Introduction
The balance between cerebral oxygen supply and
demand is necessary for the brain to maintain normal physiological
activity. Patients with severe traumatic brain injury (sTBI)
exhibit serious cerebral oxygen metabolism dysfunction at an early
stage, which is a leading cause of mortality. Appropriate treatment
for maintaining the cerebral oxygen supply-demand balance and
reducing the relevant complications has great clinical significance
(1). The body is in a state of
inflammation following sTBI and the serum C-reactive protein (CRP)
level increases rapidly, exacerbating the pathological damage
(2,3). CRP has been reported to be a
sensitive indicator that reflects cerebral trauma severity
(4). Ulinastatin, a protease
inhibitor, is predominantly used to treat acute and chronic
pancreatitis. It has been reported that ulinastatin exhibits
cerebral protective effects and may inhibit the release of
inflammatory mediators, however, there is limited research on the
use of ulinastatin in the treatment for sTBI (5). Therefore, the present study focused
on the application of ulinastatin in the treatment of sTBI and
investigated the effects of ulinastatin on cerebral oxygen
metabolism and the level of CRP.
Subjects and methods
Subjects
In total, 92 patients admitted to the Intensive Care
Unit (ICU) in the First Affiliated Hospital of Xinxiang Medical
University (Xinxiang, China) between February 2010 and May 2013
with a clinical diagnosis of sTBI were enrolled in the study.
Patients were included in the study if the following criteria were
met: Diagnosis of sTBI by computed tomography or magnetic resonance
imaging; Glasgow Coma Scale (GCS) score of <8; and admittance to
ICU within 8 h after injury (6).
Exclusion criteria included combined brain complications, combined
severe injury and patient mortality within seven days following
injury (7). A total of 92 patients
with sTBI were randomly divided into two groups (n=46 per group).
The male-to-female ratio, age range, average age and GCS score in
the control group were 41:5, 28–63 years, 45.27±15.33 years and
5.49±0.71, respectively, while in the observation group, the
parameters were 39:7, 25–61 years, 43.19±15.60 years and 5.52±0.74,
respectively. The gender ratio, age and GCS score of the two groups
exhibited no statistically significant differences (P>0.05). The
study was conducted in accordance with the Declaration of Helsinki
and with approval from the Ethics Committee of the First Affiliated
Hospital of Xinxiang Medical University. Written informed consent
was obtained from all the participants.
Treatment
All the patients admitted to the ICU were
administered conventional therapy, including ventilator-assisted
therapy, oxygen therapy, intracranial pressure reduction,
dehydration, bleeding control, neuroprotection and appropriate
symptomatic treatments. The control group received conventional
therapy plus a placebo (0.9% sodium chloride), while the
observation group received conventional therapy plus ulinastatin
(200,000 units; Techpool Bio-Pharma Co., Ltd, Guangzhou, China) via
intravenous injection twice a day for seven days.
Cerebral oxygen metabolism
monitoring
Cerebral oxygen metabolism was monitored as
previously described (8). Arterial
and jugular venous blood was collected in the morning for blood gas
analysis (ABL80; Radiometer Medical ApS, Copenhagen, Denmark). The
parameters recorded included hemoglobin concentration (Hb), jugular
venous blood lactate (JVBL), arterial oxygen saturation
(SaO2), jugular venous bulb oxygen saturation
(SjvO2), partial pressure of O2 in the
arterial blood (PaO2) and partial pressure of
O2 in the jugular venous blood (PjvO2).
Parameters were calculated as follows: Arterial oxygen content
(CaO2) = (Hb × 1.36 × SaO2) + (0.003 ×
PaO2); venous oxygen content (CjvO2) = (Hb ×
1.36 × SjvO2) + (0.003 × PjvO2);
arteriovenous oxygen content difference (AVDO2) =
CaO2 - CjvO2; and cerebral extraction of
oxygen (CEO2) = 1 -
(CjvO2/CaO2).
Assay of CRP level
Peripheral blood was collected from the patients on
day 1, 3, 5 and 7 in the morning and the CRP levels were determined
using an ELISA kit, according to the manufacturer’s instructions
(Shanghai Hengyuan Biotechnology Co., Ltd, Shanghai, China).
