Introduction
Acute hepatic failure (AHF), a clinical syndrome
caused by multiple factors, is characterized by severe liver cell
damage. In patients with AHF, the functions of synthesis,
metabolism, transport and excretion in the liver are severely
impaired, ultimately leading to multiple organ failure and
mortality. Due to its complex clinical symptoms and high mortality
rate, the treatment of AHF is challenging for the medical community
(1,2). In addition to orthotopic liver
transplantation (OLT), stem cell transplantation has become an
effective means for the treatment of liver failure in recent years
(3–6).
The pathogenesis of AHF is associated with the
immune response and inflammatory reactions in the body. Previous
studies have revealed that macrophage activation and the secretion
of multiple cytokines plays an important role in the pathogenesis
of AHF (7,8). Hepatic apoptosis and necrosis
mediated by inflammatory cytokines are important factors in the
development of AHF (9,10). Furthermore, the inflammatory
response in the body may be regulated by anti-inflammatory factors.
Cluster of differentiation (CD)163 and interleukin (IL)-10 play
important roles in anti-inflammatory reactions. CD163 is
specifically expressed on the membranes of monocyte and macrophage
cells. Its anti-inflammatory and anti-oxidative effects play a
critical role in the occurrence and development of liver failure
(11,12). IL-10 upregulates the expression of
CD163 in monocytes and reduces the inflammatory response of hepatic
cells and the adhesion of neutrophils to sinusoidal endothelial
cells, thereby alleviating liver damage (13–15).
Parekkadan et al (16)
demonstrated that cytokines derived from bone marrow mesenchymal
stem cells (BMSCs) may prevent the necrosis of hepatic cells and
improve the survival rate of patients with fulminant hepatic
failure. Kuo et al (17)
induced lethal fulminant hepatic failure in non-obese diabetic
severe combined immunodeficient mice with CCl4.
Mesenchymal stem cell-derived hepatocytes and BMSCs were
intrasplenically or intravenously transplanted at different doses.
The study revealed that BMSC transplantation was able to
effectively prevent experimental liver failure.
In the present study, an AHF model was established
in rats. The therapeutic effect of BMSC transplantation on AHF was
investigated. Liver function was assessed by detecting the levels
of alanine aminotransferase (ALT), aspartate aminotransferase
(AST), albumin (ALB), direct bilirubin (DBIL) and indirect
bilirubin (IBIL) in the serum. Pathological liver damage was
revealed by hematoxylin and eosin (H&E) staining. The dynamic
changes in the levels of CD163 and IL-10 in the serum and liver
tissue were also measured. Furthermore, the cell apoptosis rate in
the liver was observed by terminal deoxynucleotidyl transferase
dUTP nick end labeling (TUNEL) staining.
Materials and methods
Animals
Sprague-Dawley (SD) rats [healthy males; weighing
~250–300 g; specific pathogen-free (SPF)-class] were provided by
the Animal Center of the Centers for Disease Control in Xinjiang
(License no. SCXK Xin 2003-0002). The rats were kept under standard
conditions. All animal experiments were performed with the approval
of the Medical Ethics Committee of Xinjiang Medical University
(Urumqi, China).
Separation, culture and identification of
rat BMSCs
BMSCs were isolated from the bone marrow of SD rats.
Briefly, 50,000 units heparin was injected intraperitoneally into
each rat. Following injection for 15 min, the rats were sacrificed
and whole bone marrow was collected from the bilateral tibia. Cells
from the whole bone marrow were seeded in a 75-cm2 Petri
dish at a concentration of 1×109 cells/l. Following
incubation for 7–10 days, colonies were established. Cells from the
colonies were collected and plated into dishes. After achieving
70–80% confluence, adherent cells were trypsinized using 0.25%
(w/v) trypsin/ethylenediaminetetraacetic acid (EDTA; Invitrogen
Life Technologies, Carlsbad, CA, USA) and replated at a dilution of
1:3. At the third passage, BMSCs were identified and cultured for
future experiments.
BMSCs were identified by flow cytometric analysis
(Gallios Flow Cytometer, Beckman Coulter Inc., Brea, CA, USA).
Briefly, the cells were collected, washed with phosphate-buffered
saline (PBS) and resuspended at a concentration of
1×109/l. The single cell suspension was incubated with
fluorescein isothiocyanate (FITC)-labeled mouse anti-CD45, CD29,
CD11 and CD90 antibodies (BioLegend, Inc., San Diego, CA, USA).
Following incubation at room temperature for 15 min, the cells were
washed twice with PBS and analyzed by flow cytometry.
Animal model and BMSC
transplantation
The model of AHF was induced by the intraperitoneal
injection of 10% D-galactosamine (1.4 g/kg, administered twice in
12 h) and 0.005% lipopolysaccharide (LPS; 20 μg/kg, administered
once in 12 h)(both from Sigma, St. Louis, MO, USA). Following model
establishment, the rats were fasted for another 12 h prior to BMSC
transplantation.
Isolated BMSCs were transplanted through portal and
tail vein injection. A total of 12 SD rats without any prior
treatment were used as the normal group. A total of 48 SD rats were
used for the animal model establishment. These were randomly
divided into the control group with liver failure (n=16), the tail
vein transplantation group (n=16) and the portal vein
transplantation group (n=16). For the control group, rats were
administered the same volume of saline by intraperitoneal
injection. For the tail vein group, rats were injected with BMSCs
(1.4×107 cells/kg) through the tail vein. For the portal
vein group, the rats were anaesthetized and the abdominal cavity
was exposed. BMSCs (1.4×107 cells/kg) were injected
through the portal vein. At 24, 120 and 168 h following
transplantation, blood samples and liver tissue were collected from
the rats for further analysis. Liver tissues were fixed with 4%
paraformaldehyde.
Serum analysis
Blood samples were centrifuged and the serum was
isolated. The levels of ALT, AST ALB, DBIL and IBIL in the serum
were measured using an automatic biochemical analyzer (UniCel DxC
800; Beckman Coulter, Miami, FL, USA). The levels of CD163 and
IL-10 were detected using an enzyme-linked immunosorbent assay
(ELISA) according to the manufacturers’ instructions. The
anti-CD163 antibody was purchased from the Shanghai Westang
Bio-Tech, Co. Ltd Co., Ltd. (Shanghai, China), and the anti-IL-10
antibody was purchased from eBioscience, Inc. (San Diego, CA,
USA).
H&E staining
Liver tissues were embedded in paraffin, cut into
4-μm sections and stained with H&E. For pathological
observation under a light microscope (Olympus BX50, Olympus, Tokyo,
Japan), five views at low magnification (x200) and five views at
high magnification (x400) were randomly selected from each
slide.
TUNEL assay
The cell apoptosis rate in the liver was detected by
a TUNEL assay kit (Roche Applied Science, Rotkreuz, Switzerland).
Briefly, paraffin sections were dewaxed, hydrated and rinsed with
PBS. Subsequently, H2O2 in methanol (3 ml/l)
solution was added to block endogenous peroxidase activity. The
liver sections were permeabilized by adding permeabilization
solution (1 g/l Triton X-100 dissolved in 0.1% sodium citrate).
