Introduction
It is not uncommon in clinical settings to encounter
patients with combined malignant gastric outlet obstruction (GOO)
and common bile duct obstruction (CBO). This can be caused by
pancreatic cancer, cholangiocarcinoma and ampullary duodenal
cancer, as well as a number of other malignant tumors (1,2).
Conventional treatment is a surgical bypass procedure, which is
associated with significant complications and high mortality rates
(3). Therefore, since the
introduction of the self-expanding metal stent (SEMS), stent
placement has become the preferred option in clinical palliative
management (4,5). For patients with symptoms resulting
in a progressive deterioration in the quality of life and limited
life expectancy, treatment is focused on palliation to ensure that
quality of life is maintained (6–9).
These symptoms include significant obstructive jaundice, dark
urine, itching, severe nausea, vomiting, intolerance to oral
feeding and abdominal pain. Endoscopic stent placement is now a
standard therapy for the management of biliary strictures (10–12)
and has been well accepted as clinical routine practice in
malignant CBO (13–15), malignant GOO (16,17),
malignant duodenal obstruction (18–20)
and malignant colonic obstruction (21–24).
However, few studies on dual endoscopic SEMS placement with the
co-existence of GOO and CBO have been published. It is believed
that, since extension of the duodenoscope to the duodenal papilla
is made difficult by GOO, this practice has become unpopular in
clinics. In the present study, our experience in applying
endoscopic biliary and duodenal stenting in 17 patients was
summarized and the techniques used to obtain a satisfactory
clinical outcome were described.
Materials and methods
Patients
The study was approved by the Ethics Committee of
Chao-Yang Hospital (Beijing, China). In total, 17 patients aged
62–87 years, including 14 males and three females, were reviewed.
All exhibited GOO and CBO, and received endoscopic biliary and
duodenal stent placements between January 2008 and May 2012.
Fourteen of the patients had pancreatic cancer, two had
cholangiocarcinoma and one had duodenal cancer, all of which were
unresectable. The locations of the GOO and CBO are listed in
Table I. Patients had clear
symptoms of GOO and CBO prior to treatment including skin and
sclera jaundice, dark brown urine, lighter stool color, vomiting
and abdominal pain. GOO and CBO were confirmed by biochemical
tests, computed tomography, magnetic resonance imaging and
endoscopy. Improvements in oral intake were monitored using the
Gastric Outlet Obstruction Scoring System (GOOSS) (6).
 | Table IDemographic summary and location of
obstructions. |
Table I
Demographic summary and location of
obstructions.
| Parameter | Value |
|---|
| Gender (n) |
| Male | 14 |
| Female | 3 |
| Age (years) | 76.6±6.5 |
| Malignancy (n) |
| Pancreatic
cancer | 14 |
|
Cholangiocarcinoma | 2 |
| Primary duodenal
carcinoma | 1 |
| Location of CBO
(n) |
| Distal common bile
duct | 10 |
| Mid CBO | 2 |
| Proximal and mid
CBO | 4 |
| Papilla | 1 |
| Location of GOO
(n) |
| Pylorus | 2 |
| Above the major
papilla | 5 |
| At the major
papilla | 8 |
| Under the major
papilla | 1 |
Surgical procedure
Patients were fasted for three days before surgery.
The stomach tube was placed for decompression when required to
ensure a clear vision of the endoscope. Anisodamine (20 mg; Modern
Hasen Pharmaceutical Co. Ltd., Shanghai, China) and diazepam (10
mg; Shanghai Xudong Haipu Pharmaceutical Co., Ltd., Shanghai,
China) were administered intravenously for gastric motility
inhibition and sedation, respectively, prior to the surgery.
