Introduction
Type 2 diabetes mellitus (T2DM), which is an
endocrine and metabolic disease, has become the third most common
type of non-infectious disease worldwide following cardiovascular
disease and cancer (1).
Conventional treatment of T2DM tends to lead to various
complications. Previous studies investigating obesity treatments
have demonstrated that Roux-en-Y gastric bypass (GBP) is able to
induce the remission of T2DM (2–4), and
a further study revealed that GBP is not only able to treat T2DM
patients with obesity, but also to prevent the occurrence of
complications (5–7). However, whether GBP exhibits the same
effect in non-obese patients with T2DM remains unclear. Studies
investigating the effects of GBP in non-obese patients with T2DM
are limited. Shah et al observed that GBP safely and
effectively eliminated T2DM in individuals of Asian Indian origin
with a body mass index (BMI) <35 kg/m2 (8); however, the sample size of the study
was only 15 individuals and the follow-up period was only 9 months.
Following the examination of a number of studies published in
English between 1979 and 2009, Fried et al concluded that
there were 343 patients with a mean BMI <35 kg/m2 who
resorted to surgical resolution of T2DM (9). Studies investigating the effects of
GBP in T2DM patients with a BMI <30 kg/m2 are even
more limited.
As a modified GBP procedure, duodenal-jejunal bypass
(DJB) does not change the volume of the stomach or restrict food
intake as it bypasses the duodenum and upper jejunum. With the aid
of Goto-Kakizaki (G-K) rats, Rubino and Marescaux established a
spontaneous non-obese model of T2DM, which demonstrated that DJB
may be used directly in the treatment of T2DM rather than in weight
control or the treatment of obesity (10). However, genetic variations are
possible in the spontaneous G-K rat model of T2DM, and G-K rats
have a characteristic of inadequate β-cell proliferation that is
restricted in the human condition (11). Due to this, and the ability of a
high-fat diet (HFD) to induce insulin resistance (IR) and a low
dose of streptozotocin (STZ) to cause β-cell damage and thereby
induce diabetes mellitus, rats with experimentally induced T2DM
were considered to be an appropriate animal model for use the
present study and have the potential to illustrate the pathogenesis
of human T2DM.
Intensive glycemic control has a protective effect
on the microvascular complications of T2DM whereas its effects on
macrovascular complications are controversial (12–14).
Atherosclerosis is a low-grade subclinical chronic inflammatory
disease; the nuclear factor κB (NF-κB) and c-jun
NH2-terminal kinase (JNK) pathways are two inflammatory
signaling pathways that are involved in the occurrence and
development of atherosclerosis (15–17).
JNK-NF-κB cross communication may play an important role in
determining the focal nature of arterial inflammation and
atherosclerosis (18). However,
studies investigating the protective effect of DJB against
atherosclerosis in the aorta are limited.
Thus, the primary objective of the current study was
to investigate whether DJB was able to induce the remission of T2DM
in non-obese and non-spontaneous diabetic rats. The second
objective was to explore the protective effect of DJB against
ascending aortic atherosclerosis and analyze the changes in the
NF-κB and JNK signaling pathways following DJB surgery in order to
identify the possible mechanisms underlying the protective effect.
To the best of our knowledge, this is the first study to
investigate the protective effect of DJB against atherosclerosis in
the aorta.
Materials and methods
Materials
Streptozotocin (STZ) was purchased from Sigma, (St.
Louis, MO, USA). The insulin (INS) radioimmunoassay kit was
purchased from Beijing North Institute of Biological Technology
(Beijing, China). The serum triglyceride (TG) and total cholesterol
(TC) analysis kits were purchased from Changchun Huili Biological
Technology Co., Ltd. (Changchun, China) and the low density
lipoprotein (LDL) kit was purchased from Shanghai Rongsheng
Biological Pharmaceutical Co., Ltd. (Shanghai, China). The tumor
necrosis factor (TNF)-α enzyme-linked immunosorbent assay (ELISA)
kit was purchased from Shanghai BiovolBiotech (Shanghai, China).
The HFD feed formula contained: 20% fat (50% lard and 50% yolk
powder), 20% sugar and 60% regular chow (GB1492413-2001 contains
the nutrition standards of regular chow).
Experimental animals
Four-week-old male Sprague-Dawley (SD) rats (weight,
80–100 g) were acquired from the Experimental Animal Center of
Chongqing Medical University, [Chongqing, China; animal license No.
SYXK (Chongqing) 2012-0001]. All rats were acclimated to their
environment for one week prior to the beginning of the experiment.