Following permeabilization, the TUNEL reaction buffer and
Converter-POD were added. Finally, the liver sections were
incubated with 3,3′-diaminobenzidine (DAB) for chromogenic
reaction. Sections were counter-stained with hematoxylin to
identify the background TUNEL-negative cells. Hepatic apoptosis was
observed under a microscope (Olympus BX50, Olympus). For the
negative control, phosphate buffer instead of the primary antibody
was added. The apoptotic cells were characterized by brown
particles confined within the nucleus. Five fields at high
magnification (x400) were randomly selected from each slice. The
percentage of apoptotic cells was calculated as the ratio of the
TUNEL positive cell number to the total liver cell number per
field.
Western blot analysis
Protein samples were extracted from the liver tissue
and separated with 10% polyacrylamide gel electrophoresis. The
proteins were transferred onto membranes. Following blocking, the
membranes were incubated with antibodies. The primary antibodies
were mouse anti-CD163 (1:200; sc-58965; Santa Cruz Biotechnology,
Inc., Santa Cruz, CA, USA), mouse anti-IL-10 (1:250; ab25073;
Abcam, Cambridge, MA, USA) and glyceraldehyde 3-phosphate
dehydrogenase (GAPDH; 1:1,000; sc-25778; Santa Cruz Biotechnology).
The secondary antibody was goat anti-mouse immunoglobulin G (IgG;
Thermo Scientific, Pierce Biotechnology, Inc., Rockford, IL, USA).
Finally, the membranes were developed using enhanced
chemiluminescence (ECL; Amersham Pharmacia Biotech, Piscataway, NJ,
USA). The gray value was measured using Quantity One software
(Bio-Rad, Hercules, CA, USA). The gray value of GAPDH was used as
an internal control.
Statistical analysis
Data were analyzed using SPSS software, version 18.0
(SPSS, Inc., Chicago, IL, USA). Data are expressed as mean ±
standard deviation. Differences between the groups were compared
using randomized block analysis of variance (ANOVA). Differences
between measurements were analyzed using ANOVA following rank
conversion. Correlation analysis was conducted using Spearman’s
correlation analysis. P<0.05 was considered to indicate a
statistically significant difference.
Results
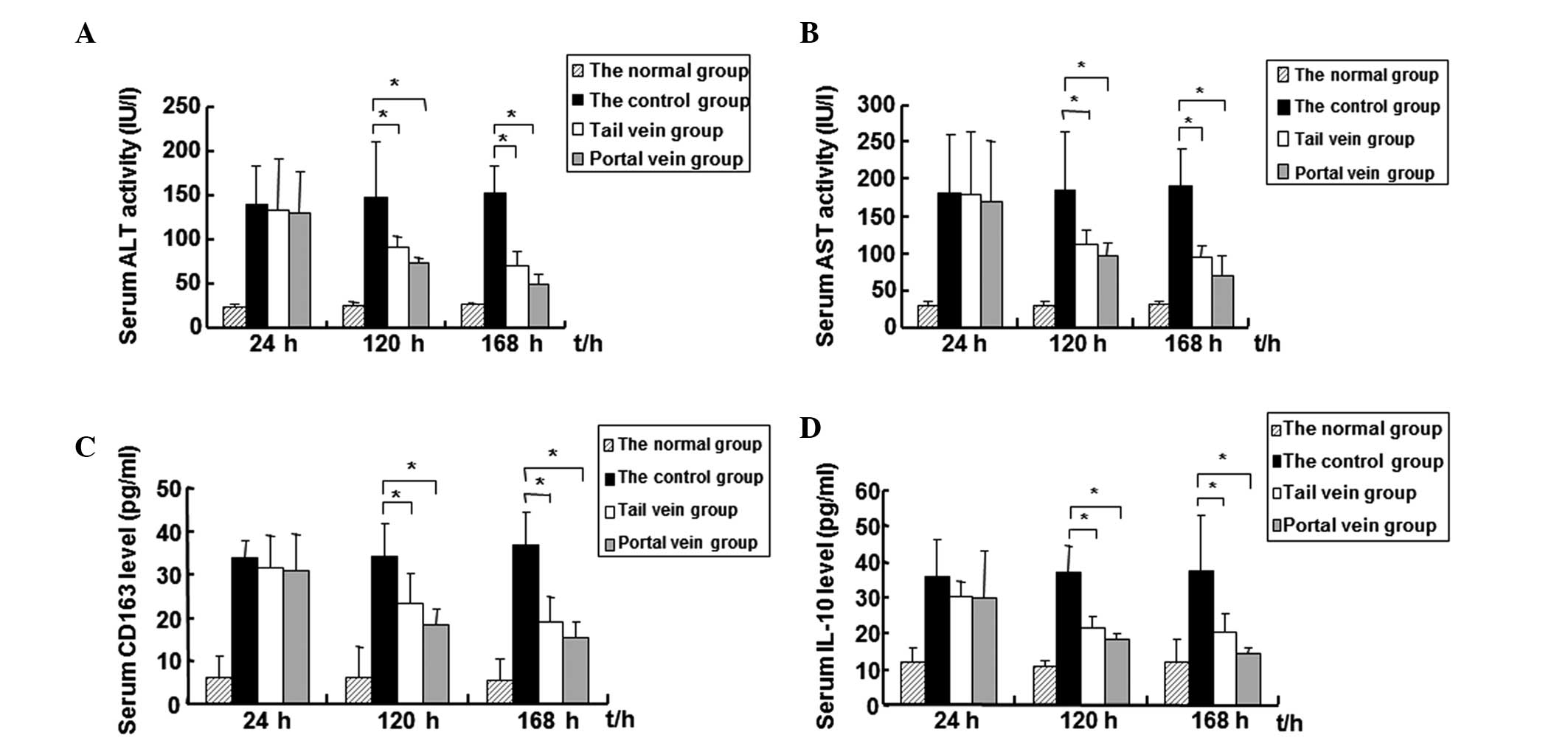
Levels of ALT, AST, DBIL, IBIL, CD163 and
IL-10 in the serum decrease while the level of ALB increases
following BMSC transplantation
Levels of ALT, AST, ALB, DBIL and IBIL in the serum
are biomarkers of liver injury and reflect liver function to a
certain extent. To evaluate liver function following BMSC
transplantation, the blood samples of rats were collected at 24,
120 and 168 h following transplantation. The levels of ALT, AST,
ALB, DBIL and IBIL in the serum were measured using an automatic
biochemical analyzer. The results are shown in Fig. 1A and B, and Tables I–III. As shown in Fig. 1A and B, the levels of ALT and AST
in the tail and portal vein groups gradually decreased over the
treatment time period. At 168 h (1 week) following transplantation,
the ALT and AST levels had decreased to their lowest level. The
levels of ALT and AST in the AHF control group remained at a high
level throughout the experimental period. Statistically, there were
no significant differences in the levels of ALT and AST among the
three groups at 24 h following BMSC transplantation. At 120 and 168
h following transplantation, the levels of ALT and AST in the tail
and portal vein groups were significantly lower compared with those
in the control group (P<0.05). Notably, the levels of ALT and
AST in the portal vein group were slightly lower than those in the
tail vein group at the three time points; however, the differences
between the two groups were not statistically significant.