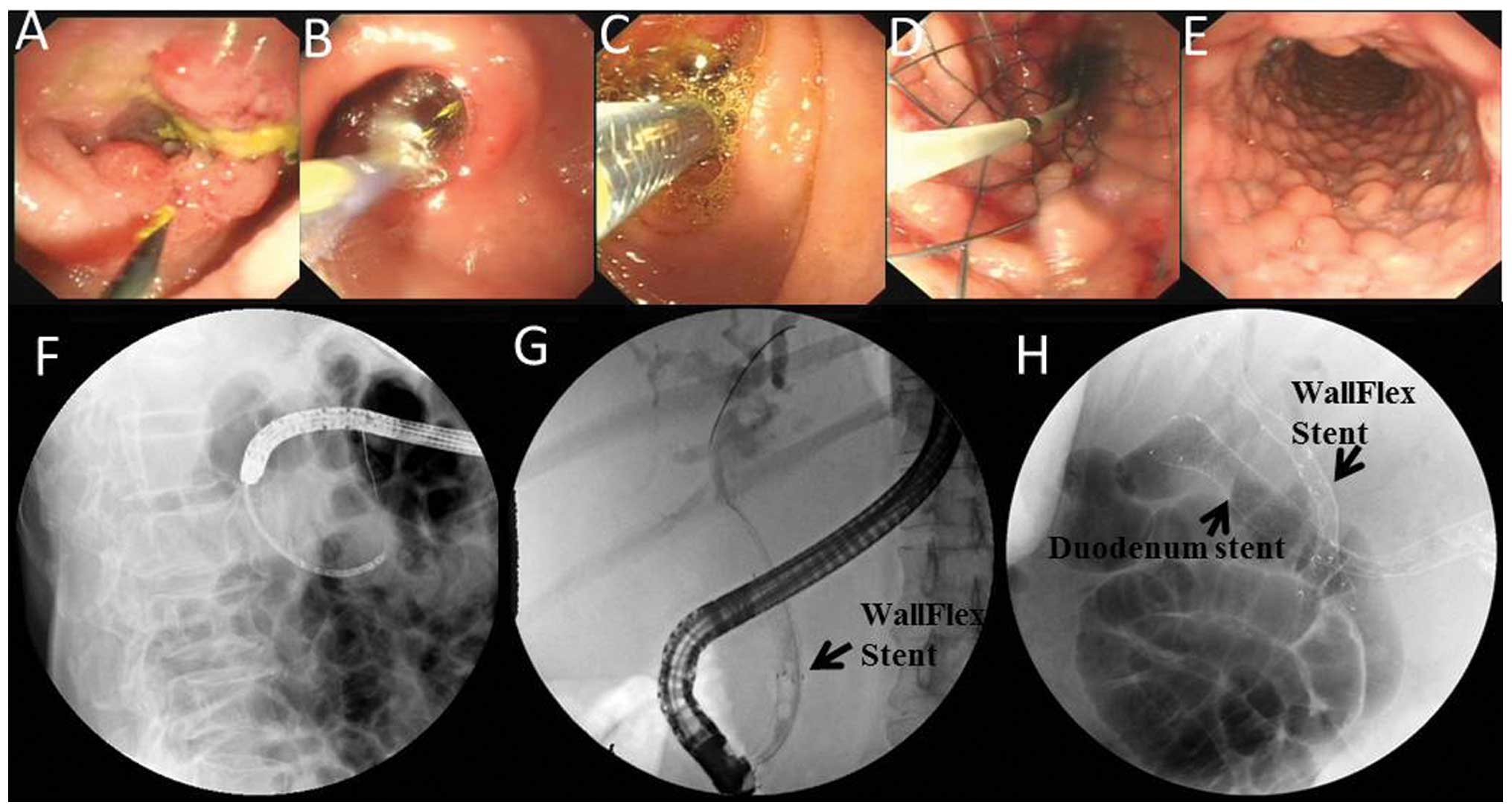
Stages of the surgical procedure are shown in
Fig. 1. The initial step was to
establish the duodenal passage. An ultra-slim gastric endoscope
(Olympus Corp., Tokyo, Japan) was placed into the gastric antrum or
duodenum, reaching to the distal end of the obstruction segment. A
Jagwire® guidewire (Boston Scientific, Natick, MA, USA)
was then inserted through the endoscope chamber into the jejunum
(Fig. 1A). The obstruction size
was measured while the endoscope was pulled out. If the ultra-slim
endoscope failed to pass through the stricture segment, the
guidewire was inserted from the biopsy channel. A double-lumen
catheter was then introduced along the guidewire to the distal end
of the stricture. Diatrizoate (30%; Hansen Pharmaceutical Co.,
Ltd., Hunan, China) was injected through the catheter while the
catheter was pulled to the proximal end of the stricture for the
obstruction length measurement. The guidewire was then retained and
the ultra-slim gastric endoscope or catheter was withdrawn,
followed by insertion of an electronic duodenoscope (TJF240;
Olympus Corp.) along the guidewire to reach the duodenal bulb, and
then insertion of a CRE™ dilation balloon (Boston Scientific) to
gradually dilate the duodenal stricture under direct visualization
(Fig. 1B). The ideal expansion
would be ≥13.5 mm in diameter to allow the duodenoscope to pass
through.
