Introduction
Benign lymphoepithelial lesions (BLELs) show three
histological characteristics: Hyperplasia and infiltration of
lymphocytes into the gland, atrophy of the gland parenchyma and
hyperplasia and infiltration of epimyoepithelial islands in the
gland duct. In 1952, Godwin denominated the condition as ‘benign
lymphoepithelial lesion’ (1),
which was newly classified as a benign salivary gland tumor in 1991
(2). BLELs were not considered to
be tumors, but rather a type of reactive hyperplasia, characterized
by a benign, long progression, which was not life-threatening and
was rarely malignant in patients. BLELs appear mainly in unilateral
or bilateral parotid tissues and the submandibular gland; however,
cases of lymphoepithelial lesions of the salivary gland are rare,
comprising <3% of benign salivary gland tumors. At present, no
standard therapy regimen is available for BLELs; however,
glucocorticoid therapy, such as the administration of
cyclophosphamide with prednisone, as an alternative to surgery has
been reported (3,4). A recent study demonstrated that BLELs
are sensitive to radiotherapy, which may be beneficial in recurrent
lesions (5). Although surgery and
radiation are the main treatment methods (6–9),
BLELs of the salivary gland have been rarely studied and no common
therapy criteria or adoptive cellular immunotherapy have been
reported.
Case report
A 22-year-old female was admitted to the Jilin
Cancer Hospital (Changchun, China) in May 2013. In January 2009, a
2.0×3.0 cm painless mass was surgically removed from the left
parotid gland of the patient. Postoperative pathology characterized
the mass as a lymphocytic hyperplasia; however, parotid duct cells
were also detected within the lymphocytes. Morphological results
and immunohistochemical staining supported the diagnosis of a
BLEL.
BLEL recurrence and long term
development
After six months, the left parotid gland became
locally swollen again and intermittent management with traditional
Chinese medicine was unable to achieve remission. In October 2010,
the size of the mass reached 5.0×6.0 cm. A computerized tomography
(CT) scan of the parotid gland indicated a soft tissue mass in the
left neck area without uniform density or a clear border with the
left parotid gland, and evident infiltration in the surrounding
tissue. The mass was considered to be a recurrence of the BLEL in
the left parotid gland; however, the patient did not agree to
further surgical therapy. The mass in the left parotid gland area
became gradually enlarged, and was more evident when the patient
became ill with a cold; however, the mass was slightly reduced
following anti-infective treatment (mainly with cephalosporins).
The patient also received traditional Chinese medicine for six
months and local acupuncture therapy for 40 days. However, the mass
in the left parotid gland area was continually increasing in size