Similarly, compared with the levels in the control group, the serum
levels of DBIL and IBIL in the tail and portal vein groups were
significantly decreased at 120 and 168 h (P<0.05; Table II). However, the tail and portal
vein groups had significantly higher levels of ALB at 168 h
compared with the control group (P<0.05; Table III). Furthermore, the differences
in the serum levels of DBIL, IBIL and ALB were not significant
between the tail and portal vein groups. These results suggest that
liver injury was reduced and liver function was improved following
BMSC transplantation.
 | Table ISerum levels of ALT and AST in each
group at the three time points (IU/l). |
Table I
Serum levels of ALT and AST in each
group at the three time points (IU/l).
| 24 h | 120 h | 168 h |
|---|
|
|
|
|
|---|
| Groups | ALT | AST | ALT | AST | ALT | AST |
|---|
| Normal | 24.00±3.74 | 29.50±6.35 | 26.50±3.87 | 30.75±4.29 | 27.00±2.45 | 32.50±4.20 |
| Control | 140.20±44.42 | 182.00±79.78 | 152.00±72.60 | 188.00±90.24 | 155.40±34.81 | 193.20±55.54 |
| Tail vein | 134.60±58.08 | 179.20±86.68 | 95.33±12.19a | 113.33±18.71a | 71.50±16.36a | 95.67±13.84a |
| Portal vein | 131.00±54.47 | 173.50±93.10 | 76.50±7.29a | 99.17±14.28a | 49.33±13.50a | 71.50±24.56a |
 | Table IIISerum levels of ALB in each group at
the three time points (IU/l). |
Table III
Serum levels of ALB in each group at
the three time points (IU/l).
| Groups | 24 h | 120 h | 168 h |
|---|
| Normal | 40.00±3.92 | 39.5±2.89 | 42.75±6.95 |
| Control | 24.78±1.77 | 23.86±1.69 | 21.63±4.62 |
| Tail vein | 23.80±3.18 | 24.82±4.08 | 25.87±3.52a |
| Portal vein | 25.04±2.70 | 25.66±2.59 | 25.97±4.68a |
 | Table IISerum levels of DBIL and TBIL in each
group at the three time points (IU/l). |
Table II
Serum levels of DBIL and TBIL in each
group at the three time points (IU/l).
| 24 h | 120 h | 168 h |
|---|
|
|
|
|
|---|
| Groups | DBIL | IBIL | DBIL | IBIL | DBIL | IBIL |
|---|
| Normal | 1.78±0.40 | 1.9±0.50 | 3.15±1.57 | 2.38±1.03 | 1.92±1.07 | 3.38±1.48 |
| Control | 12.08±5.90 | 13.4±2.60 | 30.46±9.54 | 29.64±8.97 | 30.83±4.98 | 24.68±6.57 |
| Tail vein | 10.92±5.21 | 10.38±7.44 | 6.82±1.15a | 7.02±1.84a | 5.73±4.35a | 5.57±2.28a |
| Portal vein | 10.94±5.01 | 7.00±3.93 | 7.12±2.83a | 4.98±2.69a | 6.08±4.35a | 4.07±2.00a |
Changes in the levels of the inflammatory factors
(CD163 and IL-10) in the serum were also detected by an ELISA
assay. In the control group, the AHF model rats did not undergo
stem cell transplantation. Results are shown in Fig. 1C and D, and Table IV. As shown in Fig. 1C and D, the serum levels of CD163
and IL-10 in the control group increased over time, indicating a
deterioration in liver function. At 24 h following BMSC
transplantation, the levels of CD163 and IL-10 in the tail and
portal vein groups were not observed to be significantly different
when compared with the control group. However, at 120 and 168 h
following BMSC transplantation, the levels of CD163 and IL-10 in
the tail and portal vein groups gradually decreased and were
significantly lower than those in the control group (P<0.01).
Similarly, the levels of CD163 and IL-10 in the portal vein group
were lower than those in the tail vein group. However, these
differences were not found to be statistically significant.
 | Table IVSerum levels of CDl63 and IL-10 in
each group at the three time points (pg/ml). |
Table IV
Serum levels of CDl63 and IL-10 in
each group at the three time points (pg/ml).
| 24 h | 120 h | 168 h |
|---|
|
|
|
|
|---|
| Groups | CDl63 | IL-10 | CDl63 | IL-10 | CDl63 | IL-10 |
|---|
| Normal | 6.00±5.38 | 11.81±4.65 | 6.17±7.09 | 11.06±1.36 | 5.66±4.95 | 11.90±6.69 |
| Control | 32.49±4.73 | 31.10±9.66 | 34.28±7.30 | 35.23±9.60 | 37.04±7.50 | 37.52±15.67 |
| Tail vein | 32.04±7.04 | 30.39±4.37 | 23.80±6.85a | 23.72±5.28a | 15.47±8.81a | 20.74±5.00a |
| Portal vein | 31.32±8.27 | 30.20±13.21 | 14.73±5.83a | 19.01±2.04a | 9.43±6.08a | 13.20±2.59a |
A correlation analysis was carried out between the
levels of CDl63 and IL-10 and the levels of ALT and AST at 168 h.
Significant correlations were identified between CD163 and ALT
(r=0.460, P=0.048) and AST (r=0.492, P=0.033). There were also
significant correlations between IL-10 and ALT (r=0.530, P=0.02)
and AST (r=0.618, P=0.005). Furthermore, the levels of CD163 were
positively correlated with the levels of IL-10 (r=0.733,
P=0.001).
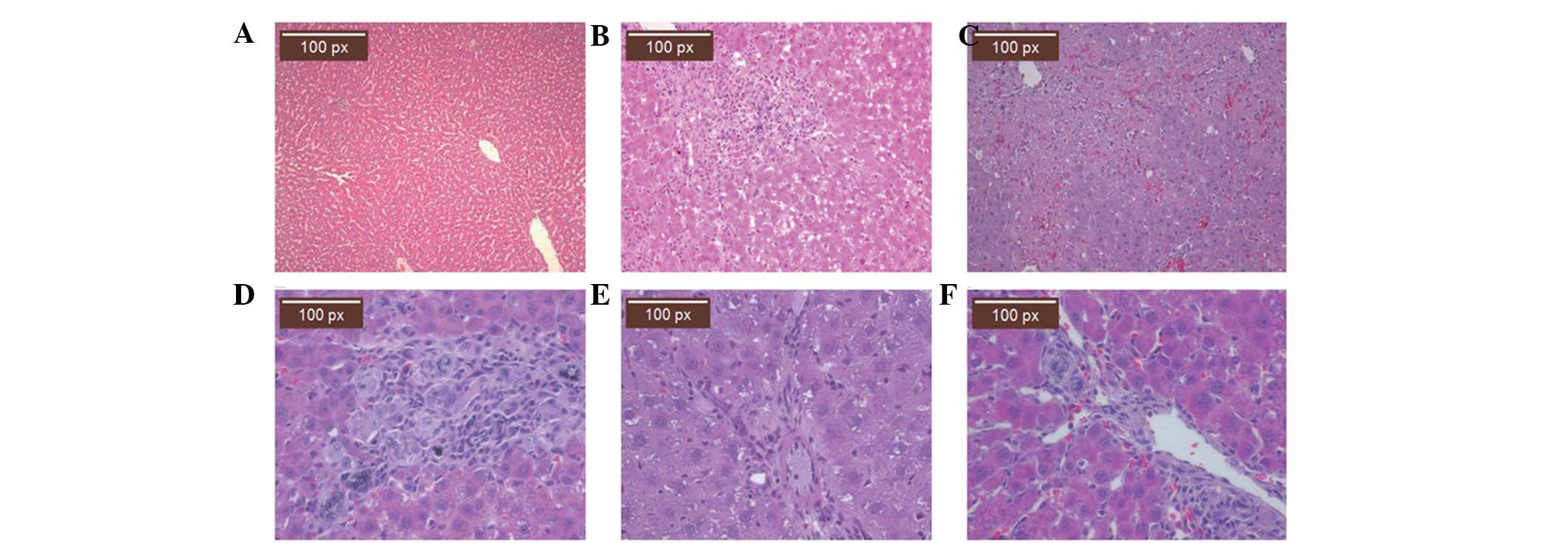
BMSC transplantation alleviates the
pathological features of liver damage in an AHF rat model
To observe the pathological features following BMSC
transplantation, liver tissue was collected and stained with
H&E. Fig. 2A shows the
histological features of healthy rat liver tissue. In the normal
liver tissue, the structure of the hepatic lobule was intact.