Following a successful dilation of the duodenum, the
duodenoscope was then moved forward into the descending section of
the duodenum. Papillary intubation and cholangiography were
performed, and a guidewire was re-introduced through the catheter
to the distal end of the bile duct stricture. With the guidewire,
an introducer carrying a biliary WallFlex™ stent (Boston
Scientific) with an appropriate length was placed into the common
bile duct (Fig. 1C and F).
The ultra-slim gastric endoscope was then
re-introduced into the duodenum, through which a guidewire was
inserted into the jejunum. The ultra-slim endoscope was replaced
with an ordinary gastric endoscope carrying a duodenal stent
(Boston Scientific) into the stricture (Fig. 1D and G). One end of the stent was
placed on the opening of the pyloric side (Fig. 1E and H).
Postoperative evaluation and
treatment
Antibiotics were administered for three days after
the surgery as a preventive measure. Serum amylase levels were
checked 2 h after the surgery and, if normal, a liquid diet was
allowed. Postoperative observation was focused on signs and
symptoms for upper gastrointestinal complications including
hyperamylasemia and upper gastrointestinal bleeding and
perforation. No special diet formula was administered if the
obstruction symptoms disappeared. Total bilirubin, direct
bilirubin, alkaline phosphatase, GOOSS score and nutritional
indicators, including triglycerol, albumin and hemoglobulin, were
measured on day 7. Telephone follow-up was performed for migration,
occlusion, possible procedure- or device-related complications and
survival time.
Statistical analysis
The statistical analysis was performed using IBM
SPSS statistical software version 21.0 (IBM-SPSS, Cary, NC, USA).
Paired differences prior and subsequent to surgery were assessed
with a Student’s t-test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Postoperative observations
Seventeen stenting procedures were performed
successfully on patients with both GOO and CBO in the Beijing
Chao-Yang Hospital (Beijing, China) between January 2008 and May
2012 with a success rate of 100%. Adequate clinical palliation was
observed, and details are listed in Table II. Improvements in the incidence
of spontaneous clinical manifestation were evidenced by the
immediate disappearance of vomiting and abdominal pain, as well as
the gradual disappearance of jaundice. Serum amylase levels were
checked at 2 h after the surgery. The majority of the patients
exhibited normal levels, with the exception of three patients who
developed transient hyperamylasemia, and who recovered without
intervention within 72 h. Minor bleeding occurred only in one case
in the duodenal stricture during balloon dilation, and ceased
following application of an ice-cold adrenaline saline spray.
Biochemical measurements were taken after seven days. Average total
bilirubin decreased by 40%, direct bilirubin decreased by 44% and
alkaline phosphatase decreased by 60% postoperatively (Table II). The GOOSS score increased from
0.9±1.1 points preoperatively to 2.1±0.7 points postoperatively.
These differences were statistically significant (P<0.01).