and reached a diameter of 15 cm. On April 27 2013, the patient
developed a fever of up to 40°C, accompanied with shivering,
weakness and a loss of appetite, which was more severe in the
afternoon and at night. Remission was observed following
self-medication with oral ibuprofen; however, the temperature of
the patient increased after several hours and a light yellow, clear
liquid was discharged from the ulceration on the skin surface of
the left parotid gland mass. On May 4 2013, the patient visited the
Jilin Cancer Hospital, where the local ulceration and infection of
the left parotid gland mass was managed with anti-infective
treatment for three days; however, the high temperature of the
patient did not decrease and the mass did not reduce in size. The
patient was admitted to the hospital for further therapy on May 8
2013, and physical examination identified a large mass of 17×14 cm
on the left side of the patient’s face, a red and swollen skin
surface and multiple ruptures in the middle of the mass with a
light yellow liquid discharge. The peripheral skin of the mass was
tenacious and swollen, and the skin temperature was high. A blood
routine examination and liver and renal functions were found to be
normal. Color ultrasound revealed a visible 18.2×8.5-cm low-echo
area with strong-echo stripes under the skin on the left side of
the patient’s face, without the appearance of a clear margin. Color
Doppler flow imaging revealed an abundant blood flow in the mass
and the absence of normal parotid gland tissue, indicating a solid
space-occupying lesion on the left parotid gland. A CT scan of the
left parotid gland revealed an abnormal mass in a low-density image
and an undefined margin of the lesion, with the superior border
extending towards the orbit, the inferior border at the
submaxillary level, the inner border at the left parapharyngeal
space and the outside border at the skin of the left-side of the
face. The mass reached 13.4×9.7 cm in an axial view, showing
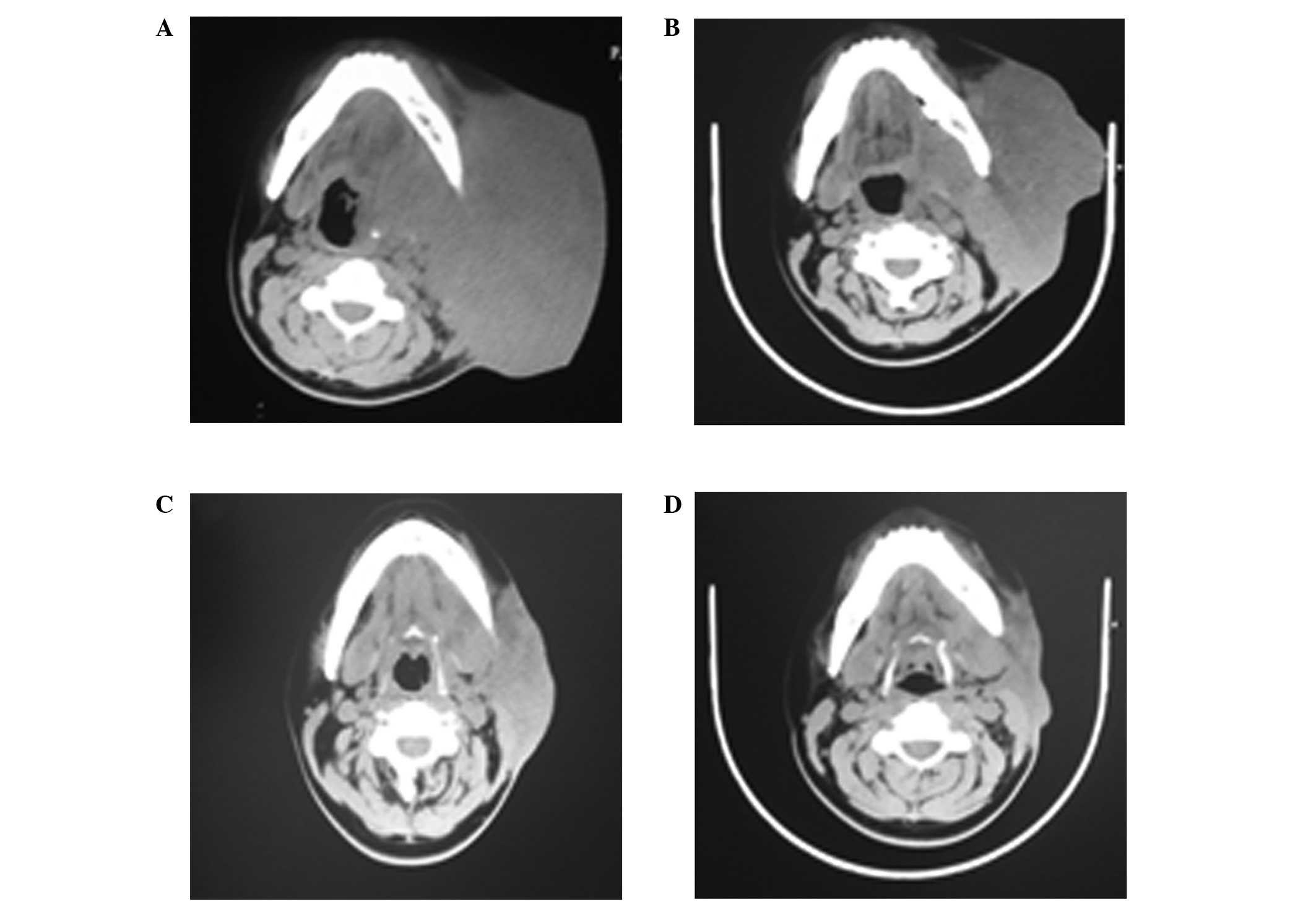
uniform density and a CT value of 47 HU (Fig. 1A), with the left parotid gland
unable to be distinguished. The lesion was wrapped around the left
sphenoid bone and mandible. In addition, morphological changes were
observed, indicating recurrence of the BLEL in the left parotid
gland with bone resorption of the sphenoid bone and mandible. A
bacterial culture of the mass discharge indicated a
Staphylococcus aureus infection, which was sensitive to
levofloxacin. The body temperature of the patient returned to
normal levels following the administration of levofloxacin for one
week. A biopsy was not performed due to the weakness, high fever,
local swelling and infection of the patient, as well as the
abundant blood flow detected in the mass with color ultrasound. No
consensus was reached with regard to further surgical intervention.