The rats were housed in standard polypropylene cages and maintained
under controlled room temperature (22±2°C) and humidity (55±5%)
with a 12/12 h light/dark cycle. The T2DM model group rats received
a HFD diet for 4 weeks and were subsequently injected
intraperitoneally with low-dose STZ (30 mg/kg) dissolved in citrate
solution (0.1 M citric acid and 0.2 M sodium phosphate, pH
4.2–4.5). The rats that were injected with STZ developed diabetes,
as indicated by the levels of fasting blood glucose (FBG) being
≥7.8 mmol/l twice or the levels of non-fasting blood glucose being
≥11.1 mmol/l twice during the 4 weeks following the injection
(19). The rats with T2DM were
randomly divided into three groups: the sham-surgery group (A; n=6)
that received a sham surgery; the T2DM control group (B; n=6) that
did not undergo surgery and; the DJB group (D; n=6) that underwent
DJB surgery. The SD rats of the matched normal control group (C;
n=6) received a regular chow diet; rats in groups A, B and D were
fed a HFD. The rats were allowed unlimited access to food and
water. INS was not administered to any of the animals. The rats
were fast for 12–14 h, blood samples were collected in the morning
and the levels of FBG, lipids, INS and TNF-α were measured. The
rats were sacrificed 12 weeks following DJB surgery to obtain the
ascending aortic tissue. The current study was conducted in
accordance with the Principles of Laboratory Animal Care (20) for the care and use of experimental
animals, and the procedures were approved by the Animal Care
Committee of Chongqing Medical University.
Establishment of DJB and sham-surgery
models
The rats were fasted for 12–14 h and anesthetized
with 1% sodium pentobarbital (40 mg/kg) via an intraperitoneal
injection. For the rats undergoing DJB, the gastric volume was
maintained intact while the entire duodenum and the proximal
jejunum were bypassed. The stomach was divided from the beginning
of the duodenum. A length of 8 cm from the ligament of Treitz was
measured to locate the site for the gastrojejunal anastomosis,
which was performed using a 6-0 Prolene suture. The continuity of
the biliopancreatic secretions was re-established by anastomosing
the biliary limb to the alimentary limb of small bowel 12 cm
distally to the gastrojejunal anastomosis in a Roux-en-Y fashion
(10,21). For the sham surgery, transections
and reanastomosis of the gastrointestinal tract were performed at
the given sites (corresponding to where enterotomies were performed
for the DJB surgery) and the physiological circuit of food was
maintained through the bowel. When required, the surgery was
prolonged to produce a similar degree of anesthesiological stress
to that of the rats who underwent DJB surgery (10).
Determination of the levels of glucose,
lipids, INS, and TNF-α in the blood
Rats were fasted for 12–14 h and blood was collected
from the tail vein to analyze the levels of FBG with a glucometer
(LifeScan OneTouch®; LifeScan, Milpitas, CA, USA).
Alternatively, blood was collected from the retro-orbital plexus of
the rats under light ether anesthesia using capillary tubes and
transferred into Eppendorf tubes. Two methods of blood are