Hepatocytes of similar cellular sizes were arranged in cords within
the hepatic lobule. These cords radiated outwards from the central
veins. The pathological features of the liver tissue from rats with
AHF are shown in Fig. 2B and C. In
Fig. 2B, the pathological features
of the liver tissue at 24 h following the injection of
D-galactosamine in the control group are shown. The hepatic lobule
had lost its normal structure and the hepatocytes were swollen and
degenerated. There was inflammatory cell infiltration in the portal
area. In Fig. 2C, the pathological
features of the liver tissue at 168 h following the injection of
D-galactosamine in the control group are shown. Hepatocytes
revealed diffuse and confluent necrosis with bridging. Significant
proliferation of inflammatory cells was observed in the portal
area. The pathological features of the liver tissue with BMSC
transplantation are shown in Fig.
2D (120 h following BMSC transplantation through the portal
vein), Fig. 2E (168 h following
BMSC transplantation through the portal vein) and Fig. 2F (168 h following BMSC
transplantation through the tail vein). In the portal and tail vein
transplantation groups, inflammatory cell infiltration was
significantly reduced compared with that in the control group. The
hepatic lobules were gradually restored. Bile duct hyperplasia in
the portal area was also observed. Statistically, the inflammatory
activity in the transplantation groups was significantly improved
compared with that in the control group (P<0.05; Table V).
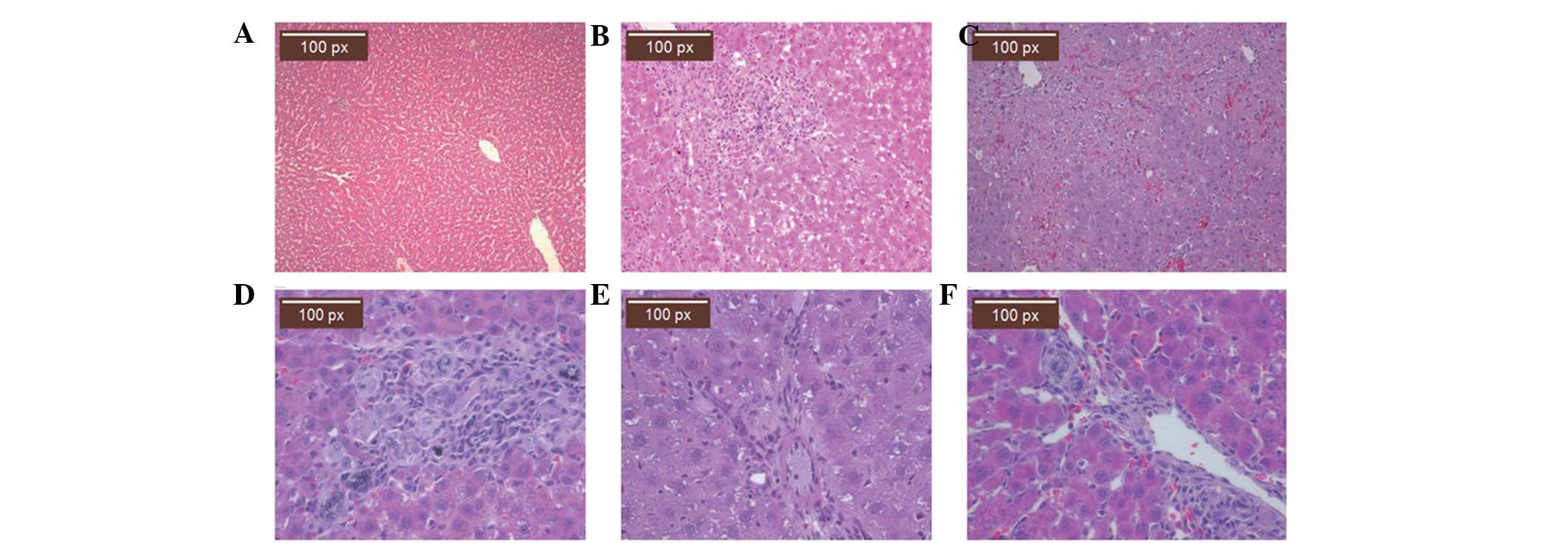 | Figure 2Pathological features of liver tissue
by hematoxylin and eosin (H&E) staining. At 24, 120 and 168 h
following bone marrow mesenchymal stem cell (BMSC) transplantation,
liver tissue was collected from healthy, control, tail vein and
portal vein group rats. The tissues were stained with H&E. (A)
Histological features of healthy rat liver tissue (magnification,
×100). Pathological features of liver tissue in (B) the control
group at 24 h (magnification, ×200), (C) the control group at 168 h
(magnification, ×200), (D) the portal vein group at 120 h following
BMSC transplantation (magnification, ×400), (E) the portal vein
group at 168 h following BMSC transplantation (magnification, ×400)
and (F) the tail vein group at 168 h following BMSC transplantation
(magnification, ×400). |
 | Table VInflammatory activity of the liver
tissues in each group at the three time points. |
Table V
Inflammatory activity of the liver
tissues in each group at the three time points.
