Introduction
Eccrine spiradenoma (ES) is a rare, benign adnexal
neoplasm that has been historically designated as a tumor of
eccrine differentiation. ES is able to be present on any part of
the body (1), with ~1/5 cases
occurring in the extremities (2).
ES can appear at any age, and no gender predominance has been
reported. The treatment of choice of ES is surgical excision with
clear margins, while recurrence has been documented in the
literature (3). Malignant
transformation of ES is rare, but malignant ES is quite aggressive
and can occur within a long-standing lesion that makes the early
definitive diagnosis of ES of major importance. ES may easily be
mistaken for glomus lesions or angioleiomyoma due to its
painfulness and florid vascularization. In the current case study,
a noteworthy case of ES in the left knee is presented, with focus
upon its clinical presentation, histopathological characteristics
and differential diagnosis from other painful subcutaneous tumors
that exhibit a similarly high degree of vascularization.
Case report
Case summary
A 44-year-old male presented with a blue intradermal
nodule ~1 cm in size localized in the left knee. The tumor was
initially observed 10 years previously without any associated pain
or pruritus and gradually enlarged thereafter. Dermatological
examination revealed a firm, tender and blue nodule with a smooth
surface and obscure boundaries (Fig.
1). Stromal infiltration was evident without epidermal
connections. Routine investigations were within normal limits and
the patient revealed no other significant past medical or family
history. Surgical excision of the subcutaneous lesion was performed
and the tissue was submitted for microscopic examination. The
patient was treated by a local, complete excision without
recurrence 16 months later. The study was approved by the Second