mentioned because blood collected from the tail vain is limited and
greater amounts of blood are required to separate the serum in
order to detect the TC, TG, LDL, and TNF-α levels. The serum was
separated by centrifuging at 1,000 × g for 15 min, collected and
stored at −80°C. Levels of TC, TG, LDL and TNF-α were measured
using commercially available colorimetric diagnostic kits according
to the manufacturers’ instructions. The serum INS was assayed by
radioimmunoassay according to the manufacturer’s instructions.
Homeostatic model assessment-insulin resistance (HOMA-IR) was
calculated (HOMA-IR =Fasting blood glucose × Fasting insulin /
22.5) to evaluate insulin sensitivity.
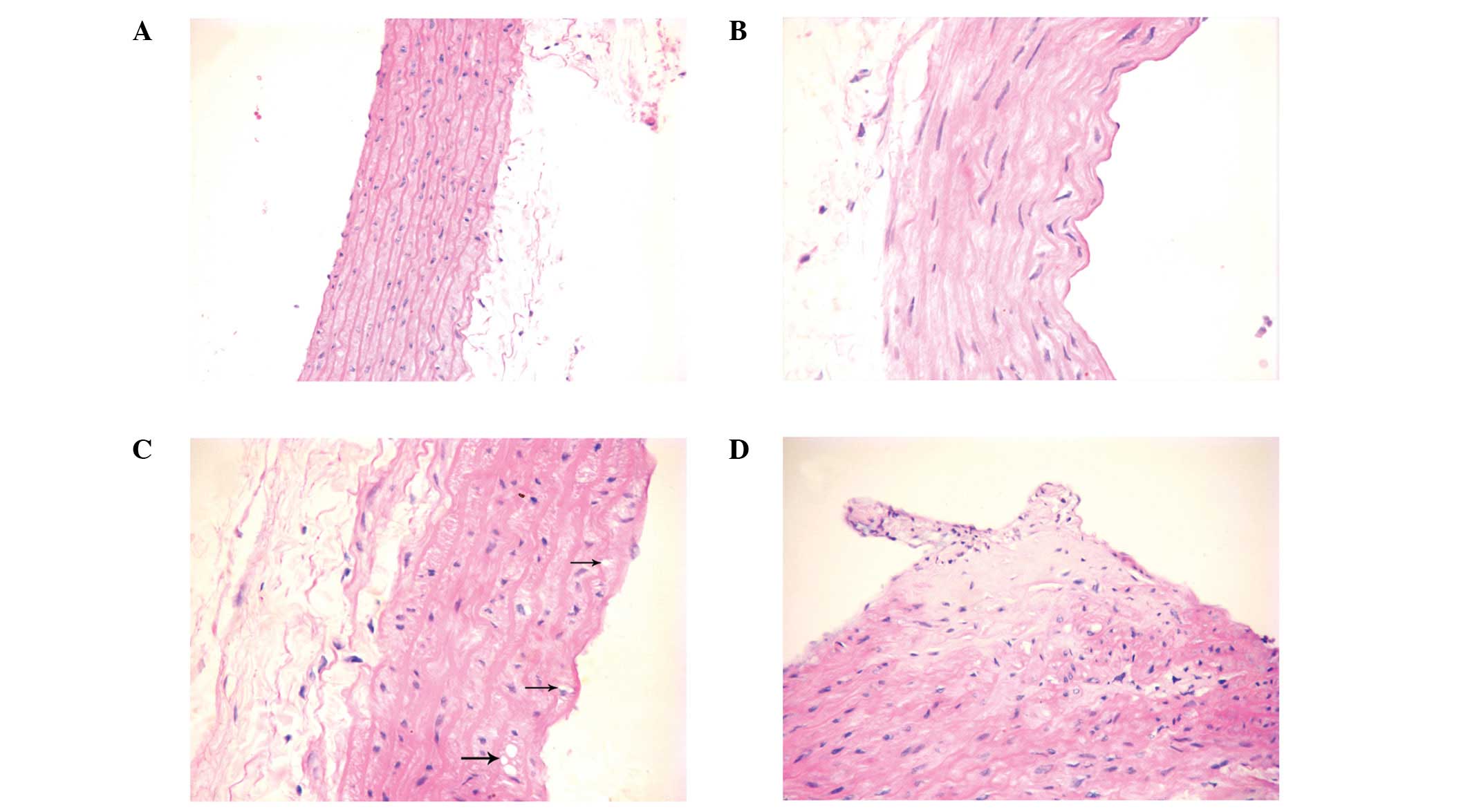
Histological analysis
Formalin-fixed, paraffin-embedded ascending aortic
tissue sections (4 μm) were stained with hematoxylin and eosin for
observation under a light microscope (model cx21, Olympus, Tokyo,
Japan).
Quantitative polymerase chain reaction
(qPCR)
RNA was extracted from the aortic tissue using
RNAiso Plus reagent (Takara Bio, Inc., Shiga, Japan) following the
manufacturer’s instructions. Following DNase treatment, RNA was
reverse transcribed into cDNA using a PrimeScript™ RT
reagent kit with gDNA Eraser (Takara Bio, Inc.). Cycling and qPCR
detection were performed using a CFX96™ Real-Time PCR Detection
system (Bio-Rad, Hercules, CA, USA). The cycling conditions were as
follows: 95°C for 30 sec, followed by 39 cycles at 95°C for 5 sec
and 60°C for 30 sec. The gene-specific primers were designed using
primer analysis software premier version 5.0 (Premier Biosoft, Palo
Alto, CA, USA) and the expression of glyceraldehyde 3-phosphate
dehydrogenase (GAPDH) was used as the internal control for
normalization. The primer pairs used for amplification were: JNK1,
5′-TGGATTTGGAGGAGCGAACTAA-3′ (forward) and
5′-ATTGACAGACGGCGAAGACG-3′ (reverse); inhibitor of κB kinase
(IKKβ), 5′-AGTTTGGCATCACATCGGACA-3′ (forward) and
5′-ACCCATCGGGCTCCTCTGTA-3′ (reverse); and GAPDH,
5′-CCGTATCGGACGCCTGGTTA-3′ (forward) and
5′-CCGTGGGTAGAGTCATACTGGAAC-3′ (reverse). Transcription abundance
was expressed as fold increase over that of the control gene as
calculated by the 2−ΔΔCt method.
Western blot analysis
Aortic tissue was pulverized into powder in liquid
nitrogen and subsequently homogenized in ice-cold modified
radioimmunoprecipitation assay (RIPA) buffer. The protein
concentration was determined using the bicinchoninic acid (BCA)
assay. Equal amounts of protein per lane from each sample were
separated on 10% sodium dodecyl sulfate polyacylamide gels and
transferred onto polyvinylidene fluoride membranes (Millipore,
Billerica, MA, USA). The membranes were incubated with probes
overnight using the following antibodies: anti-IKKβ/p-IKKβ (1:1,000
dilution; Abcam, Cambridge, UK), anti-JNK1/p-JNK1 (1:1,000
dilution; Abcam) and anti-GAPDH (1:1,000 dilution; Proteintech,
Chicago, IL, USA). The immunolabeled membranes were incubated with
goat anti-rabbit immunoglobulin G (IgG) secondary antibodies
(1:1,000 dilution; Proteintech) for 2 h. The bands were visualized
by enhanced chemiluminescence (Millipore) and quantified using
Quantity One software (Bio-Rad, USA).