Drugs inhibiting vascular endothelial growth (Endostar and Shenyi
capsules) were administered for five days, but were discontinued by
the patient due to local pain and swelling. Chemoradiotherapy was
subsequently considered; however, due to the young age of the
patient and the examination results not indicating malignance, the
patient did not agree to the therapy.
Dendritic cell-cytokine-induced killer
cell (DC-CIK) biotherapy
Following failed conservative treatment, DC-CIK
therapy was initiated based on the immune index result of the
patient, which found the percentage of inhibitory T cells to be
32.2% (CD8+CD28−; normal range, 9.8–21.8%)
and the CD4+/CD8+ ratio to be 0.42 (Table I), indicating low immunity. The
patient signed informed consent for the treatment protocol, which
was approved for tumor patients by the Health Department of Jilin
Province (Changchun, China) and the Ethics Committee of the Jilin
Cancer Hospital.
 | Table IChanges in the T cell subpopulations
during DC-CIK adoptive cellular immunotherapy treatment. |
Table I
Changes in the T cell subpopulations
during DC-CIK adoptive cellular immunotherapy treatment.
| Analysis date | Total T
lymphocytesa (CD3+),
% | Suppressor T
cellsb
(CD3+CD8+), % | Inhibitory T
cellsc
(CD3+CD28−), % | Regulatory T
cellsd
(CD4+CD25+), % | Immune statuse (CD4+/CD8+
ratio) |
|---|
| Jun 8 2012 | 79.2 | 59.3 | 32.2 | 0.7 | 0.42 |
| Jun 28 2012 | 55.7 | 38.6 | 28.8 | 1.2 | 0.47 |
| Jul 17 2012 | 35.7 | 18.1 | 14.8 | 1.0 | 0.87 |
| Sep 5 2012 | 54.3 | 30.1 | 20.8 | 1.7 | 0.68 |
Source of cells
Antigen-presenting DCs and CIK cells were produced
using heat shock protein-70, extracted from a head and neck
squamous carcinoma cell strain supplied by the Jilin Cancer
Hospital, and cocultured with cord blood DCs.
DC-CIK protocol
The duration of the first treatment session was 10
days, after which the treatment was discontinued for 10 days.
Following the initial treatment course, the lesion in the left
parotid gland area was reduced, while the local infection and skin
ulceration were soothed. Biotherapy was continued for three months
(four sessions of treatment), after which the left parotid gland
lesion disappeared and the skin ulceration was healed.
Treatment outcome
Parotid gland CT scans (Fig. 1B–D) indicated that the primary
lesion of the left parotid gland area disappeared gradually and the
bone destruction was completely recovered. The patient was
discharged from hospital and the condition remained stable without
signs of recurrence during a follow-up period of 10 months;
however, the patient remains under close observation.
Discussion
BLELs, also known as Mikulicz disease (MD), were
first reported by Mikulicz in 1888 and are characterized by
chronic, painless and symmetric swelling of tear and salivary
glands (10–12). When a BLEL is combined with certain
systematic diseases, including sarcoidosis leukemia, viral
infections and macroglobulinemia, the condition is also known as
Mikulicz syndrome. In 1933, the Swedish optician, Sjögren,
identified a chronic systematic disease, known as Sjögren’s
syndrome (SS), which primarily involved the salivary and tear
glands (13). SS manifests as a
dry mouth and xerotic keratitis, and occasionally occurs alongside
other chronic connective tissue diseases. Due to the similar
histological and pathological findings in MD and SS patients,
Morgan and Raven proposed that MD is a subdisease of SS (14). Mihas et al hypothesized that
MD, BLEL and SS may be conditions of the same disease process, with
malignant lymphoma being a common complication (15). Due to the symptom similarities, the
diagnosis of a BLEL is mainly based on clinical observations. An
homogeneous, painless mass with a clear boundary at the tear gland,
the absence of bone destruction and accompanied by a swollen
salivary gland and dry mouth, can be diagnosed as a BLEL. However,
prior to BLEL diagnosis, dry eyes, systematic connective tissue
diseases and lymphoma and inflammatory pseudotumors should be
excluded. In addition, diffuse hyperplasia and lymphocyte
infiltration of the gland, atrophy of the gland parenchyma and the
formation of epimyoepithelial islands in the gland duct should be
pathologically confirmed (4).