Nutritional status was found to be significantly improved following
the surgery (Table II).
 | Table IIComparison of patients prior and
subsequent to the stenting surgery. |
Table II
Comparison of patients prior and
subsequent to the stenting surgery.
| Item | Prior to surgery | Following
surgery | P-value |
|---|
| Clinical
manifestations (n) |
| Vomiting | 17 | 1 | |
| Abdominal pain | 17 | 2 | |
| Jaundice | 17 | 4 | |
| Dark urine | 17 | 0 | |
| Serological
tests |
| Total bilirubin
(μM/l) | 263.4±62.5 | 157.6±25.1 | <0.01 |
| Direct bilirubin
(μM/l) | 233.2±66.5 | 130.9±27.7 | <0.01 |
| Alkaline phosphatase
(IU/l) | 534.2±78.7 | 216.3±23.3 | <0.01 |
| Triglycerol
(mmol/l) | 0.61±0.07 | 0.68±0.08 | <0.01 |
| Albumin (g/l) | 32.08±2.15 | 33.13±1.54 | <0.01 |
| Hemoglobulin
(g/l) | 135.60±14.35 | 145.30±8.44 | <0.01 |
| GOOSS score | 0.9±1.1 | 2.1±0.7 | <0.01 |
Follow-up
No stent migration was found during the follow-up
period. Occlusion occurred in one case at the distal end of the
stent after three months due to tumor infiltration or compression.
A three-cavity jejunal feeding tube was placed for decompression
and nutrition. Restricture was found at the biliary location in two
cases due to tumor invasion, which caused obstructive jaundice;
this symptom was relieved following percutaneous transhepatic
drainage. The mean survival time of patients was 192 days ranging
between 70 and 332 days.
Discussion
Surgical treatment, including biliary-enteric
anastomosis or gastrojejunostomy, has been traditionally applied in
cases of GOO and CBO. However, such traumatic surgery has been
associated with serious complications and a failure to increase
patient survival rate. For patients unable to tolerate surgery,
decompression and enteral feeding tubes have typically been
provided as alternative methods (22,25–27).
In recent years, this traditional approach has been gradually
replaced by other minimally invasive approaches. SEMS placement is
an approach that has demonstrated advantages and cost effectiveness
over the traditional treatments (4,5). In
the cases of CBO and GOO, however, few reports have been published
regarding dual stents for palliation of these two obstructions.
Certain studies used oral duodenal stenting in combination with
percutaneous transhepatic biliary metal stent implantation
(28,29). The endoscopic procedure with dual
stenting should be the first choice for its minimal invasiveness,
lower tissue damage, and fewer postoperative complications. Dual
stents were successfully installed in the present study in 17
patients with GOO and CBO without any significant complications.
The data demonstrated that the procedure was safe and effective,
and the quality of life of the patients was significantly improved
following the procedure.
Several key elements should be addressed for a
successful result in this dual stenting procedure. Firstly, it is
very important to establish an endoscopic duodenal corridor.
Conventionally, it has been considered that endoscopes cannot reach
the duodenal papilla due to GOO. It is difficult for the endoscope
to pass through the obstruction without causing complications, such
as bleeding, perforation or tumor rupture. The CRE wire-guided
balloon dilation catheter has gained traction to overcome this
problem by applying controlled radial expansion (30–33).
Guided by the wire, the axis of the balloon can be kept in parallel
with the axis of the luminal cavity, thus preventing the tip of the
balloon catheter from piercing into the duodenal wall or tumor,
which could cause bleeding or perforation. Therefore, the balloon
can be negotiated across the stricture, during which appropriate
pressure can be gradually applied to avoid any abrupt shearing
force, and the center of the balloon can be always kept at the
center of the stricture.
Usually, endoscopic retrograde
cholangiopancreatography (ERCP) following CRE balloon dilation for
the duodenum would be difficult since i) the duodenum space is
smaller than the normal duodenum, even subsequent to dilation; ii)
the normal structure of the duodenal papilla may have been damaged
by tumor invasion; and iii) balloon dilatation may cause tissue
edema that further increases the difficulty of recognizing the
papilla. Due to the smaller space inside the duodenum, the
experience in the present study was that the exposed metal stents
inside the duodenum should be ≤10 mm to avoid damage of the
contralateral duodenal wall. In addition, since patients often
experienced prolonged biliary obstruction that caused the
accumulation of higher pressure in the bile duct, extra precaution
was taken when the angiography was performed, including the
withdrawal of a small portion of bile prior to injection of the
contrast reagent, and ensuring only necessary volumes of the
contrast reagent were injected.