Statistical analysis
Data were analyzed using SPSS 15.0 software (SPSS,
Inc., Chicago, IL, USA) and all the data are expressed as the mean
± standard deviation. Data were analyzed using the unpaired
Student’s t test for comparisons between two groups and the
χ2 test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Comparison of cerebral oxygen metabolism
parameters between the two groups
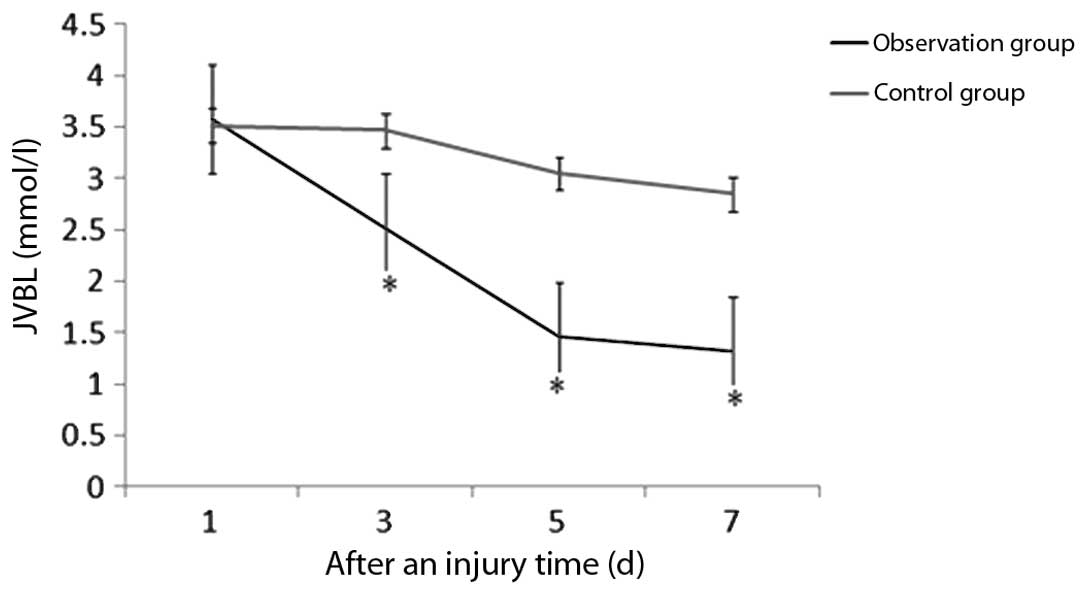
JVBL, SjvO2, AVDO2 and
CEO2 measurements for the two groups are shown in
Table I. As shown in Fig. 1, the level of JVBL in the control
group decreased as compared with the level at day 1, however, no
statistically significant differences were observed (P>0.05). By
contrast, the observation group exhibited a significant decrease in
JVBL levels (P<0.05) when compared with the level on day 1, and
the levels were also lower compared with the control group
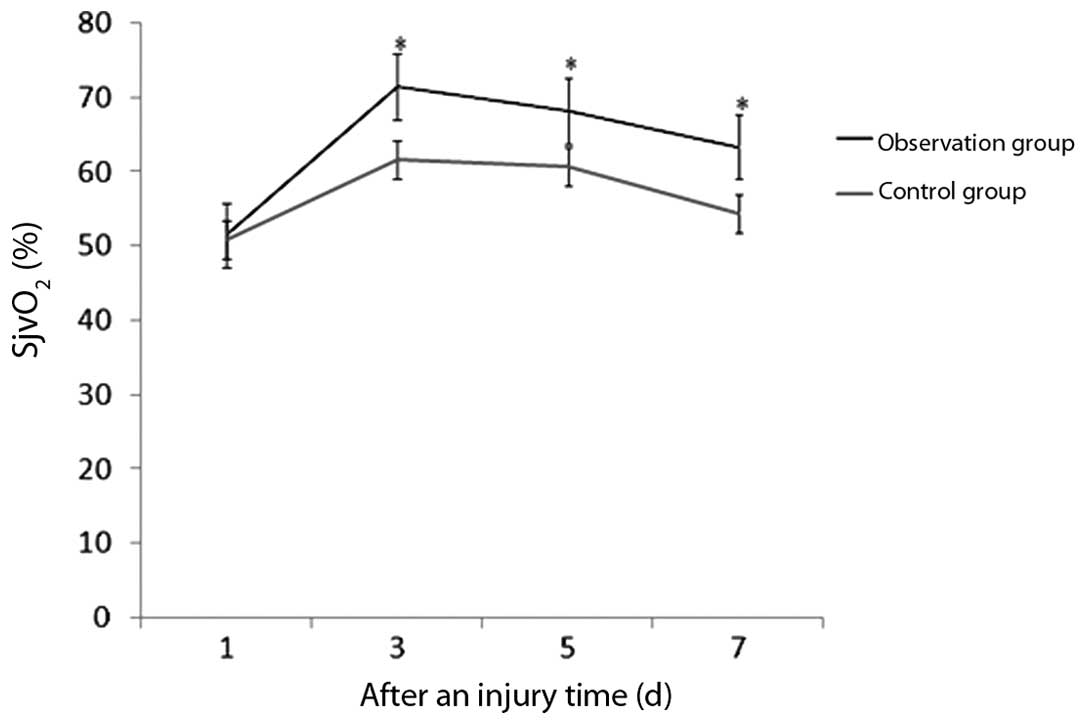