Affiliated Hospital of Xi’an Jiaotong University (Xi’an, China) and
written informed consent was obtained from the patient.
Histopathological examination
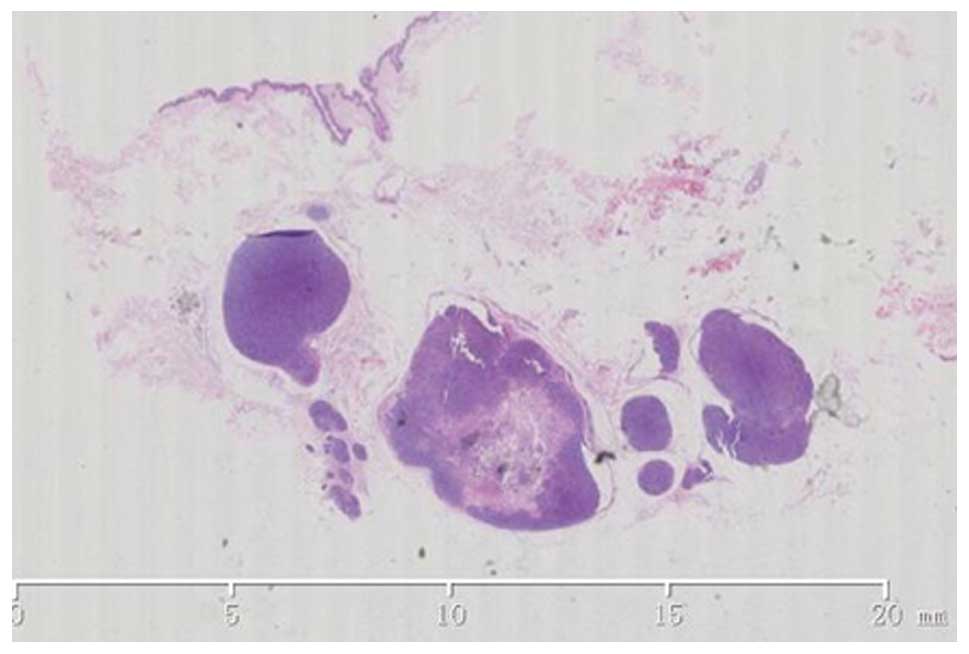
An excisional biopsy was performed. Histological
examination revealed multiple strongly basophilic lobules arranged
in sheets in the dermal and subcutaneous tissue. The overlying
epidermis was almost intact without connections to the tumor island
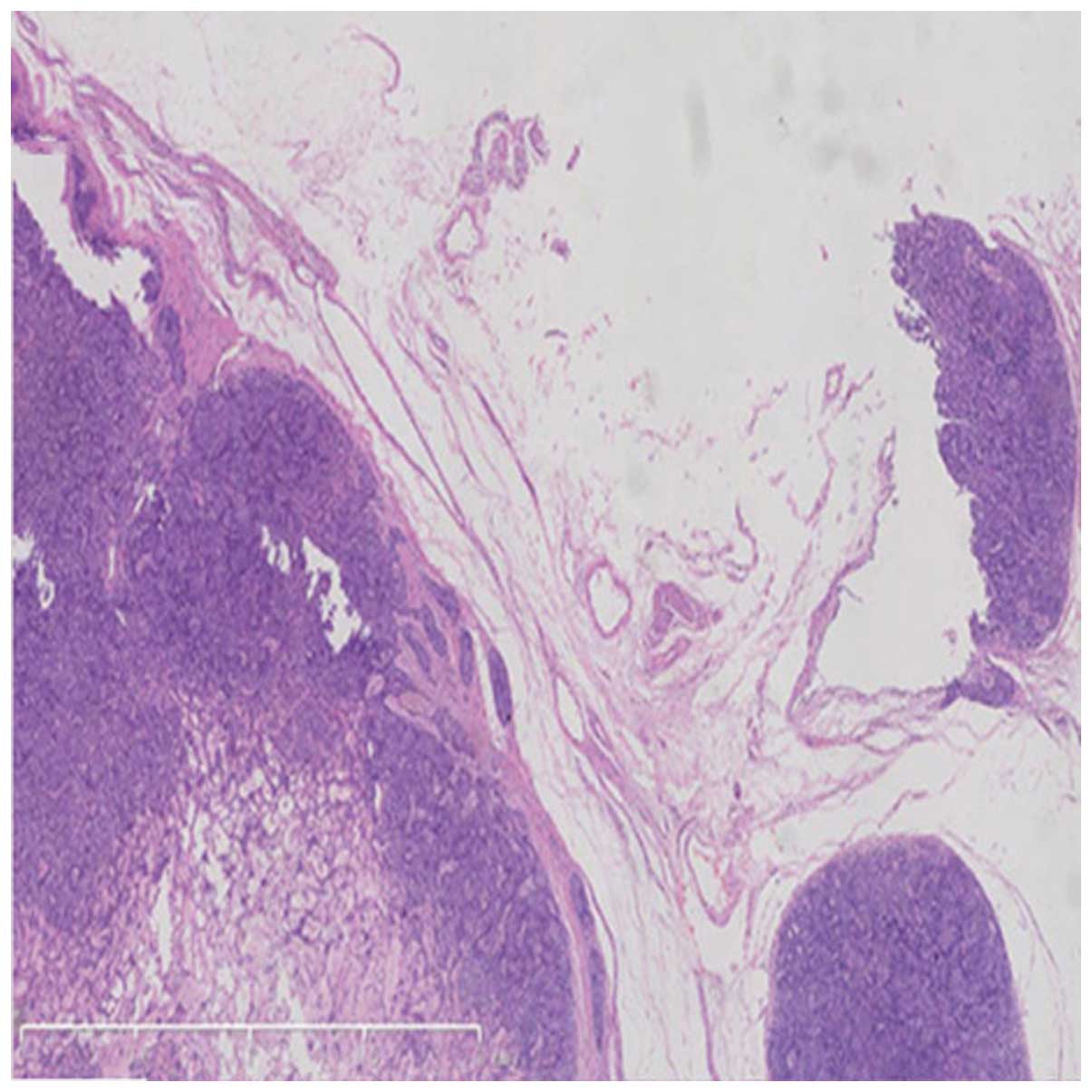
(Fig. 2). The nodule was well
marginated and encased by an abundant eosinophilic capsule
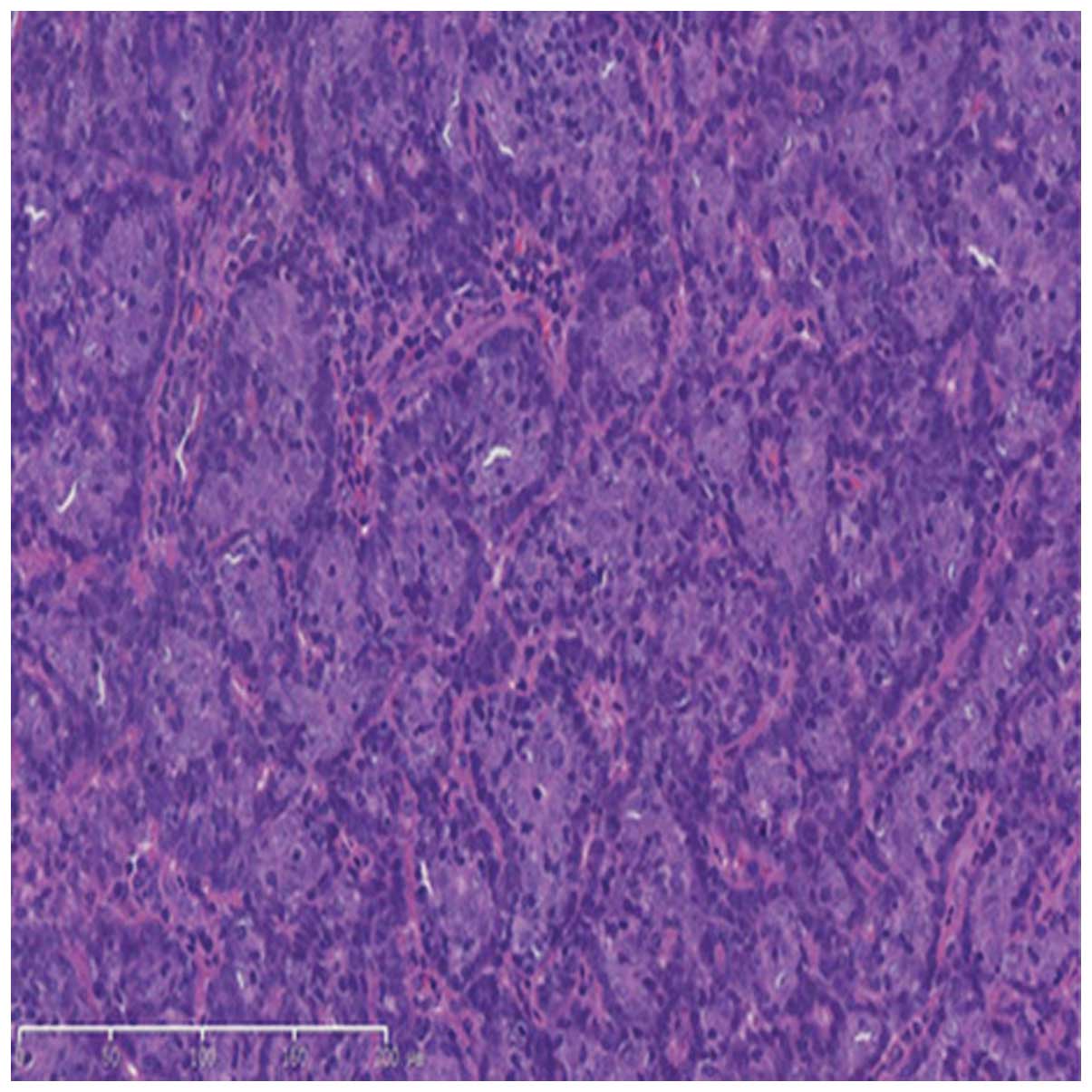
(Fig. 3). Two types of cells were
recognized in the lobules, namely small, darkly stained basaloid
cells located at the periphery and larger cells with a pale and
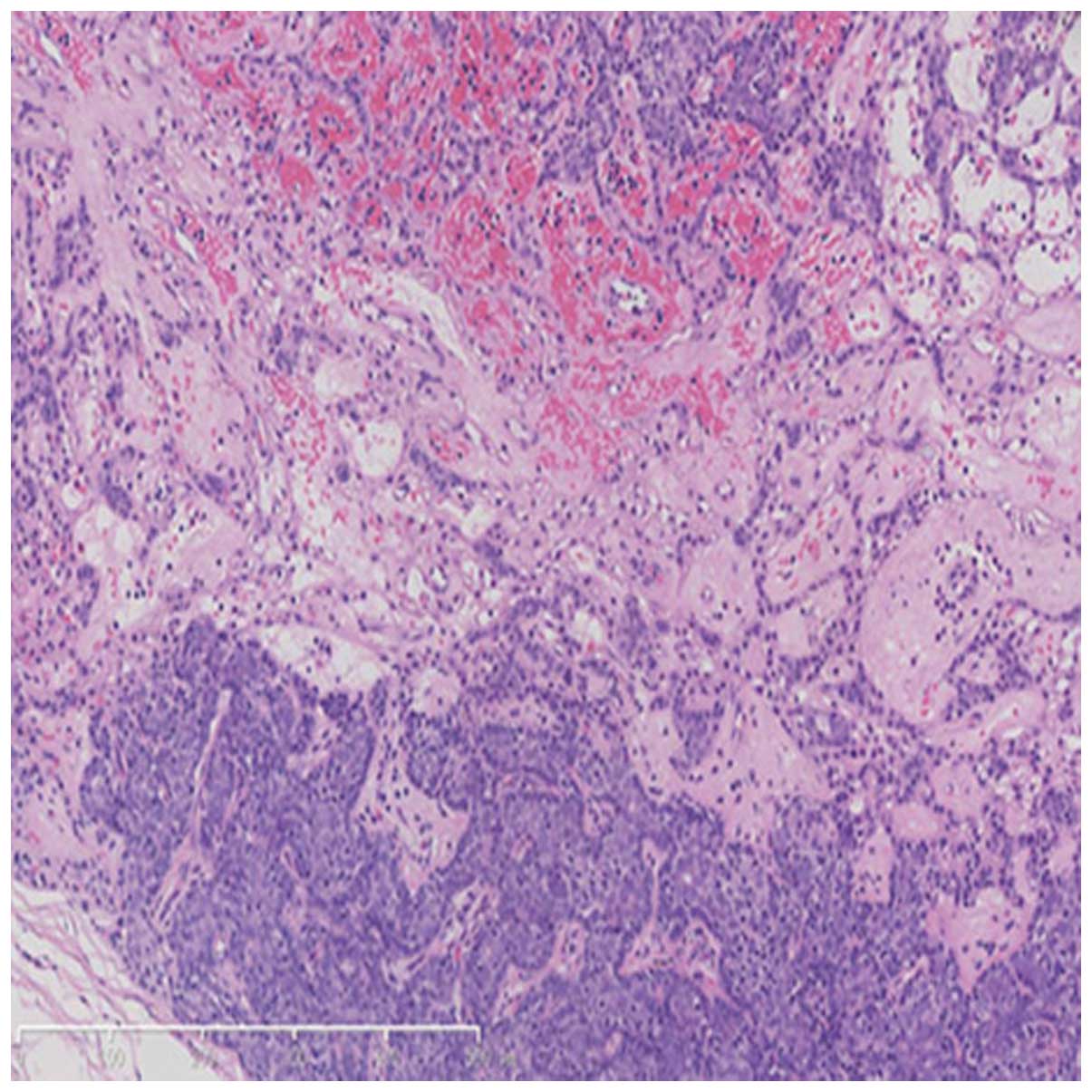
acidophilic nucleus situated mainly in the center (Fig. 4). Tumor cells were arranged
irregularly into small cystic sweat gland ducts, lined with the