| Groups | 24 h | 120 h | 168 h |
|---|
| Control | 43.20±10.73 | 46.40±14.31 | 46.67±12.82 |
| Tail vein | 41.60±17.34 | 22.00±16.84a | 18.33±8.78a |
| Portal vein | 38.20±22.54 | 20.60±7.60a | 12.67±8.78a |
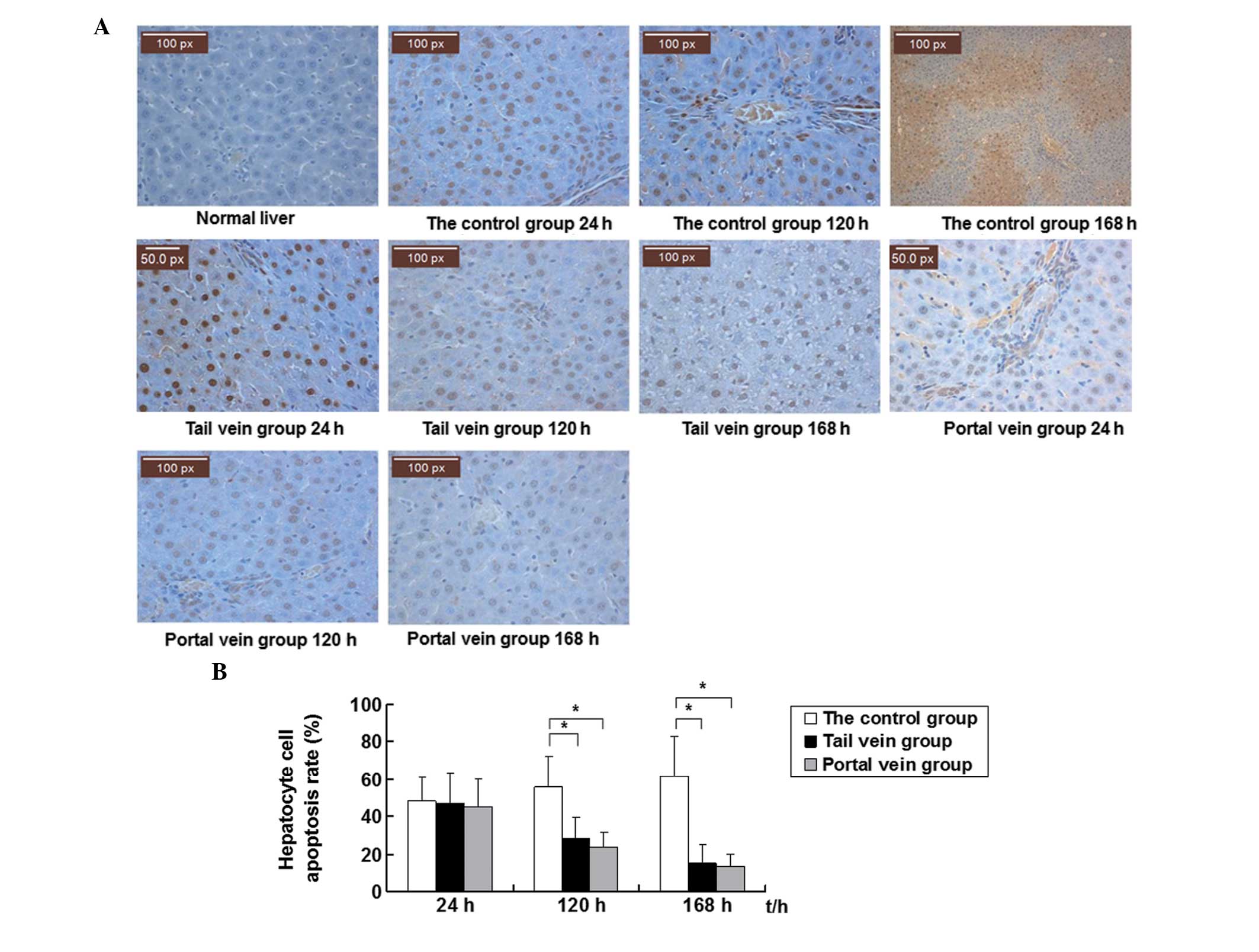
BMSC transplantation inhibits hepatic
apoptosis
Hepatic apoptosis was detected by TUNEL staining.
Representative TUNEL staining results are shown in Fig. 3A. In the normal liver tissue, TUNEL
negative cells or normal hepatocytes were characterized by blue
staining. TUNEL positive cells or the apoptotic cells were
characterized by brown particles confined within the nucleus. The
apoptotic cells were detected as early as 24 h following
transplantation in all three groups. In the control group, the
level of apoptosis increased with the progression of liver failure
and peaked at 168 h. However, the level of apoptosis decreased at
120 h following BMSC transplantation in the tail and portal vein
groups. Normal hepatocytes were observed. At 168 h following BMSC
transplantation, the level of apoptosis in the tail and portal vein
groups decreased to the lowest level of the experimental
period.
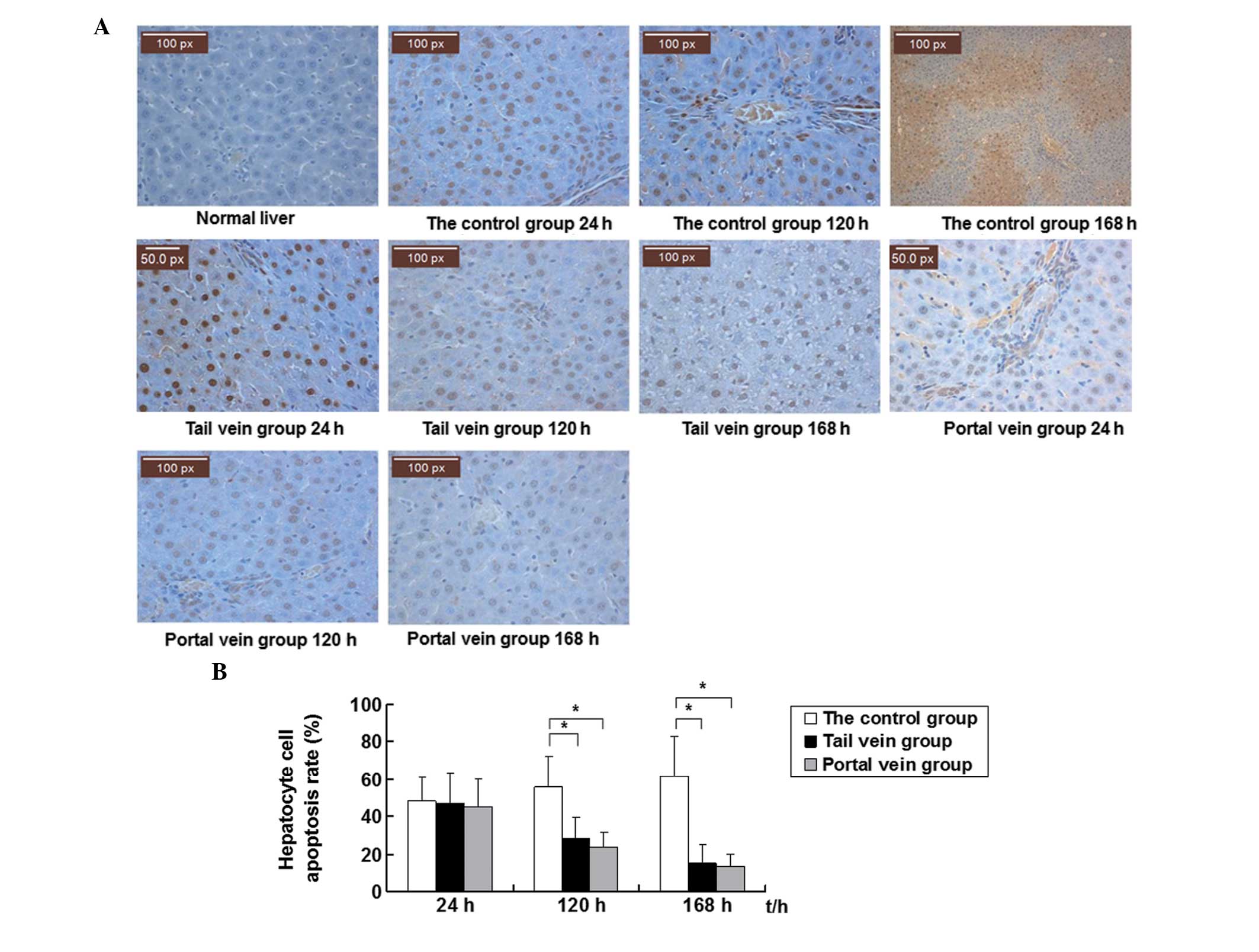 | Figure 3Apoptosis analysis of liver tissue by
terminal deoxynucleotidyl transferase dUTP nick end labeling
(TUNEL) staining. At 24, 120 and 168 h following bone marrow
mesenchymal stem cell (BMSC) transplantation, liver tissue was
collected from the normal, control, tail vein and portal vein group
rats. Hepatic apoptosis was analyzed by TUNEL staining. (A)
Representative TUNEL staining results of normal, control, tail vein
and portal vein group liver tissue at the three time points
(magnification, ×400). Normal hepatocytes are characterized by blue
staining. Apoptotic cells are characterized by brown particles
confined within the nucleus. (B) Apoptosis rate of hepatocytes in
the control, tail vein and portal vein groups at the three time
points. Five fields at high magnification (magnification, ×400)
were randomly selected in each slice. The number of apoptotic cells
was calculated. The apoptosis rate was calculated as the ratio of
TUNEL positive cell number to the total liver cell number/field.