(P<0.05). The value of SjvO2 in the patients
increased following injury and peaked on day 3. Statistically
significant differences were observed between the two groups with
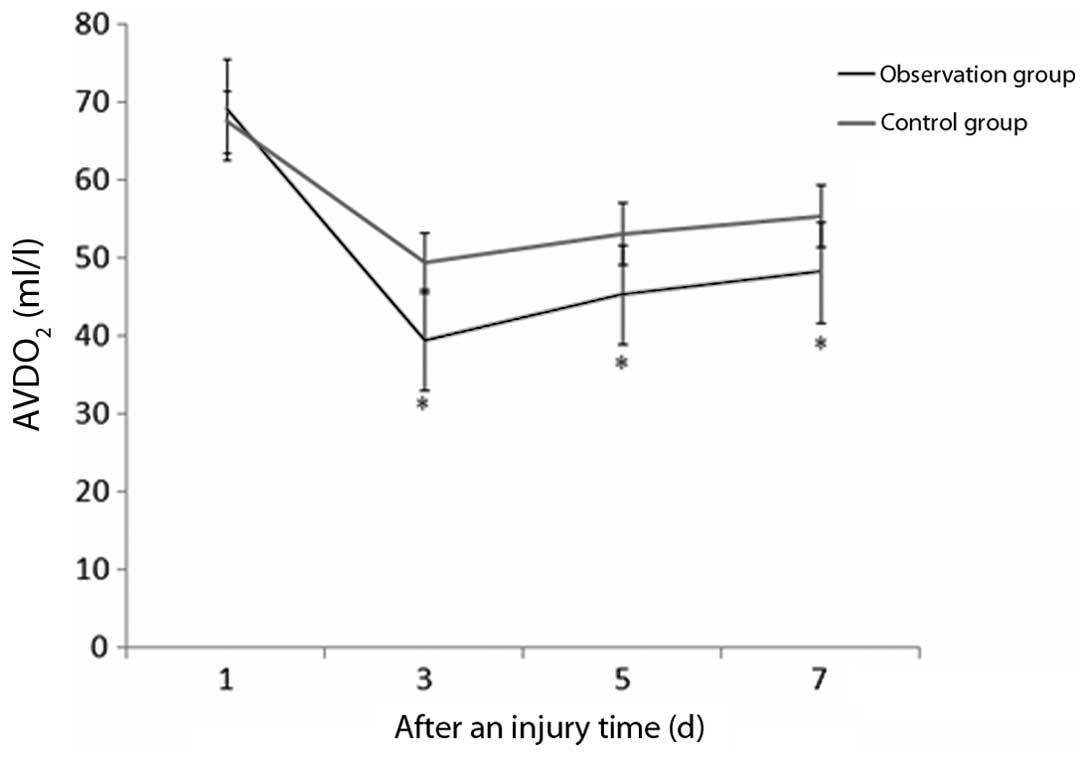
regard to SjvO2 on day 3, 5 and 7 (Fig. 2). The AVDO2 level in the
two groups decreased, and statistically significant differences
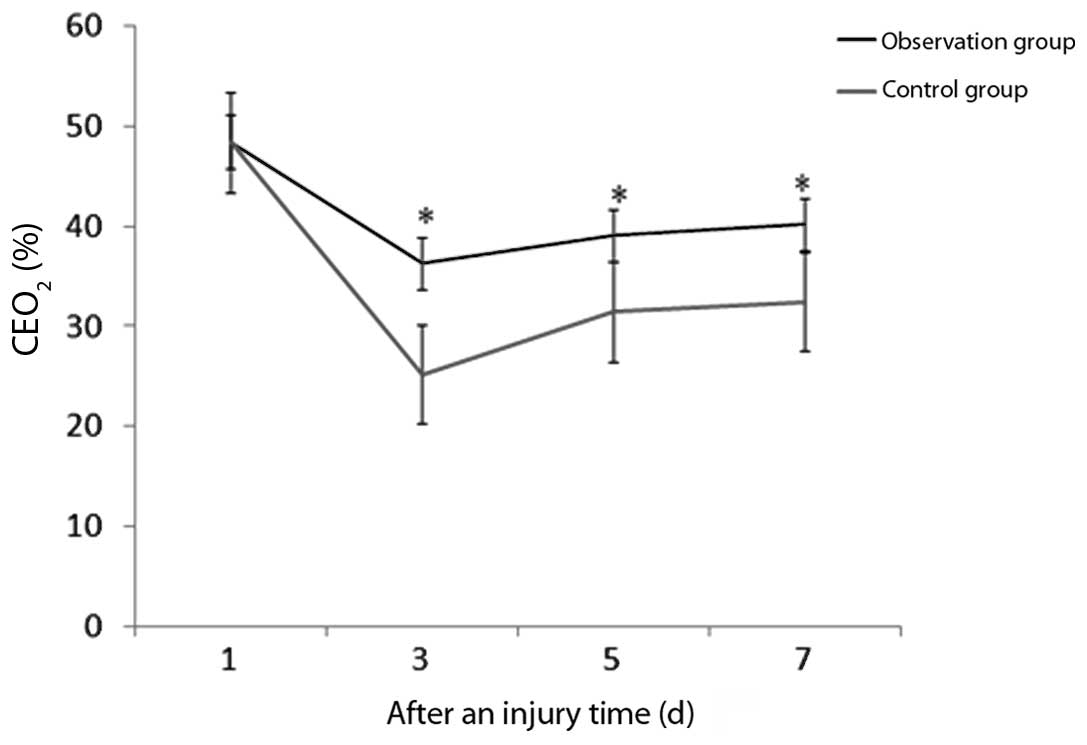
were observed between the groups (Fig.
3). In addition, the CEO2 level in the two groups
decreased, with the level in the control group decreasing
significantly as compared with observation group (Fig. 4).
 | Table IComparison of cerebral oxygen
metabolism parameters between the two groups. |
Table I
Comparison of cerebral oxygen
metabolism parameters between the two groups.
| Groups | Index | Day 1 | Day 3 | Day 5 | Day 7 |
|---|
| Observation | JVBL (mmol/l) | 3.58±1.14 | 2.53±0.69a,b | 1.46±0.53a,b | 1.32±0.39a,b |
| SjvO2
(%) | 51.49±7.21 | 71.47±7.85a,b | 68.21±5.48a,b | 63.36±5.13a,b |