acidophilic epithelial cells. Certain tubular differentiations were
conspicuous among the tumor cells, as well as lymphocyte
infiltration and abundant telangiectasia, with irregular clearance
identified in the lumen. However, mitosis was not observed
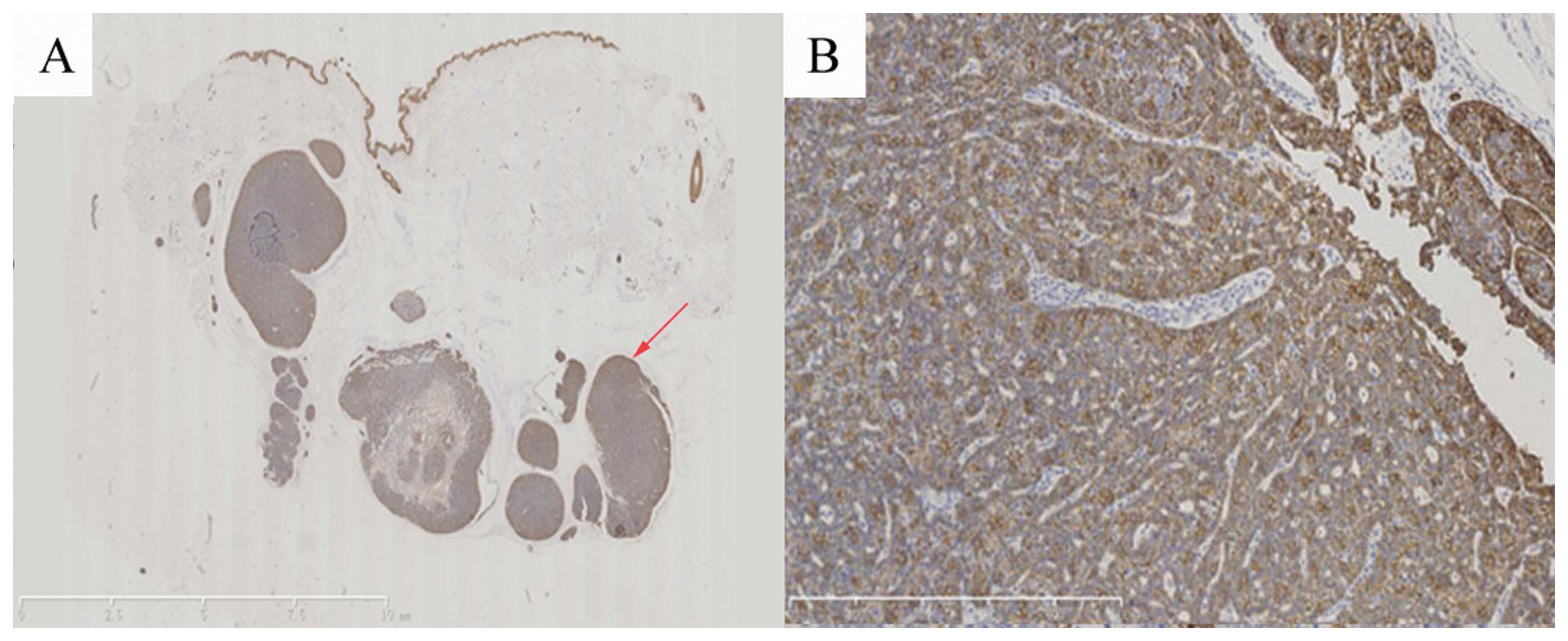
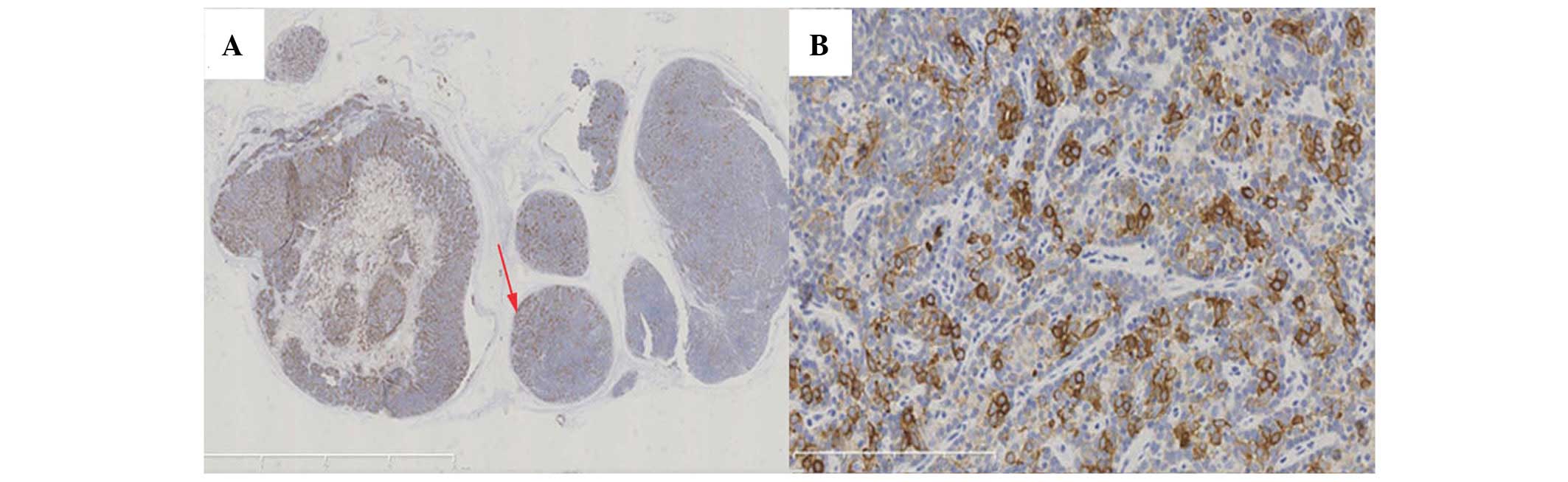
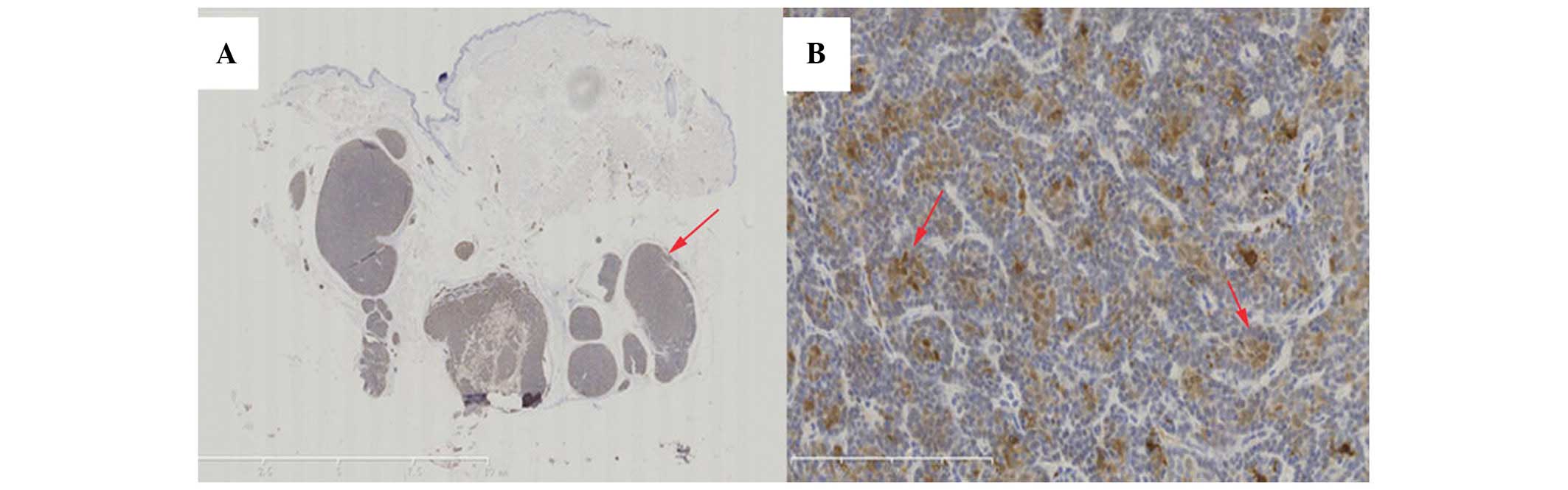
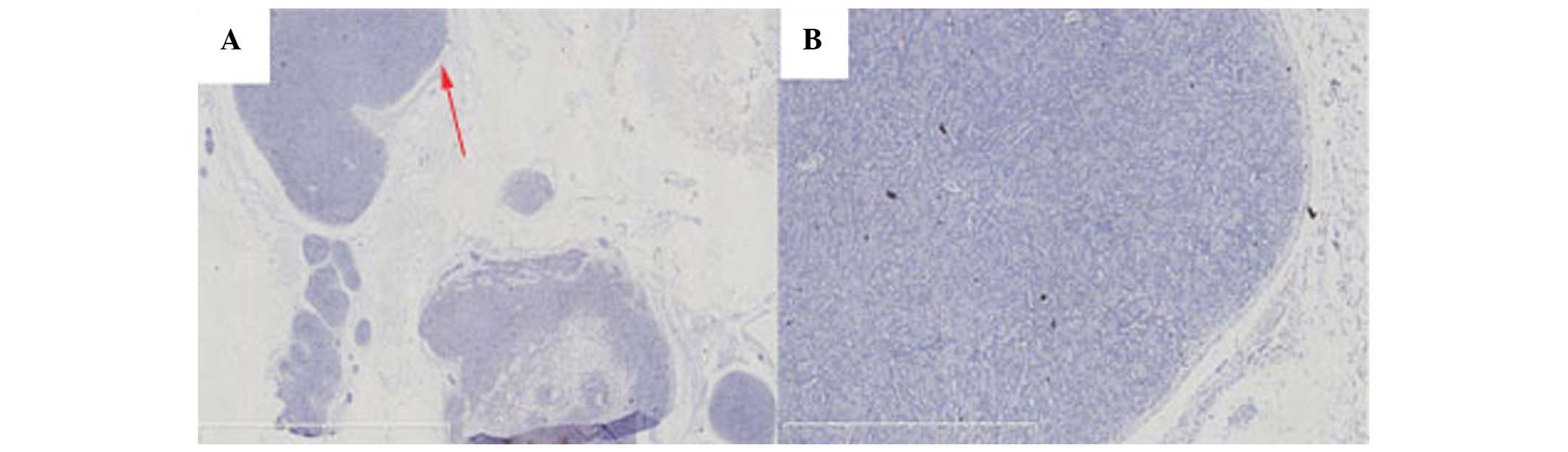
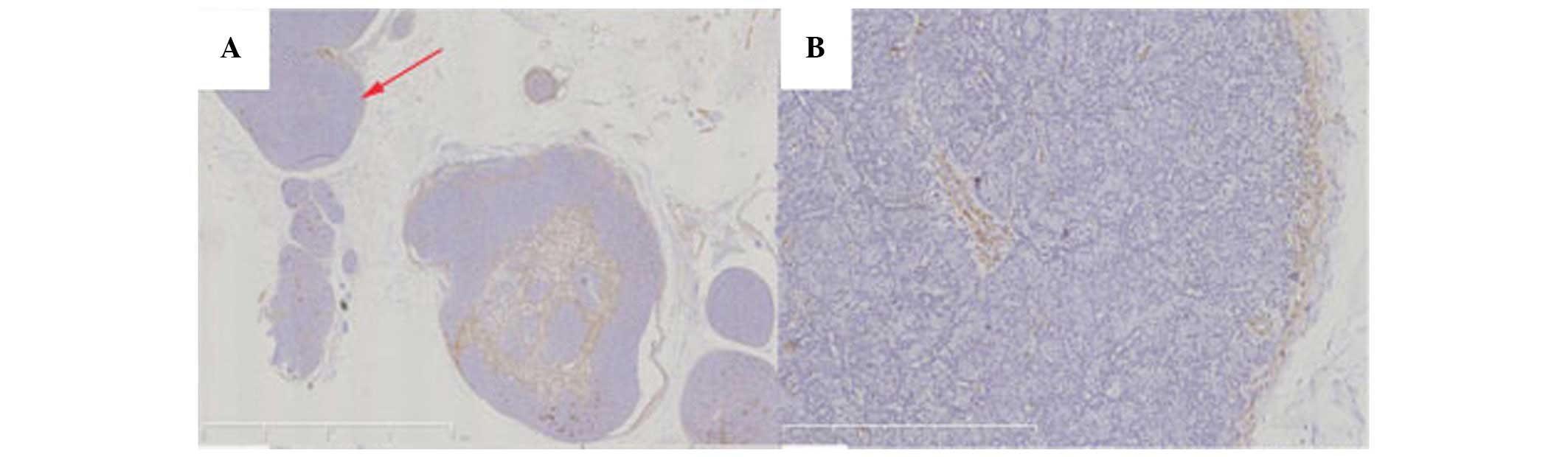
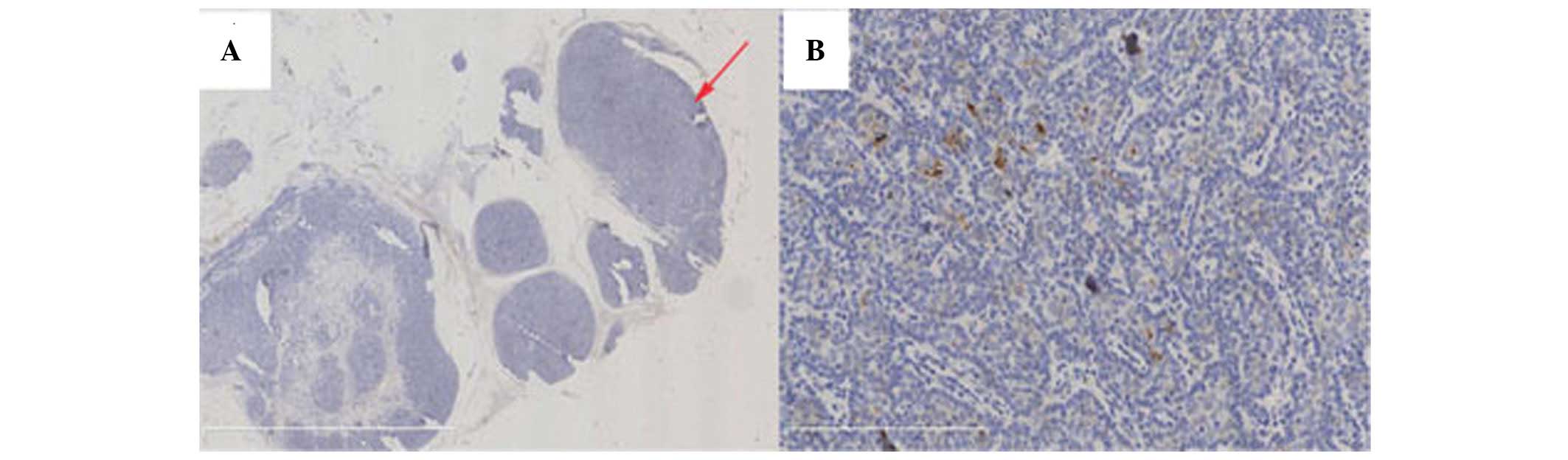
(Fig. 5). The immunohistochemical
staining of the tumors revealed positive immunoreactions for
cytokeratin (CK)5/CK6 (Fig. 6),
CK8/CK18 (Fig. 7) and S100
(Fig. 8); and negative
immunoreactions for carcinoembryonic antigen (CEA; Fig. 9) and smooth muscle actin (SMA)
(Fig. 10). Staining with
anti-endomysial antibody (EMA) revealed positive vacuole-like
structures on the surfaces of the glands and intracytoplasmic