The etiology of BLELs remains unclear. Tsubota et
al revealed that although the pathologies of MD and SS are
similar, the lacrimal gland acinar cells in SS patients were
apoptotic with high protein expression levels of Fas and FasL, in
contrast to the acinar cells of MD patients (16). In addition, Yamamoto et al
observed that the serum concentration of the IgG4 antibody in BLEL
patients was much higher when compared with the SS patients, and
hypothesized that BLELs are a systematic disease correlating with
IgG4 (17). Gupta et al
revealed that the BLEL epimyoepithelial islands were predominantly
surrounded by B lymphocytes and partially by T lymphocytes,
indicating that humoral immunity was involved in BLELs (18). Initial T cell blood analysis of the
patient in the present study revealed a high percentage of total T
lymphocytes (CD3+), suppressor T cells
(CD3+CD8+) and inhibitory T cells
(CD3+CD28−), while a low
CD4+/CD8+ ratio and number of regulatory T
cells were observed. CD3+CD8+ cells have been
identified as malignant in 85% of granular lymphocyte leukemias
(19), and previous studies have
revealed that large granular lymphocyte leukemias are strongly
associated with SS, in addition to other autoimmune diseases
(20–22). A low
CD4+/CD8+ ratio, also observed in
HIV-infected patients, is generally a sign of a weak immune system.
Thus, in combination with the abnormally high percentages of
inhibitory and suppressor T cells, the patient in the present study
was considered to have a weakened immune system. In order to
strengthen the patient’s immunity, DC-CIK therapy was attempted,
which had been previously used in the treatment of non-small cell
lung cancer (23–25). As a result, the percentages of
suppressor, inhibitory and regulatory T cells returned to within
the normal ranges and the CD4+/CD8+ ratio
increased. However, the total T lymphocyte percentage decreased to
below the normal range. Although the exact hematological mechanisms
remain unclear and further analysis is required, considering the
outcome of this first trial, DC-CIK therapy may be a promising
approach for the treatment of BLELs.
References
|
1
|
Godwin JT: Benign lymphoepithelial lesion
of the parotid gland adenolymphoma, chronic inflammation,
lymphoepithelioma, lymphocytic tumor, Mikulicz disease. Cancer.
5:1089–1103. 1952. View Article : Google Scholar
|
|
2
|
Seifert G, Brocheriou C, Cardesa A and
Eveson JW: WHO international histological classification of
tumours. Tentative histological classification of salivary gland
tumours. Pathol Res Pract. 186:555–581. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Albrecht H, Stellbrink HJ and Greten H:
Resolution of HIV-associated cystic benign lymphoepithelial lesion
of the parotid gland in a patient undergoing chemotherapy for
non-Hodgkin’s lymphoma. Scand J Infect Dis. 28:621–623.
1996.PubMed/NCBI
|
|
4
|
Tang DR, Shi XF, Sun FY, Zhao H and Jin
YJ: Clinical features and therapy of benign lymphoepithelial
lesion. Zhonghua Yan Ke Za Zhi. 45:441–445. 2009.(In Chinese).
|
|
5
|
Mourad WF, Hu KS, Shourbaji RA, Lin W and
Harrison LB: Radiation therapy for benign lymphoepithelial cysts of
parotid glands in HIV patients. Laryngoscope. 123:1184–1189. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hsiung CY, Huang CC, Wang CJ, Huang EY and
Huang HY: Lymphoepithelioma-like carcinoma of salivary glands:
treatment results and failure patterns. Br J Radiol. 79:52–55.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sato K, Kawana M, Sato Y and Takahashi S:
Malignant lymphoma in the head and neck associated with benign
lymphoepithelial lesion of the parotid gland. Auris Nasus Larynx.