*P<0.05, control vs. tail vein and portal vein
groups. |
Quantitative results are shown in Fig. 3B. Five fields at high magnification
(x400) were randomly selected in each slice. The number of
apoptotic cells in each field was counted. The apoptosis rate was
calculated as the ratio of the TUNEL positive cell number to the
total liver cell number per field. At 24 h following
transplantation, there were no statistically significant
differences in the apoptosis rate among the control (48.00±12.88%),
tail vein (47.20±15.71%) and portal vein groups (45.00±14.78%).
However, at 120 and 168 h following transplantation, the number of
apoptotic cells was reduced in the portal and tail vein groups,
whereas in the control group, the number of apoptotic cells was
slightly increased compared with the respective values at 24h. The
apoptosis rate at 120 h following transplantation in the control,
tail vein and portal vein groups was 55.40±16.94, 28.6±11.22 and
23.40±82.95%, respectively. At 168 h following transplantation, the
rate of apoptosis in the control, tail vein and portal vein groups
was 61.33±21.55%, 15.00±10.39 and 13.17±65.24%, respectively.
Statistically, the apoptosis rates in the portal and tail vein
groups were significantly lower compared with those in the control
group (P<0.05) at 120 h and 168 h following transplantation.
There was no significant difference in the rate of apoptosis
between the portal and tail vein groups. These data demonstrate
that BMSC transplantation is able to inhibit hepatic apoptosis.
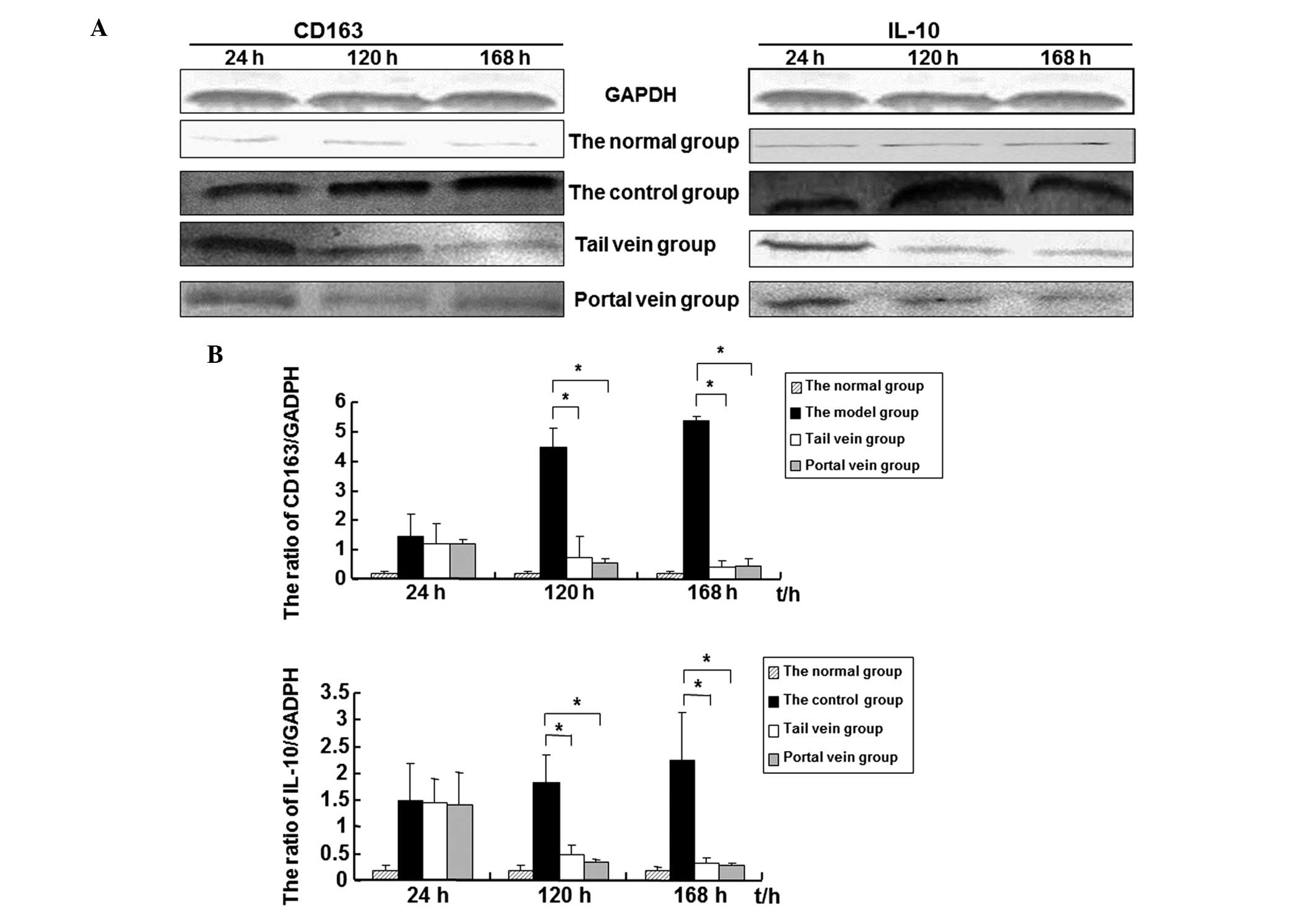
Expression levels of the CD163 and IL-10
proteins decrease in rat liver tissue following BMSC
transplantation
Western blot analysis was performed to detect the
expression levels of CD163 and IL-10 in rat liver tissue.
Representative western blot analysis results are shown in Fig. 4A and quantitative results are shown
in Fig. 4B and Table VI. In the control group, the
expression levels of CD163 and IL-10 gradually increased from 24 to
168 h following transplantation. However, in the portal and tail
vein groups, the expression levels of CD163 and IL-10 gradually
decreased from 24 to 168 h following transplantation.