lumens in certain tumor cells (Fig.
11). From these results, a diagnosis of the tumor as ES was
established.
Differential diagnosis
ES may be easily mistaken for other lesions that
characteristically present with localized pain and/or a marked
degree of vascularization. These include: i) aggregated lymphatic
nodules; in the primary clinical differential diagnosis, the
immunohistochemical results are usually clear (tubular
differentiation was demonstrated in the present case); ii) glomus
tumor, a benign neoplasm characteristically associated with
conspicuous vasculature components (poor vasculature was observed
in the current case); and iii) angioleiomyoma, a benign tumor
arising from the vascular smooth muscle typically expressing SMA
(which was negative in the present case).
Discussion
Eccrine spiradenoma (ES), as first described in
1956, is a rare, benign adnexal neoplasm that is able to present on
any part of the body, with ~1/5 of cases occurring in the
extremities (4). The present study
reported a case of ES located in the left knee. It classically
presents in patients between the ages of 20 and 40 years and is
primarily described as a firm or soft and spongy textured, round or
ovoid-shaped and blue-colored lobulated mass, ranging in size from
0.5 to 5 cm in diameter. The most striking clinical feature of ES
lesions is the presence of pain or tenderness (3); however, no excruciating pain was
presented in the current case. The majority of ES presentations are
solitary, with males and females being affected equally (5). The presence of concomitant cylindroma
and trichoepithelioma in certain ES patients may increase the
possibility of Brooke-Spiegler syndrome (6). Malignant transformation is extremely
rare and generally arises from long-standing benign ES (7).
Histologically, ES may present in a variety of ways,
including as tumors arranged in sheets, cords or islands, often
precluding a straightforward diagnosis. Tumor cells are strongly
basophilic, resembling lymph nodes when observed under a low power
microscope. In certain cases, lymphocyte infiltration and abundant
telangiectasia are observed in the tumor region, with irregular
clearance presented around the lumen. A differential diagnosis for
glomus tumors should be performed when vascular hyperplasia is
statistically significant. Occasionally, a nerve trunk may be
observed in the vicinity of the lobules, as identified in the
present case.
The diagnosis of ES may be elusive given its
multiple presentations without a change in the skin surface.
Correct diagnosis is critical due to the potential for malignancy.
The primarily clinical feature of ES is the presence of pain in the
patient (8) and painful dermal
tumors should be taken into consideration on initial evaluation.