| AVDO2
(ml/l) | 69.18±14.32 | 39.56±11.39a,b | 45.38±9.24a,b | 48.26±12.43a,b |
| CEO2
(%) | 48.48±4.52 | 36.25±5.83a,b | 39.13±5.23a,b | 40.18±5.47b |
| Control | JVBL (mmol/l) | 3.52±1.12 | 3.47±0.72 | 3.05±0.44 | 2.85±0.36 |
| SjvO2
(%) | 50.83±7.05 | 61.52±6.59a | 60.72±5.22a | 54.27±5.06 |
| AVDO2
(ml/l) | 67.55±13.40 | 49.41±12.18a | 53.19±7.32a | 55.45±13.30 |
| CEO2
(%) | 48.39±4.43 | 25.19±5.07a | 31.46±4.92a | 32.43±4.15a |
Comparison of the CRP levels between the
two groups
As shown in Table
II, the CRP levels of the two groups increased and peaked on
day 3 in the observation group. The CRP levels in the observation
group significantly decreased on day 5 (35.27±15.18 mg/l) and day 7
(22.65±10.48 mg/l), and were lower than the values observed in the
control group (56.19±13.24 mg/l and 47.36±15.73 mg/l,
respectively); statistically significant differences were observed
between the two groups (P<0.05).