Statistical analyses
All results are expressed as mean ± standard error
of the mean. Multiple group means were compared by one-way analysis
of variance (ANOVA). P<0.05 was considered to indicate a
statistically significant difference. SPSS software, version 17.0
(SPSS, Inc., Chicago, IL, USA) was used to carry out the
analyses.
Results
General results
For the first week following surgery, the body
weights of the rats in groups A and D declined (data not shown);
however, they exceeded preoperative levels in the second week
(although they remained lower than that of the rats in group C;
P<0.05) and continued to gradually increase. The body weight
increase of the rats in groups A and B was slower than in those of
groups C and D following surgery and this difference was
significant at 12 weeks (P<0.05).
Three days following STZ injection, the levels of
FBG began to increase in the rats with T2DM. The standard for the
FBG levels in diabetic models was reached two weeks following STZ
injection and continued to increase slowly. By contrast, the levels
of FBG in group C rats remained normal (P<0.05).
From the first week following surgery, the levels of
FBG markedly decreased in the rats in group D (data not shown), and
returned to normal between weeks 2 and 12. However, the levels of
FBG in the rats in groups A and B continued to slowly increase
(P<0.05).
In the second week following surgery, the levels of
TC, TG, LDL, INS and TNF-α, and HOMA-IR in the rats in group D were
markedly lower compared with those in the rats in groups A and B
(P<0.05). All levels in group D were restored to normal after 12
weeks, with no difference from those in the rats in group C
(P>0.05). However, all levels in the rats in groups A and B
continued to increase (P<0.05; Table I).
 | Table IGeneral results. |
Table I
General results.
| Characteristics | Group A | Group B | Group C | Group D |
|---|
| Body weight (g) |
| 0 week | 266.50±8.07 | 265.33±8.62 | 264.17±6.40 | 265.83±7.73 |
| 2 week | 274.50±8.26c | 281.00±8.07c | 306.00±5.44 | 279.50±7.81c |
| 12 week | 323.67±9.07c | 325.83±8.16c | 441.50±9.20 | 437.67±9.75a,b |
| FBG (mmol/l) |
| 0 week | 16.27±2.46c | 16.52±2.90c | 4.43±0.64 | 16.8±2.27c |
| 2 week | 17.05±1.64c | 17.03±2.67c | 4.40±0.62 | 5.82±0.25a,b |
| 12 week | 19.58±1.39c | 20.08±1.10c | 4.95±0.34 | 5.13±0.44a,b |
| TG (mmol/l) |
| 0 week | 2.47±0.23c | 2.54±0.25c | 0.95±0.16 | 2.50±0.26c |
| 2 week | 3.12±0.24c | 3.24±0.23c | 0.96±0.13 | 1.69±0.08a–c |
| 12 week | 4.18±0.26c | 4.12±0.28c | 1.19±0.15 | 1.35±0.18a,b |
| TC (mmol/l) |
| 0 week | 6.10±0.21c | 6.13±0.18c | 3.42±0.23 | 6.08±0.17c |
| 2 week | 6.75±0.21c | 6.71±0.28c | 3.58±0.31 | 5.41±0.25a–c |
| 12 week | 8.25±0.29c | 8.28±0.32c | 3.90±0.13 | 4.13±0.38a,b |
| LDL (mmol/l) |
| 0 week | 3.44±0.18c | 3.43±0.24c | 0.86±0.06 | 3.42±0.18c |
| 2 week | 3.72±0.21c | 3.76±0.19c | 0.90±0.11 | 2.47±0.22a–c |
| 12 week | 4.92±0.23c | 4.89±0.29c | 1.10±0.18 | 1.35±0.25a,b |
| INS (μIU/ml) |
| 0 week | 12.03±0.49c | 12.08±0.64c | 7.74±0.44 | 12.21±0.51c |
| 2 week | 14.56±0.89c | 14.42±0.80c | 7.85±0.33 | 12.46±0.70a–c |
| 12 week | 18.75±0.92c | 18.80±1.25c | 7.91±0.19 | 8.22±0.48a,b |
| HOMA-IR |
| 0 week | 8.72±1.56c | 8.88±1.74c | 1.52±0.22 | 9.15±1.36c |
| 2 week | 11.06±1.55c | 10.90±1.69c | 1.53±0.19 | 3.22±0.27a–c |
| 12 week | 16.32±1.41c | 16.79±1.62c | 1.74±0.16 | 1.88±0.26a,b |
| TNF-α (pg/ml) |
| 0 week | 138.83±7.55c | 137.88±9.29c | 84.67±3.94 | 138.19±8.11c |
| 12 week |
174.73±10.57c | 176.33±9.08c | 91.98±4.35 | 100.06±5.87a,b |
Pathological analysis
A total of 12 weeks following surgery, slight
lesions in the ascending aortic tissue appeared in the rats in
group D, including arterial tunica intima thickening and the
broadening of the subendothelial layer (Fig. 1B). Foam cells appeared in four rats
in group A and three rats in group B (Fig. 1C). Atherosclerotic plaques appeared
in two rats in group A and three rats in group B (Fig. 1D). The ascending aortic tissue of
the rats in group C was normal (Fig.