Statistically, there were no significant differences among the
three groups in the expression levels of CD163 or IL-10 at 24 h
following transplantation. At 120 and 168 h following
transplantation, the expression levels of CD163 and IL-10 in the
portal and tail vein groups were significantly lower than those in
the control group (P<0.05). At the same time, the difference
between the portal and tail vein groups in the expression levels of
CD163 and IL-10 was not significant. Correlation analysis was
carried out between the expression levels of CDl63 and IL-10 in
liver tissue. The results revealed that the expression levels of
CDl63 were positively correlated with the expression levels of
IL-10 at 120 h (r=0.909, P=0.001) and 168 h (r=0.913, P=0.001).
 | Table VIExpression levels of CDl63 and IL-10
protein in liver tissue (relative to GAPDH). |
Table VI
Expression levels of CDl63 and IL-10
protein in liver tissue (relative to GAPDH).
| 24 h | 120 h | 168 h |
|---|
|
|
|
|
|---|
| Groups | CDl63 | IL-10 | CDl63 | IL-10 | CDl63 | IL-10 |
|---|
| Normal | 0.20±0.64 | 0.19±0.10 | 0.20±0.56 | 0.18±0.10 | 0.19±0.09 | 0.18±0.08 |
| Control | 1.47±0.74 | 1.50±0.70 | 4.48±0.68 | 1.82±0.52 | 5.37±0.17 | 2.27±0.87 |
| Tail vein | 1.21±0.68 | 1.46±0.45 | 0.75±0.72a | 0.49±0.17a | 0.41±0.23a | 0.32±0.10a |
| Portal vein | 1.18±0.17 | 1.40±0.61 | 0.54±0.16a | 0.35±0.56a | 0.47±0.23a | 0.28±0.56a |
Discussion
Orthotopic liver transplantation (OLT) is the
therapy used as a last resort following the failure of medical
management (18,19). Apart from OLT, stem cell
transplantation, with the characteristics of simplicity,
flexibility and fewer side-effects on the patients, has become
another effective means of treating liver failure in recent years
(20–22).
The present study revealed that BMSC transplantation
may effectively improve liver function, inhibit hepatic apoptosis
and alleviate the pathological damage of liver failure in rats.
There was no statistically significant difference in the effect of
BMSC transplantation between the portal and tail vein groups. This
may be due to the spontaneous gathering of stem cells at the
damaged site. Cell necrosis in injured tissues releases a series of
signaling molecules, triggering the mobilization of bone marrow
stem cells to the peripheral blood. The corresponding stem cells
bind with specific receptors expressed on the injured tissues and
attach to the damaged site in order to repair the injured tissues
(23,24). However, this may also be caused by
the short detection time of the present study, since the effect of
BMSC transplantation was not analyzed for longer than 168 h. Thus,
whether the effect of portal vein transplantation differs to that
of tail vein transplantation requires further investigation.
Previous studies have demonstrated that BMSCs
promote hepatic regeneration, inhibit inflammation, apoptosis and
hepatic stellate cell activation, degrade the redundant
extracellular matrix and improve liver fibrosis via the paracrine
production of cytokines and growth factors (25–27).
In the current study, the apoptosis rate of hepatocytes following
transplantation was significantly decreased, indicating that BMSCs
were able to reduce the inflammatory response in the liver and
inhibit hepatic apoptosis.
Studies have demonstrated that there are varying
degrees of endotoxemia and inflammatory cascades in AHF, leading to
changes in the levels of cytokines (28). Endotoxemia, macrophage
overactivation and proinflammatory cytokines may induce the
expression of CD163. CD163 activates monocyte and macrophage cells
in vivo and mediates heme oxygenase-1 synthesis. Heme
oxygenase-1 exerts anti-inflammatory, antioxidant and
anti-apoptotic effects on the body. Degradation of heme by heme
oxygenases results in the production of CO, iron and biliverdin
(29,30). Previous studies have demonstrated
that IL-10 and the macrophage colony-stimulating factor (M-CSF) may
induce the differentiation of monocytes into macrophages, which may
further upregulate CD163 mRNA and protein expression. However,
CD163 may also induce macrophages to secrete anti-inflammatory
cytokines, including IL-10 (31,32).
A study has identified that CD163 is a receptor of the tumor
necrosis factor (TNF)-like weak inducer of apoptosis (TWEAK)
cytokine; by binding with TWEAK, CD163 may induce the endocytosis
of TWEAK and inhibit the proapoptotic function of TWEAK (33). In the current study, the levels of
CD163 and IL-10 in the serum and liver tissue were detected by
ELISA and western blot analysis. It was observed that the
expression levels of CDl63 were correlated with the expression
levels of IL-10. The levels of CD163 and IL-10 increased with the
increase in the level of apoptosis, indicating an anti-apoptotic
role of CD163 and IL-10 in the liver.
Liver failure is a severe disease with a high
mortality rate. Thus, evaluating the patient condition and
prognosis objectively, effectively and in a timely manner is of
great importance. The current liver failure prognosis assessment
system is widely used in clinical practice. However, in order to
improve its accuracy, new evaluation indices are required. In the
present study, following BMSC transplantation, the levels of ALT,
AST, DBIL and IBIL significantly decreased with time whereas the
level of ALB significantly increased. These data suggest that liver
function was improved by BMSC transplantation. Furthermore, with
the elevation of the levels of ALT and AST in the plasma, the
levels of CDl63 and IL-10 in the serum and liver tissue of rats
with AHF were significantly increased in the control group compared
with those in normal mice. These levels of CDl63 and IL-10 were
significantly higher than those in the BMSC transplantation group.
Furthermore, the levels of CDl63 and IL-10 were significantly
correlated with the levels of ALT and AST, which reflected the
sharp deterioration in liver function and disease severity. These
results suggest that CDl63 and IL-10 play important roles in the
pathogenesis of AHF and that CDl63 and IL-10 may be used as
sensitive serum marker proteins for the diagnosis and prognosis of
AHF. Following BMSC transplantation, the levels of CDl63 and IL-10
in the serum and liver tissue decreased and liver function was
gradually restored. These data indicate that BMSC transplantation
may improve the immune status of AHF model rats and that BMSC
transplantation had a protective effect on rats with AHF. Thus,
through downregulating the levels of CDl63 and IL-10, BMSC
transplantation promoted the inflammatory and anti-inflammatory
cytokines to reach a new equilibrium. This may be one of the
mechanisms by which BMSCs exert their therapeutic functions on AHF.
In summary, the present results demonstrated the therapeutic effect
of BMSCs on AHF. In the future, CD163 and IL-10 may be used as
sensitive serum prognosis indicators in the early assessment of
patients undergoing liver transplantation.
In summary, BMSCs are of great scientific and
clinical value for the treatment of AHF. However, further studies
are necessary to explore the potential of BMSC differentiation and
treatment mechanisms. Further study is also required to observe the
changes in liver function and cytokines for longer than 168 h
following liver BMSC transplantation in order to clarify the
treatment mechanisms and investigate the effect of BMSC
transplantation.
Acknowledgements
The authors of the present study would like to thank
the staff of the Key Laboratory of Xinjiang Medical Animal Model
Research for their ongoing support. They are grateful to Mrs. Hui
Liu, Mrs. Qing Wei and Mr. Shutao Zheng for their help with cell
irradiation and performing the cell transplantation and biopsy
procedures. This study was supported by grants from the Key
Laboratory of Xinjiang Medical Animal Model Research of China (No.