Finally, duodenal stenting requires precise
positioning. A drawback force would help position the stent while
it was released from the introducer to keep it within the stricture
segment. In addition, great care should be taken to avoid the
guidewire penetrating through the mesh of the exposed portion of
the biliary stent. X-ray-guided endoscopic guidewire placement
cannot precisely determine the guidewire position. Application of
the ultra-slim endoscope is much more convenient for guiding as
well as observing the procedure of the stent placement.
Although endoscopic biliary metal stenting and
duodenal stenting exhibit a minimally invasive character,
complications can still be an occasionally serious problem. Major
complications include hyperamylasemia, post-ERCP pancreatitis,
cholangitis, biliary fistula, bleeding, perforation and migration.
Three patients in the present study were observed to develop
transient hyperamylasemia (17.6%) and one patient exhibited
duodenal bleeding following dilation (5.9%), which is similar to
what has been reported in the literature (34).
The major long-term complication is stent
restricture due to tumor infiltration. Duodenal stent restricture
can be relieved by a new stent placement in the original duodenal
stent. For common bile duct stent restricture, it is not
appropriate to perform ERCP-related processing since the duodenal
stent blocks the duodenal papilla. One of the options would be to
perform percutaneous transhepatobiliary puncture for biliary
drainage, while inserting the guidewire through the drainage into
the distal end of duodenum. An expandable balloon of 8–19 mm with
the guidewire could expand the duodenal stent mesh so that the mesh
could be opened wide enough to allow biliary stent placement. The
balloon could also be used to assist the complete expansion of the
biliary stent. No clear interference was observed between the
duodenal and biliary stents, which is consistent with previously
reported results (29,35).
One of the parameters monitored postoperatively in
the present study was the nutritional status of the patients. The
data showed that levels of triglycerol, albumin and hemoglobulin
improved following the surgery, indicating that the nutritional
status of the patients did not continue deteriorating. Furthermore,
the improvement in the GOOSS score demonstrated the benefit of the
procedure for the quality of life of the patients.
In conclusion, endoscopic dual stent placement for
combined GOO and CBO is a safe and effective procedure that can
greatly improve the quality of life and nutritional status of
patients. However, the recanalization of GOO and CBO does not
address the cause of the malignant obstruction. With regard to the
continued growth and spread of tumors, it would be interesting to
explore the possibilities of preventing restricture by local
chemotherapy or biotherapy with stenting (36).
Acknowledgements
This study was sponsored by institutional funding of
the Beijing Chao-Yang Hospital, 2012.
References
|
1
|
Khullar SK and DiSario JA: Gastric outlet
obstruction. Gastrointest Endosc Clin N Am. 6:585–603. 1996.
|
|
2
|
Johnson CD and Ellis H: Gastric outlet
obstruction now predicts malignancy. Br J Surg. 77:1023–1024. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Oida T, Mimatsu K, Kano H, Kawasaki A,
Kuboi Y, Fukino N, Kida K, Aramaki O and Amano S: Palliative
enteric bypass for malignant gastric outflow obstruction after
pancreaticoduodenectomy in early recurrent pancreatic cancer.
Hepatogastroenterology. 58:1360–1367. 2011. View Article : Google Scholar
|
|
4
|
Kozarek RA, Ball TJ and Patterson DJ:
Metallic self-expanding stent application in the upper
gastrointestinal tract: caveats and concerns. Gastrointest Endosc.