1A).
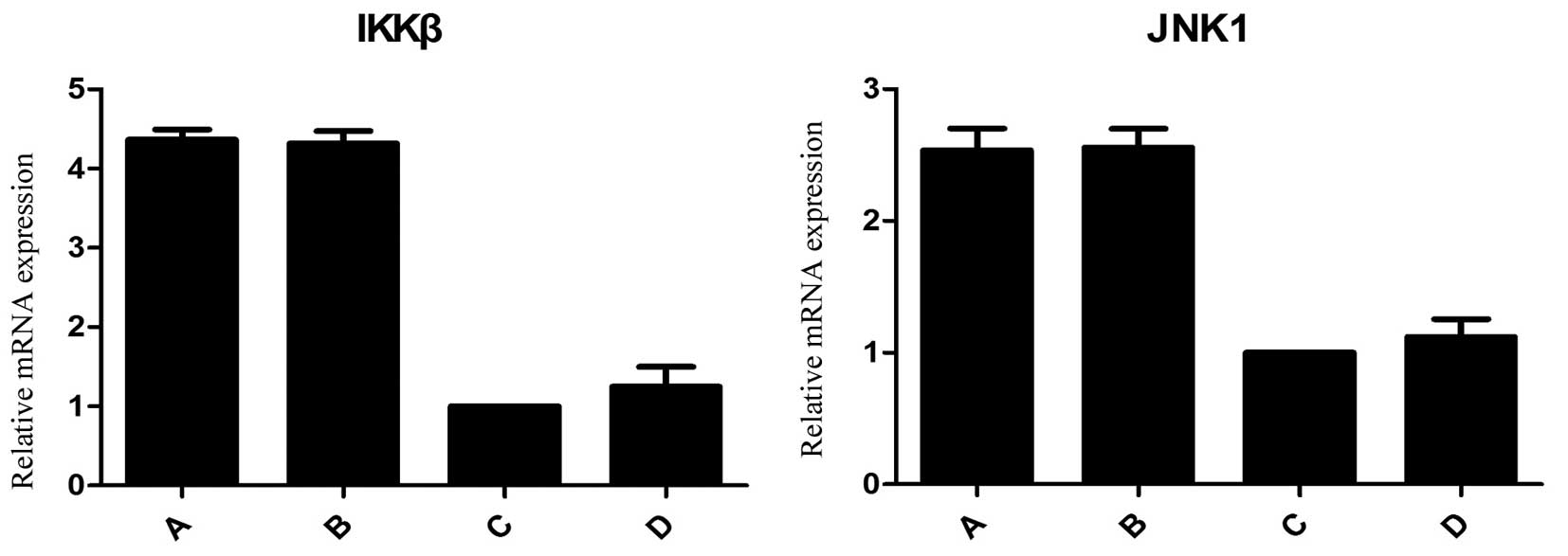
Expression levels of IKKβ and JNK1
mRNA
At 12 weeks following surgery, the mRNA expression
levels of IKKβ and JNK1 in the rats of groups A and B were
significantly higher compared with those in the rats in groups C
and D (P<0.05). No difference was observed in these mRNA levels
between the rats in groups C and D (P>0.05; Fig. 2).
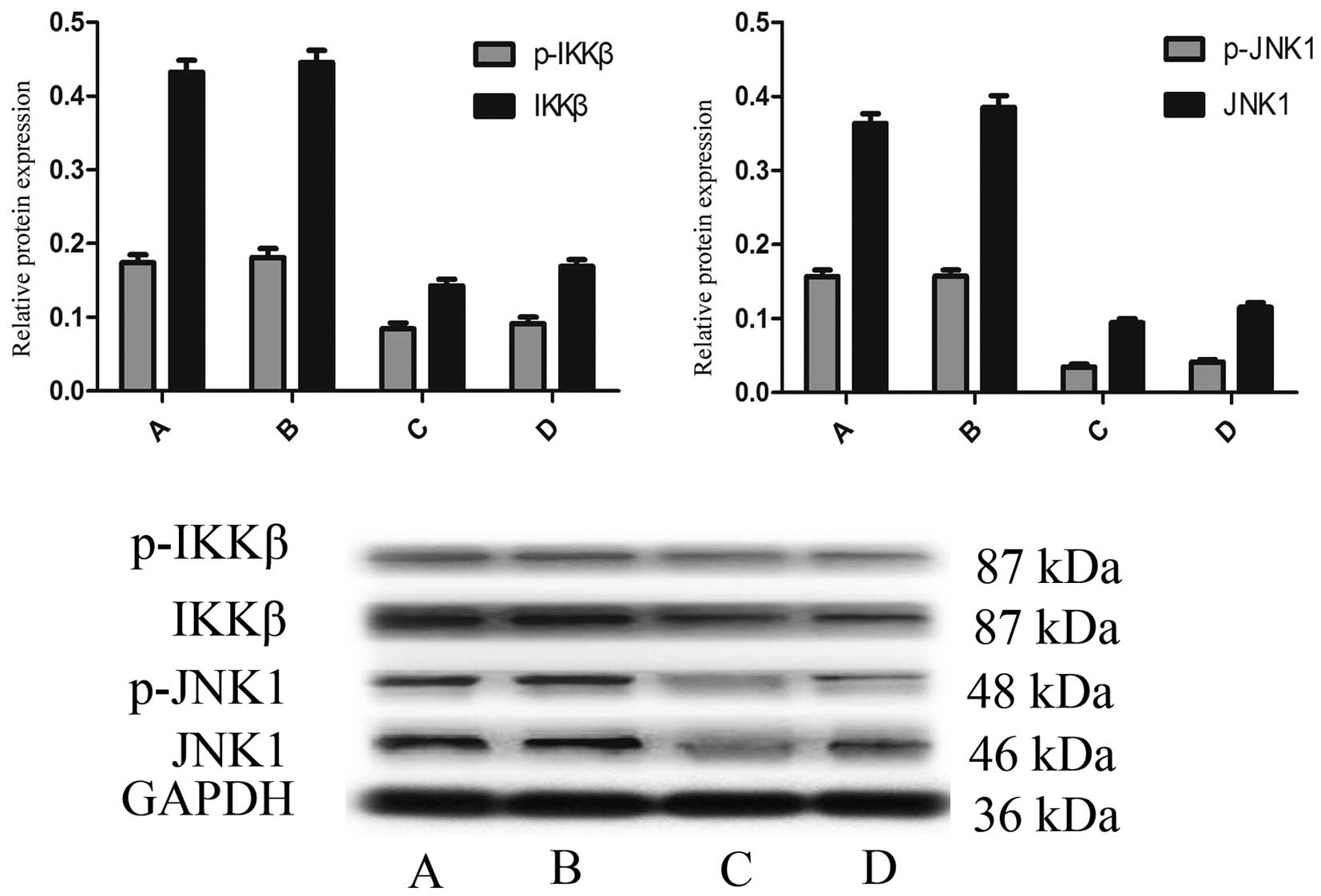
Detection of IKKβ, p-IKKβ, JNK1 and
p-JNK1 proteins
Western blot analysis revealed that the expression
levels of IKKβ, p-IKKβ, JNK1 and p-JNK1 proteins were significantly
increased in the rats in groups A and B 12 weeks following surgery,
whereas they were only slightly increased in the rats in group D
(P<0.05), which was consistent with the qPCR results. No
statistically significant difference was identified in the levels
of these proteins between the rats in groups C and D (P>0.05;
Fig. 3).
Discussion
GBP may primarily contribute to the reduction of
blood glucose levels in patients with T2DM rather than the control
of weight (22–24). In severely obese patients with
T2DM, GBP surgery has been shown to result in improved glucose
control compared with that achieved by medical therapy (25). In a study of obese patients with
uncontrolled T2DM, a significantly greater proportion of patients
achieved glycemic control through 12-month medical therapy and
bariatric surgery compared with medical therapy alone (26). Whether GBP has the same effect on
non-obese patients remains unclear. In the present study, the T2DM
model rats were non-obese and their FBG levels decreased
significantly one week following DJB. As the trauma of surgery
affected the rats’ food intake, their body weight slightly declined
in the first week. However, two weeks following surgery, the body
weights of the rats were restored and even exceeded preoperative