 | Table IIComparison of the CRP levels between
the two groups (mg/l). |
Table II
Comparison of the CRP levels between
the two groups (mg/l).
| Groups | Day 1 | Day 3 | Day 5 | Day 7 |
|---|
| Observation
(n=46) | 32.15±10.28 | 51.46±11.39 | 35.27±15.18a | 22.65±10.48a |
| Control (n=46) | 31.49±10.07 | 47.22±12.36 | 56.19±13.24 | 47.36±15.73 |
Comparison of gastrointestinal bleeding
and mortality rates between the two groups
Gastrointestinal bleeding and mortality rates were
also recorded for 30 days. In the control group, 20 patients
(43.48%) showed gastrointestinal bleeding and 15 patients (32.61%)
succumbed to their illness. In the observation group, only 11
patients (23.91%) showed gastrointestinal bleeding and eight
mortalities (17.39%) were recorded. Statistically significant
differences were observed when compared with the control group
(P<0.05).
Discussion
Cerebral ischemia-hypoxia occurs following the
development of sTBI. Since the cerebral oxygen metabolism
indicators, including JVBL, SjvO2, AVDO2 and
CEO2, reflect the state of cerebral microcirculation and
oxygen supply-demand, monitoring the associated indicators is an
effective method for the early detection of cerebral ischemia and
hypoxia (9). In addition, the body
is in a state of inflammation with increased serum CRP levels
following sTBI, and the serum CRP levels decrease when the body is
recovered (10). Ulinastatin, as a
protease inhibitor, has significant anti-inflammatory effects and
has been used to treat pancreatitis. Recently, clinical studies
have revealed that ulinastatin improves the circulation of shock
caused by cell damage and exhibits cerebral protective effects
(11). To date, there has been
limited clinical use of ulinastatin in the treatment of sTBI. Thus,
the present study aimed to investigate the effects of ulinastatin
on cerebral oxygen metabolism and CRP levels.
A decrease of blood flow in cerebral circulation
induces the brain tissue to draw oxygen from the blood at a higher
proportion in order to maintain normal metabolism. By contrast,
when the blood flow increases, the proportion of oxygen drawn from
blood decreases, which results in increased oxygen content in
cerebral circulation (12). Since
the internal jugular vein is the main channel of cerebral
circulation, blood gas analysis of the internal jugular vein
indirectly reflects cerebral oxygen metabolism (elevated
SjvO2 indicates hyperemia in the brain).
AVDO2 and CEO2, calculated using Fick’s
equations, directly reflect the cerebral microcirculation and
oxygen supply-demand (13,14). The results of the present study
revealed that ulinastatin decreases the levels of JVBL and
AVDO2 and increases the levels of SjvO2 and
CEO2 in patients with sTBI. These results further
demonstrate that ulinastatin improves cerebral ischemia-hypoxia and
enhances the utilization of oxygen (15). A previous study reported that
ulinastatin reduces the rate of mortality by decreasing
gastrointestinal bleeding and protecting immunological and renal
functions (16). The results of
the present study demonstrated that the CRP level increased rapidly
following sTBI and ulinastatin administration lowered the CRP level
significantly. Less gastrointestinal bleeding and a lower mortality
rate was observed in the observation group, indicating that
ulinastatin is effective in the treatment of sTBI. The potential
mechanism of ulinastatin with regard to the treatment of sTBI may
involve the clearance of oxygen free radicals and inhibiting the
release of lysosomal enzymes and inflammatory mediators (17).
In conclusion, ulinastatin administration
effectively improves the prognosis of patients with sTBI by
improving cerebral oxygen metabolism, lowering the CRP level and
reducing gastrointestinal bleeding and the mortality rate.