38:1–6. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Topazian M, Ring E and Grendell J:
Palliation of obstructing gastric cancer with steel mesh,
self-expanding endoprostheses. Gastrointest Endosc. 38:58–60. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Adler DG and Baron TH: Endoscopic
palliation of malignant gastric outlet obstruction using
self-expanding metal stents: experience in 36 patients. Am J
Gastroenterol. 97:72–78. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Piesman M, Kozarek RA, Brandabur JJ,
Pleskow DK, Chuttani R, Eysselein VE, Silverman WB, Vargo JJ II,
Waxman I, Catalano MF, Baron TH, Parsons WG III, Slivka A and
Carr-Locke DL: Improved oral intake after palliative duodenal
stenting for malignant obstruction: a prospective multicenter
clinical trial. Am J Gastroenterol. 104:2404–2411. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tempero M, Arnoletti JP, Ben-Josef E,
Bhargava P, Casper ES, Kim P, Malafa MP, Nakakura EK, Shibata S,
Talamonti M, Wang H and Willett C: Pancreatic adenocarcinoma.
Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw.
5:998–1033. 2007.PubMed/NCBI
|
|
9
|
van Hooft JE, Uitdehaag MJ, Bruno MJ,
Timmer R, Siersema PD, Dijkgraaf MG and Fockens P: Efficacy and
safety of the new WallFlex enteral stent in palliative treatment of
malignant gastric outlet obstruction (DUOFLEX study): a prospective
multicenter study. Gastrointest Endosc. 69:1059–1066.
2009.PubMed/NCBI
|
|
10
|
Andersen JR, Sørensen SM, Kruse A,
Rokkjaer M and Matzen P: Randomised trial of endoscopic
endoprosthesis versus operative bypass in malignant obstructive
jaundice. Gut. 30:1132–1135. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Artifon EL, Sakai P, Cunha JE, Dupont A,
Filho FM, Hondo FY, Ishioka S and Raju GS: Surgery or endoscopy for
palliation of biliary obstruction due to metastatic pancreatic
cancer. Am J Gastroenterol. 101:2031–2037. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Speer AG, Cotton PB, Russell RC, Mason RR,
Hatfield AR, Leung JW, MacRae KD, Houghton J and Lennon CA:
Randomised trial of endoscopic versus percutaneous stent insertion
in malignant obstructive jaundice. Lancet. 2:57–62. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen YZ, Wang JH, Feng BS, et al:
Endoscopic biliary stenting for malignant biliary obstruction in
124 cases. Zhonghua Xiao Hua Nei Jing Za Zhi. 28:341–342. 2011.(In
Chinese).
|
|
14
|
Luigiano C, Ferrara F, Cennamo V, Fabbri
C, Bassi M, Ghersi S, Consolo P, Morace C, Polifemo AM, Billi P,
Ceroni L, Alibrandi A and D’Imperio N: A comparison of uncovered
metal stents for the palliation of patients with malignant biliary
obstruction: nitinol vs. stainless steel. Dig Liver Dis.
44:128–133. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Varadarajulu S, Tutuian R, Gostout C,
Kozarek R, Wilcox CM and Cotton PB: Efficacy of the Za
self-expandable metal stent for palliation of malignant biliary
obstruction. J Clin Gastroenterol. 38:77–80. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Larssen L, Medhus AW and Hauge T:
Treatment of malignant gastric outlet obstruction with stents: an
evaluation of the reported variables for clinical outcome. BMC
Gastroenterol. 9:452009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yao LQ and Zhong ZS: Application progress
of endoscopic metal stents for treatment of gastric outlet
obstruction. Zhonghua Xiao Hua Nei Jing Za Zhi. 24:474–476.
2007.(In Chinese).
|
|
18
|
Chen YX, Li GH, Zhou XJ and Lv NH:
Endoscopic stenting combined with X-ray monitoring for the
treatment of malignant duodenal obstruction: analysis of 9 cases.
Zhonghua Xiao Hua Nei Jing Za Zhi. 27:40–41. 2010.(In Chinese).
|
|
19
|
Johnston SD, McKelvey ST, Moorehead RJ,
Spence RA and Tham TC: Duodenal stents for malignant duodenal
strictures. Ulster Med J. 71:30–33. 2002.PubMed/NCBI
|
|
20
|
Li DM, Li RX, Hou W, et al: Endoscopic
metal stenting of malignant gastroduodenal obstruction: efficacy
observation. Zhonghua Xiao Hua Nei Jing Za Zhi. 25:556–557.