levels, and the FBG levels became normal. A total of 12 weeks
following surgery, the FBG levels in the DJB-group rats were
normal, although their body weights exceeded those of the rats in
the sham-surgery and T2DM groups, whose FBG levels continued to
increase. The slow increase in body weight in the rats of the
sham-surgery and T2DM groups was affected by diabetes. Therefore,
it may be concluded that DJB is able to directly control the blood
glucose levels of non-obese patients with T2DM without dependence
on weight control.
Two weeks following DJB surgery, the levels of FBG
in the rats in the DJB group returned to normal; however, the
levels of INS remained higher compared with those in the rats in
the normal control group, which indicated a significant improvement
in IR. This result corresponded with observations made by Pournaras
et al in patients with T2DM (27), whose study concluded that the
increase in INS secretion may be caused by an enhanced
glucagon-like peptide 1 (GLP-1) reaction.
Roux-en-Y GBP and biliopancreatic diversion (BPD)
are the two most widely used methods of GBP surgery used to treat
obesity and T2DM simultaneously in obese patients with T2DM
(28–30). As weight loss is not essential in
non-obese patients with T2DM, treating T2DM is the direct
objective. DJB does not change the volume of the stomach, as it
bypasses the duodenum and upper jejunum, and thus it does not
restrict food intake. Therefore, in the present study, DJB was
adopted in non-obese rats with T2DM in order to investigate whether
it was able to induce the remission of T2DM. The results of the
current study were consistent with those of Rubino and Marescaux in
G-K rats (10), which also
demonstrated that the duodenum and upper jejunum may play an
important role in the pathogenesis and treatment of T2DM.
