metalloproteinase 1, 3 and 9 gene polymorphisms in the
predisposition to pelvic organ prolapse. Arch Gynecol Obstet.
285:1581–1586. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Goepel C, Johanna Kantelhardt E, Karbe I,
Stoerer S and Dittmer J: Changes of glycoprotein and collagen
immunolocalization in the uterine artery wall of postmenopausal
women with and without pelvic organ prolapse. Acta Histochem.
113:375–381. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Abramowitch SD, Feola A, Jallah Z and
Moalli PA: Tissue mechanics, animal models, and pelvic organ
prolapse: a review. Eur J Obstet Gynecol Reprod Biol. 144(Suppl 1):
S146–S158. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Edwall L, Carlström K and Fianu Jonasson
A: Markers of collagen synthesis and degradation in urogenital
tissue and serum from women with and without uterovaginal prolapse.
Mol Hum Reprod. 14:193–197. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Petros PE: Re: Alterations in connective
tissue metabolism in stress incontinence and prolapse: B. Chen and
J. Yeh J Urol 2011; 186: 1768–1772. J Urol. 187:22812012.PubMed/NCBI
|
|
15
|
Ma Y, Guess M, Datar A, et al: Knockdown
of Hoxa11 in vivo in the uterosacral ligament and uterus of mice
tesults in altered collagen and matrix metalloproteinase activity.
Biol Reprod. 86:1002012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ewies AA, Al-Azzawi F and Thompson J:
Changes in extracellular matrix proteins in the cardinal ligaments
of post-menopausal women with or without prolapse: a computerized
immunohistomorphometric analysis. Hum Reprod. 18:2189–2195. 2003.
View Article : Google Scholar
|
|
17
|
Zhou L, Lee JH, Wen Y, et al:
Biomechanical properties and associated collagen composition in
vaginal tissue of women with pelvic organ prolapse. J Urol.
188:875–880. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Iwahashi M and Muragaki Y: Decreased type
III collagen expression in human uterine cervix of prolapse uteri.
Exp Ther Med. 2:271–274. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Klutke J, Ji Q, Campeau J, et al:
Decreased endopelvic fascia elastin content in uterine prolapse.
Acta Obstet Gynecol Scand. 87:111–115. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Söderberg MW, Byström B, Kalamajski S,
Malmström A and Ekman-Ordeberg G: Gene expressions of small
leucine-rich repeat proteoglycans and fibulin-5 are decreased in
pelvic organ prolapse. Mol Hum Reprod. 15:251–257. 2009.PubMed/NCBI
|
|
21
|
Jung HJ, Jeon MJ, Yim GW, Kim SK, Choi JR
and Bai SW: Changes in expression of fibulin-5 and lysyl
oxidase-like 1 associated with pelvic organ prolapse. Eur J Obstet
Gynecol Reprod Biol. 145:117–122. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Takacs P, Nassiri M, Gualtieri M,
Candiotti K and Medina CA: Uterosacral ligament smooth muscle cell
apoptosis is increased in women with uterine prolapse. Reprod Sci.
16:447–452. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pal L, Hailpern SM, Santoro NF, et al:
Increased incident hip fractures in postmenopausal women with
moderate to severe pelvic organ prolapse. Menopause. 18:967–973.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Feola A, Abramowitch S, Jones K, Stein S
and Moalli P: Parity negatively impacts vaginal mechanical
properties and collagen structure in rhesus macaques. Am J Obstet
Gynecol. 203:5952010.PubMed/NCBI
|
|
25
|
Connell KA, Guess MK, Chen H, Andikyan V,
Bercik R and Taylor HS: HOXA11 is critical for development and
maintenance of uterosacral ligaments and deficient in pelvic
prolapse. J Clin Invest. 118:1050–1055. 2008.PubMed/NCBI
|