2008.(In Chinese).
|
|
21
|
Cho YK, Kim SW, Lee BI, Lee KM, Lim CH,
Kim JS, Chang JH, Park JM, Lee IS, Choi MG, Choi KY and Chung IS:
Clinical outcome of self-expandable metal stent placement in the
management of malignant proximal colon obstruction. Gut Liver.
5:165–170. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Scott-Mackie P, Morgan R, Farrugia M,
Glynos M and Adam A: The role of metallic stents in malignant
duodenal obstruction. Br J Radiol. 70:252–255. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Tominaga K, Maetani I, Sato K, Shigoka H,
Omuta S, Ito S and Saigusa Y: Favorable long-term clinical outcome
of uncovered D-weave stent placement as definitive palliative
treatment for malignant colorectal obstruction. Dis Colon Rectum.
55:983–989. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhong YS, Yao LQ, Xu JM, et al:
Self-expanding metallic stents for acute obstruction of the
proximal colorectal cancer. Zhonghua Xiao Hua Nei Jing Za Zhi.
27:505–508. 2010.(In Chinese).
|
|
25
|
Sankarankutty AK, Mente ED, Cardoso NM and
Castro-E-Silva O: T-tube or no T-tube for bile duct anastomosis in
orthotopic liver transplantation. Hepatobiliary Surg Nutr.
2:171–173. 2013.PubMed/NCBI
|
|
26
|
Farooq A, Patel R, Sorefan N and Ammori
BJ: Laparoscopic exclusion gastroenterostomy for palliation of
gastric outlet obstruction secondary to recurrent
cholangiocarcinoma. Hepatogastroenterology. 51:1886–1888.
2004.PubMed/NCBI
|
|
27
|
Feretis C, Benakis P, Dimopoulos C,
Georgopoulos K, Milas F, Manouras A and Apostolidis N: Palliation
of malignant gastric outlet obstruction with self-expanding metal
stents. Endoscopy. 28:225–228. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Akinci D, Akhan O, Ozkan F, Ciftci T,
Ozkan OS, Karcaaltincaba M and Ozmen MN: Palliation of malignant
biliary and duodenal obstruction with combined metallic stenting.
Cardiovasc Intervent Radiol. 30:1173–1177. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhang XQ, Liu CW, Wang SQ, et al:
Treatment of malignant biliary and duodenal obstruction using
percutaneous trans-hepatic catheterization in combination with
per-oral stent placement. Fang She Xue Shi Jian Bian Ji Bu.
22:514–517. 2007.(In Chinese).
|
|
30
|
Benjamin SB, Cattau EL and Glass RL:
Balloon dilation of the pylorus: therapy for gastric outlet
obstruction. Gastrointest Endosc. 28:253–254. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Benjamin SB, Glass RL, Cattau EL Jr and
Miller WB: Preliminary experience with balloon dilation of the
pylorus. Gastrointest Endosc. 30:93–95. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kochhar R and Kochhar S: Endoscopic
balloon dilation for benign gastric outlet obstruction in adults.
World J Gastrointest Endosc. 2:29–35. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yusuf TE and Brugge WR: Endoscopic therapy
of benign pyloric stenosis and gastric outlet obstruction. Curr
Opin Gastroenterol. 22:570–573. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Vlavianos P and Zabron A: Clinical
outcomes, quality of life, advantages and disadvantages of metal
stent placement in the upper gastrointestinal tract. Curr Opin
Support Palliat Care. 6:27–32. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
van Groeningen CJ: Intravenous and
intra-arterial chemotherapeutic possibilities in biliopancreatic
cancer. Ann Oncol. 10(Suppl 4): 305–307. 1999.PubMed/NCBI
|
|
36
|
Fisher SB, Fisher KE and Maithel SK:
Molecular targeted therapy for biliary tract malignancy: defining
the target. Hepatobiliary Surg Nutr. 1:53–54. 2012.PubMed/NCBI
|