JNK may be induced by the endoplasmic reticulum
stress triggered by excessive nutrients to cause an inflammatory
effect (31). As inflammatory
processes play a pivotal role in the pathogenesis of
atherosclerosis, anti-inflammatory therapy is expected to become
one of the most promising strategies in the treatment of
atherosclerosis (32). Further
studies have revealed that atherosclerotic processes may be
suppressed through the inhibition of the JNK and NF-κB signaling
pathways in macrophages and aortic smooth muscle cells (33,34).
In the current study, the fact that glucose homeostasis, lipid
metabolism and inflammation were improved over time in group D
following DJB surgery indicated that the inflammatory effect was
decreased. Furthermore, the expression levels of IKKβ and JNK1 mRNA
in the aortas of the group D rats were lower compared with those in
the rats in groups A and B. Western blotting results revealed that
the expression levels of the IKKβ, p-IKKβ, JNK1 and p-JNK1 proteins
in the rats in groups A and B significantly increased, while they
remained low in the rats in group D with no significant difference
from those in the rats in group C. This may be due to the NF-κB and
JNK1 inflammatory signaling pathways being activated in groups A
and B, but inhibited in group D. Foam cells and atherosclerotic
plaques were observed in the aortas of the rats in groups A and B
16 weeks following STZ injection, while only slight lesions
appeared in the rats in group D. This indicated that DJB surgery
may protect the aorta from atherosclerosis.
In conclusion, DJB was able to induce the remission
of T2DM in non-obese rats without weight loss. Furthermore, it
delayed or prevented the occurrence and development of
atherosclerosis in the aortas of non-obese rats with T2DM. This
protective effect was possibly achieved through modulation of the
NF-κB and JNK1 signaling pathways.
There were several limitations of the present study.
Firstly, the long-term effects of DJB remain unknown as the
observation time was limited to 12 weeks. Previous studies have
revealed that certain patients with T2DM relapse over a longer
follow-up period subsequent to DJB (35,36).
Larger, long-term studies are required to confirm the results, and
investigation of the cause of relapse may facilitate understanding
of the underlying mechanisms and improve the treatment of T2DM.
Acknowledgements
Dr Chen received funding from the Chongqing
Municipal Health Bureau (No. 2012-2-435).
References
|
1
|
Shinde J, Tadldone T, Barletta M, et al:
Alpha-glucosidase inhibitory activity of Syzygium cumini (Linn.)
Skeels seed kernel in vitro and in Goto-Kakizaki (GK) rats.
Carbohydr Res. 343:1278–1281. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Foley EF, Benotti PN, Borlase BC,
Hollingshead J and Blackburn GL: Impact of gastric restrictive
surgery on hypertension in the morbidly obese. Am J Surg.
163:294–297. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Pories WJ, Swanson MS, MacDonald KG, et
al: Who would have thought it? An operation proves to be the most
effective therapy for adult-onset diabetes mellitus. Ann Surg.
222:339–350. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Smith SC, Edwards CB and Goodman GN:
Changes in diabetic management after Roux-en-Y gastric bypass. Obes
Surg. 6:345–348. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Adams TD, Gress RE, Smith SC, et al:
Long-term mortality after gastric bypass surgery. N Engl J Med.
357:753–761. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Batsis JA, Sarr MG, Collazo-Clavell ML, et
al: Cardiovascular risk after bariatric surgery for obesity. Am J
Cardiol. 102:930–937. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Christou NV, Lieberman M, Sampalis F and
Sampalis JS: Bariatric surgery reduces cancer risk in morbidly
obese patients. Surg Obes Relat Dis. 4:691–695. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shah SS, Todkar JS, Shah PS and Cummings
DE: Diabetes remission and reduced cardiovascular risk after
gastric bypass in Asian Indians with body mass index <35
kg/m2. Surg Obes Relat Dis. 6:332–338. 2010. View Article : Google Scholar
|
|
9
|
Fried M, Ribaric G, Buchwald JN, et al:
Metabolic surgery for the treatment of type 2 diabetes in patients
with BMI <35 kg/m2: an integrative review of early
studies. Obes Surg. 20:776–790. 2010. View Article : Google Scholar
|
|
10
|
Rubino F and Marescaux J: Effect of
duodenal-jejunal exclusion in a non-obese animal model of type 2
diabetes: a new perspective for an old disease. Ann Surg. 239:1–11.
2004. View Article : Google Scholar
|
|
11
|
Cefalu WT: Animal models of type 2
diabetes: clinical presentation and pathophysiological relevance to
the human condition. ILAR J. 47:186–198. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
ADVANCE Collaborative Group. Patel A,
MacMahon S, Chalmers J, et al: Intensive blood glucose control and
vascular outcomes in patients with type 2 diabetes. N Engl J Med.