29:209–214. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schneider M and Rizzardi C:
Lymphoepithelial carcinoma of the parotid glands and its
relationship with benign lymphoepithelial lesions. Arch Pathol Lab
Med. 132:278–282. 2008.PubMed/NCBI
|
|
9
|
Ussmüller J, Reinecke T, Donath K and
Jaehne M: Chronic myoepithelial sialadenitis - symptomatology,
clinical signs, differential diagnostics. Laryngorhinootologie.
81:111–117. 2002.(In German).
|
|
10
|
Andrade RE, Hagen KA and Manivel JC:
Distribution and immunophenotype of the inflammatory cell
population in the benign lymphoepithelial lesion (Mikulicz’s
disease). Hum Pathol. 19:932–941. 1988.PubMed/NCBI
|
|
11
|
Sewkani A, Purohit D, Singh V, Jain A,
Varshney R and Varshney S: Lymphoepithelial cyst of the pancreas: a
rare case report and review of literature. Indian J Surg.
72:427–432. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cho HJ, Kyung Myung J, Kim YH, Choi SH and
Park SH: Benign lymphoepithelial tumor of the pituitary.
Neuropathology. 33:413–417. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sjögren H: Zur kenntis der
keratoconjunctivitis sicca II. Allgemeine Symptomatologie und
Ätiologie. Acta Ophthalmol. 13:1–39. 1935.
|
|
14
|
Morgan AD and Raven RW: Sjögren’s
syndrome: a general disease. Br J Surg. 40:154–162. 1952.
|
|
15
|
Mihas AA, Lawson PB, Dreiling BJ, Gurram
VS and Heuman DM: Mikulicz syndrome associated with a malignant
large cell gastric lymphoma: a case report and review of the
literature. Int J Gastrointest Cancer. 33:123–127. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tsubota K, Fujita H, Tsuzaka K and
Takeuchi T: Mikulicz’s disease and Sjögren’s syndrome. Invest
Ophthalmol Vis Sci. 41:1666–1673. 2000.
|
|
17
|
Yamamoto M, Naishiro Y, Suzuki C, et al:
Proteomics analysis in 28 patients with systemic IgG4-related
plasmacytic syndrome. Rheumatol Int. 30:565–568. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gupta N, Gupta R, Rajwanshi A and Bakshi
J: Multinucleated giant cells in HIV-associated benign
lymphoepithelial cyst-like lesions of the parotid gland on FNAC.
Diagn Cytopathol. 37:203–204. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rose MG and Berliner N: T-cell large
granular lymphocyte leukemia and related disorders. Oncologist.
9:247–258. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ergas D, Tsimanis A, Shtalrid M, Duskin C
and Berrebi A: T-gamma large granular lymphocyte leukemia
associated with amegakaryocytic thrombocytopenic purpura, Sjögren’s
syndrome, and polyglandular autoimmune syndrome type II, with
subsequent development of pure red cell aplasia. Am J Hematol.
69:132–134. 2002.PubMed/NCBI
|
|
21
|
Molad Y, Okon E, Stark P and Prokocimer M:
Sjögren’s syndrome associated T cell large granular lymphocyte
leukemia: a possible common etiopathogenesis. J Rheumatol.
28:2551–2552. 2001.
|
|
22
|
Coakley G: Sjögren’s syndrome associated T
cell large granular lymphocyte leukemia: a possible common
etiopathogenesis. J Rheumatol. 29:18032002.
|
|
23
|
Shi SB, Ma TH, Li CH and Tang XY: Effect
of maintenance therapy with dendritic cells: cytokine-induced
killer cells in patients with advanced non-small cell lung cancer.
Tumori. 98:314–319. 2012.PubMed/NCBI
|
|
24
|
Li H, Wang C, Yu J, et al: Dendritic
cell-activated cytokine-induced killer cells enhance the anti-tumor
effect of chemotherapy on non-small cell lung cancer in patients
after surgery. Cytotherapy. 11:1076–1083. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yang L, Ren B, Li H, et al: Enhanced
antitumor effects of DC-activated CIKs to chemotherapy treatment in
a single cohort of advanced non-small-cell lung cancer patients.
Cancer Immunol Immunother. 62:65–73. 2013. View Article : Google Scholar : PubMed/NCBI
|