Entities including angioma, angioleiomyoma and neuroma should be
considered in the further differential diagnosis of ES given their
similar presentations. The diagnosis may be distinguished
histologically if the clinical picture is not distinctive. However,
the histological results of ES have been observed to be consistent
with those of cylindroma within the same biopsy, as numerous tumors
demonstrate overlapping features between the two entities (9). A previous study suggested that the
two entities may represent two extremes on a continuous spectrum of
dermal tumors that originate from a common progenitor (3). The histological differentiation of
cylindroma and ES is less straightforward; although, with the help
of pathological and immunohistochemical presentations, an improved
diagnosis may be achieved. Furthermore, when the tubular
differentiation of the intralobular duct cells is less significant,
it may be mistaken for an aggregated lymphatic nodule.
Immunohistochemical methods may be used for its differential
identification.
A clinical differential diagnosis of glomus
tumor/aggregated lymphatic nodule was offered in the current case.
The diagnosis could not be confirmed from the clinical and
histological investigations and an immunohistochemical assay was
performed. A diagnosis of ES was suggested on the basis of ductal
differentiation and poor vasculature identified following
immunohistochemical staining of the excised tumor mass.
ES has been historically designated as a tumor of
eccrine lineage, although the current view is that it may arise due
to an apocrine process (3,10). In the current case, the
immunophenotype of the tumor exhibited characteristic features of
eccrine differentiation along with the expression of the S100
protein and CK5/CK6. Staining with an anti-EMA antibody revealed
small vacuole-like positivity of the lumen surfaces, while the
tumor cell staining for CEA and SMA antibodies was negative. There
was no clear evidence of myoepithelial differentiation. However,
tubular differentiation of tumor cells was also demonstrated, which
would be expected in an apocrine neoplasm (11,12).
Thus, further investigation was required.
Treatments for ES have not been well established;
however, surgical excision is currently the gold standard option,
with low rates of recurrence documented (3). Other treatment options, including
radiotherapy, carbon dioxide laser ablation and chemotherapy, have
also been proposed although no studies have substantiated an
optimal practice (13). For cases
of familial ES, genetic counseling has been advised (14).
Acknowledgements
The authors would like to express special thanks to
Professors Jianfang Sun, Changzheng Huang and Hao Chen for their
help with diagnosis.
References
|
1
|
Nadig SK, Alderdice JM, Adair RA and Rao
TJ: Eccrine spiradenoma: an unusual presentation with otalgia.
Otolaryngol Head Neck Surg. 130:277–278. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wong DR, Olson DA and Dresner HS: A rare
case of eccrine spiradenoma of the upper lip. The Laryngoscope.
120:S522010. View Article : Google Scholar
|
|
3
|
Englander L, Emer JJ, McClain D, Amin B
and Turner RB: A rare case of multiple segmental eccrine
spiradenomas. J Clin Aesthet Dermatol. 4:38–44. 2011.PubMed/NCBI
|
|
4
|
Kersting DW and Helwig EB: Eccrine
spiradenoma. AMA Arch Derm. 73:199–227. 1956. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nath AK, Kumari R and Thappa DM: Eccrine
spiradenoma with chondroid syringoma in Blaschkoid distribution.
Indian J Dermatol Venereol Leprol. 75:600–602. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Weyers W, Nilles M, Eckert F and Schill
WB: Spiradenomas in Brooke-Spiegler syndrome. Am J Dermatopathol.
15:156–161. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Braun-Falco M, Bonel H, Ring J and Hein R:
Linear spiradenoma with focal malignant transformation. J Eur Acad
Dermatol Venereol. 17:308–312. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Park HR, Im SB, Kim HK, Shin DS and Park
YL: Painful eccrine spiradenoma containing nerve fibers: a case
report. Dermatology. 224:301–306. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bumgardner AC, Hsu S, Nunez-Gussman JK and
Schwartz MR: Trichoepitheliomas and eccrine spiradenomas with
spiradenoma/cylindroma overlap. Int J Dermatol. 44:415–417. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jin W, Kim GY, Lew BL, et al: Sonographic
findings of an eccrine spiradenoma: case report and literature
review. J Ultrasound Med. 27:813–818. 2008.PubMed/NCBI
|
|
11
|
Wong TY, Suster S, Cheek RF and Mihm MC
Jr: Benign cutaneous adnexal tumors with combined
folliculosebaceous, apocrine, and eccrine differentiation:
Clinicopathologic and immunohistochemical study of eight cases. Am
J Dermatopathol. 18:124–136. 1996. View Article : Google Scholar
|
|
12
|
Lian F and Cockerell CJ: Cutaneous
appendage tumors: familial cylindromatosis and associated tumors
update. Adv Dermatol. 21:217–234. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Andreoli MT and Itani KM: Malignant
eccrine spiradenoma: a meta-analysis of reported cases. Am J Surg.
201:695–699. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ter Poorten MC, Barrett K and Cook J:
Familial eccrine spiradenoma: a case report and review of the
literature. Dermatol Surg. 29:411–414. 2003.PubMed/NCBI
|