References
|
1
|
Rockswold SB, Rockswold GL, Zaun DA and
Liu J: A prospective, randomized Phase II clinical trial to
evaluate the effect of combined hyperbaric and normobaric hyperoxia
on cerebral metabolism, intracranial pressure, oxygen toxicity, and
clinical outcome in severe traumatic brain injury. J Neurosurg.
118:1317–1328. 2013. View Article : Google Scholar
|
|
2
|
Lee KS, Shim JJ, Yoon SM and Bae HG:
Prognostic value of the C-reactive protein levels in the head
injury. J Kor Eurotraumatol Soc. 1:57–60. 2005.
|
|
3
|
da Gullo JS, Bertotti MM, Silva CC, et al:
Hospital mortality of patients with severe traumatic brain injury
is associated with serum PTX3 levels. Neurocrit Care. 14:194–199.
2011.PubMed/NCBI
|
|
4
|
Cao LJ, Wang J, Hao PP, Sun CL and Chen
YG: Effects of ulinastatin, a urinary trypsin inhibitor, on
synaptic plasticity and spatial memory in a rat model of cerebral
ischemia/reperfusion injury. Chin J Physiol. 54:435–442.
2011.PubMed/NCBI
|
|
5
|
Wang X, Xue Q, Yan F, et al: Ulinastatin
as a neuroprotective and anti-inflammatory agent in infant piglets
model undergoing surgery on hypothermic low-flow cardiopulmonary
bypass. Paediatr Anaesth. 23:209–216. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Stewart TC, Alharfi IM and Fraser DD: The
role of serious concomitant injuries in the treatment and outcome
of pediatric severe traumatic brain injury. J Trauma Acute Care
Surg. 75:836–842. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Schmidt AT, Hanten G, Li X, et al:
Emotional prosody and diffusion tensor imaging in children after
traumatic brain injury. Brain Inj. 27:1528–1535. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lord LD, Expert P, Huckins JF and
Turkheimer FE: Cerebral energy metabolism and the brain’s
functional network architecture: an integrative review. J Cereb
Blood Flow Metab. 33:1347–1354. 2013.
|
|
9
|
McCarthy MC, Moncrief H, Sands JM, et al:
Neurologic outcomes with cerebral oxygen monitoring in traumatic
brain injury. Surgery. 146:585–591. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mayer CL, Huber BR and Peskind E:
Traumatic brain injury, neuroinflammation, and post-traumatic
headaches. Headache. 53:1523–1530. 2013.PubMed/NCBI
|
|
11
|
Wang XH, Wei RL, Fan H and Hu JH: The
protective effects of edaravone combined with ulinastatin on the
treatment of brain iniury in rats with severe acute pancreatitis.
Zhonghua Gan Dan Wai Ke Za Zhi. 19:544–549. 2013.(In Chinese).
|
|
12
|
Bouzat P, Millet A, Boue Y, et al: Changes
in brain tissue oxygenation after treatment of diffuse traumatic
brain injury by erythropoietin. Crit Care Med. 41:1316–1324. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kamenskaia OV, Loginova IIu, Karpenko AA,
Karas’kov AM and Kuzhuget RA: Oxygen supply to the brain in chronic
disturbances of cerebral circulation in patients with pathology of
brachiocephalic arteries. Kardiologiia. 53:49–53. 2013.(In
Russian).
|
|
14
|
Faraco G, Moraga A, Moore J, et al:
Circulating endothelin-1 alters critical mechanisms regulating
cerebral microcirculation. Hypertension. 62:759–766. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tu Y, Diao YF, Yang XP, Sun HT and Zhang
S: Effect of ulinastatin in traumatic brain injury with multiple
injuries. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 24:677–679.
2012.(In Chinese).
|
|
16
|
Xu CE, Zou CW, Zhang MY and Guo L: Effects
of high-dose ulinastatin on inflammatory response and pulmonary
function in patients with type-A aortic dissection after
cardiopulmonary bypass under deep hypothermic circulatory arrest. J
Cardiothorac Vasc Anesth. 27:479–484. 2013. View Article : Google Scholar
|
|
17
|
Cao BP, Zhang L, Su N, Wang K, Bian H, Fei
Z and Li B: Protective effects of ulinastatin on mice with
traumatic brain injury. Zhonghua Shen Jing Wai Ke Ji Bing Yan Jiu
Za Zhi. 12:244–246. 2013.(In Chinese).
|