XJDX1103-2012-01) and by the funding project of key discipline of
Internal Medicine, Xinjiang Uygur Autonomous Region.
References
|
1
|
Lee WM, Squires RH Jr, Nyberg SL, Doo E
and Hoofnagle JH: Acute liver failure: Summary of a workshop.
Hepatology. 47:1401–1415. 2008.PubMed/NCBI
|
|
2
|
Kung JW and Forbes SJ: Stem cells and
liver repair. Curr Opin Biotechnol. 20:568–574. 2009. View Article : Google Scholar
|
|
3
|
Oertel M and Shafritz DA: Stem cells, cell
transplantation and liver repopulation. Biochim Biophys Acta.
1782:61–74. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Locke JE, Shamblott MJ and Cameron AM:
Stem cells and the liver: clinical applications in transplantation.
Adv Surg. 43:35–51. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Salama H, Zekri AR, Zern M, et al:
Autologous hematopoietic stem cell transplantation in 48 patients
with end-stage chronic liver diseases. Cell Transplant.
19:1475–1486. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mark AL, Sun Z, Warren DS, et al: Stem
cell mobilization is life saving in an animal model of acute liver
failure. Ann Surg. 252:591–596. 2010.PubMed/NCBI
|
|
7
|
Antoniades CG, Berry PA, Wendon JA and
Vergani D: The importance of immune dysfunction in determining
outcome in acute liver failure. J Hepatol. 49:845–861. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Stuart WD, Kulkarni RM, Gray JK,
Vasiliauskas J, Leonis MA and Waltz SE: Ron receptor regulates
Kupffer cell-dependent cytokine production and hepatocyte survival
following endotoxin exposure in mice. Hepatology. 53:1618–1628.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Taylor RC, Cullen SP and Martin SJ:
Apoptosis: controlled demolition at the cellular level. Nat Rev Mol
Cell Biol. 9:231–241. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Malhi H, Guicciardi ME and Gores GJ:
Hepatocyte death: a clear and present danger. Physiol Rev.
90:1165–1194. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sulahian TH, Hintz KA, Wardwell K and
Guyre PM: Development of an ELISA to measure soluble CD163 in
biological fluids. J Immunol Methods. 252:25–31. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hiraoka A, Horiike N, Akbar SM, Michitaka
K, Matsuyama T and Onji M: Soluble CD163 in patients with liver
diseases: very high levels of soluble CD163 in patients with
fulminant hepatic failure. J Gastroenterol. 40:52–56. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sulahian TH, Högger P, Wahner AE, et al:
Human monocytes express CD163, which is upregulated by IL-10 and
identical to p155. Cytokine. 12:1312–1321. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pae HO and Chung HT: Heme oxygenase-l: its
therapeutic roles in inflammatory diseases. Immune Netw. 9:12–19.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Buechler C, Ritter M, Orsó E, Langmann T,
Klucken J and Schmitz G: Regulation of scavenger receptor CD163
expression in human monocytes and macrophages by pro- and
antiinflammatory stimuli. J Leukoc Biol. 67:97–103. 2000.PubMed/NCBI
|
|
16
|
Parekkadan B, van Poll D, Suganuma K,
Carter EA, Berthiaume F, Tilles AW and Yarmush ML: Mesenchymal stem
cell-derived molecules reverse fulminant hepatic failure. PLoS One.
2:e9412007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kuo TK, Hung SP, Chuang CH, et al: Stem
cell therapy for liver disease: parameters governing the success of
using bone marrow mesenchymal stem cells. Gastroenterology.
134:2111–2121. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ismail A, Fouad O, Abdelnasser A,
Chowdhury A and Selim A: Stem cell therapy improves the outcome of
liver resection in cirrhotics. J Gastrointest Cancer. 41:17–23.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Stutchfield BM, Forbes SJ and Wigmore SJ:
Prospects for stem cell transplantation in the treatment of hepatic
disease. Liver Transpl. 16:827–836. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Cho KA, Ju SY, Cho SJ, et al: Mesenchymal
stem cells showed the highest potential for the regeneration of
injured liver tissue compared with other subpopulations of the bone
marrow. Cell Biol Int. 33:772–777. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Enns GM and Millan MT: Cell-based
therapies for metabolic liver disease. Mol Genet Metab. 95:3–10.
2008. View Article : Google Scholar
|
|
22
|
Miyazaki M, Hardjo M, Masaka T, et al:
Isolation of a bone marrow-derived stem cell line with high
proliferation potential and its application for preventing acute
fatal liver failure. Stem Cells. 25:2855–2863. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sensebé L and Bourin P: Mesenchymal stem
cells for therapeutic purposes. Transplantation. 87(9 Suppl):
S49–S53. 2009.
|
|
24
|
Miura M, Miura Y, Padilla-Nash HM, et al:
Accumulated chromosomal instability in murine bone marrow
mesenchymal stem cells leads to malignant transformation. Stem
Cells. 24:1095–1103. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liu F, Liu ZD, Wu N, Cong X, Fei R, Chen
HS and Wei L: Transplanted endothelial progenitor cells ameliorate
carbon tetrachloride-induced liver cirrhosis in rats. Liver
Transpl. 15:1092–1100. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
26
|
Muraca M: Evolving concepts in cell
therapy of liver disease and current clinical perspectives. Dig
Liver Dis. 43:180–187. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Rust C and Gores GJ: Apoptosis and liver
disease. Am J Med. 108:567–574. 2000. View Article : Google Scholar
|
|
28
|
Ortiz LA, Dutreil M, Fattman C, Pandey AC,
Torres G, Go K and Phinney DG: Interleukin 1 receptor antagonist
mediates the antiinflammatory and antifibrotic effect of
mesenchymal stem cells during lung injury. Proc Natl Acad Sci USA.
104:11002–11007. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Møller HJ, Frikke-Schmidt R, Moestrup SK,
Nordestgaard BG and Tybjærg-Hansen A: Serum soluble CD163 predicts
risk of type 2 diabetes in the general population. Clin Chem.
57:291–297. 2011.PubMed/NCBI
|
|
30
|
Louis H, Le Moine O, Peny MO, et al:
Hepatoprotective role of interleukin 10 in
galactosamine/lipopolysaccharide mouse liver injury.
Gastroenterology. 112:935–942. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Philippidis P, Mason JC, Evans BJ, Nadra
I, Taylor KM, Haskard DO and Landis RC: Hemoglobin scavenger
receptor CDl63 mediates interleukin-10 release and heme oxygenase-1
synthesis: antiinflammatory monocyte-macrophage responses in
vitro, in resolving skin blisters in vivo, and after
cardiopulmonary bypass surgery. Circ Res. 94:119–126. 2004.
View Article : Google Scholar
|
|
32
|
Fabriek BO, van Bruggen R, Deng DM, et al:
The macrophage scavenger receptor CD163 functions as an innate
immune sensor for bacteria. Blood. 113:887–892. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Moreno JA, Muñoz-García B, Martín-Ventura
JL, et al: The CD163-expressing macrophages recognize and
internalize TWEAK: potential consequences in atherosclerosis.
Atherosclerosis. 207:103–110. 2009. View Article : Google Scholar : PubMed/NCBI
|