358:2560–2572. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Duckworth W, Abraira C, Moritz T, et al:
Glucose control and vascular complications in veterans with type 2
diabetes. N Engl J Med. 360:129–139. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Athyros VG, Tziomalos K, Karagiannis A and
Mikhailidis DP: Preventing macrovascular complications of diabetes:
where do we stand with glycemic control? Expert Opin Investig
Drugs. 17:1777–1779. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kyriakis JM and Avruch J: Mammalian MAPK
signal transduction pathways activated by stress and inflammation:
a 10-year update. Physiol Rev. 92:689–737. 2012.PubMed/NCBI
|
|
16
|
Pamukcu B, Lip GY and Shantsila E: The
nuclear factor - kappa B pathway in atherosclerosis: a potential
therapeutic target for atherothrombotic vascular disease. Thromb
Res. 128:117–123. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Madonna R and De Caterina R: Relevance of
new drug discovery to reduce NF-κB activation in cardiovascular
disease. Vascul Pharmacol. 57:41–47. 2012.PubMed/NCBI
|
|
18
|
Cuhlmann S, Van der Heiden KV, Saliba D,
et al: Disturbed blood flow induces RelA expression via c-Jun
N-terminal kinase 1: a novel mode of NF-κB regulation that promotes
arterial inflammation. Circ Res. 108:950–959. 2011.PubMed/NCBI
|
|
19
|
Zhang M, Lv XY, Li J, Xu ZG and Chen L:
The characterization of high-fat diet and multiple low-dose
streptozotocin induced type 2 diabetes rat model. Exp Diabetes Res.
2008:7040452008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
National Institutes of Health. Guide for
the Care and Use of Laboratory Animals. National Institutes of
Health publication. no. 85-23, revised in 1985.
|
|
21
|
Rubino F, Forgione A, Cummings DE, et al:
The mechanism of diabetes control after gastrointestinal bypass
surgery reveals a role of the proximal small intestine in the
pathophysiology of type 2 diabetes. Ann Surg. 244:741–749. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Laferrère B, Teixeira J, McGinty J, et al:
Effect of weight loss by gastric bypass surgery versus hypocaloric
diet on glucose and incretin levels in patients with type 2
diabetes. J Clin Endocrinol Metab. 93:2479–2485. 2008.PubMed/NCBI
|
|
23
|
Cohen RV, Schiavon CA, Pinheiro JS, Correa
JL and Rubino F: Duodenal-jejunal bypass for the treatment of type
2 diabetes in patients with body mass index of 22–34
kg/m2: a report of 2 cases. Surg Obes Relat Dis.
3:195–197. 2007.
|
|
24
|
Gumbs AA, Modlin IM and Ballantyne GH:
Changes in insulin resistance following bariatric surgery: role of
caloric restriction and weight loss. Obes Surg. 15:462–473. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mingrone G, Panunzi S, De Gaetano AD, et
al: Bariatric surgery versus conventional medical therapy for type
2 diabetes. N Engl J Med. 366:1577–1585. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Schauer PR, Kashyap SR, Wolski K, et al:
Bariatric surgery versus intensive medical therapy in obese
patients with diabetes. N Engl J Med. 366:1567–1576. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Pournaras DJ, Osborne A, Hawkins SC, et
al: Remission of type 2 diabetes after gastric bypass and banding:
mechanisms and 2 year outcomes. Ann Surg. 252:966–971.
2010.PubMed/NCBI
|
|
28
|
Rubino F and Gagner M: Potential of
surgery for curing type 2 diabetes mellitus. Ann Surg. 236:554–559.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Buchwald H and Williams SE: Bariatric
surgery worldwide 2003. Obes Surg. 14:1157–1164. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Scopinaro N, Marinari GM, Camerini GB,
Papadia FS and Adami GF: Specfic effects of biliopancreatic
diversion on the major components of metabolic syndrome:a long-term
follow-up study. Diabetes Care. 28:2406–2411. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kaneto H, Matsuoka TA, Katakami N, et al:
Oxidative stress and the JNK pathway are involved in the
development of type 1 and type 2 diabetes. Curr Mol Med. 7:674–686.
2007. View Article : Google Scholar
|
|
32
|
Li JJ and Fang CH: C-reactive protein is
not only an inflammatory marker but also a direct cause of
cardiovascular diseases. Med Hypotheses. 62:499–506. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lou Y, Liu S, Zhang C, et al: Enhanced
atherosclerosis in TIPE2-deficient mice is associated with
increased macrophage responses to oxidized low-density lipoprotein.
J Immunol. 191:4849–4857. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Lee YJ, Kim JS, Kang DG and Lee HS:
Buddleja officinalis suppresses high glucose-induced
vascular smooth muscle cell proliferation: role of
mitogen-activated protein kinases, nuclear factor-kappaB and matrix
metalloproteinases. Exp Biol Med (Maywood). 235:247–255. 2010.
View Article : Google Scholar
|
|
35
|
DiGiorgi M, Rosen DJ, Choi JJ, et al:
Re-emergence of diabetes after gastric bypass in patients with mid-
to long-term follow-up. Surg Obes Relat Dis. 6:249–253. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Arterburn DE, Bogart A, Sherwood NE, et
al: A multisite study of long-term remission and relapse of type 2
diabetes mellitus following gastric bypass. Obes Surg. 23:93–102.
2013. View Article : Google Scholar
|